A 23-Year Observational Follow-Up Clinical Evaluation of Direct Posterior Composite Restorations
Abstract
:1. Introduction
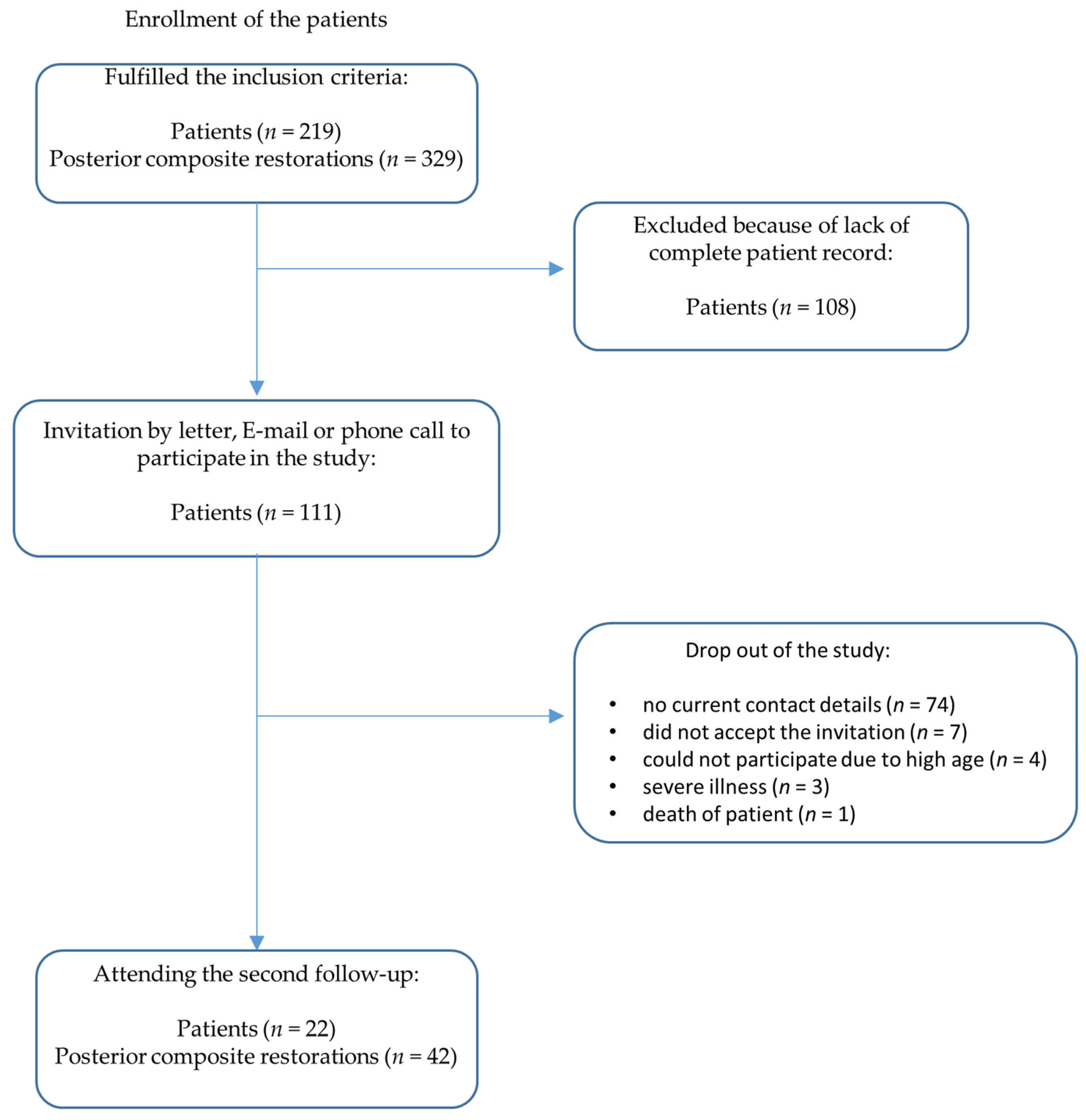
2. Materials and Methods
- Application of the posterior composite restoration happened in the 1995/1996 student courses of the Department of Operative Dentistry.
- All restorations were placed in permanent vital teeth that showed no pain symptoms at the time of placement.
- A micro-hybrid composite was used for the restorations (Herculite XRV, Kerr, Karlsruhe, Germany).
- The application followed a predefined clinical protocol.
- All patients were aged 18–70 years at the time of placement.
- All patients had been consecutively evaluated at the first follow-up examination between 1995 and 1997 within 36 months after the insertion of restorations.
- No night guard or similar device was provided to the patients.
- Surface luster;
- Aesthetic anatomical form;
- 3.
- Fracture of material and retention;
- 4.
- Marginal adaptation;
- 5.
- Occlusal contour and wear;
- 6.
- Approximal anatomical form;
- 7.
- Tooth integrity (enamel crack, tooth fractures).
- 1—clinically excellent/very good;
- 2—clinically good;
- 3—clinically sufficient/satisfactory;
- 4—clinically unsatisfactory;
- 5—clinically poor;
- 6—restoration or tooth missing.
