A Prospective Study of the Family Quality of Life, Illness Perceptions, and Coping in Mothers of Children Newly Diagnosed with Autism Spectrum Disorder and Communication Difficulties
Abstract
1. Introduction
1.1. ASD’s Impact on Family (Pozo et al., 2011) [5]
1.2. Parents’ Perceptions about ASD and Coping Strategies
1.3. Purpose of the Study
2. Materials and Methods
2.1. Participants
2.2. Instruments
- The Beach Center Family Quality of Life Scale (FQoL)
- 2.
- The Brief Illness Perception Questionnaire (Brief IPQ)
- 3.
- The Brief-COPE inventory
2.3. Statistical Analysis
3. Results
3.1. Characteristics of the Sample
3.2. Descriptive Statistics of the Instruments
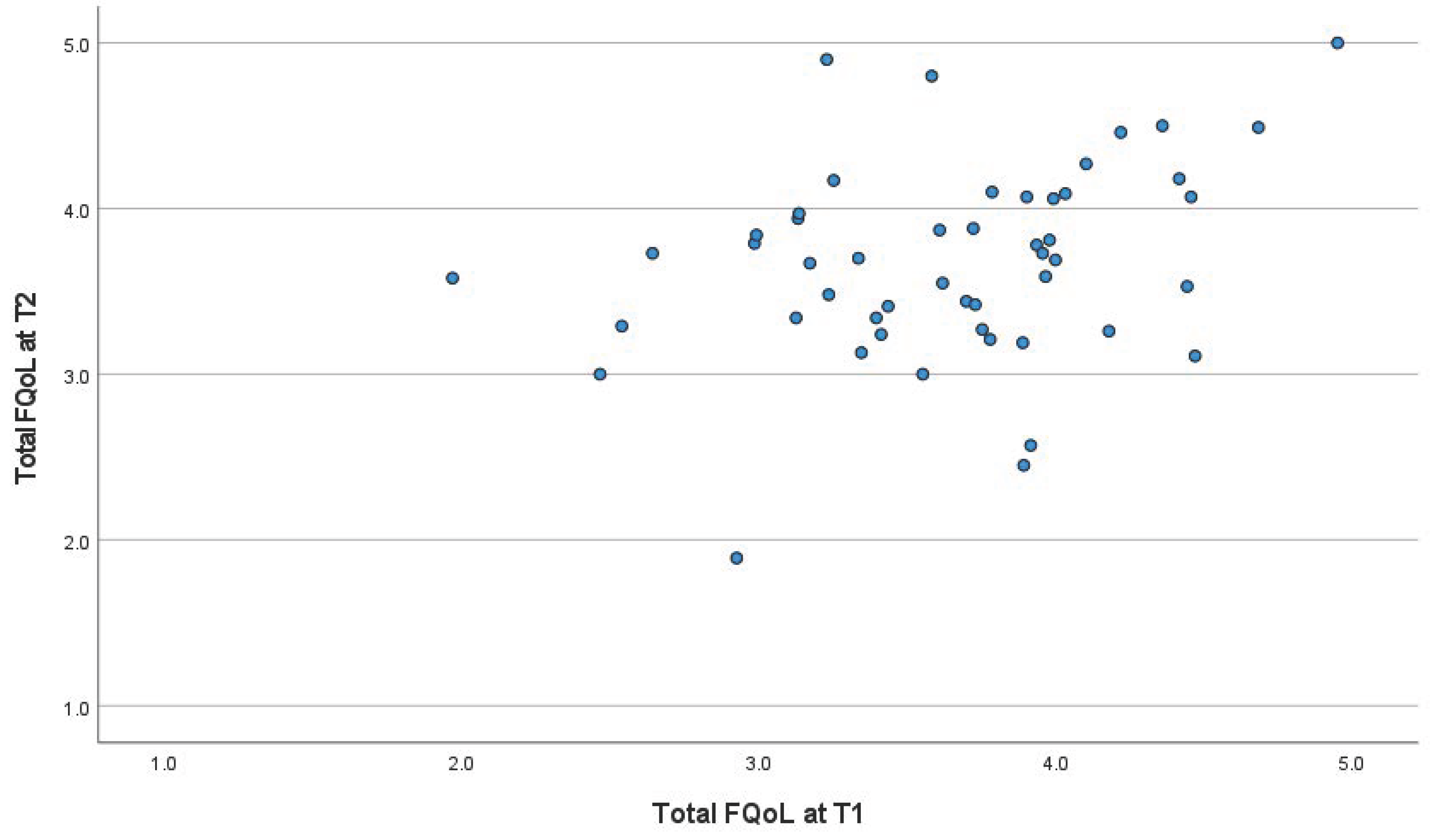
3.3. Correlations of the Family Quality of Life
3.4. Multiple Regression Analysis
4. Discussion
Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A
| Demographic Characteristics of the Families of Children with Autism Spectrum Disorder (ASD) (N = 53) | |
| Mothers’ age (years) Mean ± SD (range) | 39.08 ± 4.43 (31–49) |
| Mothers’ age groups | |
| 30–39 (N, %) | 30 (56.6) |
| 40–49 (N, %) | 23 (43.4) |
| Marital status (N, %) | |
| Married | 42 (79.2) |
| Divorced | 9 (17) |
| Unmarried | 2 (3.8) |
| Mother’s educational level (N, %) | |
| Gymnasium school (preparatory high school) | 2 (3.8) |
| High school | 26 (49.1) |
| University degree | 25 (47.2) |
| Mother’s profession (N, %) | |
| Economically inactive | 21 (39.6) |
| Farmer | 3 (5.7) |
| Private employee | 14 (26.4) |
| Civil servant | 13 (24.5) |
| Freelancer | 2 (3.8) |
| Relevant family medical history (N, %) | |
| Developmental disorder | 12 (22.6) |
| Mental disorders | 10 (18.9) |
| Neurological disorder | 1 (1.9) |
| None | 30 (56.6) |
| Monthly family income (euro) | |
| 0–400 | 6 (11.3) |
| 401–800 | 15 (28.3) |
| 801–1500 | 16 (30.2) |
| 1501–2500 | 10 (18.9) |
| 2500+ | 6 (11.3) |
| SD: standard deviation. | |
References
- Shu, B.C. Quality of life of family caregivers of children with autism: The mother’s perspective. Autism 2009, 13, 81–91. [Google Scholar] [CrossRef] [PubMed]
- Papadopoulos, D. Mothers’ experiences and challenges raising a child with autism spectrum disorder: A qualitative study. Brain Sci. 2021, 11, 309. [Google Scholar] [CrossRef] [PubMed]
- Rivard, M.; Morin, D.; Coulombe, P.; Morin, M.; Mello, C. The Diagnostic Period for Autism: Risk and Protective Factors for Family Quality of Life in Early Childhood. J. Autism Dev. Disord. 2022, 53, 3755–3769. [Google Scholar] [CrossRef] [PubMed]
- Mello, C.; Rivard, M.; Morin, D.; Patel, S.; Morin, M. Symptom Severity, Internalized and Externalized Behavioral and Emotional Problems: Links with Parenting Stress in Mothers of Children Recently Diagnosed with Autism. J. Autism Dev. Disord. 2022, 52, 2400–2413. [Google Scholar] [CrossRef] [PubMed]
- Pozo, P.; Sarriá, E.; Brioso, Á. Psychological adaptation in parents of children with autism spectrum disorders. In A Comprehensive Book on Autism Spectrum Disorders; IntechOpen: London, UK, 2011; Volume 6, pp. 107–130. [Google Scholar]
- Kasari, C.; Brady, N.; Lord, C.; Tager-Flusberg, H. Assessing the minimally verbal school-aged child with autism spectrum disorder. Autism Res. 2013, 6, 479–493. [Google Scholar] [CrossRef] [PubMed]
