Mentalized Affectivity, Helicopter Parenting, and Psychopathological Risk in Emerging Adults: A Network Analysis
Abstract
1. Introduction
1.1. Mentalized Affectivity in Emerging Adulthood
1.2. Emerging Adults and Helicopter Parenting
1.3. The Present Study
2. Materials and Methods
2.1. Participants
2.2. Procedure
2.3. Measures
2.4. Data Analytic Plan
3. Results
3.1. Missing Values Analysis and Descriptive Statistics
3.2. Associations between Dimensions
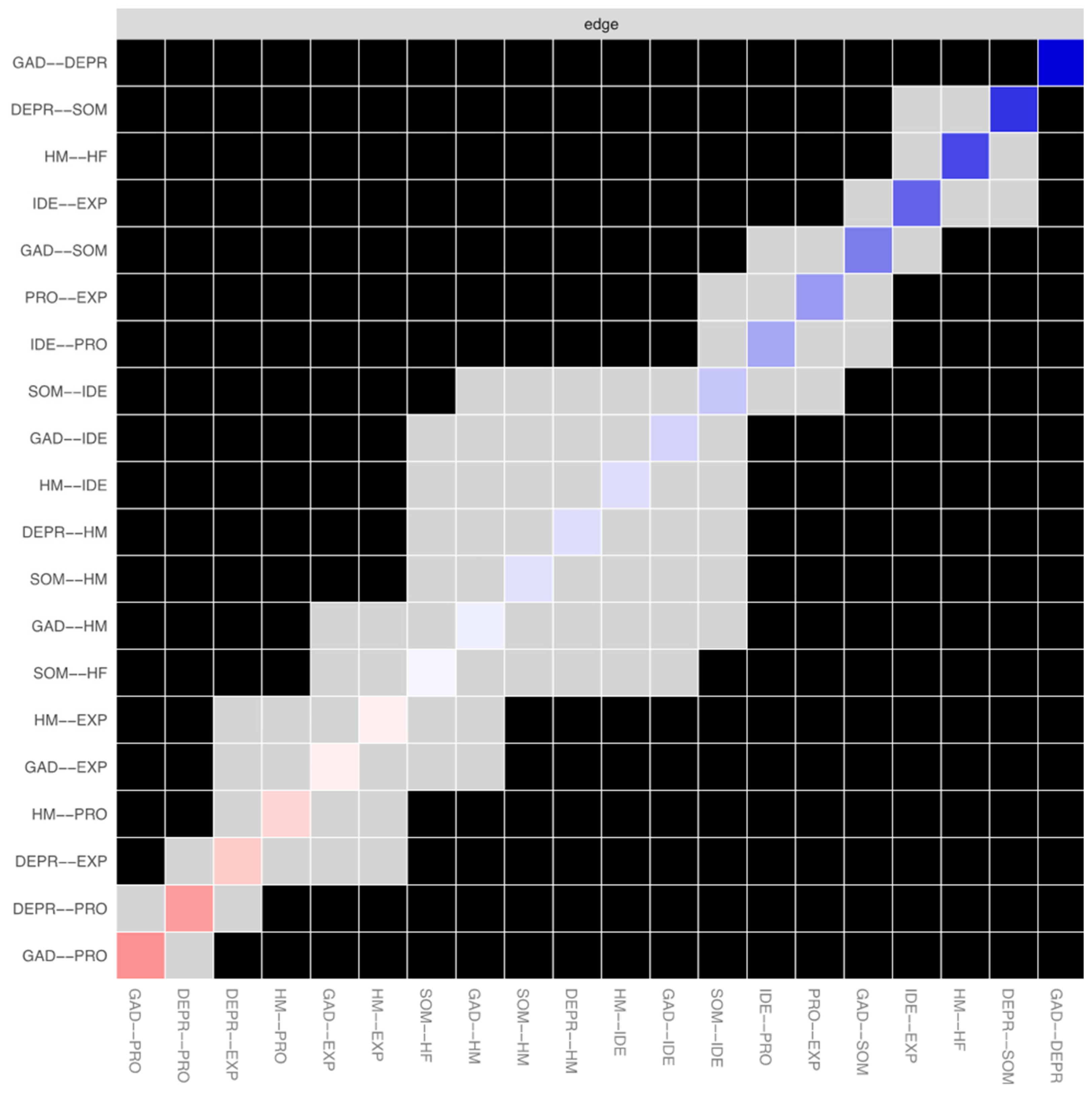
3.3. Network Stability
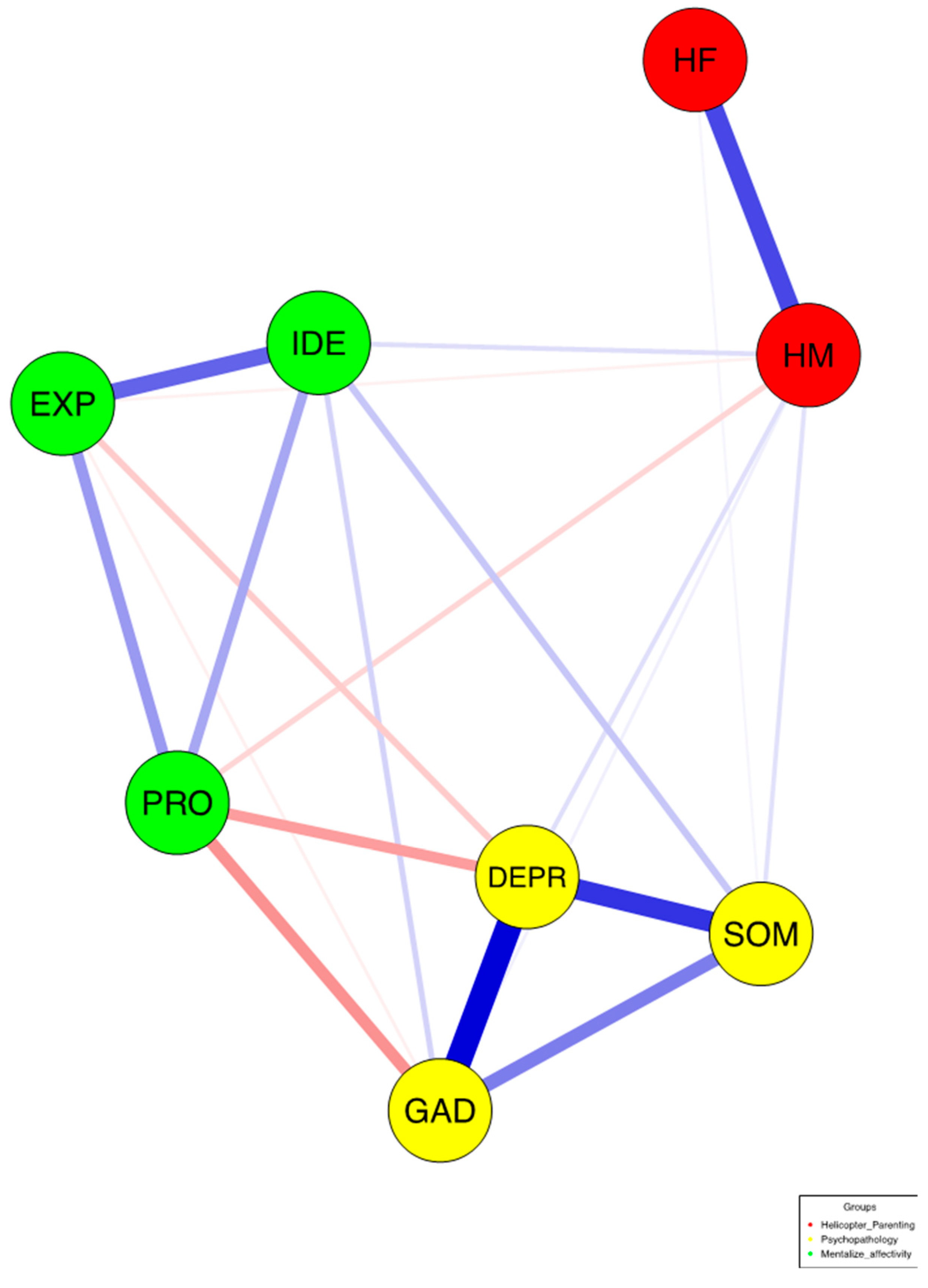
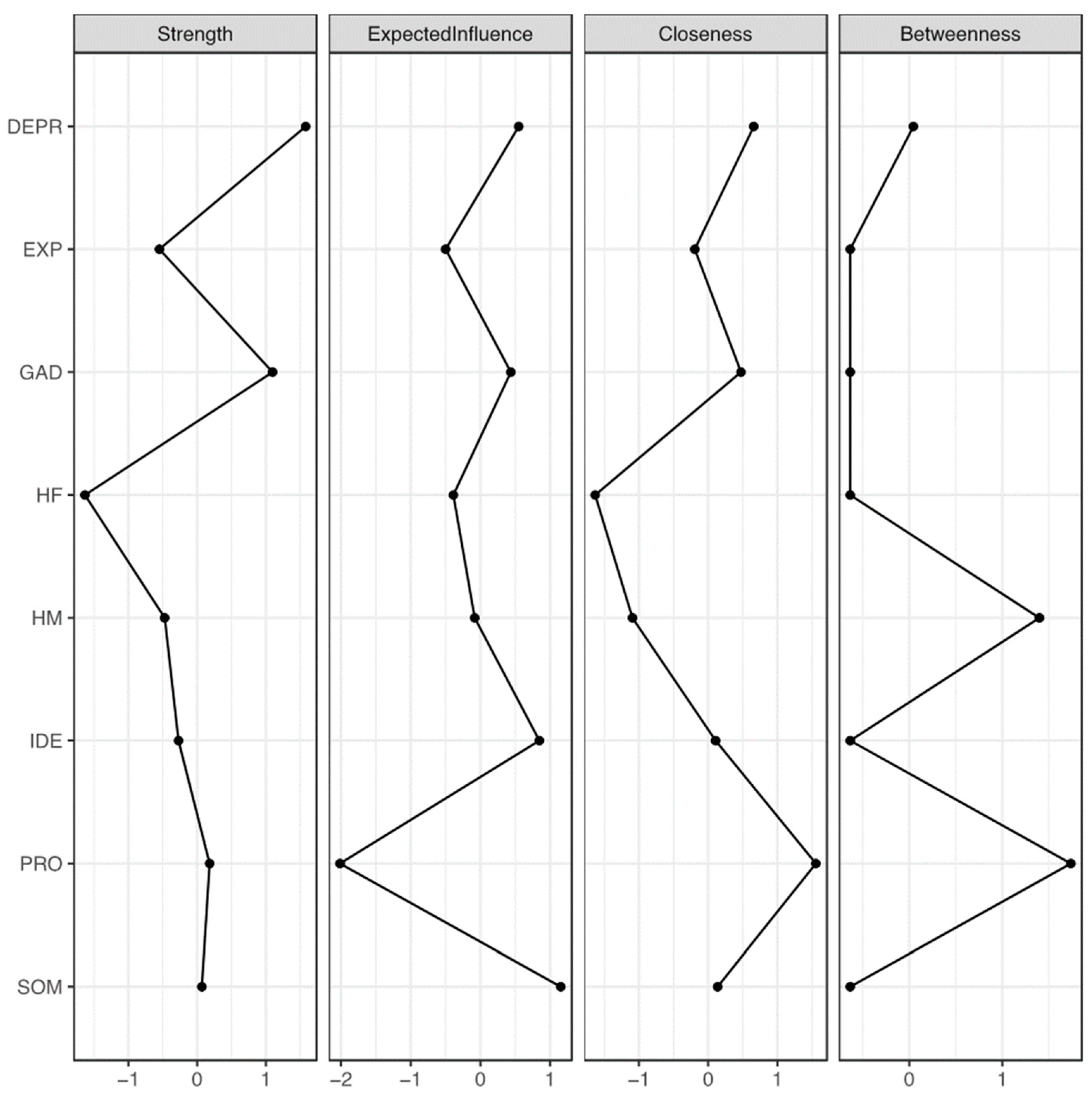
3.4. Network Estimation
3.5. Network Inference
3.6. Gender Invariance
4. Discussion
Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Arnett, J.J. Emerging adulthood: A theory of development from the late teens through the twenties. Am. Psychol. 2000, 55, 469–480. [Google Scholar] [CrossRef] [PubMed]
- Arnett, J.J. Emerging Adulthood: The Winding Road from the Late Teens through the Twenties; Oxford University Press: New York, NY, USA, 2023. [Google Scholar]
- Arnett, J.J. Afterword: Aging out of care—Toward realizing the possibilities of emerging adulthood. New Dir. Youth Dev. 2007, 113, 151–161. [Google Scholar] [CrossRef] [PubMed]
- Sumner, R.; Burrow, A.L.; Hill, P.L. Identity and purpose as predictors of subjective well-being in emerging adulthood. Emerg. Adulthood 2015, 3, 46–54. [Google Scholar] [CrossRef]
- Grosemans, I.; Hannes, K.; Neyens, J.; Kyndt, E. Emerging adults embarking on their careers: Job and identity explorations in the transition to work. Youth Soc. 2020, 52, 795–819. [Google Scholar] [CrossRef]
- Wells, R.S.; Lynch, C.M. Delayed college entry and the socioeconomic gap: Examining the roles of student plans, family income, parental education, and parental occupation. J. High. Educ. 2012, 83, 671–697. [Google Scholar] [CrossRef]
