Injectable Platelet-Rich Fibrin and Advanced Platelet-Rich Fibrin Demonstrate Enhanced Anti-Biofilm Effect Compared to Enamel Matrix Derivatives on Decontaminated Titanium Surfaces
Abstract
1. Introduction
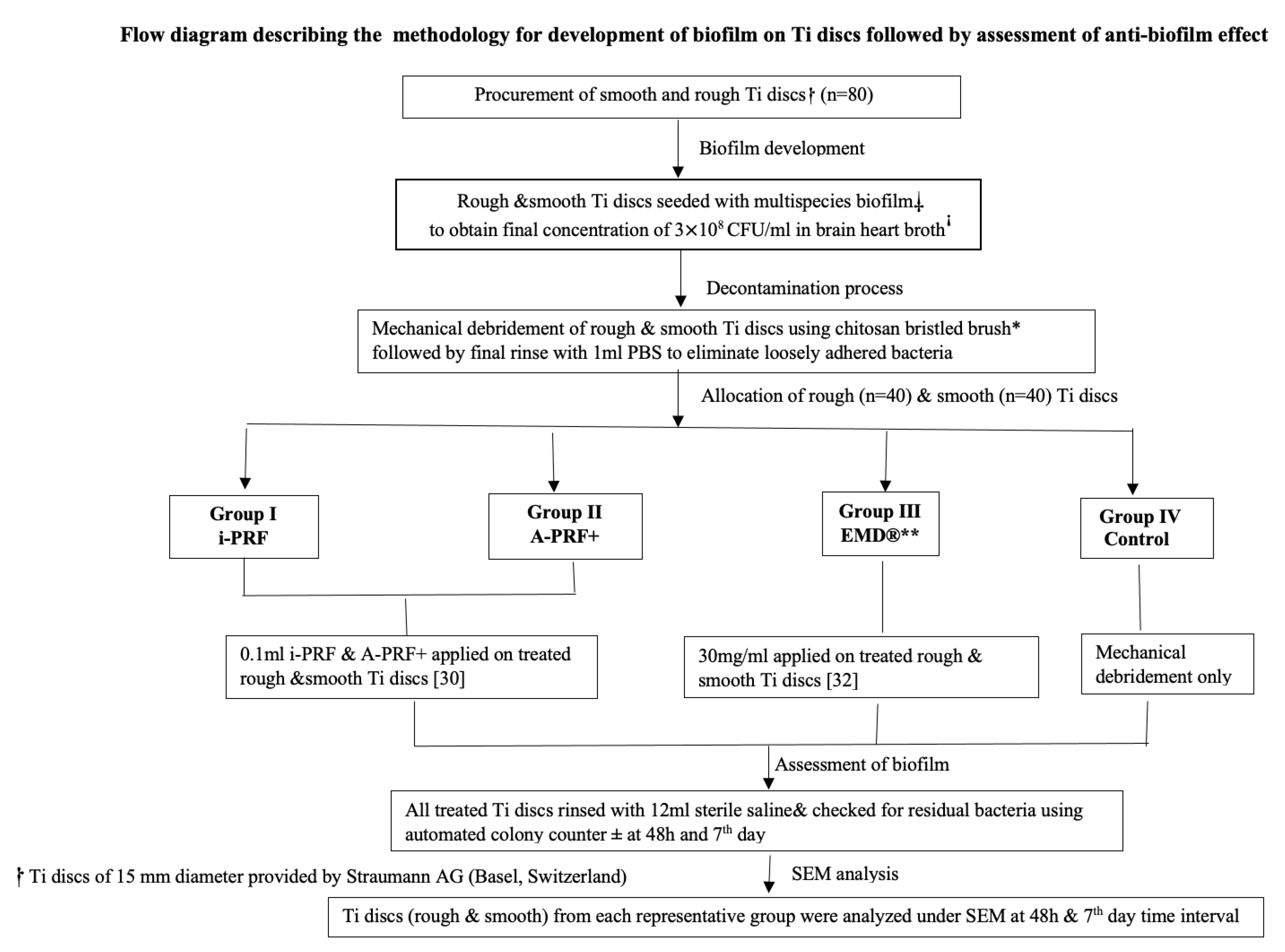
2. Materials and Methods
2.1. Development of Biofilm on Ti Discs
2.2. Automated Colony Counting for Microbial Colonies
2.3. Decontamination Process
2.4. Preparation of Biologic Constituents Required for the Study
2.5. Application of Experimental Agents
2.6. Statistical Analysis
3. Results
Description of Scanning Electron Microscopy (SEM) Images
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Albrektsson, T.; Isidor, F. Consensus report of session IV. In Proceedings of the First European Workshop on Periodontology; Lang, N.P., Karring, T., Eds.; Quintessence: London, UK, 1994; pp. 365–369. [Google Scholar]
- Berglundh, T.; Armitage, G.; Araujo, M.G.; Avila-Ortiz, G.; Blanco, J.; Camargo, P.M.; Chen, S.; Cochran, D.; Derks, J.; Figuero, E.; et al. Peri-implant diseases and conditions: Consensus report of workgroup 4 of the 2017 World Workshop on the Classification of Periodontal and Peri-Implant Diseases and Conditions. J. Clin. Periodontol. 2018, 45 (Suppl. S20), S286–S291. [Google Scholar] [CrossRef]
- Diaz, P.; Gonzalo, E.; Villagra, L.J.G.; Miegimolle, B.; Suarez, M.J. What is the prevalence of peri-implantitis? A systematic review and meta-analysis. BMC Oral Health 2022, 22, 449. [Google Scholar] [CrossRef]
- Renvert, S.; Polyzois, I.; Maguire, R. Re-osseointegration on previously contaminated surfaces: A systematic review. Clin. Oral Implant. Res. 2009, 20 (Suppl. S4), 216–227. [Google Scholar] [CrossRef]
- Charalampakis, G.; Ramberg, P.; Dahlén, G.; Berglundh, T.; Abrahamsson, I. Effect of cleansing of biofilm formed on titanium discs. Clin. Oral Implant. Res. 2015, 26, 931–936. [Google Scholar] [CrossRef]
- Boccia, G.; Di Spirito, F.; D’Ambrosio, F.; Di Palo, M.P.; Giordano, F.; Amato, M. Local and Systemic Antibiotics in Peri-Implantitis Management: An Umbrella Review. Antibiotics 2023, 12, 114. [Google Scholar] [CrossRef]
- Valderrama, P.; Wilson, T.G., Jr. Detoxification of implant surfaces affected by peri-implant disease: An overview of surgical methods. Int. J. Dent. 2013, 2013, 740680. [Google Scholar] [CrossRef]