- Tager-Flusberg, H.; Kasari, C. Minimally verbal school-aged children with autism spectrum disorder: The neglected end of the spectrum. Autism Res. 2013, 6, 468–478. [Google Scholar] [CrossRef]
- Vasilopoulou, E.; Nisbet, J. The quality of life of parents of children with autism spectrum disorder: A systematic review. Res. Autism Spectr. Disord. 2016, 23, 36–49. [Google Scholar] [CrossRef]
- Dardas, L.A.; Ahmad, M.M. Quality of life among parents of children with autistic disorder: A sample from the Arab world. Res. Dev. Disabil. 2014, 35, 278–287. [Google Scholar] [CrossRef] [PubMed]
- McStay, R.L.; Trembath, D.; Dissanayake, C. Stress and Family Quality of Life in Parents of Children with Autism Spectrum Disorder: Parent Gender and the Double ABCX Model. J. Autism Dev. Disord. 2014, 44, 3101–3118. [Google Scholar] [CrossRef] [PubMed]
- Eapen, V.; Črnčec, R.; Walter, A.; Tay, K.P. Conceptualisation and Development of a Quality of Life Measure for Parents of Children with Autism Spectrum Disorder. Autism Res. Treat. 2014, 2014, 160783. [Google Scholar] [CrossRef]
- Papadopoulos, A.; Tafiadis, D.; Tsapara, A.; Skapinakis, P.; Tzoufi, M.; Siafaka, V. Validation of the Greek version of the Affiliate Stigma Scale among mothers of children with autism spectrum disorder. BJPsych Open. 2022, 8, e30. [Google Scholar] [CrossRef]
- Reed, P.; Osborne, L.A. Reaction to diagnosis and subsequent health in mothers of children with autism spectrum disorder. Autism 2019, 23, 1442–1448. [Google Scholar] [CrossRef] [PubMed]
- Smith, S.; Tallon, M.; Clark, C.; Jones, L.; Mörelius, E. You Never Exhale Fully Because You’re Not Sure What’s NEXT: Parents’ experiences of stress caring for children with chronic conditions. Front. Pediatr. 2022, 10, 902655. [Google Scholar] [CrossRef] [PubMed]
- Picardi, A.; Gigantesco, A.; Tarolla, E.; Stoppioni, V.; Cerbo, R.; Cremonte, M.; Alessandri, G.; Lega, I.; Nardocci, F. Parental burden and its correlates in families of children with autism spectrum disorder: A multicentre study with two comparison groups. Clin. Pract. Epidemiol. Ment. Health 2018, 14, 143. [Google Scholar] [CrossRef] [PubMed]
- Karst, J.S.; Van Hecke, A.V. Parent and family impact of autism spectrum disorders: A review and proposed model for intervention evaluation. Clin. Child. Fam. Psychol. Rev. 2012, 15, 247–277. [Google Scholar] [CrossRef] [PubMed]
- Ginieri-Coccossis, M.; Rotsika, V.; Skevington, S.; Papaevangelou, S.; Malliori, M.; Tomaras, V.; Kokkevi, A. Quality of life in newly diagnosed children with specific learning disabilities (SpLD) and differences from typically developing children: A study of child and parent reports. Child. Care Health Dev. 2013, 39, 581–591. [Google Scholar] [CrossRef] [PubMed]
- Papadopoulos, A.; Siafaka, V.; Tsapara, A.; Tafiadis, D.; Kotsis, K.; Skapinakis, P.; Tzoufi, M. Measuring parental stress, illness perceptions, coping and quality of life in families of children newly diagnosed with autism spectrum disorder. BJPsych Open 2023, 9, e84. [Google Scholar] [CrossRef] [PubMed]
- Pecor, K.W.; Barbayannis, G.; Yang, M.; Johnson, J.; Materasso, S.; Borda, M.; Garcia, D.; Garla, V.; Ming, X. Quality of life changes during the covid-19 pandemic for caregivers of children with adhd and/or asd. Int. J. Environ. Res. Public Health 2021, 18, 3667. [Google Scholar] [CrossRef] [PubMed]