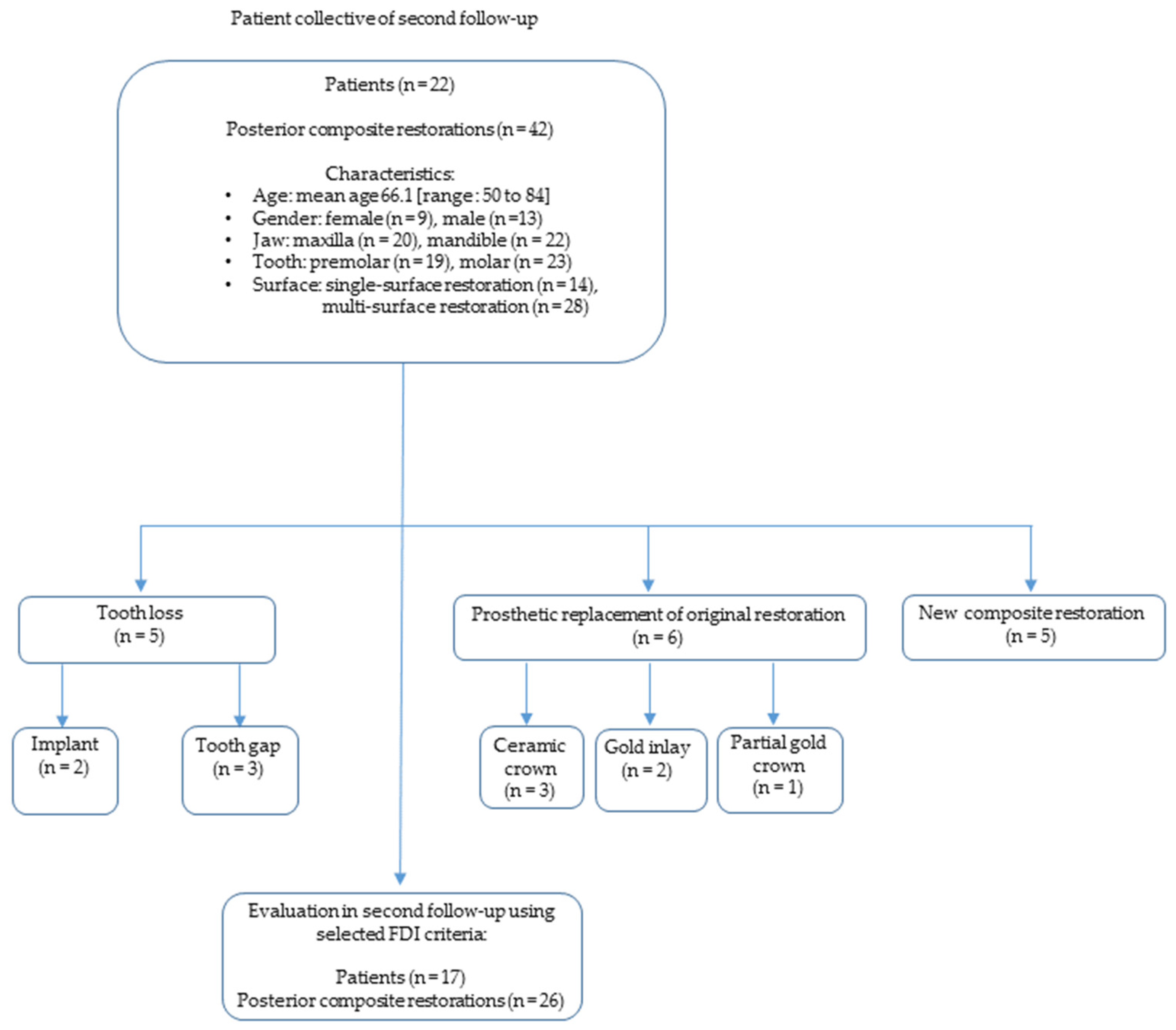
3. Results
3.1. Clinical Performance in Accordance with Selected FDI Criteria
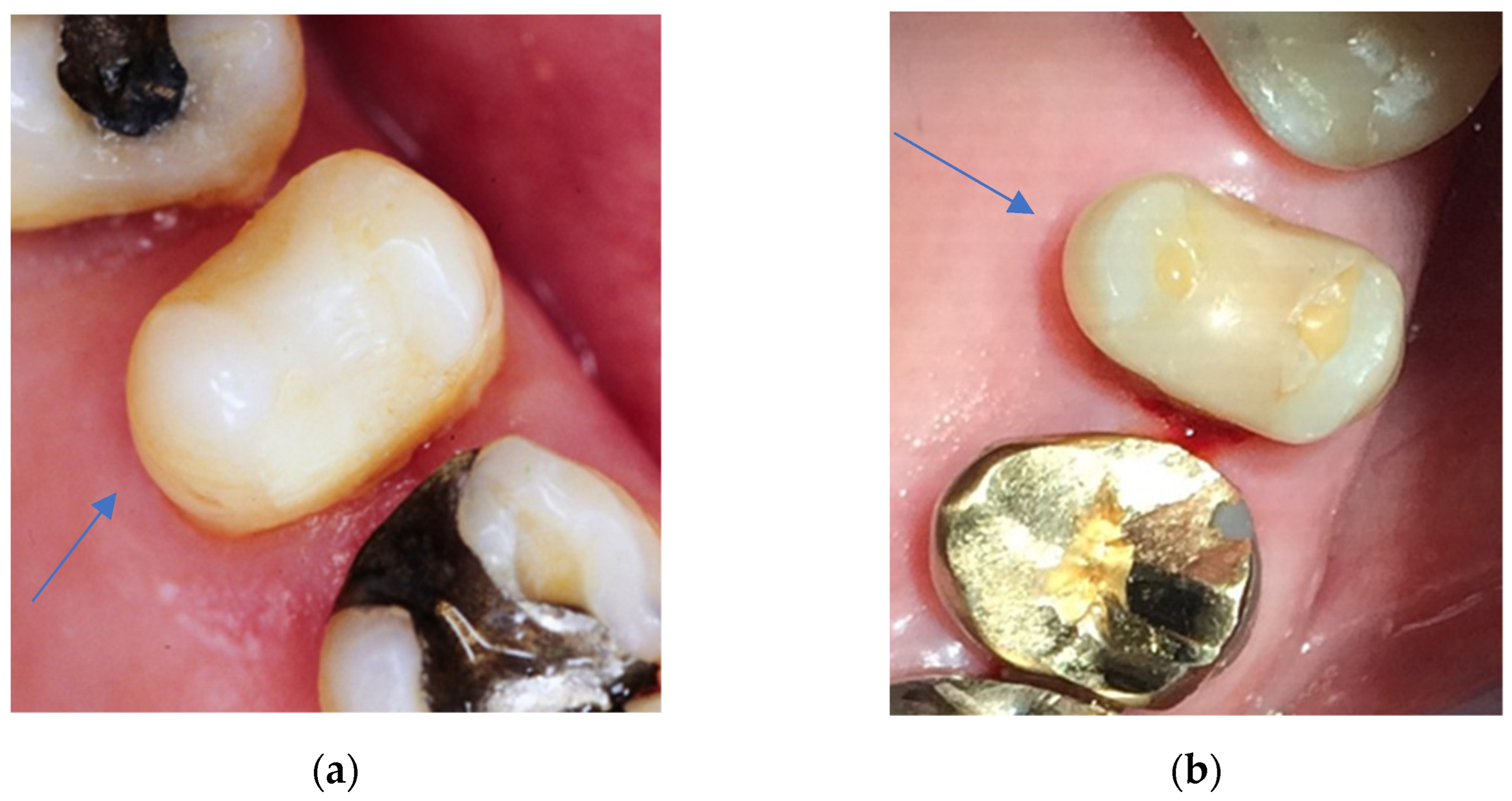
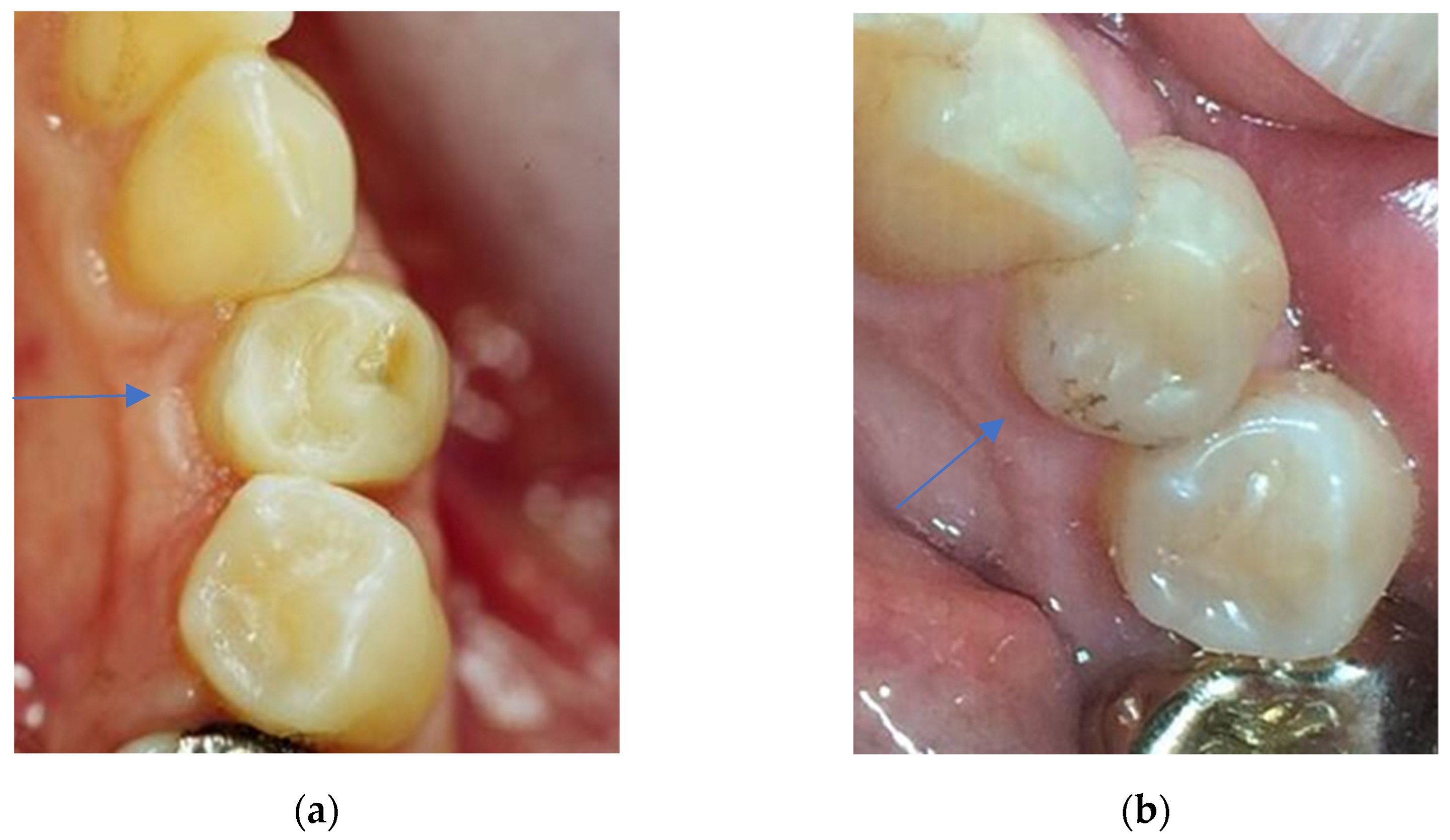
3.1.1. Aesthetic Properties
3.1.2. Functional Properties
3.1.3. Biological Properties
3.2. Comparison of Groups
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- van Dijken, J.W.V.; Pallesen, U. Posterior bulk-filled resin composite restorations: A 5-year randomized controlled clinical study. J. Dent. 2016, 51, 29–35. [Google Scholar] [CrossRef] [PubMed]
- Javaheri, D.S. Placement technique for direct posterior composite restorations. Pract. Proced. Aesthet. Dent. 2001, 13, 195–200. [Google Scholar] [PubMed]
