A Rare Case of Transient Acantholytic Dermatosis (AKA. Grover’s Disease) with Concomitant Pediculosis Pubis: An Atypical Presentation and First Documented Case Report
Abstract
:1. Introduction
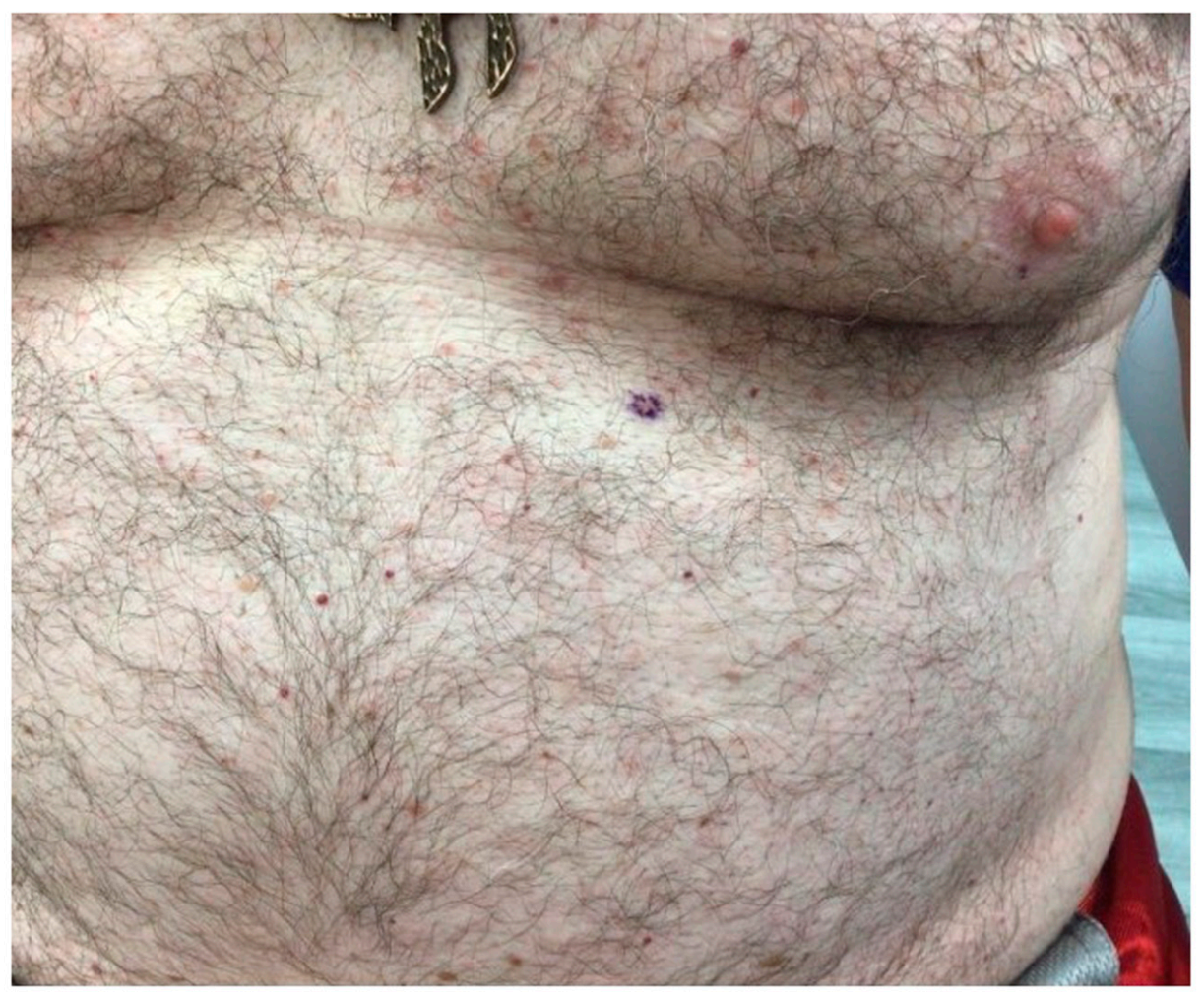
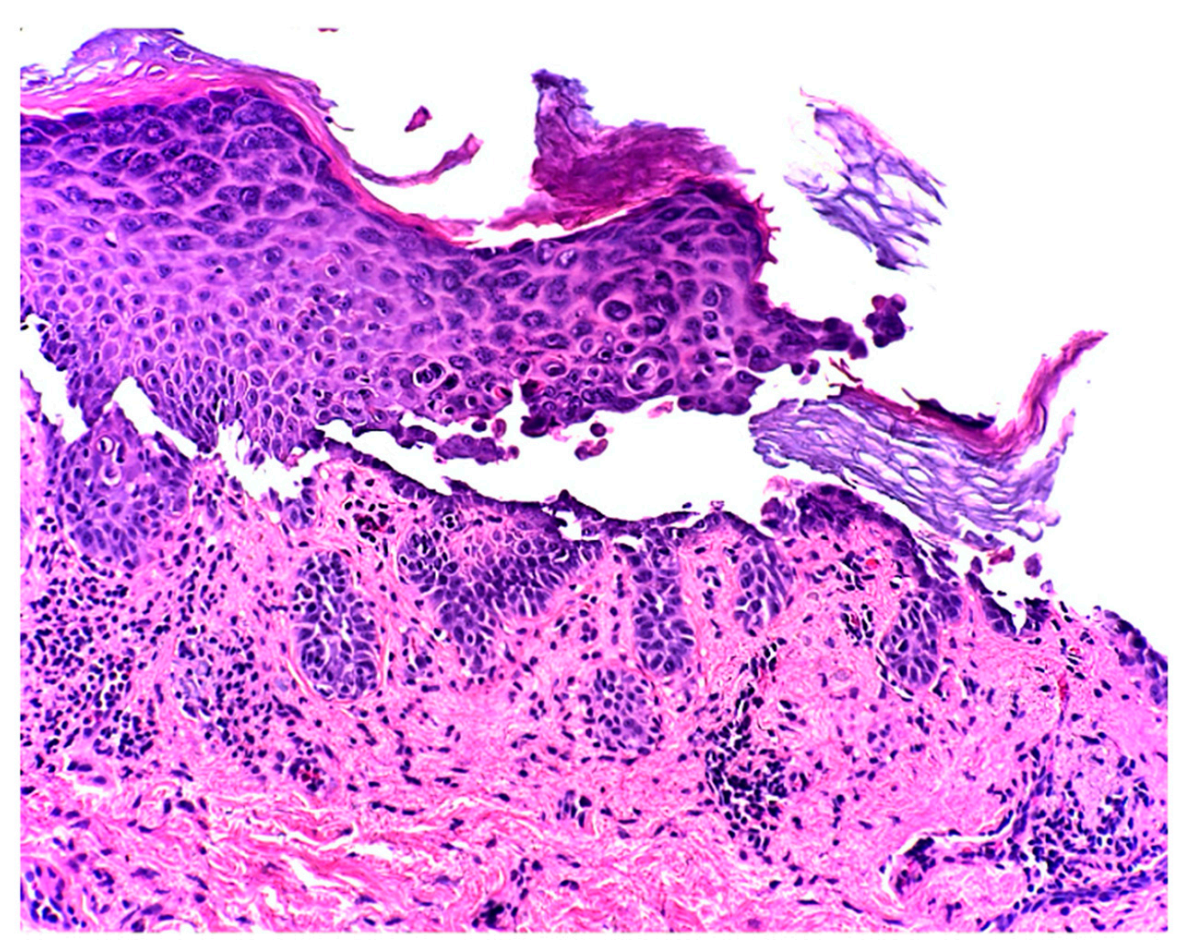
2. Case Report
3. Discussion
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- Grover, R.W. Transient acantholytic dermatosis. Arch. Dermatol. 1970, 101, 426–434. [Google Scholar] [CrossRef] [PubMed]
- Lacarrubba, F.; Boscaglia, S.; Nasca, M.R.; Caltabiano, R.; Micali, G. Grover’s disease: Dermoscopy, reflectance confocal microscopy and histopathological correlation. Dermatol. Pract. Concept. 2017, 7, 51–54. [Google Scholar] [CrossRef] [PubMed]
- Streit, M.; Paredes, B.E.; Braathen, L.R.; Brand, C.U. Transitorische akantholytische Dermatose (M. Grover). Eine Analyse des klinischen Spektrums anhand von 21 histologisch erfassten Fällen [Transitory acantholytic dermatosis (Grover disease). An analysis of the clinical spectrum based on 21 histologically assessed cases]. Hautarzt 2000, 51, 244–249. [Google Scholar] [CrossRef] [PubMed]
- Bragg, B.N.; Simon, L.V. Pediculosis. In StatPearls; StatPearls Publishing: Treasure Island, FL, USA, 2020. [Google Scholar]
- Specchio, F.; Argenziano, G.; Tiodorovic-Zivkovic, D.; Moscarella, E.; Lallas, A.; Zalaudek, I.; Longo, C. Dermoscopic clues to diagnose acantholytic dyskeratosis. Dermatol. Pract. Concept. 2015, 5, 59–60. [Google Scholar] [CrossRef] [PubMed]
- Giacomel, J.; Zalaudek, I.; Argenziano, G. Dermatoscopy of Grover’s disease and solitary acantholytic dyskeratoma shows a brown, star-like pattern. Australas. J. Dermatol. 2012, 53, 315–316. [Google Scholar] [CrossRef] [PubMed]
- Kaddu, S.; Müllegger, R.R.; Kerl, H. Grover’s disease associated with Sarcoptes scabiei. Dermatology 2001, 202, 252–254. [Google Scholar] [CrossRef] [PubMed]