- Suma, K.; Adamson, L.B.; Bakeman, R.; Robins, D.L.; Abrams, D.N. After Early Autism Diagnosis: Changes in Intervention and Parent–Child Interaction. J. Autism Dev. Disord. 2016, 46, 2720–2733. [Google Scholar] [CrossRef] [PubMed]
- Kent, R.G.; Carrington, S.J.; Le Couteur, A.; Gould, J.; Wing, L.; Maljaars, J.; Noens, I.; van Berckelaer-Onnes, I.; Leekam, S.R. Diagnosing autism spectrum disorder: Who will get a DSM-5 diagnosis? J. Child Psychol. Psychiatry 2013, 54, 1242–1250. [Google Scholar] [CrossRef] [PubMed]
- Crane, L.; Chester, J.W.; Goddard, L.; Henry, L.A.; Hill, E. Experiences of Autism Diagnosis: A Survey of over 1000 parents in the United Kingdom. Autism 2016, 20, 153–162. [Google Scholar] [CrossRef] [PubMed]
- Vernhet, C.; Michelon, C.; Dellapiazza, F.; Rattaz, C.; Geoffray, M.M.; Roeyers, H.; Picot, M.-C.; Baghdadli, A.; ELENA Study Group. Perceptions of parents of the impact of autism spectrum disorder on their quality of life and correlates: Comparison between mothers and fathers. Qual. Life Res. 2022, 31, 1499–1508. [Google Scholar] [CrossRef] [PubMed]
- Al Anbar, N.N.; Dardennes, R.M.; Prado-Netto, A.; Kaye, K.; Contejean, Y. Treatment choices in autism spectrum disorder: The role of parental illness perceptions. Res. Dev. Disabil. 2010, 31, 817–828. [Google Scholar] [CrossRef] [PubMed]
- Diefenbach, M.A.; Leventhal, H. The Common-Sense Model of Illness Representation: Theoretical and Practical Considerations. J. Social. Distress Homelessness 1996, 5, 11–38. [Google Scholar] [CrossRef]
- Leventhal, H. Findings and Theory in the Study of Fear Communications; Academic Press: New York, NY, USA, 1970; Volume 5. [Google Scholar]
- Karademas, E.C.; Karamvakalis, N.; Zarogiannos, A. Life context and the experience of chronic illness: Is the stress of life associated with illness perceptions and coping? Stress. Health 2009, 25, 405–412. [Google Scholar] [CrossRef]
- Leventhal, H.; Leventhal, E.A.; Cameron, L. Representations, procedures, and affect in illness self-regulation: A perceptual-cognitive model. In Handbook of Health Psychology; Baum, A., Revenson, T.A., Singer, J.E., Eds.; Lawrence Erlbaum: Mahwah, NJ, USA, 2001; Volume 3, pp. 19–48. [Google Scholar]
- Mire, S.S.; Gealy, W.; Kubiszyn, T.; Burridge, A.B.; Goin-Kochel, R.P. Parent Perceptions About Autism Spectrum Disorder Influence Treatment Choices. Focus. Autism Other Dev. Disabl. 2017, 32, 305–318. [Google Scholar] [CrossRef]
- Dos Anjos, B.B.; De Morais, N.A. Experiences of Families with Autistic Children: An Integrative Literature Review; Ciencias Psicologicas: Montevideo, Uruguay, 2021; Volume 15. [Google Scholar]
- Essex, E.L.; Seltzer, M.M.; Krauss, M.W. Differences in coping effectiveness and well-being among aging mothers and fathers of adults with mental retardation. Am. J. Ment. Retard. 1999, 104, 545–563. [Google Scholar] [CrossRef] [PubMed]
- Lazarus, R.S. The Role of Coping in the Emotions and How Coping Changes over the Life Course. In Handbook of Emotion, Adult Development, and Aging; Elsevier: Amsterdam, The Netherlands, 1996; pp. 289–306. [Google Scholar]
- Lazarus, R.S.; Folkman, S. Stress, Appraisal, and Coping; Springer Publishing Company: Berlin/Heidelberg, Germany, 1984. [Google Scholar]
- Lazarus, R.S. Further Annual Reviews from Psychological Stress to the Emotions: A History of Changing Outlooks. 1993. Available online: www.annualreviews.org (accessed on 1 April 2023).
