Impacts of a COVID-19 Educational Video: Evaluation of the Influence of Race, Gender, Political Affiliation, Study Major, and Age on Vaccine Acceptance among University Students
Abstract
:1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Survey Instrument
2.3. Measurements
2.4. Statistical Analysis
3. Results
3.1. Demographics
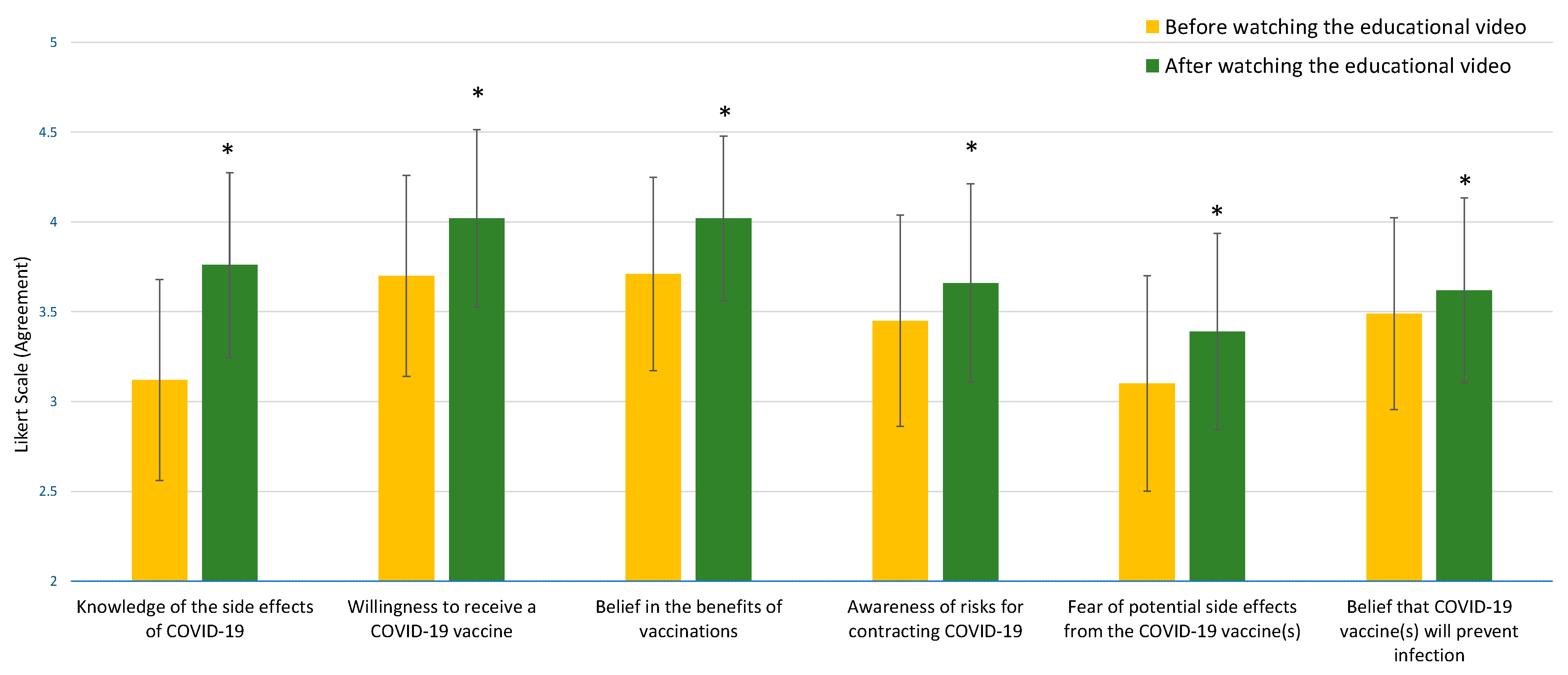
3.2. Effects of Video
3.3. Impact of the Video and Demographic Factors: Race, Study Majors, Gender, Political Affiliation, Age, and Influenza Vaccine History
3.4. Motivating Factors Affecting COVID-19 Vaccine Willingness
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Wu, F.; Zhao, S.; Yu, B.; Chen, Y.-M.; Wang, W.; Song, Z.-G.; Hu, Y.; Tao, Z.-W.; Tian, J.-H.; Pei, Y.-Y.; et al. A New Coronavirus Associated with Human Respiratory Disease in China. Nature 2020, 579, 265–269. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Director-General’s Opening Remarks at the Media Briefing on COVID-19—11 March 2020. Available online: https://who.int/director-general/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-COVID-19---11-march-2020 (accessed on 6 August 2023).