- Subramani, K.; Wismeijer, D. Decontamination of titanium implant surface and re-osseointegration to treat peri-implantitis: A literature review. Int. J. Oral. Maxillofac. Implant. 2012, 27, 1043–1054. [Google Scholar]
- de Avila, E.D.; van Oirschot, B.A.; van den Beucken, J.J.J.P. Biomaterial-based possibilities for managing peri-implantitis. J. Periodontol. Res. 2020, 55, 165–173. [Google Scholar] [CrossRef]
- Sculean, A.; Windisch, P.; Szendroi-Kiss, D.; Horvath, A.; Rosta, P.; Becker, J.; Gera, I.; Schwarz, F. Clinical and histologic evaluation of an enamel matrix derivative combined with a biphasic calcium phosphate for the treatment of human intrabony periodontal defects. J. Periodontol. 2008, 79, 1991–1999. [Google Scholar] [CrossRef]
- Sculean, A.; Nikolidakis, D.; Nikou, G.; Ivanovic, A.; Chapple, I.L.; Stavropoulos, A. Biomaterials for promoting periodontal regeneration in human intrabony defects: A systematic review. Periodontol. 2000 2015, 68, 182–216. [Google Scholar] [CrossRef]
- Larsson, L.; Decker, A.M.; Nibali, L.; Pilipchuk, S.P.; Berglundh, T.; Giannobile, W.V. Regenerative medicine for periodontal and peri-implant diseases. J. Dent. Res. 2016, 95, 255–266. [Google Scholar] [CrossRef]
- Bosshardt, D.D. Biological mediators and periodontal regeneration: A review of enamel matrix proteins at the cellular and molecular levels. J. Clin. Periodontol. 2008, 35, 87–105. [Google Scholar] [CrossRef]
- Wennstrom, J.L.; Lindhe, J. Some effects of enamel matrix proteins on wound healing in the dento-gingival region. J. Clin. Periodontol. 2002, 29, 9–14. [Google Scholar] [CrossRef]
- Walter, C.; Jawor, P.; Bernimoulin, J.P.; Hagewald, S. Moderate effect of enamel matrix derivative (Emdogain Gel) on Porphyromonas gingivalis growth in vitro. Arch. Oral Biol. 2006, 51, 171–176. [Google Scholar] [CrossRef]
- Sculean, A.; Auschill, T.M.; Donos, N.; Brecx, M.; Arweiler, N.B. Effect of an enamel matrix protein derivative (Emdogain) on ex vivo dental plaque vitality. J. Clin. Periodontol. 2001, 28, 1074–1078. [Google Scholar] [CrossRef]
- Choukroun, J.; Adda, F.; Schoeffler, C.; Vervelle, A. Une opportunité en paro-implantologie: Le PRF. Implantodontie 2001, 42, e62. [Google Scholar]