- Pepperell, T.A.; Paynter, J.; Gilmore, L. Social support and coping strategies of parents raising a child with autism spectrum disorder. Early Child Dev. Care 2018, 188, 1392–1404. [Google Scholar] [CrossRef]
- Lutz, H.R.; Patterson, B.J.; Klein, J. Coping with autism: A journey toward adaptation. J. Pediatr. Nurs. 2012, 27, 206–213. [Google Scholar] [CrossRef] [PubMed]
- O’Nions, E.; Happé, F.; Evers, K.; Boonen, H.; Noens, I. How do Parents Manage Irritability, Challenging Behaviour, Non-Compliance and Anxiety in Children with Autism Spectrum Disorders? A Meta-Synthesis. J. Autism Dev. Disord. 2018, 48, 1272–1286. [Google Scholar] [CrossRef] [PubMed]
- Tarakeshwar, N.; Pargament, K.I. Religious Coping in Families of Children with Autism. Focus. Autism Other Dev. Disabl. 2001, 16, 247–260. [Google Scholar] [CrossRef]
- Lin, C.R.; Tsai, Y.F.; Chang, H.L. Coping mechanisms of parents of children recently diagnosed with autism in Taiwan: A qualitative study. J. Clin. Nurs. 2008, 17, 2733–2740. [Google Scholar] [CrossRef] [PubMed]
- Navot, N.; Jorgenson, A.G.; Vander Stoep, A.; Toth, K.; Webb, S.J. Family planning and family vision in mothers after diagnosis of a child with autism spectrum disorder. Autism 2016, 20, 605–615. [Google Scholar] [CrossRef] [PubMed]
- Feng, Y.; Zhou, X.; Qin, X.; Cai, G.; Lin, Y.; Pang, Y.; Chen, B.; Deng, T.; Zhang, L. Parental self-efficacy and family quality of life in parents of children with autism spectrum disorder in China: The possible mediating role of social support. J. Pediatr. Nurs. 2022, 63, 159–167. [Google Scholar] [CrossRef] [PubMed]
- Wang, H.; Hu, X.; Han, Z.R. Parental stress, involvement, and family quality of life in mothers and fathers of children with autism spectrum disorder in mainland China: A dyadic analysis. Res. Dev. Disabil. 2020, 107, 103791. [Google Scholar] [CrossRef] [PubMed]
- Dai, Y.; Chen, M.; Deng, T.; Huang, B.; Ji, Y.; Feng, Y.; Liu, S.; Zhang, L. The importance of parenting self-efficacy and social support for family quality of life in children newly diagnosed with autism spectrum disorder: A one-year follow-up study. Autism Res. 2023, 17, 148–161. [Google Scholar] [CrossRef] [PubMed]
- Hoffman, L.; Marquis, J.; Poston, D.; Summers, J.A.; Turnbull, A. Assessing family outcomes: Psychometric evaluation of the beach center family quality of life scale. J. Marriage Fam. 2006, 68, 1069–1083. [Google Scholar] [CrossRef]
- Hoffman, C.; Rice, D.; Sung, H.Y. Persons with chronic conditions: Their prevalence and costs. J. Am. Med. Assoc. 1996, 276, 1473–1479. [Google Scholar] [CrossRef]
- Samuel, P.S.; Rillotta, F.; Brown, I. Review: The development of family quality of life concepts and measures. J. Intellect. Disabil. Res. 2012, 56, 1–16. [Google Scholar] [CrossRef] [PubMed]
- Mello, C.; Rivard, M.; Terroux, A.; Mercier, C. Quality of life in families of young children with autism spectrum disorder. Am. J. Intellect. Dev. Disabil. 2019, 124, 535–548. [Google Scholar] [CrossRef] [PubMed]
- Parpa, E.; Katsantonis, N.; Tsilika, E.; Galanos, A.; Sassari, M.; Mystakidou, K. Psychometric Properties of the Family Quality of Life Scale in Greek Families with Intellectual Disabilities. J. Dev. Phys. Disabil. 2016, 28, 393–405. [Google Scholar] [CrossRef]
- Broadbent, E.; Petrie, K.J.; Main, J.; Weinman, J. The Brief Illness Perception Questionnaire. J. Psychosom. Res. 2006, 60, 631–637. [Google Scholar] [CrossRef] [PubMed]
- Charles, S. Carver. You want to measure coping but your protocol’s too long: Consider the brief COPE. Int. J. Behav. Med. 1997, 4, 92–100. [Google Scholar]
- Kapsou, M.; Panayiotou, G.; Kokkinos, C.M.; Demetriou, A.G. Dimensionality of coping: An empirical contribution to the construct validation of the Brief-COPE with a Greek-speaking sample. J. Health Psychol. 2010, 15, 215–229. [Google Scholar] [CrossRef]
- Mire, S.S.; Tolar, T.D.; Brewton, C.M.; Raff, N.S.; McKee, S.L. Validating the Revised Illness Perception Questionnaire as a Measure of Parent Perceptions of Autism Spectrum Disorder. J. Autism Dev. Disord. 2018, 48, 1761–1779. [Google Scholar] [CrossRef] [PubMed]
- Ntre, V.; Papanikolaou, K.; Triantafyllou, K.; Giannakopoulos, G.; Kokkosi, M.; Kolaitis, G. Psychosocial and Financial Needs, Burdens and Support, and Major Concerns among Greek Families with Children with Autism Spectrum Disorder (ASD). Int. J. Caring Sci. 2018, 11, 985–995. [Google Scholar]