- Centers for Disease Control and Prevention. How to Protect Yourself & Others. Available online: https://cdc.gov/coronavirus/2019-ncov/prevent-getting-sick/prevention.html (accessed on 6 August 2023).
- Kavan, S. Selected social impacts and measures resulting from the COVID-19 epidemic in the Czech Republic on the specific example of the South Bohemian Region. Health Soc. Care Community 2021, 29, e224–e231. [Google Scholar] [CrossRef] [PubMed]
- Fuller, J.A.; Hakim, A.; Victory, K.R.; Date, K.; Lynch, M.; Dahl, M.; Henao, O.; CDC. COVID-19 Response Team. Mitigation Policies and COVID-19–Associated Mortality—37 European Countries, January 23-June 30, 2020. MMWR Morb. Mortal. Wkly Rep. 2021, 70, 58–62. [Google Scholar] [CrossRef] [PubMed]
- Ling, G.H.T.; Md Suhud, N.A.B.; Leng, P.C.; Yeo, L.B.; Cheng, C.T.; Ahmad, M.H.H.; Ak Matusin, A.M.R. Factors Influencing Asia-Pacific Countries’ Success Level in Curbing COVID-19: A Review Using a Social–Ecological System (SES) Framework. Int. J. Environ. Res. Public Health 2021, 18, 1704. [Google Scholar] [CrossRef] [PubMed]
- Centers for Disease Control and Prevention. CDC Strategy for Global Response to COVID-19 (2020–2023). Available online: https://cdc.gov/coronavirus/2019-ncov/global-COVID-19/global-response-strategy.html#:~:text=Reduce%20transmission%20of%20SARS%2DCoV,%2D%20and%20middle%2Dincome%20countries (accessed on 6 August 2023).
- Moreland, A.; Herlihy, C.; Tynan, M.A.; Sunshine, G.; McCord, R.F.; Hilton, C.; Poovey, J.; Werner, A.K.; Jones, C.D.; Fulmer, E.B.; et al. Timing of State and Territorial COVID-19 Stay-at-Home Orders and Changes in Population Movement—United States, 1 March–31 May 2020. MMWR Morb. Mortal. Wkly. Rep. 2020, 69, 1198–1203. [Google Scholar] [CrossRef] [PubMed]
- Centers for Disease Control and Prevention. Expired Order: Wearing of Face Masks While on Conveyances and at Transportation Hubs. Available online: https://www.cdc.gov/quarantine/masks/mask-travel-guidance.html (accessed on 6 August 2023).
- U.S. Department of Health and Human Services. COVID-19 Vaccines. Available online: https://hhs.gov/coronavirus/COVID-19-vaccines/index.html (accessed on 6 August 2023).
- U.S Food and Drug Administration. Pfizer-BioNTech COVID-19 Vaccine. Available online: https://wayback.archive-it.org/7993/20201217213102/https://fda.gov/emergency-preparedness-and-response/coronavirus-disease-2019-COVID-19/pfizer-biontech-COVID-19-vaccine (accessed on 6 August 2023).
- U.S Food and Drug Administration. Moderna COVID-19 Vaccines. Available online: https://fda.gov/vaccines-blood-biologics/coronavirus-COVID-19-cber-regulated-biologics/moderna-COVID-19-vaccines (accessed on 6 August 2023).
- U.S Food and Drug Administration. Janssen COVID-19 Vaccine. Available online: https://fda.gov/vaccines-blood-biologics/coronavirus-COVID-19-cber-regulated-biologics/janssen-COVID-19-vaccine (accessed on 6 August 2023).