- Benzi, I.M.A.; Carone, N.; Parolin, L.; Martin-Gagnon, G.; Ensink, K.; Fontana, A. Different epistemic stances for different traumatic experiences: Implications for mentalization. Res. Psychother. Psychopathol. Process Outcome 2023, 26, 708. [Google Scholar] [CrossRef]
- Benzi IM, A.; Fontana, A.; Lingiardi, V.; Parolin, L.; Carone, N. “Don’t leave me behind!” Problematic Internet use and fear of missing out through the lens of epistemic trust in emerging adulthood. Curr. Psychol. 2024, 43, 13775–13784. [Google Scholar] [CrossRef]
- Carone, N.; Benzi, I.M.A.; Parolin, L.A.L.; Fontana, A. “I can’t miss a thing”—The contribution of defense mechanisms, grandiose narcissism, and vulnerable narcissism to fear of missing out in emerging adulthood. Personal. Individ. Differ. 2023, 214, 112333. [Google Scholar] [CrossRef]
- Persike, M.; Seiffge-Krenke, I.; Cok, F.; Głogowska, K.; Pavlopoulos, V.; Tantaros, S.; Perchec, C.; Rohail, I.; Saravia, J.C. Emerging adults’ psychopathology in seven countries: The impact of identity-related risk factors. Emerg. Adulthood 2020, 8, 179–194. [Google Scholar] [CrossRef]
- Arnett, J.J. Emerging adulthood: What is it, and what is it good for? Child Dev. Perspect. 2007, 1, 68–73. [Google Scholar] [CrossRef]
- Reinherz, H.Z.; Paradis, A.D.; Giaconia, R.M.; Stashwick, C.K.; Fitzmaurice, G. Childhood and adolescent predictors of major depressive disorder in the transition to adulthood. Am. J. Psychiatry 2003, 160, 2141–2147. [Google Scholar] [CrossRef] [PubMed]
- Schwartz, S.J. Turning point for a turning point: Advancing emerging adulthood theory and research. Emerg. Adulthood 2016, 4, 307–317. [Google Scholar] [CrossRef]
- Solmi, M.; Radua, J.; Olivola, M.; Croce, E.; Soardo, L.; de Pablo, G.S.; Shin, J.I.; Kirkbride, J.B.; Jones, P.; Kim, J.H.; et al. Age at onset of mental disorders worldwide: Large-scale meta-analysis of 192 epidemiological studies. Mol. Psychiatry 2022, 27, 281–295. [Google Scholar] [CrossRef] [PubMed]