- Pozo, P.; Sarriá, E. Prediction of stress in mothers of children with autism spectrum disorders. Span. J. Psychol. 2014, 17, E6. [Google Scholar] [CrossRef] [PubMed]
- Feinberg, E.; Augustyn, M.; Fitzgerald, E.; Sandler, J.; Suarez, Z.F.C.; Chen, N.; Cabral, H.; Beardslee, W.; Silverstein, M. Improving maternal mental health after a child’s diagnosis of autism spectrum disorder: Results from a randomized clinical trial. JAMA Pediatr. 2014, 168, 40–46. [Google Scholar] [CrossRef] [PubMed]
- Oprea, C.; Stan, A. Mothers of Autistic Children. How do They Feel? Procedia Soc. Behav. Sci. 2012, 46, 4191–4194. [Google Scholar] [CrossRef][Green Version]
- Gatzoyia, D.; Kotsis, K.; Koullourou, I.; Goulia, P.; Carvalho, A.F.; Soulis, S.; Hyphantis, T. The association of illness perceptions with depressive symptoms and general psychological distress in parents of an offspring with autism spectrum disorder. Disabil. Health J. 2014, 7, 173–180. [Google Scholar] [CrossRef] [PubMed]
- Baker, B.L.; Blacher, J.; Olsson, M.B. Preschool children with and without developmental delay: Behaviour problems, parents’ optimism and well-being. J. Intellect. Disabil. Res. 2005, 49, 575–590. [Google Scholar] [CrossRef] [PubMed]
- Da Paz, N.S.; Siegel, B.; Coccia, M.A.; Epel, E.S. Acceptance or Despair? Maternal Adjustment to Having a Child Diagnosed with Autism. J. Autism Dev. Disord. 2018, 48, 1971–1981. [Google Scholar] [CrossRef] [PubMed]
- Luong, J.; Yoder, M.K.; Canham, D. Southeast Asian parents raising a child with autism: A qualitative investigation of coping styles. J. Sch. Nurs. 2009, 25, 222–229. [Google Scholar] [CrossRef] [PubMed]
- Ho, K.M.; Keiley, M.K. Dealing with Denial: A Systems Approach for Family Professionals Working with Parents of Individuals with Multiple Disabilities. Fam. J. 2003, 11, 239–247. [Google Scholar] [CrossRef]
- Al-Kandari, S.; Alsalem, A.; Abohaimed, S.; Al-Orf, F.; Al-Zoubi, M.; Al-Sabah, R.; Shah, N. Brief Report: Social Support and Coping Strategies of Mothers of Children Suffering from ASD in Kuwait. J. Autism Dev. Disord. 2017, 47, 3311–3319. [Google Scholar] [CrossRef] [PubMed]
- Carlsson, E.; Miniscalco, C.; Kadesjö, B.; Laakso, K. Negotiating knowledge: Parents’ experience of the neuropsychiatric diagnostic process for children with autism. Int. J. Lang. Commun. Disord. 2016, 51, 328–338. [Google Scholar] [CrossRef] [PubMed]
- Twoy, R.; Connolly, P.M.; Novak, J.M. Coping strategies used by parents of children with autism. J. Am. Acad. Nurse Pract. 2007, 19, 251–260. [Google Scholar] [CrossRef] [PubMed]
- Poslawsky, I.E.; Naber, F.B.A.; Van Daalen, E.; Van Engeland, H. Parental reaction to early diagnosis of their children’s autism spectrum disorder: An exploratory study. Child. Psychiatry Hum. Dev. 2014, 45, 294–305. [Google Scholar] [CrossRef] [PubMed]
- Ekas, N.V.; Lickenbrock, D.M.; Whitman, T.L. Optimism, social support, and well-being in mothers of children with autism spectrum disorder. J. Autism Dev. Disord. 2010, 40, 1274–1284. [Google Scholar] [CrossRef] [PubMed]
- McAuliffe, T.; Cordier, R.; Vaz, S.; Thomas, Y.; Falkmer, T. Quality of Life, Coping Styles, Stress Levels, and Time Use in Mothers of Children with Autism Spectrum Disorders: Comparing Single Versus Coupled Households. J. Autism Dev. Disord. 2017, 47, 3189–3203. [Google Scholar] [CrossRef] [PubMed]
- Malhotra, S.; Khan, W.; Bhatia, M.S. Quality of Life of Parents having Children with Developmental Disabilities. Delhi Psychiatry J. 2012, 15, 171–176. [Google Scholar]
- Bonis, S.A.; Sawin, K.J. Risks and Protective Factors for Stress Self-Management in Parents of Children with Autism Spectrum Disorder: An Integrated Review of the Literature. J. Pediatr. Nurs. 2016, 31, 567–579. [Google Scholar] [CrossRef] [PubMed]
- Predescu Elena, Ş.R. Family Quality of Life in Autism Spectrum Disorders (ASD). In Autism—Paradigms, Recent Research and Clinical Applications; Fitzgerald, M., Yip, J., Eds.; IntechOpen: London, UK, 2017; Available online: https://www.intechopen.com/books/autism-paradigms-recent-research-and-clinical-applications/family-quality-of-life-in-autism-spectrum-disorders-asd- (accessed on 1 April 2023).