- Owen, C.A.; Campbell, E.J. The cell biology of leukocyte-mediated proteolysis. J. Leukoc. Biol. 1999, 65, 137–150. [Google Scholar] [CrossRef]
- Davis, V.L.; Abukabda, A.B.; Radio, N.M.; Witt-Enderby, P.A.; Clafshenkel, W.P.; Cairone, J.V.; Rutkowski, J.L. Platelet-rich preparations to improve healing. Part II: Platelet activation and enrichment, leukocyte inclusion, and other selection criteria. J. Oral Implantol. 2014, 40, 511–521. [Google Scholar] [CrossRef]
- Marrelli, M.; Tatullo, M. Influence of PRF in the healing of bone and gingival tissues. Clinical and histological evaluations. Eur. Rev. Med. Pharmacol. Sci. 2013, 17, 1958–1962. [Google Scholar]
- Ghanaati, S.; Booms, P.; Orlowska, A.; Kubesch, A.; Lorenz, J.; Rutkowski, J.; Landes, C.; Sader, R.; Kirkpatrick, C.; Choukroun, J. Advanced platelet-rich fibrin: A new concept for cell-based tissue engineering by means of inflammatory cells. J. Oral Implantol. 2014, 40, 679–689. [Google Scholar] [CrossRef]
- Wang, X.; Zhang, Y.; Choukroun, J.; Ghanaati, S.; Miron, R.J. Behavior of Gingival Fibroblasts on Titanium Implant Surfaces in Combination with either Injectable-PRF or PRP. Int. J. Mol. Sci. 2017, 18, 331. [Google Scholar] [CrossRef]
- Miron, R.J.; Fujioka-Kobayashi, M.; Hernandez, M.; Kandalam, U.; Zhang, Y.; Ghanaati, S.; Choukroun, J. Injectable platelet rich fibrin (i-PRF): Opportunities in regenerative dentistry? Clin. Oral Investig. 2017, 21, 2619–2627. [Google Scholar] [CrossRef]
- Schuldt, L.; Bi, J.; Owen, G.; Shen, Y.; Haapasalo, M.; Häkkinen, L.; Larjava, H. Decontamination of rough implant surfaces colonized by multispecies oral biofilm by application of leukocyte- and platelet-rich fibrin. J. Periodontol. 2021, 92, 875–885. [Google Scholar] [CrossRef]
- Balaji, V.; Thiagarajan, R.; Niazi, T.; Ulaganathan, G.; Manikandan, D. Antimicrobial effects of platelet rich fibrin: A systematic review on current evidence of research. J. Interdiscip. Dent. 2021, 11, 2–11. [Google Scholar] [CrossRef]
- Shen, Y.; Qian, W.; Chung, C.; Olsen, I.; Haapasalo, M. Evaluation of the effect of two chlorhexidine preparations on biofilm bacteria in vitro: A three-dimensional quantitative analysis. J. Endod. 2009, 35, 981–985. [Google Scholar] [CrossRef]