- Stone, A.L.; Becker, L.G.; Huber, A.M.; Catalano, R.F. Review of risk and protective factors of substance use and problem use in emerging adulthood. Addict. Behav. 2012, 37, 747–775. [Google Scholar] [CrossRef] [PubMed]
- LeBlanc, N.J.; Brown, M.; Henin, A. Anxiety disorders in emerging adulthood. In Clinical Handbook of Anxiety Disorders. Current Clinical Psychiatry; Bui, E., Charney, M., Baker, A., Eds.; Humana: Cham, Switzerland, 2020. [Google Scholar] [CrossRef]
- Auerbach, R.P.; Mortier, P.; Bruffaerts, R.; Alonso, J.; Benjet, C.; Cuijpers, P.; Demyttenaere, K.; Ebert, D.D.; Green, J.G.; Hasking, P.; et al. WHO world mental health surveys international college student project: Prevalence and distribution of mental disorders. J. Abnorm. Psychol. 2018, 127, 623–638. [Google Scholar] [CrossRef] [PubMed]
- Essau, C.A.; Lewinsohn, P.M.; Lim, J.X.; Ho, M.R.; Rohde, P. Incidence, recurrence and comorbidity of anxiety disorders in four major developmental stages. J. Affect. Disord. 2018, 228, 248–253. [Google Scholar] [CrossRef]
- Asselmann, E.; Beesdo-Baum, K. Predictors of the course of anxiety disorders in adolescents and young adults. Curr. Psychiatry Rep. 2015, 17, 7. [Google Scholar] [CrossRef]
- Kessler, R.C.; Berglund, P.; Demler, O.; Jin, R.; Merikangas, K.R.; Walters, E.E. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Arch. Psychiatry 2005, 62, 593–602. [Google Scholar] [CrossRef]
- US Department of Health and Human Services. Major Depression. National Institute of Mental Health; 2022. Available online: https://www.nimh.nih.gov/health/statistics/major-depression#:~:text=Prevalence%20of%20Major%20Depressive%20Episode%20Among%20Adults,figure%201%20shows&text=The%20prevalence%20of%20major%20depressive,18%2D25%20(18.6%25) (accessed on 7 June 2024).