- Reed, P.; Picton, L.; Grainger, N.; Osborne, L.A. Impact of diagnostic practices on the self-reported health of mothers of recently diagnosed children with ASD. Int. J. Environ. Res. Public Health 2016, 13, 888. [Google Scholar] [CrossRef] [PubMed]
- Pisula, E.; Porębowicz-Dörsmann, A. Family functioning, parenting stress and quality of life in mothers and fathers of Polish children with high functioning autism or Asperger syndrome. PLoS ONE 2017, 12, e0186536. [Google Scholar] [CrossRef] [PubMed]
- Kuru, N.; Piyal, B. Perceived social support and quality of life of parents of children with Autism. Niger. J. Clin. Pract. 2018, 21, 1182–1189. [Google Scholar] [CrossRef] [PubMed]
- Hsiao, Y.J.; Higgins, K.; Pierce, T.; Whitby, P.J.S.; Tandy, R.D. Parental stress, family quality of life, and family-teacher partnerships: Families of children with autism spectrum disorder. Res. Dev. Disabil. 2017, 70, 152–162. [Google Scholar] [CrossRef] [PubMed]
- Calonge-Torres, M.; Reyes, A.L.; Avendaño, E.L.; Conducto, C.C.; Bautista, M.L. Quality of life of parents of children with autism spectrum disorder aged 3 to 18 years living in an urban area. Arch. Dis. Child. 2017, 102 (Suppl. S1), A197. [Google Scholar]
- Alenazi, D.; Hammad, S.; Mohamed, A. Effect of autism on parental quality of life in Arar city, Saudi Arabia. J. Fam. Community Med. 2020, 27, 15–22. [Google Scholar]
- Özgür, B.G.; Aksu, H.; Eser, E. Factors affecting quality of life of caregivers of children diagnosed with autism spectrum disorder. Indian. J. Psychiatry 2018, 60, 278–285. [Google Scholar] [CrossRef] [PubMed]
- Brown, R.I.; MacAdam–Crisp, J.; Wang, M.; Iarocci, G. Family Quality of Life When There Is a Child with a Developmental Disability. J. Policy Pract. Intellect. Disabil. 2006, 3, 238–245. [Google Scholar] [CrossRef]
- Veroni, E. Examing Services Available to Greek Parents of Children with Autism Spectrum Disorders (ASD). Camb. Open-Rev. Educ. Res. e-J. 2016, 3, 98–110. [Google Scholar]
- Piovesan, J.; Scortegagna, S.A.; De Marchi, A.C.B. Quality of Life and Depressive Symptomatology in Mothers of Individuals with Autism. Psico-USF 2015, 20, 505–515. [Google Scholar] [CrossRef]
- Lu, M.; Yang, G.; Skora, E.; Wang, G.; Cai, Y.; Sun, Q.; Li, W. Self-esteem, social support, and life satisfaction in Chinese parents of children with autism spectrum disorder. Res. Autism Spectr. Disord. 2015, 17, 70–77. [Google Scholar] [CrossRef]
- Harper, A.; Dyches, T.T.; Harper, J.; Roper, S.O.; South, M. Respite care, marital quality, and stress in parents of children with autism spectrum disorders. J. Autism Dev. Disord. 2013, 43, 2604–2616. [Google Scholar] [CrossRef] [PubMed]
- Nealy, C.E.; O’Hare, L.; Powers, J.D.; Swick, D.C. The impact of autism spectrum disorders on the family: A qualitative study of mothers’ perspectives. J. Fam. Soc. Work. 2012, 15, 187–201. [Google Scholar] [CrossRef]
- Saggu, R. Parental Perceptions of the Diagnostic Process for Autism Spectrum Disorder in British. Ph.D. Thesis, Walden University, Minneapolis, MN, USA, 2016. Dissertation Abstracts International: Section B: The Sciences and Engineering; Volume 76. Available online: http://ovidsp.ovid.com/ovidweb.cgi?T=JS&PAGE=reference&D=psyc13a&NEWS=N&AN=2016-16233-255 (accessed on 1 April 2023).
- Balubaid, R.; Sahab, L. The coping strategies used by parents of children with autism in Saudi Arabia. J. Educ. Pract. 2017, 8, 141–151. [Google Scholar]
- Al-Oran, H.; Khuan, L.; Ying, L.P.; Hassouneh, O. Coping Mechanism among Parents of Children with Autism Spectrum Disorder: A Review. Iran. J. Child. Neurol. 2022, 16, 9–17. [Google Scholar] [PubMed]
- Higgins, L.; Mannion, A.; Chen, J.L.; Leader, G. Adaptation of Parents Raising a Child with ASD: The Role of Positive Perceptions, Coping, Self-efficacy, and Social Support. J. Autism Dev. Disord. 2023, 53, 1224–1242. [Google Scholar] [CrossRef] [PubMed]
- Pozo, P.; Sarriá, E. Still stressed but feeling better: Well-being in autism spectrum disorder families as children become adults. Autism 2015, 19, 805–813. [Google Scholar] [CrossRef] [PubMed]
- Abd Latif, M.H.; Wan Ismail, W.S.; Abdul Manaf, M.R.; Abdul Taib, N.I. Factors Influencing Despair, Self-blame, and Acceptance Among Parents of Children with Autism Spectrum Disorder (ASD): A Malaysian Perspective. J. Autism Dev. Disord. 2023. [Google Scholar] [CrossRef] [PubMed]
- Eaton, K.; Ohan, J.L.; Stritzke, W.G.K.; Corrigan, P.W. Failing to Meet the Good Parent Ideal: Self-Stigma in Parents of Children with Mental Health Disorders. J. Child. Fam. Stud. 2016, 25, 3109–3123. [Google Scholar] [CrossRef]