- Krämer, N.; Reinelt, C.; Frankenberger, R. Ten-year Clinical Performance of Posterior Resin Composite Restorations. J. Adhes. Dent. 2015, 17, 433–441. [Google Scholar] [CrossRef] [PubMed]
- Ferracane, J.L. Is the wear of dental composites still a clinical concern? Is there still a need for in vitro wear simulating devices? Dent. Mater. 2006, 22, 689–692. [Google Scholar] [CrossRef] [PubMed]
- Opdam, N.J.M.; van de Sande, F.H.; Bronkhorst, E.; Cenci, M.S.; Bottenberg, P.; Pallesen, U.; Gaengler, P.; Lindberg, A.; Huysmans, M.C.D.N.J.M.; van Dijken, J.W. Longevity of posterior composite restorations: A systematic review and meta-analysis. J. Dent. Res. 2014, 93, 943–949. [Google Scholar] [CrossRef] [Green Version]
- Colson, D.G. A safe protocol for amalgam removal. J. Environ. Public Health 2012, 2012, 517391. [Google Scholar] [CrossRef]
- Rasines Alcaraz, M.G.; Veitz-Keenan, A.; Sahrmann, P.; Schmidlin, P.R.; Davis, D.; Iheozor-Ejiofor, Z. Direct composite resin fillings versus amalgam fillings for permanent or adult posterior teeth. Cochrane Database Syst. Rev. 2014, CD005620. [Google Scholar] [CrossRef] [Green Version]
- EUR-Lex Access to European Union law. Regulation (EU) 2017/852 of the European Parliament and of the Council of 17 May 2017 on mercury, and repealing Regulation (EC) No 1102/2008 (Text with EEA relevance). Available online: https://eur-lex.europa.eu/legal-content/EN/TXT/?uri=CELEX:32017R0852 (accessed on 21 December 2022).