- Akhtar, P.; Ma, L.; Waqas, A.; Naveed, S.; Li, Y.; Rahman, A.; Wang, Y. Prevalence of depression among university students in low and middle income countries (LMICs): A systematic review and meta-analysis. J. Affect. Disord. 2020, 274, 911–919. [Google Scholar] [CrossRef]
- Mondi, C.F.; Reynolds, A.J.; Ou, S.R. Predictors of depressive symptoms in emerging adulthood in a low-income urban cohort. J. Appl. Dev. Psychol. 2017, 50, 45–59. [Google Scholar] [CrossRef]
- Twenge, J.M.; Cooper, A.B.; Joiner, T.E.; Duffy, M.E.; Binau, S.G. Age, period, and cohort trends in mood disorder indicators and suicide-related outcomes in a nationally representative dataset, 2005–2017. J. Abnorm. Psychol. 2019, 128, 185–199. [Google Scholar] [CrossRef] [PubMed]
- Fischer, S.; Gaab, J.; Ehlert, U.; Nater, U.M. Prevalence, overlap, and predictors of functional somatic syndromes in a student sample. Int. J. Behav. Med. 2013, 20, 184–193. [Google Scholar] [CrossRef] [PubMed]
- Petersen, M.W.; Schröder, A.; Jørgensen, T.; Ørnbøl, E.; Dantoft, T.M.; Eliasen, M.; Carstensen, T.W.; Eplov, L.F.; Fink, P. Prevalence of functional somatic syndromes and bodily distress syndrome in the Danish population: The DanFunD study. Scand. J. Public Health 2020, 48, 567–576. [Google Scholar] [CrossRef] [PubMed]
- Schlarb, A.A.; Claßen, M.; Hellmann, S.M.; Vögele, C.; Gulewitsch, M.D. Sleep and somatic complaints in university students. J. Pain Res. 2017, 1189–1199. [Google Scholar] [CrossRef] [PubMed]
- Costanian, C.; Tamim, H.; Assaad, S. Prevalence and factors associated with irritable bowel syndrome among university students in Lebanon: Findings from a cross-sectional study. World J. Gastroenterol. 2015, 21, 3628–3635. [Google Scholar] [CrossRef] [PubMed]
- Gulewitsch, M.D.; Enck, P.; Hautzinger, M.; Schlarb, A.A. Irritable bowel syndrome symptoms among German students: Prevalence, characteristics, and associations to somatic complaints, sleep, quality of life, and childhood abdominal pain. Eur. J. Gastroenterol. Hepatol. 2011, 23, 311–316. [Google Scholar] [CrossRef]
- Bateman, A.W.; Fonagy, P. Mentalization-based treatment of BPD. J. Personal. Disord. 2004, 18, 36–51. [Google Scholar] [CrossRef]
- Jurist, E. Minding Emotions: Cultivating Mentalization in Psychotherapy; Guilford Publications: New York, NY, USA, 2018. [Google Scholar]
- Liotti, M.; Spitoni, G.F.; Lingiardi, V.; Marchetti, A.; Speranza, A.M.; Valle, A.; Jurist, E.; Giovanardi, G. Mentalized affectivity in a nutshell: Validation of the Italian version of the Brief-Mentalized Affectivity Scale (B-MAS). PLoS ONE 2021, 16, e0260678. [Google Scholar] [CrossRef]
- Greenberg, D.M.; Kolasi, J.; Hegsted, C.P.; Berkowitz, Y.; Jurist, E.L. Mentalized affectivity: A new model and assessment of emotion regulation. PLoS ONE 2017, 12, e0185264. [Google Scholar] [CrossRef]
- Charpentier-Mora, S.; Bastianoni, C.; Cavanna, D.; Bizzi, F. Emerging adults facing the COVID-19 pandemic: Emotion dysregulation, mentalizing, and psychological symptoms. Curr. Psychol. 2024, 43, 13083–13088. [Google Scholar] [CrossRef]
- Rinaldi, T.; Castelli, I.; Greco, A.; Greenberg, D.M.; Jurist, E.; Valle, A.; Marchetti, A. The mentalized affectivity scale (MAS): Development and validation of the Italian version. PLoS ONE 2021, 16, e0249272. [Google Scholar] [CrossRef]
- Korzeniowski, C.; Ison, M.S.; Difabio de Anglat, H. A summary of the developmental trajectory of executive functions from birth to adulthood. In Psychiatry and Neuroscience Update; Gargiulo, P.Á., Mesones Arroyo, H.L., Eds.; Springer: Cham, Switzerland, 2021. [Google Scholar] [CrossRef]
- Brewer, S.K.; Zahniser, E.; Conley, C.S. Longitudinal impacts of emotion regulation on emerging adults: Variable-and person-centered approaches. J. Appl. Dev. Psychol. 2016, 47, 1–12. [Google Scholar] [CrossRef]
- Chan, S.; Rawana, J.S. Examining the associations between interpersonal emotion regulation and psychosocial adjustment in emerging adulthood. Cogn. Ther. Res. 2021, 45, 652–662. [Google Scholar] [CrossRef]
- Luyten, P.; Campbell, C.; Allison, E.; Fonagy, P. The mentalizing approach to psychopathology: State of the art and future directions. Annu. Rev. Clin. Psychol. 2020, 16, 297–325. [Google Scholar] [CrossRef]
- Ekeblad, A.; Falkenstrom, F.; Holmqvist, R. Reflective functioning as predictor of working alliance and outcome in the treatment of depression. J. Consult. Clin. Psychol. 2016, 84, 67–78. [Google Scholar] [CrossRef]
- Ensink, K.; Begin, M.; Normandin, L.; Fonagy, P. Maternal and child reflective functioning in the context of child sexual abuse: Pathways to depression and externalising difficulties. Eur. J. Psychotraumatol. 2016, 7, 30611. [Google Scholar] [CrossRef]
- Chevalier, V.; Simard, V.; Achim, J. Meta-analyses of the associations of mentalization and proxy variables with anxiety and internalizing problems. J. Anxiety Disord. 2023, 95, 102694. [Google Scholar] [CrossRef]
