Heat Treatment’s Vital Role: Elevating Orthodontic Mini-Implants for Superior Performance and Longevity—Pilot Study
Abstract
:1. Introduction
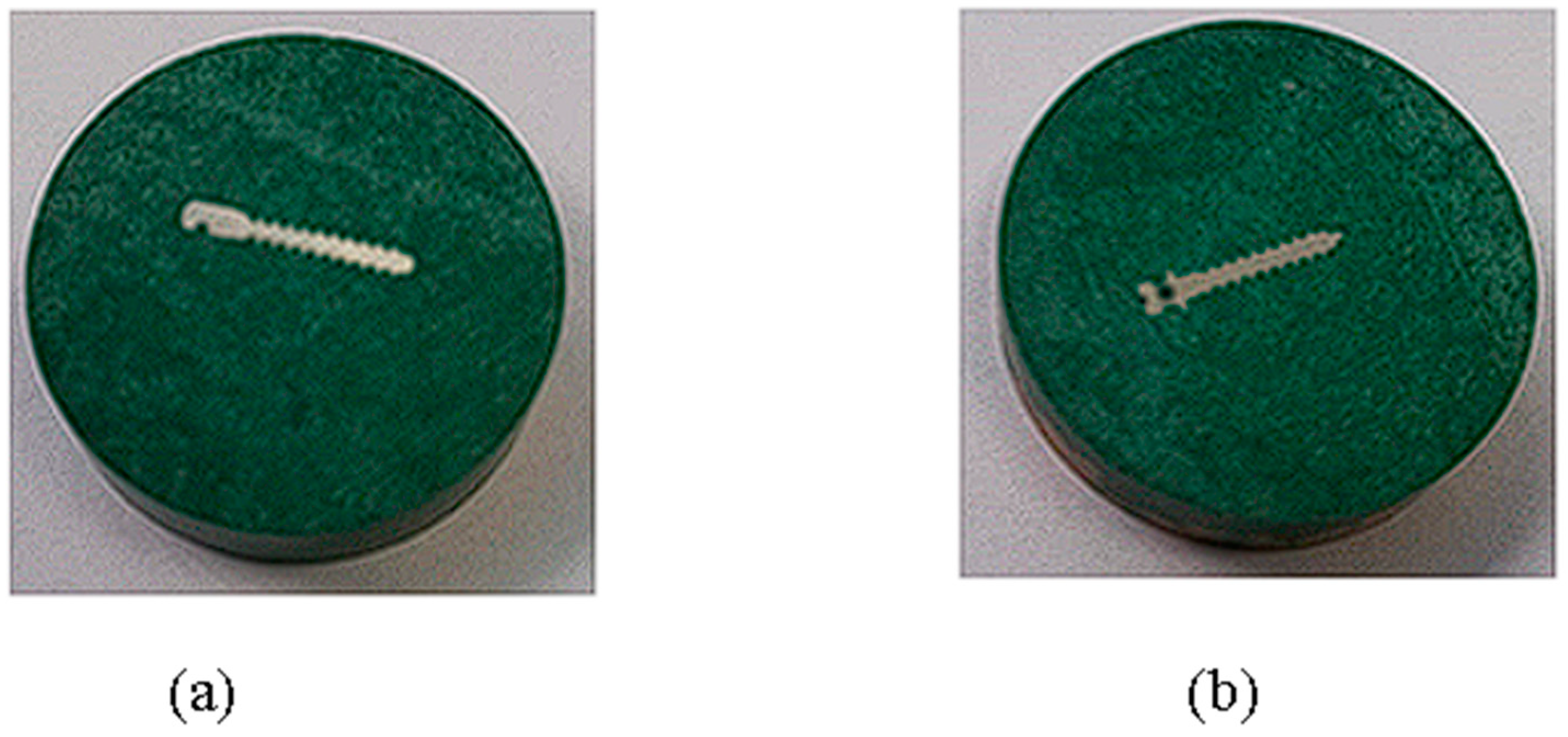
2. Materials and Methods
2.1. Study Design and Setting
2.2. Mechanical Procedure
2.3. Statistical Analysis
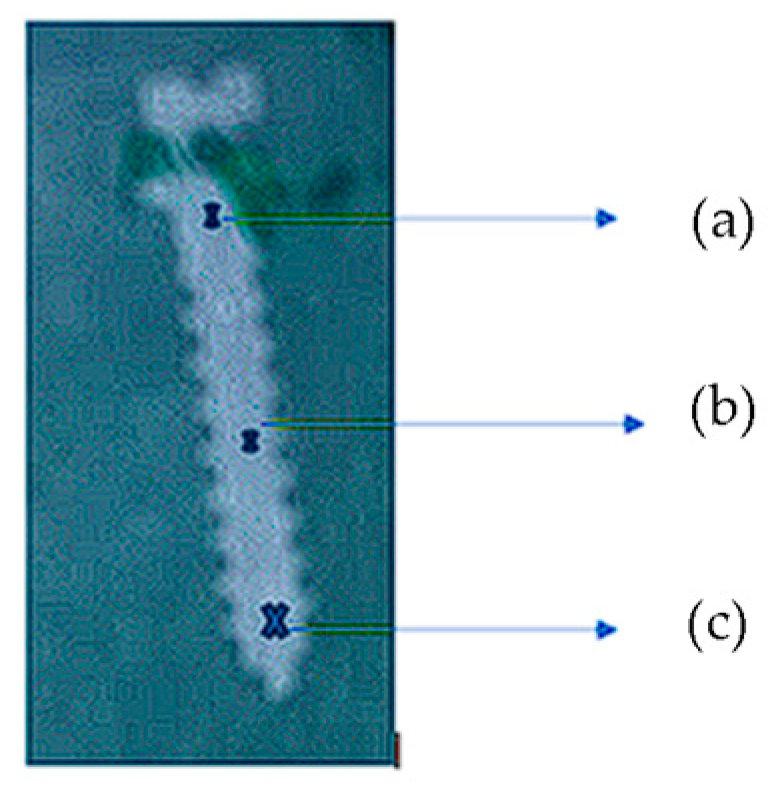
2.4. The Experimental Method Involves the Following Steps
- (a)
- Bringing an indenter with precisely defined geometry into contact with the sample under a known load and measuring the depth at which the indenter penetrates the sample;
- (b)
