Effect of Different Surface Treatments on the Shear Bond Strength of Metal Orthodontic Brackets Bonded to CAD/CAM Provisional Crowns
Abstract
:1. Introduction
2. Materials and Methods
2.1. Sample
2.2. Measurement Methods
2.2.1. Natural Teeth (NT)
2.2.2. Provisional Teeth
- Group 1 (Control group)
- Group 2 (Diamond bur)
- Group 3 (Sandblaster)
- Group 4 (Plastic Conditioner)
- Group 5 (Diamond bur + Plastic Conditioner)
- Group 6 (Sandblaster + Plastic Conditioner)
- −
- 0 = no adhesive left on the tooth (Figure 4).
- −
- 1 = less than half of the adhesive left on the tooth (Figure 5).
- −
- 2 = more than half of the adhesive left on the tooth (Figure 6).
- −
- 3 = all adhesives left on the tooth with a distinct impression of the bracket mesh (Figure 7). It should be noted that scores of 0 and 1 imply a fracture of the bond at the level of the tooth/adhesive interface (adhesive failure). Scores 2 and 3 involve a fracture at the adhesive/bracket interface (cohesive failure).




2.3. Statistical Analysis
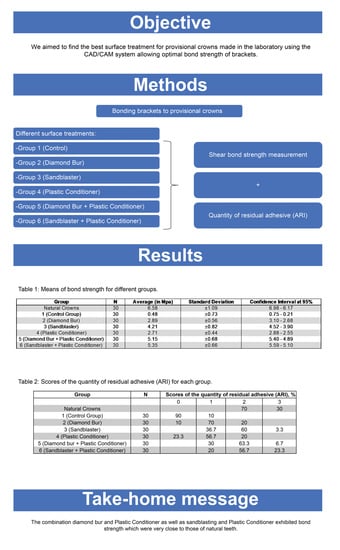
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Pabari, S.; Moles, D.R.; Cunningham, S. Assessment of motivation and psychological characteristics of adult orthodontic patients. Am. J. Orthod. Dentofac. Orthop. 2011, 140, 263–272. [Google Scholar] [CrossRef] [PubMed]
- Exbrayat, J.; Schittly, J.; Borel, J.C. Manuel de Prothèse Fixée Unitaire; Masson: Paris, France, 1992. [Google Scholar]
- Karaokutan, I.; Sayin, G.; Kara, O. In vitro study of fracture strength of provisional crown materials. J. Adv. Proathodont. 2015, 7, 27–31. [Google Scholar] [CrossRef] [PubMed]
- Uzun, G. An Overview of Dental CAD/CAM Systems. Biotechnol. Biotechnol. Equip. 2008, 22, 530–535. [Google Scholar] [CrossRef]
- Chung, C.H.; Fadem, B.W.; Levitt, H.L.; Mante, F.K. Effects of two adhesion boosters on the shear bond strength of new and rebonded orthodontic brackets. Am. J. Orthod. Dentofac. Orthop. 2000, 118, 295–299. [Google Scholar] [CrossRef]
- Dias, F.; Pinzan-Vercelino, C.; Tavares, R.; Gurgel, J.; Bramante, F.; Fialho, M. Evaluation of an alternative technique to optimize direct bonding of orthodontic brackets to temporary crowns. Dent. Press J. Orthod. 2015, 20, 57–62. [Google Scholar] [CrossRef]
- Zachrisson, Y.Ø.; Zachrisson, B.U.; Büyükyilmaz, T. Surface preparation for orthodontic bonding to porcelain. Am. J. Orthod. Dentofac. Orthop. 1996, 109, 420–430. [Google Scholar] [CrossRef]
- Tse, M. The Effect of Surface Treatments and Bonding Agents on the Shear Bond Strengths of Orthodontic Brackets Bonded to Aged Composite Resin Restorations. Master’s Thesis, The University of Western Ontario, London, ON, Canada, 2012. [Google Scholar]
- Reicheneder, C.A.; Baumert, U.; Gedrange, T.; Proff, P.; Faltermeier, A.; Muessig, D. Frictional properties of aesthetic brackets. Eur. J. Orthod. 2007, 29, 359–365. [Google Scholar] [CrossRef] [PubMed]
- Artun, J.; Bergland, S. Clinical trials with crystal growth conditioning as an alternative to acid etch enamel pretreatment. Am. J. Orthod. Dentofac. Orthop. 1984, 85, 333–340. [Google Scholar] [CrossRef]
- Davidowitz, G.; Kotick, P.G. The use of CAD/CAM in Dentistry. Dent. Clin. N. Am. 2011, 55, 559–570. [Google Scholar] [CrossRef]