- Subic-Wrana, C.; Beutel, M.E.; Knebel, A.; Lane, R.D. Theory of mind and emotional awareness deficits in patients with somatoform disorders. Psychosom. Med. 2010, 72, 404–411. [Google Scholar] [CrossRef]
- Zunhammer, M.; Halski, A.; Eichhammer, P.; Busch, V. Theory of mind and emotional awareness in chronic somatoform pain patients. PLoS ONE 2015, 10, e0140016. [Google Scholar] [CrossRef][Green Version]
- Vigdal, J.S.; Brønnick, K.K. A systematic review of “helicopter parenting” and its relationship with anxiety and depression. Front. Psychol. 2022, 13, 872981. [Google Scholar] [CrossRef]
- Segrin, C.; Woszidlo, A.; Givertz, M.; Bauer, A.; Murphy, M.T. The association between overparenting, parent-child communication, and entitlement and adaptive traits in adult children. Fam. Relat. 2012, 61, 237–252. [Google Scholar] [CrossRef]
- Ishizuka, P. Social class, gender, and contemporary parenting standards in the United States: Evidence from a national survey experiment. Soc. Forces 2019, 98, 31–58. [Google Scholar] [CrossRef]
- Schiffrin, H.H.; Liss, M.; Miles-McLean, H.; Geary, K.A.; Erchull, M.J.; Tashner, T. Helping or hovering? The effects of helicopter parenting on college students’ well-being. J. Child Fam. Stud. 2014, 23, 548–557. [Google Scholar] [CrossRef]
- Carone, N.; Gartrell, N.K.; Rothblum, E.D.; Koh, A.S.; Bos, H.M.W. Helicopter parenting, emotional avoidant coping, mental health, and homophobic stigmatization among emerging adult offspring of lesbian parents. J. Fam. Psychol. 2022, 36, 1205–1215. [Google Scholar] [CrossRef]
- Carone, N.; Benzi, I.M.A.; Muzi, L.; Parolin, L.A.L.; Fontana, A. Problematic Internet use in emerging adulthood to escape from maternal helicopter parenting: Defensive functioning as a mediating mechanism. Res. Psychother. Psychopathol. Process Outcome 2023, 26, 693. [Google Scholar] [CrossRef]
- Nelson, L.J.; Padilla-Walker, L.M.; Carroll, J.S.; Madsen, S.D.; Barry, C.M.; Badger, S. “If you want me to treat you like an adult, start acting like one!” Comparing the criteria that emerging adults and their parents have for adulthood. J. Fam. Psychol. 2007, 21, 665–674. [Google Scholar] [CrossRef]
- Nelson, L.J.; Padilla-Walker, L.M.; McLean, R.D. Longitudinal predictors of helicopter parenting in emerging adulthood. Emerg. Adulthood 2021, 9, 240–251. [Google Scholar] [CrossRef]
- Deci, E.L.; Ryan, R.M. Facilitating optimal motivation and psychological well-being across life’s domains. Can. Psychol. 2008, 49, 14–23. [Google Scholar] [CrossRef]
- Cui, M.; Darling, C.A.; Coccia, C.; Fincham, F.D.; May, R.W. Indulgent parenting, helicopter parenting, and well-being of parents and emerging adults. J. Child Fam. Stud. 2019, 28, 860–871. [Google Scholar] [CrossRef]
- Reed, K.; Duncan, J.M.; Lucier-Greer, M.; Fixelle, C.; Ferraro, A.J. Helicopter parenting and emerging adult self-efficacy: Implications for mental and physical health. J. Child Fam. Stud. 2016, 25, 3136–3149. [Google Scholar] [CrossRef]
- Villegas-Pantoja, M.; Guzm’an-Facundo, F.; Alonso-Castillo, M.; de la Rubia, J.M.; López-Garcıa, K. Parenting behaviors and their relationship with alcohol involvement in Mexican teenagers and young adults. J. Child Adolesc. Subst. Abus. 2018, 27, 227–237. [Google Scholar] [CrossRef]
- Moilanen, K.L.; Lynn Manuel, M. Helicopter parenting and adjustment outcomes in young adulthood: A consideration of the mediating roles of mastery and self-regulation. J. Child Fam. Stud. 2019, 28, 2145–2158. [Google Scholar] [CrossRef]
- Hayes, K.N.; Turner, L.A. The relation of helicopter parenting to maladaptive perfectionism in emerging adults. J. Fam. Issues 2021, 42, 2986–3000. [Google Scholar] [CrossRef]
- Hong, P.; Cui, M. Helicopter parenting and college students’ psychological maladjustment: The role of self-control and living arrangement. J. Child Fam. Stud. 2020, 29, 338–347. [Google Scholar] [CrossRef]
- Turner, L.A.; Faulk, R.D.; Garner, T. Helicopter parenting, authenticity, and depressive symptoms: A mediation model. J. Genet. Psychol. 2020, 181, 500–505. [Google Scholar] [CrossRef] [PubMed]
- Nguyen, Q.; Madison, S.; Ekas, N.V.; Kouros, C.D. Helicopter parenting behaviors and emerging adult mental health: The mediating role of emotion dysregulation. Emerg. Adulthood, 2024; online ahead of pub. [Google Scholar] [CrossRef]
- Wang, C.; Shi, H.; Li, G. Helicopter parenting and college student depression: The mediating effect of physical self-esteem. Front. Psychiatry 2024, 14, 1329248. [Google Scholar] [CrossRef] [PubMed]
- Robinaugh, D.J.; Hoekstra, R.H.; Toner, E.R.; Borsboom, D. The network approach to psychopathology: A review of the literature 2008–2018 and an agenda for future research. Psychol. Med. 2020, 50, 353–366. [Google Scholar] [CrossRef]
- Spitzer, R.L.; Kroenke, K.; Williams, J.B.; Löwe, B. A brief measure for assessing generalized anxiety disorder: The GAD-7. Arch. Intern. Med. 2006, 166, 1092–1097. [Google Scholar] [CrossRef]
- Kroenke, K.; Spitzer, R.L.; Williams, J.B. The PHQ-9: Validity of a brief depression severity measure. J. Gen. Intern. Med. 2001, 16, 606–613. [Google Scholar] [CrossRef]