- Reducing the load after reaching a maximum value, followed by monitoring the withdrawal of the indenter;
- (c)
- Determining the elastic modulus of the sample by analyzing the load–unload curves and knowing the geometry of the indenter.
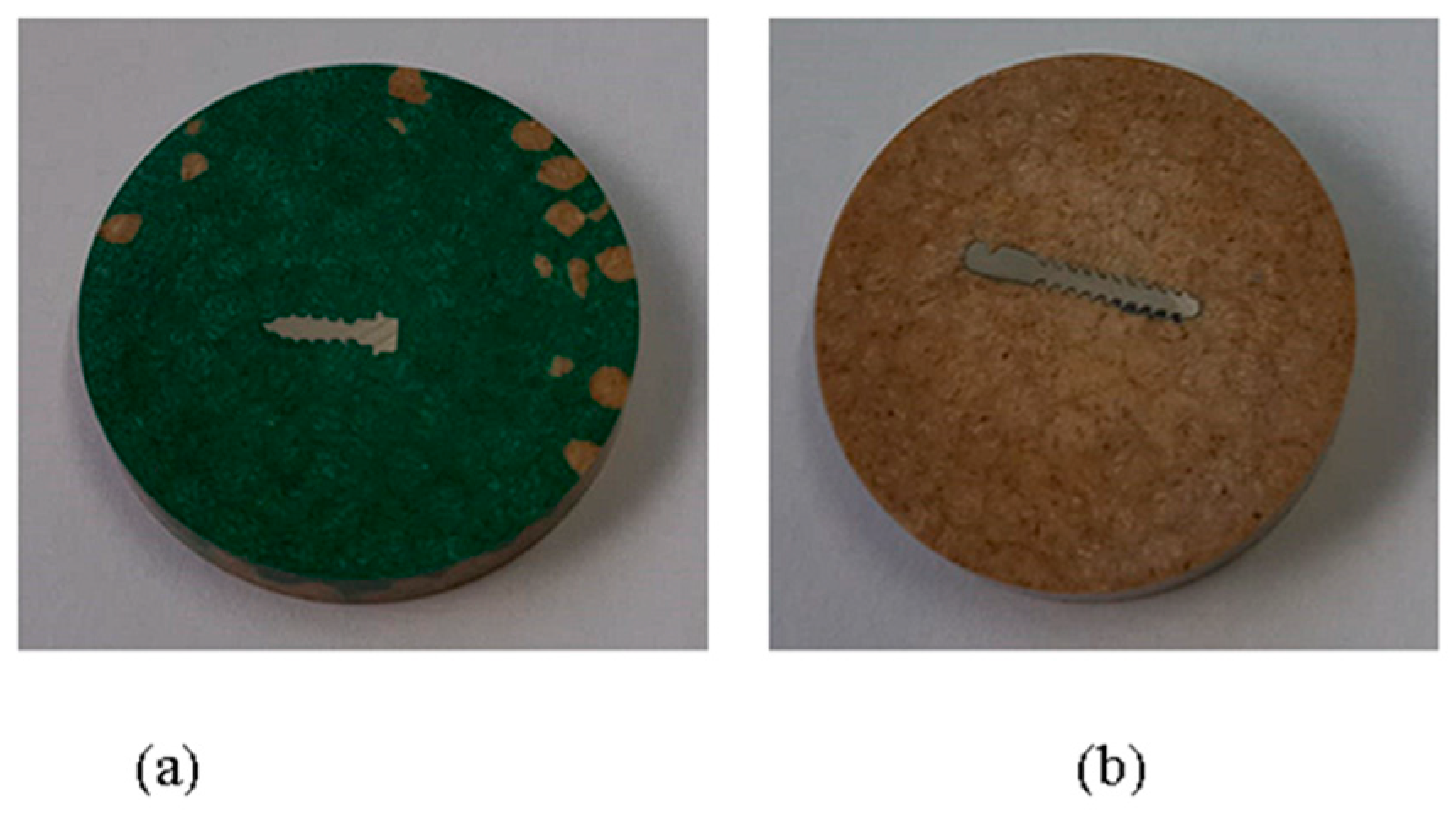
2.5. Modification of Properties through Heat Treatment
2.6. The Working Parameters Included
- (1)
- Heating the electric oven (Figure 5) to 890 °C;
- (2)
- Maintaining constant heat for 120 min;
- (3)
- Slow cooling of the mini implants;
- (4)
2.7. Advantages of the Working Method Include
- (1)
- High resolution: Microtribometers are capable of measuring at the nanometer scale, allowing for the precise characterization of the mechanical properties of materials on a small scale.
- (2)
- Versatile samples: This method can be applied to a wide variety of materials, including polymers, metals, ceramics, and composites.
- (3)
- Non-invasive: The indentation procedure is usually non-invasive, ensuring that the sample is not significantly destroyed or altered.
- (4)
- Speed: Tests can be performed in a relatively short period compared to other testing methods.
- (5)
- Flexibility: The elastic modulus, hardness, and other properties can be conveniently obtained through a single measurement.