- Manan, A.I.A.; Amit, N.; Said, Z.; Ahmad, M. The influences of parenting stress, children behavioral problems and children quality of life on depression symptoms among parents of children with autism: Preliminary findings. Malays. J. Health Sci. 2018, 16, 137–143. [Google Scholar]
- Paleari, F.; Compare, A.; Melli, S.; Zarbo, C.; Grossi, E. Self-blame, self-forgiveness and wellbeing among parents of autistic children. In Proceedings of the ECP 2015: 14th European Congress of Psychology “Linking Technology and Psychology: Feeding the Mind, Energy for Life”, Milan, Italy, 7–10 July 2015; p. 1693. [Google Scholar]
- Mira Coelho, A.; da Conceição, V. Predictors in ASD: The Importance of Parents’ Perception. Front. Psychiatry 2021, 12, 506148. [Google Scholar] [CrossRef] [PubMed]
- Sharma, N.; Chakrabarti, S.; Grover, S. Gender differences in caregiving among family—Caregivers of people with mental illnesses. World J. Psychiatry 2016, 6, 7. [Google Scholar] [CrossRef] [PubMed]
- Eapen, V.; Karlov, L.; John, J.R.; Beneytez, C.; Grimes, P.Z.; Kang, Y.Q.; Mardare, I.; Minca, D.G.; Voicu, L.; Abd Malek, K.; et al. Quality of life in parents of autistic children: A transcultural perspective. Front. Psychol. 2023, 14, 1022094. [Google Scholar] [CrossRef] [PubMed]
| FQoL—Τ1 | FQoL—Τ2 | p-Value | |||
|---|---|---|---|---|---|
| Mean | SD | Mean | SD | NS | |
| Family interaction | 3.85 | 0.75 | 3.89 | 0.70 | NS |
| Parenting | 3.68 | 0.66 | 3.80 | 0.62 | NS |
| Emotional well-being | 3.10 | 0.82 | 3.19 | 0.77 | NS |
| Physical/material well-being | 3.93 | 0.79 | 3.86 | 0.73 | NS |
| Disability-related support | 3.69 | 0.71 | 3.62 | 0.73 | NS |
| FQoL total score | 3.66 | 0.59 | 3.68 | 0.59 | NS |
| Brief IPQ—Τ1 | Brief IPQ—Τ2 | p Value | |||
|---|---|---|---|---|---|
| Mean | SD | Mean | SD | ||
| Consequences | 7.39 | 2.31 | 7.54 | 2.26 | NS |
| Timeline | 6.75 | 2.95 | 6.72 | 2.94 | NS |
| Personal Control | 6.56 | 2.24 | 6.70 | 2.23 | NS |
| Treatment Control | 7.96 | 1.74 | 7.94 | 1.75 | NS |
| Identity | 6.90 | 2.17 | 6.75 | 2.21 | NS |
| Illness Concern | 8.62 | 1.86 | 8.60 | 1.90 | NS |
| Coherence | 7.83 | 2.09 | 7.96 | 2.07 | NS |
| Emotional Representations | 8.60 | 1.74 | 8.54 | 1.77 | NS |
| Causes * (frequencies, %) | NS | ||||
| Emotional cause | 5 (9.4%) | 7 (13.5%) | |||
| Behavioral cause | 10 (18.9%) | 12 (23.1%) | |||
| Risk factors | 13 (24.5%) | 19 (36.5%) | |||
| External factors | 12 (22.6%) | 14 (26.9) | |||
| Τ1 | Τ2 | Paired Samples Test for Τ1 and Τ2 | |||
|---|---|---|---|---|---|
| Mean | SD | Mean | SD | ||
| Self-distraction | 5.01 | 1.42 | 5.02 | 1.53 | NS |
| Active coping | 5.92 | 1.66 | 6.06 | 1.36 | NS |
| Denial | 4.32 | 1.59 | 3.50 | 1.34 | t(49) = 2.86, p = 0.006 |
| Substance use | 2.03 | 0.27 | 2.16 | 0.58 | NS |
| Emotional support | 5.47 | 1.51 | 5.46 | 1.69 | NS |
| Informational support | 5.71 | 1.40 | 5.56 | 1.60 | NS |
| Behavioral disengagement | 3.07 | 1.45 | 2.76 | 1.15 | NS |
| Venting | 5.43 | 1.47 | 5.32 | 1.31 | NS |
| Positive reframing | 5.71 | 1.79 | 6.16 | 1.65 | NS |
| Planning | 6.67 | 1.35 | 6.66 | 1.22 | NS |
| Humor | 2.98 | 1.16 | 3.08 | 1.15 | NS |
| Acceptance | 6.50 | 1.38 | 6.76 | 1.33 | NS |
| Religion | 4.37 | 1.96 | 4.24 | 1.77 | NS |
| Self-blame | 5.54 | 1.90 | 4.60 | 1.67 | t(49) = 2.52, p = 0.015 |
| Family Quality of Life (FQoL) | ||||||
|---|---|---|---|---|---|---|
| Family Interaction | Parenting | Emotional Well-Being | Physical/Material Well-Being | Disability-Related Support | Total FQoL | |
| Gender of child a | NS | NS | NS | NS | NS | NS |
| Age of mother a | NS | NS | NS | 0.083 * | NS | NS |
| Education of mother a | NS | NS | NS | 0.134 * | NS | NS |
| Employment status of the mother a | NS | NS | NS | 0.190 * | NS | NS |
| Education of father a | NS | NS | NS | 0.227 ** | NS | NS |
| Marital statusa | 0.390 *** | 0.167 ** | 0.129 * | 0.238 ** | 0.268 *** | 0.353 *** |
| Family income a | 0.254 ** | 0.186 * | 0.261 ** | 0.684 *** | NS | 0.395 *** |
| Relevant family medical history a | NS | NS | NS | 0.279 ** | NS | NS |
| Attention deficit in children a | NS | NS | NS | NS | NS | NS |
| 2-word phrases time a | NS | NS | NS | NS | NS | NS |
| Severity b | NS | NS | NS | NS | NS | NS |
| Τ1 FQoL | ||||||
|---|---|---|---|---|---|---|
| Family Interaction | Parenting | Emotional Well-Being | Physical/Material Well-Being | Disability-Related Support | FQoL Total Score | |
| BRIEF IPQ | ||||||
| Consequences | −0.331 * | NS | −0.434 ** | −0.347 * | −0.474 *** | −0.467 *** |
| Timeline | NS | NS | NS | NS | −0.330 * | NS |
| Personal control | NS | NS | NS | NS | 0.328 * | NS |
| Treatment control | 0.419 ** | 0.643 *** | 0.450 ** | NS | 0.484 *** | 0.556 *** |