- Sunnegårdh-Grönberg, K.; van Dijken, J.W.V.; Funegård, U.; Lindberg, A.; Nilsson, M. Selection of dental materials and longevity of replaced restorations in Public Dental Health clinics in northern Sweden. J. Dent. 2009, 37, 673–678. [Google Scholar] [CrossRef]
- Kopperud, S.E.; Tveit, A.B.; Gaarden, T.; Sandvik, L.; Espelid, I. Longevity of posterior dental restorations and reasons for failure. Eur. J. Oral Sci. 2012, 120, 539–548. [Google Scholar] [CrossRef]
- Kaleem, M.; Satterthwaite, J.D.; Watts, D.C. Effect of filler particle size and morphology on force/work parameters for stickiness of unset resin-composites. Dent. Mater. 2009, 25, 1585–1592. [Google Scholar] [CrossRef]
- Karabela, M.M.; Sideridou, I.D. Synthesis and study of properties of dental resin composites with different nanosilica particles size. Dent. Mater. 2011, 27, 825–835. [Google Scholar] [CrossRef] [PubMed]
- Gonçalves, F.; Kawano, Y.; Braga, R.R. Contraction stress related to composite inorganic content. Dent. Mater. 2010, 26, 704–709. [Google Scholar] [CrossRef] [PubMed]
- Da Rosa Rodolpho, P.A.; Donassollo, T.A.; Cenci, M.S.; Loguércio, A.D.; Moraes, R.R.; Bronkhorst, E.M.; Opdam, N.J.M.; Demarco, F.F. 22-Year clinical evaluation of the performance of two posterior composites with different filler characteristics. Dent. Mater. 2011, 27, 955–963. [Google Scholar] [CrossRef] [PubMed]
- Demarco, F.F.; Corrêa, M.B.; Cenci, M.S.; Moraes, R.R.; Opdam, N.J.M. Longevity of posterior composite restorations: Not only a matter of materials. Dent. Mater. 2012, 28, 87–101. [Google Scholar] [CrossRef] [PubMed]
- Ferracane, J.L. Resin composite—state of the art. Dent. Mater. 2011, 27, 29–38. [Google Scholar] [CrossRef]
- Alzraikat, H.; Burrow, M.F.; Maghaireh, G.A.; Taha, N.A. Nanofilled Resin Composite Properties and Clinical Performance: A Review. Oper. Dent. 2018, 43, E173–E190. [Google Scholar] [CrossRef]
- van Dijken, J.W.V.; Pallesen, U. A randomized 10-year prospective follow-up of Class II nanohybrid and conventional hybrid resin composite restorations. J. Adhes. Dent. 2014, 16, 585–592. [Google Scholar] [CrossRef]
- Palaniappan, S.; Bharadwaj, D.; Mattar, D.L.; Peumans, M.; van Meerbeek, B.; Lambrechts, P. Three-year randomized clinical trial to evaluate the clinical performance and wear of a nanocomposite versus a hybrid composite. Dent. Mater. 2009, 25, 1302–1314. [Google Scholar] [CrossRef]
- Laegreid, T.; Gjerdet, N.R.; Johansson, A.-K. Extensive composite molar restorations: 3 years clinical evaluation. Acta Odontol. Scand. 2012, 70, 344–352. [Google Scholar] [CrossRef]
- Opdam, N.J.M.; Bronkhorst, E.M.; Loomans, B.A.C.; Huysmans, M.C.D.N.J.M. 12-year survival of composite vs. amalgam restorations. J. Dent. Res. 2010, 89, 1063–1067. [Google Scholar] [CrossRef]
- van de Sande, F.H.; Opdam, N.J.; Rodolpho, P.A.D.R.; Correa, M.B.; Demarco, F.F.; Cenci, M.S. Patient risk factors’ influence on survival of posterior composites. J. Dent. Res. 2013, 92, 78S–83S. [Google Scholar] [CrossRef] [PubMed]
- Brantley, C.F.; Bader, J.D.; Shugars, D.A.; Nesbit, S.P. Does the cycle of rerestoration lead to larger restorations? J. Am. Dent. Assoc. 1995, 126, 1407–1413. [Google Scholar] [CrossRef] [PubMed]
- Lopes, G.C.; Vieira, L.C.C.; Araujo, E. Direct composite resin restorations: A review of some clinical procedures to achieve predictable results in posterior teeth. J. Esthet. Restor. Dent. 2004, 16, 19–31. [Google Scholar] [CrossRef] [PubMed]
- Manhart, J.; Chen, H.; Hamm, G.; Hickel, R. Buonocore Memorial Lecture. Review of the clinical survival of direct and indirect restorations in posterior teeth of the permanent dentition. Oper. Dent. 2004, 29, 481–508. [Google Scholar]
- Bayne, S.C.; Schmalz, G. Reprinting the classic article on USPHS evaluation methods for measuring the clinical research performance of restorative materials. Clin. Oral Investig. 2005, 9, 209–214. [Google Scholar] [CrossRef]
- Köhler, B.; Rasmusson, C.-G.; Ödman, P. A five-year clinical evaluation of Class II composite resin restorations. J. Dent. 2000, 28, 111–116. [Google Scholar] [CrossRef]
- Raskin, A.; Michotte-Theall, B.; Vreven, J.; Wilson, N.H.F. Clinical evaluation of a posterior composite 10-year report. J. Dent. 1999, 27, 13–19. [Google Scholar] [CrossRef]