3. Results
Sample Processing Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Chandak, A.M.; Tarvade, S.D.; Sharma, M.; Kaurani, H.J. In-vitro investigation of primary stability of orthodontic mini implants with different lengths using resonance frequency analysis. J. Contemp. Orthod. 2023, 6, 146–151. [Google Scholar] [CrossRef]
- Razaghi, P.; Haghgou, J.M.; Khazaei, S.; Farhadian, N.; Fekrazad, R.; Gholami, L. The effect of photobiomodulation therapy on the stability of orthodontic mini-implants in human and animal studies: A systematic review and meta-analysis. J. Lasers Med. Sci. 2022, 13, e27. [Google Scholar] [CrossRef]
- Hilloulin, B.; Lagrange, M.; Duvillard, M.; Garioud, G. ε-greedy automated indentation of cementitious materials for phase mechanical properties determination. Cem. Concr. Compos. 2022, 129, 104465. [Google Scholar] [CrossRef]
- Anbarasu, P.; Ramesh, B.; Annamalai, I.; Subramanian, S. Mini implant ‘safe zones’ in orthodontics: A comprehensive review. Arch. Dent. Res. 2022, 12, 9–18. [Google Scholar] [CrossRef]
- Migliorati, M.; Drago, S.; Amorfini, L.; Nucera, R.; Silvestrini-Biavati, A. Maximum insertion torque loss after miniscrew placement in orthodontic patients: A randomized controlled trial. Orthod. Craniofacial Res. 2020, 24, 386–395. [Google Scholar] [CrossRef]
- Wilmes, B.; Panayotidis, A.; Drescher, D. Fracture resistance of orthodontic mini-implants: A biomechanical in vitro study. Eur. J. Orthod. 2011, 33, 396–401. [Google Scholar] [CrossRef]
- Herrera, S.; Diez-Perez, A. Clinical experience with microindentation in vivo in humans. Bone 2017, 95, 175–182. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Q.; Le Roy, R.; Vandamme, M.; Zuber, B. Long-term creep properties of cementitious materials: Comparing microindentation testing with macroscopic uniaxial compressive testing. Cem. Concr. Res. 2014, 58, 89–98. [Google Scholar] [CrossRef]
- Arnold, M.; Zhao, S.; Ma, S.; Giuliani, F.; Hansen, U.; Cobb, J.P.; Abel, R.L.; Boughton, O. Microindentation—A tool for measuring cortical bone stiffness? Bone Jt. Res. 2017, 6, 542–549. [Google Scholar] [CrossRef]
- Ryu, J.-H.; Kwon, J.-S.; Jiang, H.B.; Cha, J.-Y.; Kim, K.-M. Effects of thermoforming on the physical and mechanical properties of thermoplastic materials for transparent orthodontic aligners. Korean J. Orthod. 2018, 48, 316–325. [Google Scholar] [CrossRef]
- Zysset, P.K. Indentation of bone tissue: A short review. Osteoporos. Int. 2009, 20, 1049–1055. [Google Scholar] [CrossRef] [PubMed]
- Parthasarathy, J.; Starly, B.; Raman, S.; Christensen, A. Mechanical evaluation of porous titanium (Ti6Al4V) structures with electron beam melting (EBM). J. Mech. Behav. Biomed. Mater. 2010, 3, 249–259. [Google Scholar] [CrossRef] [PubMed]