- Köstler, E. Transitorische akantholytische Dermatose (Grover) bei Sarcoptes-scabiei-Infektion. Hautarzt 1997, 48, 915–917. [Google Scholar] [CrossRef] [PubMed]
- Jordaan, H.F.; du Toit, M.J.; Whitaker, D. Stellungnahme zur Arbeit von E. Köstler: ‘Transitorische akantholytische Dermatose (Grover) bei Sarcoptes-scabiei-Infektion’ in Hautarzt (1997) 48:915–917. Hautarzt 1999, 50, 305–306. [Google Scholar] [CrossRef]
- Davis, M.D.; Dinneen, A.M.; Landa, N.; Gibson, L.E. Grover’s disease: Clinicopathologic review of 72 cases. Mayo Clin. Proc. 1999, 74, 229–234. [Google Scholar] [CrossRef]
- Brouqui, P.; Stein, A.; Dupont, H.T.; Gallian, P.; Badiaga, S.; Rolain, J.-M.; Mege, J.L.; La Scola, B.; Berbis, P.; Raoult, D. Ectoparasitism and vector-borne diseases in 930 homeless people from Marseilles. Medicine 2005, 84, 61–68. [Google Scholar] [CrossRef]
- Burkhart, C.G. Relationship of treatment-resistant head lice to the safety and efficacy of pediculicides. Mayo Clin. Proc. 2004, 79, 661–666. [Google Scholar] [CrossRef]
- Wolstenholme, A.J.; Rogers, A.T. Glutamate-gated chloride channels and the mode of action of the avermectin/milbemycin anthelmintics. Parasitology 2005, 131, S85–S95. [Google Scholar] [CrossRef]
- Zhang, X.; Song, Y.; Ci, X.; An, N.; Ju, Y.; Li, H.; Wang, X.; Han, C.; Cui, J.; Deng, X. Ivermectin inhibits LPS-induced production of inflammatory cytokines and improves LPS-induced survival in mice. Inflamm. Res. 2008, 57, 524–529. [Google Scholar] [CrossRef]
- Hashimoto, K.; Moiin, A.; Chang, M.W.; Tada, J. Sudoriferous acrosyringeal acantholytic disease. A subset of Grover’s disease. J. Cutan. Pathol. 1996, 23, 151–164. [Google Scholar] [CrossRef]