- Fujioka-Kobayashi, M.; Miron, R.J.; Hernandez, M.; Kandalam, U.; Zhang, Y.; Choukroun, J. Optimized platelet rich fibrin with the low speed concept: Growth factor release, biocompatibility and cellular response. J. Periodontol. 2017, 88, 112–121. [Google Scholar] [CrossRef]
- Pitzurra, L.; Jansen, I.D.C.; de Vries, T.J.; Hoogenkamp, M.A.; Loos, B.G. Effects of L-PRF and A-PRF+ on periodontal fibroblasts in in vitro wound healing experiments. J. Periodontol. Res. 2020, 55, 287–295. [Google Scholar] [CrossRef]
- Dohan, D.M.; Choukroun, J.; Diss, A.; Dohan, S.L.; Dohan, A.J.; Mouhyi, J.; Gogly, B. Platelet-rich fibrin (PRF): A second-generation platelet concentrate. Part I: Technological concepts and evolution. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 2006, 101, e37–e44. [Google Scholar] [CrossRef]
- Karde, P.A.; Sethi, K.S.; Mahale, S.A.; Khedka, S.U.; Patil, A.G.; Joshi, C.P. Comparative evaluation of platelet count and antimicrobial efficacy of injectable platelet-rich fibrin with other platelet concentrates: An in vitro study. J. Indian Soc. Periodontol. 2017, 21, 97–101. [Google Scholar] [CrossRef]
- Miron, R.J.; Bosshardt, D.D.; Hedbom, E.; Zhang, Y.; Haenni, B.; Buser, D.; Sculean, A. Adsorption of enamel matrix proteins to a bovine-derived bone grafting material and its regulation of cell adhesion, proliferation, and differentiation. J. Periodontol. 2012, 83, 936–947. [Google Scholar] [CrossRef]
- Ramenzoni, L.L.; Bösch, A.; Proksch, S.; Attin, T.; Schmidlin, P.R. Effect of high glucose levels and lipopolysaccharides-induced inflammation on osteoblast mineralization over sandblasted/acid-etched titanium surface. Clin. Implant. Dent. Relat. Res. 2020, 22, 213–219. [Google Scholar] [CrossRef]
- Jasmine, S.; Tangavelu, A.; Janarthanan, K.; Krishnamoorthy, R.; Alshatwi, A. A Antimicrobial and anti-bioflm potential of injectable platelet rich fibrin- a second generation platelet concentrate-against bioflm producing oral staphylococcus isolates. Saudi J. Biol. Sci. 2020, 27, 41–46. [Google Scholar] [CrossRef]
- Kobayashi, E.; Flückiger, L.; Fujioka-Kobayashi, M.; Sawada, K.; Sculean, A.; Schaller, B.; Miron, R.J. Comparative release of growth factors from PRP, PRF, and advanced-PRF. Clin. Oral. Investig. 2016, 20, 2353–2360. [Google Scholar] [CrossRef]