- Spitzer, R.L.; Kroenke, K.; Williams, J.B.W.; Patient Health Questionnaire Study Group. Validity and utility of a self-report version of PRIME-MD: The PHQ Primary Care Study. JAMA 1999, 282, 1737–1744. [Google Scholar] [CrossRef]
- Kroenke, K.; Spitzer, R.L.; Williams, J.B. The PHQ-15: Validity of a new measure for evaluating the severity of somatic symptoms. Psychosom. Med. 2002, 64, 258–266. [Google Scholar] [CrossRef] [PubMed]
- Odenweller, K.G.; Booth-Butterfield, M.; Weber, K. Investigating helicopter parenting, family environments, and relational outcomes for millennials. Commun. Stud. 2014, 65, 407–425. [Google Scholar] [CrossRef]
- Pistella, J.; Izzo, F.; Isolani, S.; Ioverno, S.; Baiocco, R. Helicopter mothers and helicopter fathers: Italian adaptation and validation of the Helicopter Parenting Instrument. Psychol. Hub 2020, 37, 37–46. [Google Scholar] [CrossRef]
- Greenberg, D.M.; Rudenstine, S.; Alaluf, R.; Jurist, E.L. Development and validation of the Brief-Mentalized Affectivity Scale: Evidence from cross-sectional online data and an urban community-based mental health clinic. J. Clin. Psychol. 2021, 77, 2638–2652. [Google Scholar] [CrossRef] [PubMed]
- R Core Team. R: A Language and Environment for Statistical Computing; R Foundation for Statistical Computing: Vienna, Austria, 2024. [Google Scholar]
- Tabachnick, B.G.; Fidell, L.S. Using Multivariate Statistics, 6th ed.; Pearson: Boston, MA, USA, 2013. [Google Scholar]
- Epskamp, S.; Borsboom, D.; Fried, E.I. Estimating psychological networks and their accuracy: A tutorial paper. Behav. Res. Methods 2018, 50, 195–212. [Google Scholar] [CrossRef]
- Foygel, R.; Drton, M. Extended Bayesian information Criteria for Gaussian Graphical Models. Advances in Neural Information Processing Systems 23, Proceedings of the 24th Annual Conference on Neural Information Processing Systems, Vancouver, BC, Canada, 6–9 December 2010. Available online: www.researchgate.net/publication/47860378_Extended_Bayesian_Information_Criteria_for_Gaussian_Graphical_Models (accessed on 20 September 2022).
- Friedman, J.; Hastie, T.; Tibshirani, R. Sparse inverse covariance estimation with the graphical lasso. Biostatistics 2008, 9, 432–441. [Google Scholar] [CrossRef]
- Bringmann, L.F.; Elmer, T.; Epskamp, S.; Krause, R.W.; Schoch, D.; Wichers, M.; Wigman, J.T.W.; Snippe, E. What do centrality measures measure in psychological networks? J. Abnorm. Psychol. 2019, 128, 892–903. [Google Scholar] [CrossRef]
- Costantini, G.; Epskamp, S.; Borsboom, D.; Perugini, M.; Mõttus, R.; Waldorp, L.J.; Cramer, A.O.J. State of the aRt personality research: A tutorial on network analysis of personality data in R. J. Res. Personal. 2015, 54, 13–29. [Google Scholar] [CrossRef]
- Burger, J.; Isvoranu, A.-M.; Lunansky, G.; Haslbeck, J.M.B.; Epskamp, S.; Hoekstra, R.H.A.; Fried, E.I.; Borsboom, D.; Blanken, T.F. Reporting standards for psychological network analyses in cross-sectional data. Psychol. Methods 2023, 28, 806–824. [Google Scholar] [CrossRef]
- Jones, P.J.; Ma, R.; McNally, R.J. Bridge centrality: A network approach to understanding comorbidity. Multivar. Behav. Res. 2021, 56, 353–367. [Google Scholar] [CrossRef]
- van Borkulo, C.D.; van Bork, R.; Boschloo, L.; Kossakowski, J.J.; Tio, P.; Schoevers, R.A.; Borsboom, D.; Waldorp, L.J. Comparing network structures on three aspects: A permutation test. Psychol. Methods 2023, 28, 1273–1285. [Google Scholar] [CrossRef] [PubMed]
- Borsboom, D. A network theory of mental disorders. World Psychiatry 2017, 16, 5–13. [Google Scholar] [CrossRef] [PubMed]
- Borsboom, D.; Cramer AO, J. Network analysis: An integrative approach to the structure of psychopathology. Annu. Rev. Clin. Psychol. 2013, 9, 91–121. [Google Scholar] [CrossRef] [PubMed]
- Hur, J.; DeYoung, K.A.; Islam, S.; Anderson, A.S.; Barstead, M.G.; Shackman, A.J. Social context and the real-world consequences of social anxiety. Psychol. Med. 2020, 50, 1989–2000. [Google Scholar] [CrossRef]
- Kranzler, A.; Elkins, R.M.; Albano, A.M. Anxiety in emerging adulthood: A developmentally informed treatment model. In Pediatric Anxiety Disorders; Elsevier: Amsterdam, The Netherlands, 2019; pp. 499–519. [Google Scholar]
- García, A.G.; Velazquez, M.L. Relationship between academic self-efficacy, performance and anxious and depressive symptoms in emerging adult college students. Educación 2020, 29, 87–109. [Google Scholar] [CrossRef]
- Boden, J.M.; Fergusson, D.M.; Horwood, L.J. Anxiety disorders and suicidal behaviours in adolescence and young adulthood: Findings from a longitudinal study. Psychol. Med. 2007, 37, 431–440. [Google Scholar] [CrossRef]
- Salmela-Aro, K.; Aunola, K.; Nurmi, J.E. Trajectories of depressive symptoms during emerging adulthood: Antecedents and consequences. Eur. J. Dev. Psychol. 2008, 5, 439–465. [Google Scholar] [CrossRef]
- Rohde, P.; Lewinsohn, P.M.; Klein, D.N.; Seeley, J.R.; Gau, J.M. Key characteristics of major depressive disorder occurring in childhood, adolescence, emerging adulthood, adulthood. Clin. Psychol. Sci. 2013, 1, 41–53. [Google Scholar] [CrossRef]