- Scheinfeld, N.; Mones, J. Seasonal variation of transient acantholytic dyskeratosis (Grover’s disease). J. Am. Acad. Dermatol. 2006, 55, 263–268. [Google Scholar] [CrossRef]
- Zhu, H.J.; Clark, L.N.; Deloney, L.A.; McDonald, J.E. Grover disease (transient acantholytic dermatosis) in acute myeloid leukemia on FDG PET/CT. Clin. Nucl. Med. 2014, 39, e173–e175. [Google Scholar] [CrossRef]
- French, L.E.; Piletta, P.A.; Etienne, A.; Salomon, D.; Saurat, J.H. Incidence of transient acantholytic dermatosis (Grover’s disease) in a hospital setting. Dermatology 1999, 198, 410–411. [Google Scholar]
- Boutli, F.; Voyatzi, M.; Lefaki, I.; Chaidemenos, G.; Kanitakis, J. Transient acantholytic dermatosis (Grover’s disease) in a renal transplant patient. J. Dermatol. 2006, 33, 178–181. [Google Scholar] [CrossRef]
- Ippoliti, G.; Paulli, M.; Lucioni, M.; D’Armini, A.M.; Lauriola, M.; Saaleb, R.M.H. Grover’s Disease after Heart Transplantation: A Case Report. Case Rep. Transplant. 2012, 2012, 126592. [Google Scholar] [CrossRef]
- Parsons, J.M. Transient acantholytic dermatosis (Grover’s disease): A global perspective. J. Am. Acad. Dermatol. 1996, 35, 653–670. [Google Scholar] [CrossRef]
- Antunes, I.; Azevedo, F.; Mesquita-Guimarães, J.; Resende, C.; Fernandes, N.; MacEdo, G. Grover’s disease secondary to ribavirin. Br. J. Dermatol. 2000, 142, 1257–1258. [Google Scholar] [CrossRef]
- Crockett, J.S.; Burkemper, N.M. Grover disease (transient acantholytic dermatosis) induced by anastrozole. Cutis 2011, 88, 175–177. [Google Scholar]
- Mahler, S.J.; De Villez, R.L.; Pulitzer, D.R. Transient acantholytic dermatosis induced by recombinant human interleukin 4. J. Am. Acad. Dermatol. 1993, 29, 206–209. [Google Scholar] [CrossRef]
- Tscharner, G.G.; Bühler, S.; Borner, M.; Hunziker, T. Grover’s disease induced by cetuximab. Dermatology 2006, 213, 37–39. [Google Scholar] [CrossRef]