- Rambhia, S.; Heshmati, R.; Dhuru, V.; Iacopino, A. Shear bond strength of orthodontic brackets bonded to provisional crown materials utilizing two different adhesives. Angle Orthod. 2009, 79, 784–789. [Google Scholar] [CrossRef]
- Maryanchick, I.; Brendlinger, E.J.; Fallis, D.W.; Vandewalle, K.S. Shear bond strength of orthodontic brackets bonded to various esthetic pontic materials. Am. J. Orthod. Dentofac. Orthop. 2010, 137, 684–689. [Google Scholar] [CrossRef] [PubMed]
- Masioli, D.L.C.; Almeida, M.A.O. Assessment of the effect of different surface treatments on the bond strength of brackets bonded to acrylic resin. Dent. Press J. Orthod. 2011, 16, 37–47. [Google Scholar] [CrossRef]
- Soon, H.I.; Gill, D.S.; Jones, S.P. A study to investigate the bond strengths of orthodontic brackets bonded to prosthetic acrylic teeth. J. Orthod. 2015, 42, 192–199. [Google Scholar] [PubMed]
- Abdul Razak, W.S.W.; Sherriff, M.; Bister, D.; Seehra, J. Bond strength of stainless-steel orthodontic brackets bonded to prefabricated acrylic teeth. J. Orthod. 2017, 44, 105–109. [Google Scholar] [CrossRef] [PubMed]
- Pseiner, B.C.; Freudenthaler, J.; Jonke, E. Shear bond strength of fluoride-releasing orthodontic bonding and composite materials. Eur. J. Orthod. 2010, 32, 268–273. [Google Scholar] [CrossRef] [PubMed]
- Purmal, K.; Sukumaran, P. Shear bond strengths of buccal tubes. Aust. Orthod. J. 2010, 26, 84–88. [Google Scholar]
- Sukhia, H.R.; Sukhia, R.H. Bracket debonding and breakage prevalence in orthodontic patients. Pak. Oral Dent. J. 2011, 31, 73–77. [Google Scholar]
- Blakey, R.; Mah, J. Effects of surface conditioning on the shear bond strength of orthodontic brackets bonded to temporary polycarbonate crowns. Am. J. Orthod. Dentofac. Orthop. 2010, 138, 72–78. [Google Scholar] [CrossRef]
- Al Jabbari, Y.S.; Al Taweel, S.M.; Al Rifaiy, M.; Alqahtani, M.Q.; Koutsoukis, T.; Zinelis, S. Effects of surface treatment and artificial aging on the shear bond strength of orthodontics brackets bonded to four different provisional restorations. Angle Orthod. 2014, 84, 649–655. [Google Scholar] [CrossRef]
- Almeida, J.X.; Depra, M.B.; Marquezan, M.; Retamoso, L.B.; Tanaka, O. Effects of surface treatment of provisional crowns on the shear bond strength of brackets. Dent. Press J. Orthod. 2013, 18, 29–34. [Google Scholar] [CrossRef]
- Egan, F.R.; Alexander, S.; Cartwright, G.E. Bond strength of rebounded orthodontic brackets. Am. J. Orthod. Dentofac. Orthop. 1996, 109, 64–70. [Google Scholar] [CrossRef]
- Zachrisson, B.U.; Büyükyilmaz, T. Bonding in orthodontics. In Orthodontics: Current Principles and Techniques, 5th ed.; Mosby International limited: Maryland Heights, MO, USA, 2011; Volume 11, pp. 727–784. [Google Scholar]
- Chay, S.H.; Wong, S.L.; Mohamed, N.; Chia, A.; Yap, A.U. Effects of surface treatment and aging on the bond strength of orthodontic brackets to provisional materials. Am. J. Orthod. Dentofac. Orthop. 2007, 132, 577–581. [Google Scholar] [CrossRef]
- Yuasa, T.; Iijima, M.; Ito, S.; Muguruma, T.; Saito, T.; Mizoguchi, I. Effects of long-term storage and thermocycling on bond strength of two self-etching primer adhesive systems. Eur. J. Orthod. 2010, 32, 285–290. [Google Scholar] [CrossRef]