- Nikaido, T.; Takada, T.; Kitasako, Y.; Ogata, M.; Shimada, Y.; Yoshikawa, T.; Nakajima, M.; Otsuki, M.; Tagami, J.; Burrow, M.F. Retrospective study of the 10-year clinical performance of direct resin composite restorations placed with the acid-etch technique. Quintessence Int. 2007, 38, e240–e246. [Google Scholar]
- Hickel, R.; Roulet, J.-F.; Bayne, S.; Heintze, S.D.; Mjör, I.A.; Peters, M.; Rousson, V.; Randall, R.; Schmalz, G.; Tyas, M.; et al. Recommendations for conducting controlled clinical studies of dental restorative materials. Clin. Oral Investig. 2007, 11, 5–33. [Google Scholar] [CrossRef]
- Marquillier, T.; Doméjean, S.; Le Clerc, J.; Chemla, F.; Gritsch, K.; Maurin, J.-C.; Millet, P.; Pérard, M.; Grosgogeat, B.; Dursun, E. The use of FDI criteria in clinical trials on direct dental restorations: A scoping review. J. Dent. 2018, 68, 1–9. [Google Scholar] [CrossRef]
- Hickel, R.; Peschke, A.; Tyas, M.; Mjör, I.; Bayne, S.; Peters, M.; Hiller, K.-A.; Randall, R.; Vanherle, G.; Heintze, S.D. FDI World Dental Federation: Clinical criteria for the evaluation of direct and indirect restorations-update and clinical examples. Clin. Oral Investig. 2010, 14, 349–366. [Google Scholar] [CrossRef] [PubMed]
- van Dijken, J.W.V. Durability of resin composite restorations in high C-factor cavities: A 12-year follow-up. J. Dent. 2010, 38, 469–474. [Google Scholar] [CrossRef] [PubMed]
- Pallesen, U.; Qvist, V. Composite resin fillings and inlays. An 11-year evaluation. Clin. Oral Investig. 2003, 7, 71–79. [Google Scholar] [CrossRef] [PubMed]
- Opdam, N.J.M.; Loomans, B.A.C.; Roeters, F.J.M.; Bronkhorst, E.M. Five-year clinical performance of posterior resin composite restorations placed by dental students. J. Dent. 2004, 32, 379–383. [Google Scholar] [CrossRef]
- Deliperi, S.; Bardwell, D.N. Clinical evaluation of direct cuspal coverage with posterior composite resin restorations. J. Esthet. Restor. Dent. 2006, 18, 256–265. [Google Scholar] [CrossRef]
- Heintze, S.D.; Rousson, V. Clinical effectiveness of direct class II restorations-a meta-analysis. J. Adhes. Dent. 2012, 14, 407–431. [Google Scholar] [CrossRef]
- Beck, F.; Lettner, S.; Graf, A.; Bitriol, B.; Dumitrescu, N.; Bauer, P.; Moritz, A.; Schedle, A. Survival of direct resin restorations in posterior teeth within a 19-year period (1996-2015): A meta-analysis of prospective studies. Dent. Mater. 2015, 31, 958–985. [Google Scholar] [CrossRef]
- Gerhardt-Szep, S.; Schröder-Schichtel, E.; Zücker, Q.; Zahn, T.; Feierabend, S.; Rüttermann, S. Problems of Direct Composite Posterior Restorations: A Clinical Study. J Dent Probl. Solut. 2016, 93, 35–39. [Google Scholar] [CrossRef] [Green Version]
- Vogl, V.; Hiller, K.-A.; Buchalla, W.; Federlin, M.; Schmalz, G. Controlled, prospective, randomized, clinical split-mouth evaluation of partial ceramic crowns luted with a new, universal adhesive system/resin cement: Results after 18 months. Clin. Oral Investig. 2016, 20, 2481–2492. [Google Scholar] [CrossRef]
- May, S.; Cieplik, F.; Hiller, K.-A.; Buchalla, W.; Federlin, M.; Schmalz, G. Flowable composites for restoration of non-carious cervical lesions: Three-year results. Dent. Mater. 2017, 33, e136–e145. [Google Scholar] [CrossRef]
- de Paula, E.A.; Tay, L.Y.; Kose, C.; Mena-Serrano, A.; Reis, A.; Perdigão, J.; Loguercio, A.D. Randomized clinical trial of four adhesion strategies in cervical lesions: 12-month results. Int. J. Esthet. Dent. 2015, 10, 122–145. [Google Scholar] [PubMed]
- Perdigão, J.; Kose, C.; Mena-Serrano, A.P.; de Paula, E.A.; Tay, L.Y.; Reis, A.; Loguercio, A.D. A new universal simplified adhesive: 18-month clinical evaluation. Oper. Dent. 2014, 39, 113–127. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cieplik, F.; Scholz, K.J.; Anthony, J.C.; Tabenski, I.; Ettenberger, S.; Hiller, K.-A.; Buchalla, W.; Federlin, M. One-year results of a novel self-adhesive bulk-fill restorative and a conventional bulk-fill composite in class II cavities-a randomized clinical split-mouth study. Clin. Oral Investig. 2022, 26, 449–461. [Google Scholar] [CrossRef] [PubMed]
- Calibration Tool E-Calib. E-Calib. Available online: www.e-calib.info (accessed on 30 December 2018).