- Anforth, R.; Fernandez-Peñas, P.; Long, G.V. Cutaneous toxicities of RAF inhibitors. Lancet Oncol. 2013, 14, e11–e18. [Google Scholar] [CrossRef]
- Koelzer, V.H.; Buser, T.; Willi, N.; Rothschild, S.I.; Wicki, A.; Schiller, P.; Cathomas, G.; Zippelius, A.; Mertz, K.D. Grover’s-like drug eruption in a patient with metastatic melanoma under ipilimumab therapy. J. Immunother. Cancer 2016, 4, 47. [Google Scholar] [CrossRef]


Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pendlebury, G.A.; Oro, P.; Merideth, D.; Rudnick, E. A Rare Case of Transient Acantholytic Dermatosis (AKA. Grover’s Disease) with Concomitant Pediculosis Pubis: An Atypical Presentation and First Documented Case Report. Dermatopathology 2021, 8, 502-508. https://doi.org/10.3390/dermatopathology8040052
Pendlebury GA, Oro P, Merideth D, Rudnick E. A Rare Case of Transient Acantholytic Dermatosis (AKA. Grover’s Disease) with Concomitant Pediculosis Pubis: An Atypical Presentation and First Documented Case Report. Dermatopathology. 2021; 8(4):502-508. https://doi.org/10.3390/dermatopathology8040052
Chicago/Turabian StylePendlebury, Gehan A., Peter Oro, Drew Merideth, and Eric Rudnick. 2021. "A Rare Case of Transient Acantholytic Dermatosis (AKA. Grover’s Disease) with Concomitant Pediculosis Pubis: An Atypical Presentation and First Documented Case Report" Dermatopathology 8, no. 4: 502-508. https://doi.org/10.3390/dermatopathology8040052
APA StylePendlebury, G. A., Oro, P., Merideth, D., & Rudnick, E. (2021). A Rare Case of Transient Acantholytic Dermatosis (AKA. Grover’s Disease) with Concomitant Pediculosis Pubis: An Atypical Presentation and First Documented Case Report. Dermatopathology, 8(4), 502-508. https://doi.org/10.3390/dermatopathology8040052