- Plumb, I.D.; Feldstein, L.R.; Barkley, E.; Posner, A.B.; Bregman, H.S.; Hagen, M.B.; Gerhart, J.L. Effectiveness of COVID-19 mRNA vaccination in preventing COVID-19-associated hospitalization among adults with previous SARS-CoV-2 infection—United States, June 2021–February 2022. MMWR Morb. Mortal. Wkly. Rep. 2022, 71, 549–555. [Google Scholar] [CrossRef] [PubMed]
- Thompson, M.G.; Natarajan, K.; Irving, S.A.; Rowley, E.A.; Griggs, E.P.; Gaglani, M.; Klein, N.P.; Grannis, S.J.; DeSilvA, M.B.; Stenehjem, E.; et al. Effectiveness of a third dose of mRNA vaccines against COVID-19-associated emergency department and urgent care encounters and hospitalizations among adults during periods of Delta and Omicron variant predominance—VISION Network, 10 States, August 2021–January 2022. MMWR Morb. Mortal. Wkly. Rep. 2022, 71, 139–145. [Google Scholar]
- World Health Organization. Ten Health Issues WHO Will Tackle This Year. Available online: https://who.int/news-room/spotlight/ten-threats-to-global-health-in-2019 (accessed on 17 March 2021).
- MacDonald, N.E.; The SAGE Working Group on Vaccine Hesitancy. Vaccine hesitancy: Definition, scope and determinants. Vaccine 2015, 33, 4161–4416. [Google Scholar] [CrossRef]
- Centers for Disease Control and Prevention. Variants of the Virus. Available online: https://cdc.gov/coronavirus/2019-ncov/variants/index.html (accessed on 26 June 2023).
- Elliott, L.; Yan, K. Vaccine acceptance and hesitancy among college students in Nevada: A state-wide cross-sectional study. Vaccines 2022, 10, 105. [Google Scholar] [CrossRef]
- Synnott, C.K. College students COVID-19 vaccine hesitancy. SSRN Electron. J. 2020, 36, 152–159. [Google Scholar] [CrossRef]
- Wotring, A.J.; Hutchins, M.; Johnson, M.K.; Ferng, S.F.; Strawser, C.; Pfrank, H.; Warner, M.; Behrendt, L. COVID-19 vaccine uptake among college students at a Midwest university. J. Community Health. 2022, 47, 292–297. [Google Scholar] [CrossRef] [PubMed]
- Troiano, G.; Nardi, A. Vaccine hesitancy in the era of COVID-19. Public Health 2021, 194, 245–251. [Google Scholar] [CrossRef] [PubMed]
- Kaim, A.; Siman-Tov, M.; Jaffe, E.; Adini, B. Effect of a Concise Educational Program on COVID-19 Vaccination Attitudes. Front. Public Health 2021, 9, 767447. [Google Scholar] [CrossRef] [PubMed]
- Takagi, M.A.; Hess, S.; Smith, Z.; Gawronski, K.; Kumar, A.; Horsley, J.; Haddad, N.; Noveloso, B.; Zyzanski, S.; Ragina, N. The impact of educational interventions on COVID-19 and vaccination attitudes among patients in Michigan: A prospective study. Front. Public Health 2023, 11, 1144659. [Google Scholar] [CrossRef]
- Gurley, S.; Bennett, B.; Sullivan, P.S.; Kiley, M.; Linde, J.; Szczerbacki, D.; Guest, J. COVID-19 Vaccine perceptions, intentions, and uptake among young adults in the United States: Prospective college-based cohort study. JMIR Public Health Surveill. 2021, 79, e33739. [Google Scholar] [CrossRef] [PubMed]
- Brownstein, N.C.; Reddy, H.; Whiting, J.; Kasting, M.L.; Head, K.J.; Vadaparampil, S.T.; Giuliano, A.R.; Gwede, C.K.; Meade, C.D.; Christy, S.M. COVID-19 vaccine behaviors and intentions among a national sample of United States adults ages 18–45. Prev. Med. 2022, 160, 107038. [Google Scholar] [CrossRef]
- Centers for Disease Control and Prevention. COVID Data Tracker. Available online: https://covid.cdc.gov/covid-data-tracker/#new-hospital-admissions (accessed on 24 April 2023).