- Frost, H.M. A 2003 update of bone physiology and wolff’s law for clinicians. Angle Orthod. 2004, 74, 3–15. [Google Scholar] [CrossRef] [PubMed]
- He, R.; Gahlawat, S.; Guo, C.; Chen, S.; Dahal, T.; Zhang, H.; Liu, W.; Zhang, Q.; Chere, E.; White, K.; et al. Studies on mechanical properties of thermoelectric materials by nanoindentation. Phys. Status Solidi A 2015, 212, 2191–2195. [Google Scholar] [CrossRef]
- Ahmadi, M.; Karpat, Y.; Acar, O.; Kalay, Y.E. Microstructure effects on process outputs in micro scale milling of heat treated Ti6Al4V titanium alloys. J. Am. Acad. Dermatol. 2018, 252, 333–347. [Google Scholar] [CrossRef]
- Hasiak, M.; Sobieszczańska, B.; Łaszcz, A.; Biały, M.; Chęcmanowski, J.; Zatoński, T.; Bożemska, E.; Wawrzyńska, M. Production, mechanical properties and biomedical characterization of zrti-based bulk metallic glasses in comparison with 316L stainless steel and Ti6Al4V Alloy. Materials 2021, 15, 252. [Google Scholar] [CrossRef]
- Mierzejewska, Ż.A.; Hudák, R.; Sidun, J. Mechanical properties and microstructure of dmls TI6AL4V alloy dedicated to biomedical applications. Materials 2019, 12, 176. [Google Scholar] [CrossRef] [PubMed]
- Li, D.; Wang, J.; Chen, D.; Liang, P. Influence of molybdenum on tribo-corrosion behavior of 316l stainless steel in artificial saliva. J. Bio- Tribo-Corros. 2015, 1, 14. [Google Scholar] [CrossRef]
- He, Z.; He, H.; Lou, J.; Li, Y.; Li, D.; Chen, Y.; Liu, S. Fabrication, structure and mechanical and ultrasonic properties of medical TI6AL4V alloys part i: Microstructure and mechanical properties of TI6AL4V alloys suitable for ultrasonic scalpel. Materials 2020, 13, 478. [Google Scholar] [CrossRef]
- Dallago, M.; Fontanari, V.; Torresani, E.; Leoni, M.; Pederzolli, C.; Potrich, C.; Benedetti, M. Fatigue and biological properties of Ti-6Al-4V ELI cellular structures with variously arranged cubic cells made by selective laser melting. J. Mech. Behav. Biomed. Mater. 2018, 78, 381–394. [Google Scholar] [CrossRef]
- Redžepagić-Vražalica, L.; Mešić, E.; Pervan, N.; Hadžiabdić, V.; Delić, M.; Glušac, M. Impact of implant design and bone properties on the primary stability of orthodontic mini-implants. Appl. Sci. 2021, 11, 1183. [Google Scholar] [CrossRef]
- Prasadh, S.; Ratheesh, V.; Manakari, V.; Parande, G.; Gupta, M.; Wong, R. The potential of magnesium based materials in mandibular reconstruction. Metals 2019, 9, 302. [Google Scholar] [CrossRef]
- Anaya-Garza, K.; Domínguez-Crespo, M.A.; Torres-Huerta, A.; Palma-Ramírez, D.; Rodríguez-Salazar, A.E.; Ramírez-Meneses, E.; Brachetti-Sibaja, B. Electrochemical performance of uhmwpe biocompatible coatings on Ti6Al4V alloy in simulated body solutions: Influence of immersion time. ECS Trans. 2021, 101, 325–334. [Google Scholar] [CrossRef]