- Anderson, K.K.; John-Baptiste, A.; MacDougall, A.G.; Li, L.; Kurdyak, P.; Osuch, E.A. Access and health system impact of an early intervention treatment program for emerging adults with mood and anxiety disorders. Can. J. Psychiatry 2019, 64, 492–500. [Google Scholar] [CrossRef]
- Arcaro, J.; Summerhurst, C.; Vingilis, E.; Wammes, M.; Osuch, E. Presenting concerns of emerging adults seeking treatment at an early intervention outpatient mood and anxiety program. Psychol. Health Med. 2017, 22, 978–986. [Google Scholar] [CrossRef]
- Breedvelt, J.J.F.; Kandola, A.; Kousoulis, A.A.; Brouwer, M.E.; Karyotaki, E.; Bockting, C.L.H.; Cuijpers, P. What are the effects of preventative interventions on major depressive disorder (MDD) in young adults? A systematic review and meta-analysis of randomized controlled trials. J. Affect. Disord. 2018, 239, 18–29. [Google Scholar] [CrossRef] [PubMed]
- Hoffman, L.J.; Guerry, J.D.; Albano, A.M. Launching anxious young adults: A specialized cognitive-behavioral intervention for transitional aged youth. Curr. Psychiatry Rep. 2018, 20, 25. [Google Scholar] [CrossRef]
- Silfvernagel, K.; Wassermann, C.; Andersson, G. Individually tailored internet-based cognitive behavioural therapy for young adults with anxiety disorders: A pilot effectiveness study. Internet Interv. 2017, 8, 48–52. [Google Scholar] [CrossRef] [PubMed]
- LoParo, D.; Fonseca, A.C.; Matos AP, M.; Craighead, W.E. Anxiety and depression from childhood to young adulthood: Trajectories and risk factors. Child Psychiatry Hum. Dev. 2024, 55, 127–136. [Google Scholar] [CrossRef] [PubMed]
- Zimmermann, P.; Iwanski, A. Emotion regulation from early adolescence to emerging adulthood and middle adulthood: Age differences, gender differences, and emotion-specific developmental variations. Int. J. Behav. Dev. 2014, 38, 182–194. [Google Scholar] [CrossRef]
- Liu, D.Y.; Thompson, R.J. Selection and implementation of emotion regulation strategies in major depressive disorder: An integrative review. Clin. Psychol. Rev. 2017, 57, 183–194. [Google Scholar] [CrossRef]
- Cisler, J.M.; Olatunji, B.O. Emotion regulation and anxiety disorders. Curr. Psychiatry Rep. 2012, 14, 182–187. [Google Scholar] [CrossRef]
- Mirabella, M.; Carone, N.; Franco, A.; Rugo, M.A.; Speranza, A.M.; Mazzeschi, C.; Lingiardi, V.; Muzi, L. Emotional dysregulation and eating symptoms in gender dysphoria and eating disorders: The mediating role of body uneasiness. Curr. Psychol. 2024, 43, 17090–17104. [Google Scholar] [CrossRef]
- Daros, A.R.; Williams, G.E. A meta-analysis and systematic review of emotion-regulation strategies in borderline personality disorder. Harv. Rev. Psychiatry 2019, 27, 217–232. [Google Scholar] [CrossRef]
- Estévez, A.; Jáuregui, P.; Sánchez-Marcos, I.; López-González, H.; Griffiths, M.D. Attachment and emotion regulation in substance addictions and behavioral addictions. J. Behav. Addict. 2017, 6, 534–544. [Google Scholar] [CrossRef]
- Nichols, E.S.; Penner, J.; Ford, K.A.; Wammes, M.; Neufeld RW, J.; Mitchell, D.G.V.; Greening, S.G.; Théberge, J.; Williamson, P.C.; Osuch, E.A. Emotion regulation in emerging adults with major depressive disorder and frequent cannabis use. NeuroImage Clin. 2021, 30, 102575. [Google Scholar] [CrossRef] [PubMed]
- Marchica, L.A.; Keough, M.T.; Montreuil, T.C.; Derevensky, J.L. Emotion regulation interacts with gambling motives to predict problem gambling among emerging adults. Addict. Behav. 2020, 106, 106378. [Google Scholar] [CrossRef] [PubMed]
- Jiao, C.; Cui, M.; Fincham, F.D. Overparenting, loneliness, and social anxiety in emerging adulthood: The mediating role of emotion regulation. Emerg. Adulthood 2024, 12, 55–65. [Google Scholar] [CrossRef]
- Parolin, M.; Miscioscia, M.; De Carli, P.; Cristofalo, P.; Gatta, M.; Simonelli, A. Alexithymia in young adults with substance use disorders: Critical issues about specificity and treatment predictivity. Front. Psychol. 2018, 9, 645. [Google Scholar] [CrossRef]
- Moltrecht, B.; Deighton, J.; Patalay, P.; Edbrooke-Childs, J. Effectiveness of current psychological interventions to improve emotion regulation in youth: A meta-analysis. Eur. Child Adolesc. Psychiatry 2021, 30, 829–848. [Google Scholar] [CrossRef]
- Gatto, A.J.; Elliott, T.J.; Briganti, J.S.; Stamper, M.J.; Porter, N.D.; Brown, A.M.; Harden, S.M.; Cooper, L.D.; Dunsmore, J.C. Development and feasibility of an online brief emotion regulation training (BERT) program for emerging adults. Front. Public Health 2022, 10, 858370. [Google Scholar] [CrossRef]
- Boden, M.T.; Thompson, R.J.; Dizén, M.; Berenbaum, H.; Baker, J.P. Are emotional clarity and emotion differentiation related? Cogn. Emot. 2013, 27, 961–978. [Google Scholar] [CrossRef]
- Mankus, A.M.; Boden, M.T.; Thompson, R.J. Sources of variation in emotional awareness: Age, gender, and socioeconomic status. Personal. Individ. Differ. 2016, 89, 28–33. [Google Scholar] [CrossRef]