| Identity | NS | NS | NS | NS | NS | NS |
| Illness concern | −0.344 * | −0.344 * | −0.386 ** | −0.293 * | −0.410 ** | −0.442 ** |
| Coherence | NS | NS | 0.360 ** | NS | 0.328 * | 0.345 * |
| Emotional representations | −0.374 ** | −0.286 * | NS | NS | −0.288 * | −0.328 * |
| Causes | NS | NS | NS | NS | NS | NS |
| Τ2 FQoL | ||||||
| Consequences | NS | NS | NS | NS | −0.346 * | NS |
| Treatment control | 0.503 *** | 0.530 *** | 0.466 ** | NS | 0.490 *** | 0.516 *** |
| Τ1 FQoL | ||||||
|---|---|---|---|---|---|---|
| Family Interaction | Parenting | Emotional Well-Being | Physical/Material Well-Being | Disability-Related Support | FQoL Total Score | |
| BRIEF-COPE | ||||||
| Active coping | NS | NS | 0.305 * | NS | NS | NS |
| Denial | NS | −0.330 * | −0.298 * | NS | NS | −0.308 * |
| Substance use | NS | NS | 0.281 * | NS | NS | NS |
| Emotional support | NS | NS | 0.273 * | 0.366 ** | NS | 0.282 * |
| Informational support | NS | NS | 0.330 * | NS | NS | NS |
| Behavioral disengagement | NS | NS | NS | NS | −0.311 * | NS |
| Venting | NS | NS | 0.316 * | NS | 0.311 * | NS |
| Positive reframing | NS | 0.324 * | 0.305 * | NS | NS | 0.301 * |
| Humor | NS | 0.320 * | NS | NS | 0.367 ** | 0.326 * |
| Religion | NS | NS | NS | NS | 0.361 ** | NS |
| Τ2 FQoL | ||||||
| Family Interaction | Parenting | Emotional Well-Being | Physical/ Material Well-Being | Disability-Related Support | FQoL Total Score | |
| Active coping | NS | NS | 0.344 * | NS | 0.394 ** | 0.323 * |
| Denial | −0.454 ** | −0.431 ** | −0.426 ** | NS | −0.409 ** | −0.439 ** |
| Substance use | NS | NS | NS | −0.363 ** | NS | NS |
| Informational support | NS | NS | 0.298 * | NS | 0.396 ** | 0.286 * |
| Behavioral disengagement | −0.320 * | −0.295 * | NS | NS | −0.300 * | −0.304 * |
| Positive reframing | 0.486 *** | 0.381 ** | 0.350 * | NS | 0.476 *** | 0.460 ** |
| Planning | 0.344 * | NS | 0.301 * | NS | 0.325 * | 0.333 * |
| Humor | 0.303 * | NS | NS | NS | 0.329 * | 0.289 * |
| Acceptance | 0.391 ** | 0.423 ** | 0.321 * | NS | 0.368 ** | 0.402 ** |
| Family Quality of Life (FQoL)—Τ1 | |||||
|---|---|---|---|---|---|
| FQoL Total Score | |||||
| Beta | SE | p-Value | 95% C.I. for B | ||
| R2 = 65.0% | Marital status | ||||
| Married | 0.596 | 0.114 | <0.001 | 0.367–0.825 | |
| Monthly income | |||||
| 800–2500€ | −0.091 | 0.033 | 0.010 | −0.158–0.023 | |
| 2.500€+ | 0.124 | 0.029 | <0.001 | 0.066−0.182 | |
| Self-blame | −0.133 | 0.044 | 0.004 | −0.221–0.044 | |
| Positive reframing | 0.166 | 0.033 | <0.001 | 0.100–0.233 | |
| Family Quality of Life (FQoL)—Τ2 | |||||
| FQol Total Score | |||||
| Beta | SE | p-Value | 95% C.I. for B | ||
| R2 = 31.1% | Positive reframing | 0.107 | 0.047 | 0.028 | 0.012–0.202 |
| Treatment control | 0.134 | 0.045 | 0.004 | 0.044–0.224 | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Papadopoulos, A.; Tsapara, A.; Gryparis, A.; Tafiadis, D.; Trimmis, N.; Plotas, P.; Skapinakis, P.; Tzoufi, M.; Siafaka, V. A Prospective Study of the Family Quality of Life, Illness Perceptions, and Coping in Mothers of Children Newly Diagnosed with Autism Spectrum Disorder and Communication Difficulties. Eur. J. Investig. Health Psychol. Educ. 2024, 14, 2187-2204. https://doi.org/10.3390/ejihpe14080146
Papadopoulos A, Tsapara A, Gryparis A, Tafiadis D, Trimmis N, Plotas P, Skapinakis P, Tzoufi M, Siafaka V. A Prospective Study of the Family Quality of Life, Illness Perceptions, and Coping in Mothers of Children Newly Diagnosed with Autism Spectrum Disorder and Communication Difficulties. European Journal of Investigation in Health, Psychology and Education. 2024; 14(8):2187-2204. https://doi.org/10.3390/ejihpe14080146
Chicago/Turabian StylePapadopoulos, Angelos, Angeliki Tsapara, Alexandros Gryparis, Dionysios Tafiadis, Nikolaos Trimmis, Panagiotis Plotas, Petros Skapinakis, Meropi Tzoufi, and Vassiliki Siafaka. 2024. "A Prospective Study of the Family Quality of Life, Illness Perceptions, and Coping in Mothers of Children Newly Diagnosed with Autism Spectrum Disorder and Communication Difficulties" European Journal of Investigation in Health, Psychology and Education 14, no. 8: 2187-2204. https://doi.org/10.3390/ejihpe14080146
APA StylePapadopoulos, A., Tsapara, A., Gryparis, A., Tafiadis, D., Trimmis, N., Plotas, P., Skapinakis, P., Tzoufi, M., & Siafaka, V. (2024). A Prospective Study of the Family Quality of Life, Illness Perceptions, and Coping in Mothers of Children Newly Diagnosed with Autism Spectrum Disorder and Communication Difficulties. European Journal of Investigation in Health, Psychology and Education, 14(8), 2187-2204. https://doi.org/10.3390/ejihpe14080146