- Taran, V.; Garkusha, I.; Taran, A.; Muratov, R.; Vorontsov, P.; Gnidenko, Y.; Herasimov, H.; Starikov, V.; Baturin, A.; Romaniuk, S. Functional protective zrn coatings on implants for trauma surgery. Probl. At. Sci. Technol. 2020, 6, 115–118. [Google Scholar] [CrossRef]
- Baltatu, M.S.; Spataru, M.C.; Verestiuc, L.; Balan, V.; Solcan, C.; Sandu, A.V.; Geanta, V.; Voiculescu, I.; Vizureanu, P. Design, synthesis, and preliminary evaluation for Ti-Mo-Zr-Ta-Si alloys for potential implant applications. Materials 2021, 14, 6806. [Google Scholar] [CrossRef]
- Baltatu, I.; Sandu, A.V.; Vlad, M.D.; Spataru, M.C.; Vizureanu, P.; Baltatu, M.S. Mechanical characterization and in vitro assay of biocompatible titanium alloys. Micromachines 2022, 13, 430. [Google Scholar] [CrossRef]
- Baltatu, M.S.; Vizureanu, P.; Sandu, A.V.; Florido-Suarez, N.; Saceleanu, M.V.; Mirza-Rosca, J.C. New titanium alloys, promising materials for medical devices. Materials 2021, 14, 5934. [Google Scholar] [CrossRef]
- Guo, Y.; Chen, D.; Cheng, M.; Lu, W.; Wang, L.; Zhang, X. The bone tissue compatibility of a new Ti35Nb2Ta3Zr alloy with a low young’s modulus. Int. J. Mol. Med. 2013, 31, 689–697. [Google Scholar] [CrossRef]
- Essa, K.; Jamshidi, P.; Zou, J.; Attallah, M.M.; Hassanin, H. Porosity control in 316L stainless steel using cold and hot isostatic pressing. Mater. Des. 2018, 138, 21–29. [Google Scholar] [CrossRef]
- Raganya, L.; Moshokoa, N.; Machaka, R.; Obadele, B.; Makhatha, M. Microstructure and tensile properties of heat-treated Ti-Mo alloys. MATEC Web Conf. 2022, 370, 03007. [Google Scholar] [CrossRef]
- Piotrowski, B.; Baptista, A.; Patoor, E.; Bravetti, P.; Eberhardt, A.; Laheurte, P. Interaction of bone–dental implant with new ultra low modulus alloy using a numerical approach. Mater. Sci. Eng. C 2014, 38, 151–160. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.; Wang, J.; Wang, P.; Fan, X.; Li, X.; Fu, J.; Guo, Z. Low elastic modulus contributes to the osteointegration of ti-tanium alloy plug. J. Biomed. Mater. Res. Part B Appl. Biomater. 2012, 101B, 584–590. [Google Scholar] [CrossRef] [PubMed]
- Lekoadi, P.; Tlotleng, M.; Annan, K.; Maledi, N.; Masina, B. Evaluation of heat treatment parameters on microstructure and hardness properties of high-speed selective laser melted Ti6Al4V. Metals 2021, 11, 255. [Google Scholar] [CrossRef]
- Jebieshia, T.R.; Kim, J.M.; Kang, J.W.; Son, S.W.; Kim, H.D. Microstructural and very high cycle fatigue (vhcf) behavior of Ti6Al4V—A comparative study. Materials 2020, 13, 1948. [Google Scholar] [CrossRef] [PubMed]