- Saxer, U.P.; Mühlemann, H.R. Motivation und Aufklärung. SSO. Schweiz. Monatsschr. Zahnheilkd. 1975, 85, 905–919. [Google Scholar] [PubMed]
- van Dijken, J.W.V.; Lindberg, A. A 15-year randomized controlled study of a reduced shrinkage stress resin composite. Dent. Mater. 2015, 31, 1150–1158. [Google Scholar] [CrossRef] [PubMed]
- Lempel, E.; Tóth, Á.; Fábián, T.; Krajczár, K.; Szalma, J. Retrospective evaluation of posterior direct composite restorations: 10-year findings. Dent. Mater. 2015, 31, 115–122. [Google Scholar] [CrossRef]
- van de Sande, F.H.; Rodolpho, P.A.D.R.; Basso, G.R.; Patias, R.; da Rosa, Q.F.; Demarco, F.F.; Opdam, N.J.; Cenci, M.S. 18-year survival of posterior composite resin restorations with and without glass ionomer cement as base. Dent. Mater. 2015, 31, 669–675. [Google Scholar] [CrossRef]
- Burke, F.J.T.; Lucarotti, P.S.K.; Holder, R.L. Outcome of direct restorations placed within the general dental services in England and Wales (Part 2): Variation by patients’ characteristics. J. Dent. 2005, 33, 817–826. [Google Scholar] [CrossRef]
- Lucarotti, P.S.K.; Holder, R.L.; Burke, F.J.T. Outcome of direct restorations placed within the general dental services in England and Wales (Part 1): Variation by type of restoration and re-intervention. J. Dent. 2005, 33, 805–815. [Google Scholar] [CrossRef]
- Lucarotti, P.S.K.; Holder, R.L.; Burke, F.J.T. Outcome of direct restorations placed within the general dental services in England and Wales (Part 3): Variation by dentist factors. J. Dent. 2005, 33, 827–835. [Google Scholar] [CrossRef]
- Burke, F.J.T.; Lucarotti, P.S.K.; Holder, R. Outcome of direct restorations placed within the general dental services in England and Wales (Part 4): Influence of time and place. J. Dent. 2005, 33, 837–847. [Google Scholar] [CrossRef] [PubMed]
- Bogacki, R.E.; Hunt, R.J.; del Aguila, M.; Smith, W.R. Survival analysis of posterior restorations using an insurance claims database. Oper. Dent. 2002, 27, 488–492. [Google Scholar] [PubMed]
- Heintze, S.D.; Ilie, N.; Hickel, R.; Reis, A.; Loguercio, A.; Rousson, V. Laboratory mechanical parameters of composite resins and their relation to fractures and wear in clinical trials-A systematic review. Dent. Mater. 2017, 33, e101–e114. [Google Scholar] [CrossRef] [PubMed]
- Pallesen, U.; van Dijken, J.W.V. A randomized controlled 30 years follow up of three conventional resin composites in Class II restorations. Dent. Mater. 2015, 31, 1232–1244. [Google Scholar] [CrossRef] [PubMed]
- da Rosa Rodolpho, P.A.; Cenci, M.S.; Donassollo, T.A.; Loguércio, A.D.; Demarco, F.F. A clinical evaluation of posterior composite restorations: 17-year findings. J. Dent. 2006, 34, 427–435. [Google Scholar] [CrossRef] [PubMed]
- Pallesen, U.; van Dijken, J.W.V. A randomized controlled 27 years follow up of three resin composites in Class II restorations. J. Dent. 2015, 43, 1547–1558. [Google Scholar] [CrossRef]
- Ástvaldsdóttir, Á.; Dagerhamn, J.; van Dijken, J.W.V.; Naimi-Akbar, A.; Sandborgh-Englund, G.; Tranæus, S.; Nilsson, M. Longevity of posterior resin composite restorations in adults–A systematic review. J. Dent. 2015, 43, 934–954. [Google Scholar] [CrossRef]
- Frankenberger, R.; Reinelt, C.; Krämer, N. Nanohybrid vs. fine hybrid composite in extended class II cavities: 8-year results. Clin. Oral Investig. 2014, 18, 125–137. [Google Scholar] [CrossRef]
- van Dijken, J.W.V.; Pallesen, U. Eight-year randomized clinical evaluation of Class II nanohybrid resin composite restorations bonded with a one-step self-etch or a two-step etch-and-rinse adhesive. Clin. Oral Investig. 2015, 19, 1371–1379. [Google Scholar] [CrossRef]
- Loguercio, A.D.; Rezende, M.; Gutierrez, M.F.; Costa, T.F.; Armas-Vega, A.; Reis, A. Randomized 36-month follow-up of posterior bulk-filled resin composite restorations. J. Dent. 2019, 85, 93–102. [Google Scholar] [CrossRef]
- Nedeljkovic, I.; Teughels, W.; de Munck, J.; van Meerbeek, B.; van Landuyt, K.L. Is secondary caries with composites a material-based problem? Dent. Mater. 2015, 31, e247–e277. [Google Scholar] [CrossRef] [PubMed]