- Boden, M.T.; Thompson, R.J. Facets of emotional awareness and associations with emotion regulation and depression. Emotion 2015, 15, 399–410. [Google Scholar] [CrossRef]
- Szczygieł, D.; Buczny, J.; Bazińska, R. Emotion regulation and emotional information processing: The moderating effect of emotional awareness. Personal. Individ. Differ. 2012, 52, 433–437. [Google Scholar] [CrossRef]
- McKinney, C.; Morse, M.; Pastuszak, J. Effective and ineffective parenting: Associations with psychological adjustment in emerging adults. J. Fam. Issues 2016, 37, 1203–1225. [Google Scholar] [CrossRef]
- Kouros, C.; Pruitt, M.; Ekas, N.; Kiriaki, R.; Sunderland, M. Helicopter parenting, autonomy support, and students’ mental health and well-being: The moderating role of sex and ethnicity. J. Child Fam. Stud. 2017, 26, 939–949. [Google Scholar] [CrossRef] [PubMed]
- Pinquart, M. Associations of parenting dimensions and styles with externalizing problems of children and adolescents: An updated meta-analysis. Dev. Psychol. 2017, 53, 873–932. [Google Scholar] [CrossRef] [PubMed]
- Pinquart, M. Associations of parenting dimensions and styles with internalizing symptoms in children and adolescents: A meta-analysis. Marriage Fam. Rev. 2017, 53, 613–640. [Google Scholar] [CrossRef]
- Wyatt Kaminski, J.; Valle, L.A.; Filene, J.H.; Boyle, C.L. A meta-analytic review of components associated with parent training program effectiveness. J. Abnorm. Child Psychol. 2008, 36, 567–589. [Google Scholar] [CrossRef]
- Turner, K.A.; Elkins, S.R.; Walther, C.A.; Short, M.B.; Schanding, G.T., Jr. Too much of a good thing? Associations among parenting profiles and helicopter parenting. Fam. J. 2023, 31, 296–307. [Google Scholar] [CrossRef]
- Parolin, L.A.L.; Benzi IM, A.; Fanti, E.; Milesi, A.; Cipresso, P.; Preti, E. Italia Ti Ascolto [Italy, I am listening]: An app-based group psychological intervention during the COVID-19 pandemic. Res. Psychother. Psychopathol. Process Outcome 2021, 24, 517. [Google Scholar] [CrossRef]

| N | M | SD | Skewness | Kurtosis | |
|---|---|---|---|---|---|
| DEPR | 913 | 0.954 | 0.577 | 0.795 | 0.244 |
| EXP | 913 | 3.641 | 1.323 | 0.103 | −0.612 |
| GAD | 913 | 1.258 | 0.692 | 0.582 | −0.481 |
| HF | 913 | 3.101 | 0.870 | 0.303 | −0.227 |
| HM | 913 | 3.563 | 0.889 | 0.174 | −0.313 |
| IDE | 913 | 5.084 | 1.180 | −0.429 | −0.190 |
| PRO | 913 | 4.066 | 1.208 | −0.089 | −0.091 |
| SOM | 913 | 0.548 | 0.314 | 0.563 | −0.067 |
| Centrality Indexes | ||||
|---|---|---|---|---|
| Betweenness | Closeness | Strength | Expected Influence | |
| GAD | 0 | 0.014 | 1.011 | 0.563 |
| DEPR | 2 | 0.014 | 1.130 | 0.593 |
| SOM | 0 | 0.013 | 0.758 | 0.758 |
| HM | 6 | 0.009 | 0.624 | 0.421 |
| HF | 0 | 0.008 | 0.338 | 0.338 |
| IDE | 0 | 0.013 | 0.674 | 0.674 |
| PRO | 7 | 0.016 | 0.785 | −0.105 |
| EXP | 0 | 0.012 | 0.605 | 0.307 |
| GAD | DEPR | SOM | HM | HF | IDE | PRO | EXP | |
|---|---|---|---|---|---|---|---|---|
| GAD | 0.00 | 0.45 | 0.23 | 0.03 | 0.00 | 0.08 | 0.20 | −0.03 |
| DEPR | 0.45 | 0.00 | 0.35 | 0.06 | 0.00 | 0.00 | −0.17 | −0.09 |
| SOM | 0.23 | 0.35 | 0.00 | 0.05 | 0.02 | 0.10 | 0.00 | 0.00 |
| HM | 0.03 | 0.06 | 0.05 | 0.00 | 0.32 | 0.06 | −0.08 | −0.03 |
| HF | 0.00 | 0.00 | 0.02 | 0.32 | 0.00 | 0.00 | 0.00 | 0.00 |
| IDE | 0.08 | 0.00 | 0.10 | 0.06 | 0.00 | 0.00 | 0.16 | 0.27 |
| PRO | −0.20 | −0.17 | 0.00 | −0.08 | 0.00 | 0.16 | 0.00 | 0.18 |
| EXP | −0.03 | −0.09 | 0.00 | −0.03 | 0.00 | 0.27 | 0.18 | 0.00 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Published by MDPI on behalf of the University Association of Education and Psychology. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cruciani, G.; Fontana, A.; Benzi, I.M.A.; Sideli, L.; Parolin, L.A.L.; Muzi, L.; Carone, N. Mentalized Affectivity, Helicopter Parenting, and Psychopathological Risk in Emerging Adults: A Network Analysis. Eur. J. Investig. Health Psychol. Educ. 2024, 14, 2523-2541. https://doi.org/10.3390/ejihpe14090167
Cruciani G, Fontana A, Benzi IMA, Sideli L, Parolin LAL, Muzi L, Carone N. Mentalized Affectivity, Helicopter Parenting, and Psychopathological Risk in Emerging Adults: A Network Analysis. European Journal of Investigation in Health, Psychology and Education. 2024; 14(9):2523-2541. https://doi.org/10.3390/ejihpe14090167
Chicago/Turabian StyleCruciani, Gianluca, Andrea Fontana, Ilaria Maria Antonietta Benzi, Lucia Sideli, Laura Antonia Lucia Parolin, Laura Muzi, and Nicola Carone. 2024. "Mentalized Affectivity, Helicopter Parenting, and Psychopathological Risk in Emerging Adults: A Network Analysis" European Journal of Investigation in Health, Psychology and Education 14, no. 9: 2523-2541. https://doi.org/10.3390/ejihpe14090167
APA StyleCruciani, G., Fontana, A., Benzi, I. M. A., Sideli, L., Parolin, L. A. L., Muzi, L., & Carone, N. (2024). Mentalized Affectivity, Helicopter Parenting, and Psychopathological Risk in Emerging Adults: A Network Analysis. European Journal of Investigation in Health, Psychology and Education, 14(9), 2523-2541. https://doi.org/10.3390/ejihpe14090167