- Lei, J.; Ge, Y.; Liu, T.; Wei, Z. Effects of heat treatment on the microstructure and mechanical properties of selective laser melting 316L stainless steel. Shock. Vib. 2021, 2021, 6547213. [Google Scholar] [CrossRef]
- Elangeswaran, C.; Cutolo, A.; Muralidharan, G.K.; de Formanoir, C.; Berto, F.; Vanmeensel, K.; Van Hooreweder, B. Effect of post-treatments on the fatigue behaviour of 316L stainless steel manufactured by laser powder bed fusion. Int. J. Fatigue 2019, 123, 31–39. [Google Scholar] [CrossRef]
- Peng, H.; Fang, W.; Dong, C.; Yi, Y.; Wei, X.; Luo, B.; Huang, S. Nano-mechanical properties and creep behavior of TI6AL4V fabricated by powder bed fusion electron beam additive manufacturing. Materials 2021, 14, 3004. [Google Scholar] [CrossRef]




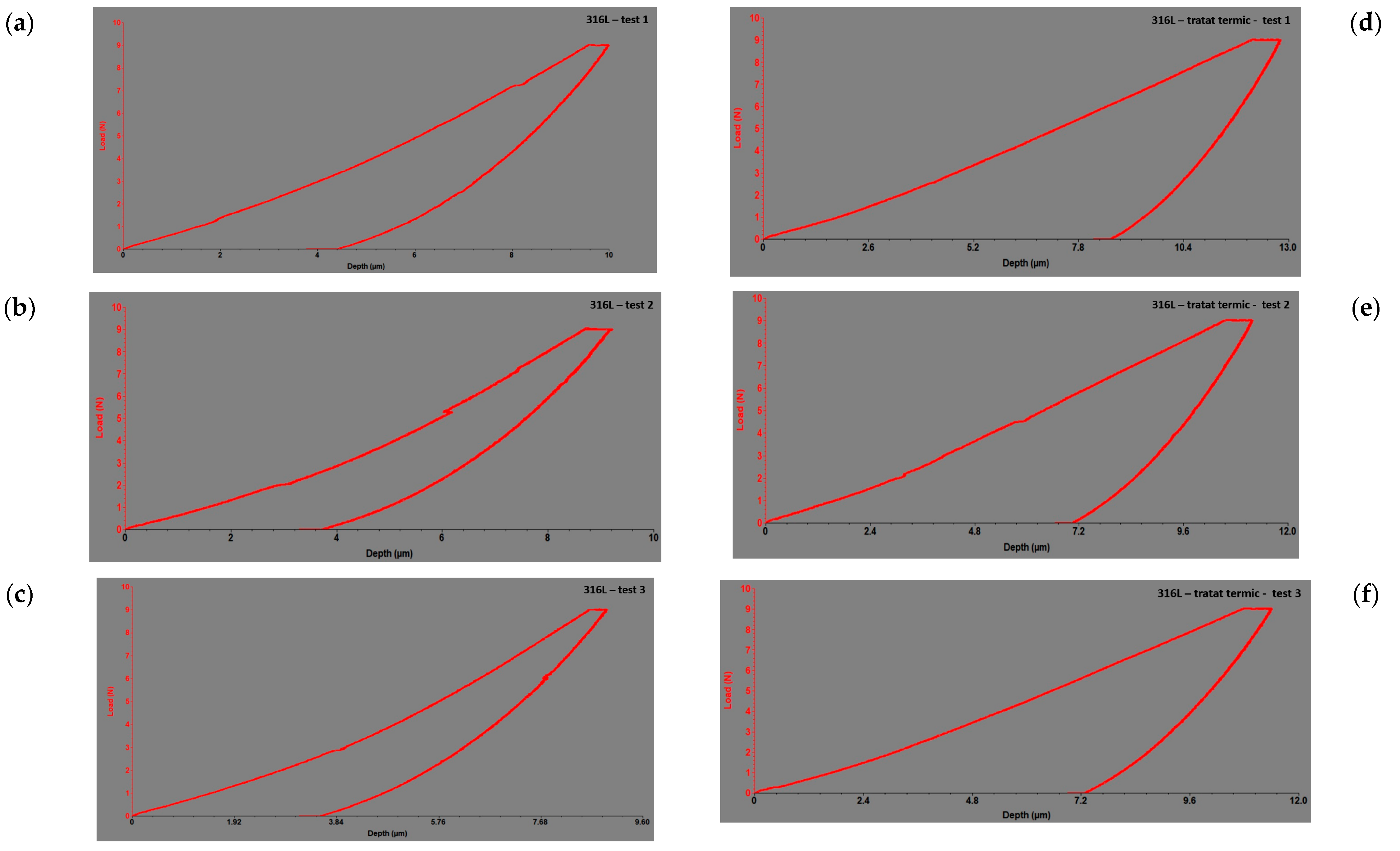
| Sample | Maximum Load Before [n] | Maximum Load After [n] | Maximum Displacement Before [µm] | Maximum Displacement After [µm] | Maximum Displacement Difference [µm] | Modulus of Elasticity Before [gpa] | Modulus of Elasticity After [gpa] | Modulus of Elasticity Difference [gpa] | Stiffness Before [n/µm] | Stiffness After [n/µm] | Stiffness Difference [n/µm] | Hardness Before [gpa] | Hardness After [gpa] | Hardness Difference [gpa] |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Group 1 TI6AL4V alloy | 4.50 | 4.50 | 8.22 | 9.21 | 0.99 | 105 | 76.81 | −28.19 | 1.554 | 0.91 | −0.644 | 2.06 | 2.45 | 0.39 |
| Group 2 316L | 4.50 | 4.50 | 6.62 | 7.54 | 0.92 | 210 | 157.87 | −52.13 | 2.074 | 1.93 | −0.144 | 0.87 | 0.63 | −0.24 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Panaite, T.; Savin, C.; Olteanu, N.D.; Karvelas, N.; Romanec, C.; Vieriu, R.-M.; Balcos, C.; Baltatu, M.S.; Benchea, M.; Achitei, D.; et al. Heat Treatment’s Vital Role: Elevating Orthodontic Mini-Implants for Superior Performance and Longevity—Pilot Study. Dent. J. 2024, 12, 103. https://doi.org/10.3390/dj12040103
Panaite T, Savin C, Olteanu ND, Karvelas N, Romanec C, Vieriu R-M, Balcos C, Baltatu MS, Benchea M, Achitei D, et al. Heat Treatment’s Vital Role: Elevating Orthodontic Mini-Implants for Superior Performance and Longevity—Pilot Study. Dentistry Journal. 2024; 12(4):103. https://doi.org/10.3390/dj12040103
Chicago/Turabian StylePanaite, Tinela, Carmen Savin, Nicolae Daniel Olteanu, Nikolaos Karvelas, Cristian Romanec, Raluca-Maria Vieriu, Carina Balcos, Madalina Simona Baltatu, Marcelin Benchea, Dragos Achitei, and et al. 2024. "Heat Treatment’s Vital Role: Elevating Orthodontic Mini-Implants for Superior Performance and Longevity—Pilot Study" Dentistry Journal 12, no. 4: 103. https://doi.org/10.3390/dj12040103