- Schneider, L.F.J.; Cavalcante, L.M.; Silikas, N. Shrinkage Stresses Generated during Resin-Composite Applications: A Review. J. Dent. Biomech. 2010, 2010, 131630. [Google Scholar] [CrossRef] [PubMed]
- da Veiga, A.M.A.; Cunha, A.C.; Ferreira, D.M.T.P.; da Silva Fidalgo, T.K.; Chianca, T.K.; Reis, K.R.; Maia, L.C. Longevity of direct and indirect resin composite restorations in permanent posterior teeth: A systematic review and meta-analysis. J. Dent. 2016, 54, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Dejak, B.; Młotkowski, A. A comparison of stresses in molar teeth restored with inlays and direct restorations, including polymerization shrinkage of composite resin and tooth loading during mastication. Dent. Mater. 2015, 31, e77–e87. [Google Scholar] [CrossRef]
- van Ende, A.; Mine, A.; de Munck, J.; Poitevin, A.; van Meerbeek, B. Bonding of low-shrinking composites in high C-factor cavities. J. Dent. 2012, 40, 295–303. [Google Scholar] [CrossRef]
- Pallesen, U.; van Dijken, J.W.V.; Halken, J.; Hallonsten, A.-L.; Höigaard, R. Longevity of posterior resin composite restorations in permanent teeth in Public Dental Health Service: A prospective 8 years follow up. J. Dent. 2013, 41, 297–306. [Google Scholar] [CrossRef]
- Palotie, U.; Eronen, A.K.; Vehkalahti, K.; Vehkalahti, M.M. Longevity of 2- and 3-surface restorations in posterior teeth of 25- to 30-year-olds attending Public Dental Service-A 13-year observation. J. Dent. 2017, 62, 13–17. [Google Scholar] [CrossRef] [Green Version]
- Borgia, E.; Baron, R.; Borgia, J.L. Quality and Survival of Direct Light-Activated Composite Resin Restorations in Posterior Teeth: A 5- to 20-Year Retrospective Longitudinal Study. J. Prosthodont. 2019, 28, e195–e203. [Google Scholar] [CrossRef] [Green Version]
- Batchelor, P.A.; Sheiham, A. Grouping of tooth surfaces by susceptibility to caries: A study in 5-16 year-old children. BMC Oral Health 2004, 4, 2. [Google Scholar] [CrossRef] [Green Version]
- Demarco, F.F.; Collares, K.; Correa, M.B.; Cenci, M.S.; Moraes, R.R.d.; Opdam, N.J. Should my composite restorations last forever? Why are they failing? Braz. Oral Res. 2017, 31, e56. [Google Scholar] [CrossRef] [Green Version]
- Laske, M.; Opdam, N.J.M.; Bronkhorst, E.M.; Braspenning, J.C.C.; Huysmans, M.C.D.N.J.M. Ten-Year Survival of Class II Restorations Placed by General Practitioners. JDR Clin. Trans. Res. 2016, 1, 292–299. [Google Scholar] [CrossRef] [PubMed]
- Laske, M.; Opdam, N.J.M.; Bronkhorst, E.M.; Braspenning, J.C.C.; Huysmans, M.C.D.N.J.M. Longevity of direct restorations in Dutch dental practices. Descriptive study out of a practice based research network. J. Dent. 2016, 46, 12–17. [Google Scholar] [CrossRef] [PubMed]
- Gordan, V.V.; Shen, C.; Riley, J.; Mjör, I.A. Two-year clinical evaluation of repair versus replacement of composite restorations. J. Esthet. Restor. Dent. 2006, 18, 144–153. [Google Scholar] [CrossRef] [PubMed]
- Kanzow, P.; Wiegand, A.; Schwendicke, F. Cost-effectiveness of repairing versus replacing composite or amalgam restorations. J. Dent. 2016, 54, 41–47. [Google Scholar] [CrossRef] [PubMed]


Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
von Gehren, M.O.; Rüttermann, S.; Romanos, G.E.; Herrmann, E.; Gerhardt-Szép, S. A 23-Year Observational Follow-Up Clinical Evaluation of Direct Posterior Composite Restorations. Dent. J. 2023, 11, 69. https://doi.org/10.3390/dj11030069
von Gehren MO, Rüttermann S, Romanos GE, Herrmann E, Gerhardt-Szép S. A 23-Year Observational Follow-Up Clinical Evaluation of Direct Posterior Composite Restorations. Dentistry Journal. 2023; 11(3):69. https://doi.org/10.3390/dj11030069
Chicago/Turabian Stylevon Gehren, Marie O., Stefan Rüttermann, Georgios E. Romanos, Eva Herrmann, and Susanne Gerhardt-Szép. 2023. "A 23-Year Observational Follow-Up Clinical Evaluation of Direct Posterior Composite Restorations" Dentistry Journal 11, no. 3: 69. https://doi.org/10.3390/dj11030069
APA Stylevon Gehren, M. O., Rüttermann, S., Romanos, G. E., Herrmann, E., & Gerhardt-Szép, S. (2023). A 23-Year Observational Follow-Up Clinical Evaluation of Direct Posterior Composite Restorations. Dentistry Journal, 11(3), 69. https://doi.org/10.3390/dj11030069