- Khairat, S.; Zou, B.; Adler-Milstein, J. Factors and reasons associated with low COVID-19 vaccine uptake among highly hesitant communities in the US. Am. J. Infect. Control 2022, 59, 262–267. [Google Scholar] [CrossRef] [PubMed]
- Jaffe, A.E.; Graupensperger, S.; Blayney, J.A.; Duckworth, J.C.; Stappenbeck, C.A. The role of perceived social norms in college student vaccine hesitancy: Implications for COVID-19 prevention strategies. Vaccine 2022, 40, 1888–1895. [Google Scholar] [CrossRef]
- Jensen, U.T.; Ayers, S.; Koshan, A.M. Video-based messages to reduce COVID-19 vaccine hesitancy and nudge vaccination intentions. PLoS ONE 2022, 17, e0265736. [Google Scholar] [CrossRef]
- Krouse, H.J. Video modelling to educate patients. J. Adv. Nurs. 2001, 33, 748–757. [Google Scholar] [CrossRef]
- Denny, M.C.; Vahidy, F.; Vu, K.Y.T.; Sharrief, A.Z.; Savitz, S.I. Video-based educational intervention associated with improved stroke literacy, self-efficacy, and patient satisfaction. PLoS ONE 2017, 12, e0171952. [Google Scholar] [CrossRef]
- Armstrong, A.W.; Idriss, N.Z.; Kim, R.H. Effects of video-based, online education on behavioral and knowledge outcomes in sunscreen use: A randomized controlled trial. Patient Educ. Couns. 2011, 83, 273–277. [Google Scholar] [CrossRef]
- Tam, J.W.; Schmitter-Edgecombe, M. A caregiver educational program: A video program to promote aging services technologies awareness. Geriatr. Nurs. 2019, 40, 78–83. [Google Scholar] [CrossRef] [PubMed]
- Kaim, A.; Siman-Tov, M.; Jaffe, E. Factors that enhance or impede compliance of the public with governmental regulation of lockdown during COVID-19 in Israel. Int. J. Disaster Risk Reduct. 2021, 66, 102596. [Google Scholar] [CrossRef] [PubMed]
- Faul, F.; Erdfelder, E.; Lang, A.G.; Buchner, A. G*Power 3: A flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav. Res. Methods 2007, 39, 175–191. [Google Scholar] [CrossRef]
- Norman, G. Likert scales, levels of measurement and the “laws” of statistics. Adv. Health Sci. Educ. Theory Pract. 2010, 15, 625–632. [Google Scholar] [CrossRef] [PubMed]
- Sullivan, G.M.; Artino, A.R. Analyzing and Interpreting Data From Likert-Type Scales. J. Grad. Med. Educ. 2013, 5, 541–542. [Google Scholar] [CrossRef]
- World Health Organization. WHO Coronavirus (COVID-19) Dashboard. Available online: https://covid19.who.int (accessed on 12 June 2022).
- Statista. Coronavirus Cases Worldwide by Country. Available online: https://statista.com/statistics/1043366/novel-coronavirus-2019ncov-cases-worldwide-by-country/ (accessed on 12 June 2022).
- Barnawi, N.A.; Alraqei, M.; Hilwan, A.; Al-Otibi, M.; Alsubaie, R.; Altowymy, S.; Abolfotouh, M.A. Impact of a Video-Based Edu-cational Intervention on the Levels of Knowledge and Concerns about COVID-19 Vaccination. Vaccines 2023, 11, 727. [Google Scholar] [CrossRef]
- Gatwood, J.; McKnight, M.; Fiscus, M.; Hohmeier, K.C.; Chisholm-Burns, M. Factors influencing likelihood of COVID-19 vaccination: A survey of Tennessee adults. Am. J. Health Syst. Pharm. 2021, 78, 879–889. [Google Scholar] [CrossRef]
- Dong, L.; Bogart, L.M.; Gandhi, P.; Aboagye, J.B.; Ryan, S.; Serwanga, R.; Ojikutu, B.O. A qualitative study of COVID-19 vaccine intentions and mistrust in Black Americans: Recommendations for vaccine dissemination and uptake. PLoS ONE 2022, 17, e0268020. [Google Scholar] [CrossRef]