- Gale, M.S.; Darvell, B.W. Thermal cycling procedures for laboratory testing of dental restorations. J. Dent. 1999, 27, 89–99. [Google Scholar] [CrossRef]
- Trites, B.; Foley, T.F.; Banting, D. Bond strength comparison of 2 self-etching primers over a 30 month storage period. Am. J. Orthod. Dentofac. Orthop. 2004, 126, 709–716. [Google Scholar] [CrossRef]
- Faltermeier, A.; Behr, M.; Müssig, D. A comparative evaluation of bracket bonding with 1-. 2-, and 3-component adhesive systems. Am. J. Orthod. Dentofac. Orthop. 2007, 132, 144–145. [Google Scholar] [CrossRef] [PubMed]
- Soliman, T.A.; Ghorab, S.; Baeshen, H. Effect of surface treatments and flash-free adhesive on the shear bond strength of ceramic orthodontic brackets to CAD/CAM provisional materials. Clin. Oral Investig. 2022, 26, 481–492. [Google Scholar] [CrossRef] [PubMed]
- Cehreli, S.B.; Polat-Ozsoy, O.; Sar, C.; Cubukcu, H.E.; Cehreli, Z.C. A comparative study of qualitative and quantitative meth- ods for the assessment of adhesive remnant after bracket debonding. Eur. J. Orthod. 2012, 34, 188–192. [Google Scholar] [CrossRef] [PubMed]
- Murray, S.D.; Hobson, R.S. Comparison of in vivo and in vitro shear bond strength. Am. J. Orthod. Dentofac. Orthop. 2003, 123, 2–9. [Google Scholar] [CrossRef] [PubMed]
- Hajrassie, M.K.; Khier, S.E. In-vivo and in-vitro comparison of bond strengths of orthodontic brackets bonded to enamel and debonded at various times. Am. J. Orthod. Dentofac. Orthop. 2007, 131, 384–390. [Google Scholar] [CrossRef]



| Group | N | Average | Standard | Confidence |
|---|---|---|---|---|
| (in MPa) | Deviation | Interval at 95% | ||
| NT | 30 | 6.58 | 1.09 | 6.98–6.17 |
| 1 | 30 | 0.48 | 0.73 | 0.75–0.21 |
| 2 | 30 | 2.89 | 0.56 | 3.10–2.68 |
| 3 | 30 | 4.21 | 0.82 | 4.52–3.70 |
| 4 | 30 | 2.71 | 0.44 | 2.88–2.55 |
| 5 | 30 | 5.15 | 0.68 | 5.40–4.89 |
| 6 | 30 | 5.35 | 0.66 | 5.59–5.10 |
| Group | N | Scores of the Quantity of Residual Adhesive (ARI), % | |||
|---|---|---|---|---|---|
| 0 | 1 | 2 | 3 | ||
| NT | 30 | 70 | 30 | ||
| 1 | 30 | 90 | 10 | ||
| 2 | 30 | 10 | 70 | 20 | |
| 3 | 30 | 36.7 | 60 | 3.3 | |
| 4 | 30 | 23.3 | 56.7 | 20 | |
| 5 | 30 | 30 | 63.3 | 6.7 | |
| 6 | 30 | 20 | 56.7 | 23.3 | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Haber, D.; Khoury, E.; Ghoubril, J.; Cirulli, N. Effect of Different Surface Treatments on the Shear Bond Strength of Metal Orthodontic Brackets Bonded to CAD/CAM Provisional Crowns. Dent. J. 2023, 11, 38. https://doi.org/10.3390/dj11020038
Haber D, Khoury E, Ghoubril J, Cirulli N. Effect of Different Surface Treatments on the Shear Bond Strength of Metal Orthodontic Brackets Bonded to CAD/CAM Provisional Crowns. Dentistry Journal. 2023; 11(2):38. https://doi.org/10.3390/dj11020038
Chicago/Turabian StyleHaber, Dany, Elie Khoury, Joseph Ghoubril, and Nunzio Cirulli. 2023. "Effect of Different Surface Treatments on the Shear Bond Strength of Metal Orthodontic Brackets Bonded to CAD/CAM Provisional Crowns" Dentistry Journal 11, no. 2: 38. https://doi.org/10.3390/dj11020038
APA StyleHaber, D., Khoury, E., Ghoubril, J., & Cirulli, N. (2023). Effect of Different Surface Treatments on the Shear Bond Strength of Metal Orthodontic Brackets Bonded to CAD/CAM Provisional Crowns. Dentistry Journal, 11(2), 38. https://doi.org/10.3390/dj11020038