- Dhanani, L.Y.; Franz, B. A meta-analysis of COVID-19 vaccine attitudes and demographic characteristics in the United States. Public Health 2022, 207, 31–38. [Google Scholar] [CrossRef]
- Lennon, R.P.; Block, R., Jr.; Schneider, E.C.; Zephrin, L.; Shah, A.; African American Research Collaborative 2021 COVID Group. Underserved population acceptance of combination influenza-COVID-19 booster vaccines. Vaccine 2022, 40, 562–567. [Google Scholar] [CrossRef]

| Demographics | Number of Participants (%) |
|---|---|
| Gender | |
| Female | 117 (41.1%) |
| Male | 167 (58.6%) |
| Non-binary gender | 1 (0.4%) |
| Age | |
| 18–21 | 76 (26.7%) |
| 22–23 | 86 (30.2%) |
| 24–25 | 63 (22.1%) |
| >25 | 60 (21.1%) |
| Race | |
| White/Caucasian | 99 (34.7%) |
| Hispanic/Latino | 93 (32.6%) |
| African American/Black | 36 (12.6%) |
| Indigenous American | 36 (12.6%) |
| Asian | 17 (6.0%) |
| Pacific Islander | 0 (0%) |
| Other/No response | 4 (1.4%) |
| Political Affiliation | |
| Republican | 118 (41.4%) |
| Democrat | 110 (38.6%) |
| Other/No response | 57 (2.0%) |
| Major | |
| Engineering and Sciences | 129 (45.3%) |
| Social Sciences | 107 (37.5%) |
| Visual and Performing Arts | 25 (8.8%) |
| Health Sciences | 14 (4.9%) |
| Other/No response | 10 (3.5%) |
| Number of influenza vaccines received in the last 5 years | |
| 0 | 35 (12.3%) |
| 1 | 42 (14.7%) |
| 2 | 91 (31.9%) |
| 3 | 58 (20.4%) |
| 4 | 18 (6.3%) |
| 5 | 31 (10.9%) |
| Other/No response | 10 (3.5%) |
| Before Watching the Video | After Watching the Video | p-Value | ||
|---|---|---|---|---|
| Knowledge of the side effects of COVID-19 infection | Strongly agree or agree | 118 (41.4%) | 188 (66.0%) | |
| Neither agree nor disagree | 84 (29.5%) | 66 (23.2%) | ||
| Strongly disagree or disagree | 83 (29.1%) | 31 (10.9%) | ||
| Mean ± SD of Likert Scores | 3.12 ± 1.18 | 3.76 ± 1.03 | <0.001 | |
| Willingness to receive a COVID-19 vaccine | Strongly agree or agree | 191 (67.0%) | 216 (75.7%) | |
| Neither agree nor disagree | 56 (19.6%) | 48 (16.8%) | ||
| Strongly disagree or disagree | 38 (13.4%) | 21 (7.5%) | ||
| Mean ± SD of Likert Scores | 3.70 ± 1.12 | 4.02 ± 0.99 | <0.001 | |
| Belief in the benefits of vaccinations | Strongly agree or agree | 177 (62.1%) | 216 (75.8%) | |
| Neither agree nor disagree | 65 (22.8%) | 48 (16.8%) | ||
| Strongly disagree or disagree | 43 (15.1%) | 21 (7.4%) | ||
| Mean ± SD of Likert Scores | 3.71 ± 1.08 | 4.02 ± 0.92 | <0.001 | |
| Awareness of risks of contracting COVID-19 | Strongly agree or agree | 162 (56.8%) | 178 (62.4%) | |
| Neither agree nor disagree | 59 (20.7%) | 61 (21.4%) | ||
| Strongly disagree or disagree | 64 (22.4%) | 46 (16.2%) | ||
| Mean ± SD of Likert Scores | 3.45 ± 1.18 | 3.66 ± 1.10 | <0.001 | |
| Fear of potential side effects from the COVID-19 vaccine(s) | Strongly agree or agree | 121 (42.5%) | 148 (51.9%) | |
| Neither agree nor disagree | 75 (26.3%) | 78 (27.4%) | ||
| Strongly disagree or disagree | 89 (31.2%) | 59 (20.7%) | ||
| Mean ± SD of Likert Scores | 3.10 ± 1.20 | 3.39 ± 1.09 | <0.001 | |
| Belief that COVID-19 vaccine(s) will prevent infection | Strongly agree or agree | 157 (55.1%) | 169 (59.3%) | |
| Neither agree nor disagree | 76 (26.7%) | 82 (28.8%) | ||
| Strongly disagree or disagree | 52 (18.2%) | 34 (11.9%) | ||
| Mean ± SD of Likert Scores | 3.49 ± 1.07 | 3.62 ± 1.03 | <0.001 | |
| Total Perception Score | Mean ± SD of Likert Scores | 20.37 ± 3.75 | 21.69 ± 3.24 | <0.001 |
| Total Perception Scores before Viewing Video | Total Perception Scores after Viewing Video | Video Influence Scores | |
|---|---|---|---|
| Total | 20.37 ± 3.75 | 21.69 ± 3.24 | 1.32 ± 3.72 |
| Race | |||
| White/Caucasian | 19.91 ± 4.04 A | 21.82 ± 3.26 | 1.91 ± 3.75 D |
| Hispanic/Latino | 20.86 ± 3.05 B | 21.03 ± 2.87 | 0.17 ± 3.67 D,E |
| African American/Black | 18.61 ± 3.89 B,C | 22.42 ± 3.51 | 3.81 ± 4.24 E,F,G |
| Indigenous American | 20.5 ± 3.57 | 21.14 ± 3.14 | 0.64 ± 2.52 F |
| Asian | 23.06 ± 3.77 A,C | 23.35 ± 3.90 | 0.29 ± 1.53 G |
| Major | |||
| Health Sciences | 20.86 ± 3.48 | 22.14 ± 2.21 | 1.29 ± 4.80 |
| Engineering and Sciences | 20.28 ± 3.98 | 21.92 ± 3.34 | 1.64 ± 4.00 |
| Social Sciences | 19.93 ± 3.62 | 21.14 ± 3.16 | 1.21 ± 3.65 |
| Visual and Performing Arts | 20.76 ± 2.39 | 21.12 ± 2.70 | 0.36 ± 2.22 |
| Gender | |||
| Male | 20.01 ± 3.63 | 21.27 ± 3.08 H | 1.26 ± 3.48 |
| Female | 20.83 ± 3.85 | 22.25 ± 3.38 H | 1.42 ± 4.07 |
| Political affiliation | |||
| Republican | 20.32 ± 2.89 I | 20.91 ± 3.22 J | 0.58 ± 2.72 |
| Democrat | 21.51 ± 3.56 I | 22.3 ± 3.47 J | 0.79 ± 3.53 |
| Strongly Agree or Agree | Neither Agree Nor Disagree | Strongly Disagree or Disagree | Mean ± SD of Likert Scores | |
|---|---|---|---|---|
| To protect the people around me and stop the spread of COVID-19 infection | 230 (80.7%) | 36 (12.6%) | 19 (6.7%) | 4.91 ± 0.93 |
| To protect oneself from getting a COVID-19 infection and its complications | 207 (72.3%) | 53 (18.6%) | 26 (9.1%) | 3.90 ± 0.97 |
| To shorten the duration of the COVID-19 pandemic | 191 (67.0%) | 66 (23.2%) | 28 (9.9%) | 3.91 ± 1.05 |
| My school requires that I obtain the COVID-19 vaccine | 162 (56.9%) | 61 (21.4%) | 62 (21.7%) | 3.50 ± 0.93 |
| To gather indoors with other people without masks | 139 (48.8%) | 64 (22.5%) | 82 (28.7%) | 3.16 ± 1.28 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lee, A.J.; Vu, T.T.; Sanz, R.M.; Kim, M.-K. Impacts of a COVID-19 Educational Video: Evaluation of the Influence of Race, Gender, Political Affiliation, Study Major, and Age on Vaccine Acceptance among University Students. Eur. J. Investig. Health Psychol. Educ. 2023, 13, 1738-1750. https://doi.org/10.3390/ejihpe13090126
Lee AJ, Vu TT, Sanz RM, Kim M-K. Impacts of a COVID-19 Educational Video: Evaluation of the Influence of Race, Gender, Political Affiliation, Study Major, and Age on Vaccine Acceptance among University Students. European Journal of Investigation in Health, Psychology and Education. 2023; 13(9):1738-1750. https://doi.org/10.3390/ejihpe13090126
Chicago/Turabian StyleLee, Audrey J., Tiffany T. Vu, Reina Marie Sanz, and Myo-Kyoung Kim. 2023. "Impacts of a COVID-19 Educational Video: Evaluation of the Influence of Race, Gender, Political Affiliation, Study Major, and Age on Vaccine Acceptance among University Students" European Journal of Investigation in Health, Psychology and Education 13, no. 9: 1738-1750. https://doi.org/10.3390/ejihpe13090126
APA StyleLee, A. J., Vu, T. T., Sanz, R. M., & Kim, M.-K. (2023). Impacts of a COVID-19 Educational Video: Evaluation of the Influence of Race, Gender, Political Affiliation, Study Major, and Age on Vaccine Acceptance among University Students. European Journal of Investigation in Health, Psychology and Education, 13(9), 1738-1750. https://doi.org/10.3390/ejihpe13090126