- Kour, P.; Pudakalkatti, P.S.; Vas, A.M.; Das, S.; Padmanabhan, S. Comparative evaluation of antimicrobial efficacy of platelet-rich plasma, platelet-rich fibrin, and injectable platelet-rich fibrin on the standard strains of porphyromonas gingivalis and aggregatibacter actinomycetemcomitans. Contemp. Clin. Dent. 2018, 9, s325–s330. [Google Scholar] [CrossRef]
- Ravi, S.; Santhanakrishnan, M. Mechanical, chemical, structural analysis and comparative release of PDGF-AA from L-PRF, A-PRF and T-PRF—An in vitro study. Biomater. Res. 2020, 24, 16. [Google Scholar] [CrossRef]
- Pham, T.A.V. Comparison of Antimicrobial Activity against Porphyromonas gingivalis between Advanced Platelet-Rich Fibrin and Injectable Platelet-Rich Fibrin. Int. J. Biomater. 2023, 27, 9194868. [Google Scholar] [CrossRef]
- Katariya, C. Comparative Evaluation of Antimicrobial Efficacy Among Various Generations of PRF from a Systemically Healthy Population-An In Vitro Study. Int. J. Dent. Oral Sci. 2021, 16, 3801–3804. [Google Scholar] [CrossRef]
- Spahr, A.; Lyngstadaas, S.P.; Boeckh, C.; Andersson, C.; Podbielski, A.; Haller, B. Effect of the enamel matrix derivative Emdogain on the growth of periodontal pathogens in vitro. J. Clin. Periodontol. 2002, 29, 62–72. [Google Scholar] [CrossRef]
- Dostie, S.; Alkadi, L.T.; Owen, G.; Bi, J.; Shen, Y.; Haapasalo, M.; Larjava, H.S. Chemotherapeutic decontamination of dental implants colonized by mature multispecies oral biofilm. J. Clin. Periodontol. 2017, 44, 403–409. [Google Scholar] [CrossRef]
- Miller, C.H.; Rice, A.S.; Garrett, K.; Stein, S.F. Gender, race and diet affect platelet function tests in normal subjects, contributing to a high rate of abnormal results. Br. J. Haematol. 2014, 165, 842–853. [Google Scholar] [CrossRef]

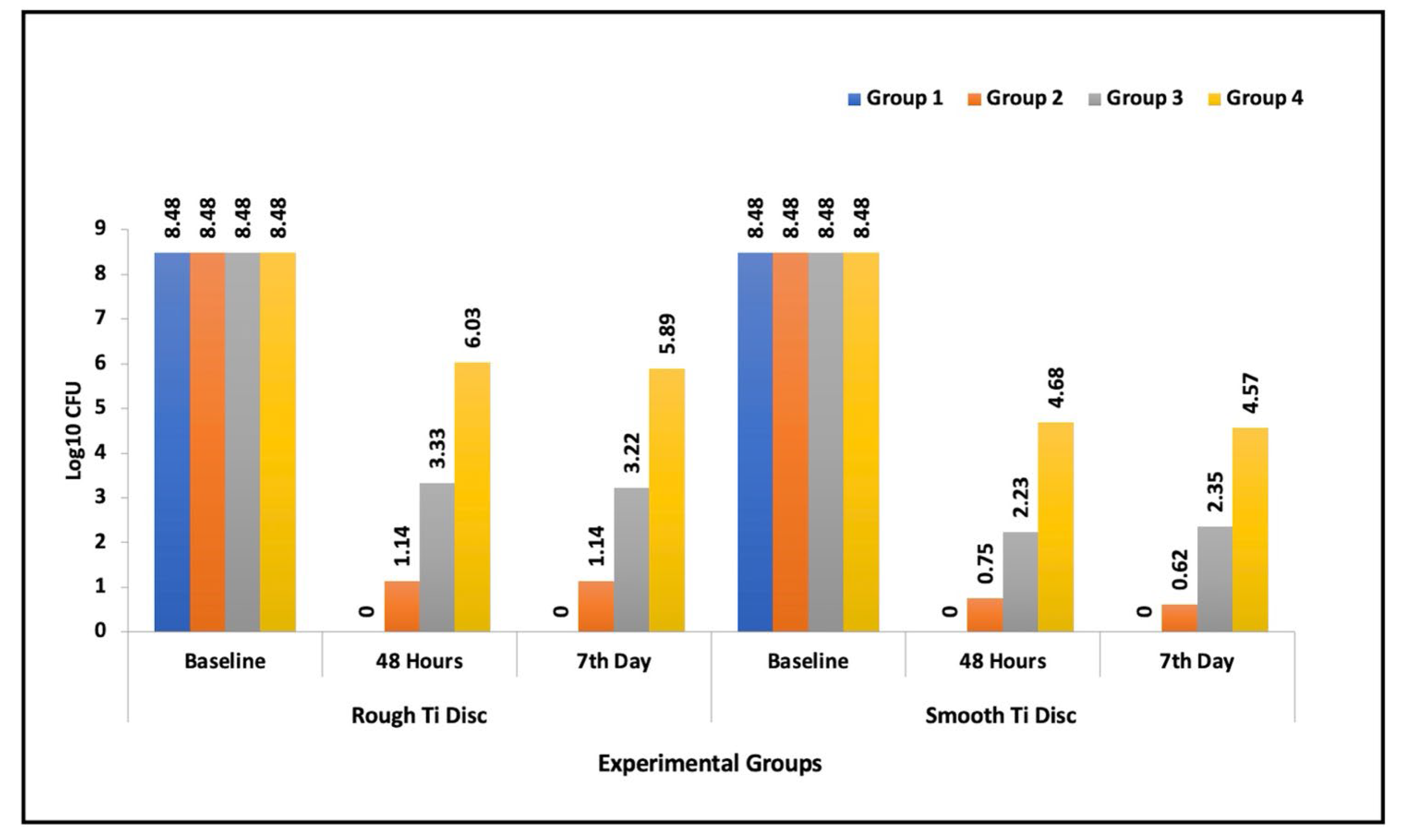
| Group | N | Mean | SD | Min | Max | Percentiles | Kruskal–Wallis Test | |||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Q1 | Median | Q3 | Chi Square Value | p-Value | ||||||||
| Rough Ti discs | Baseline | I | 10 | 8.48 | 0 | 8.48 | 8.48 | 8.48 | 8.48 | 8.48 | 0 | 1.00 (NS) |
| II | 10 | 8.48 | 0 | 8.48 | 8.48 | 8.48 | 8.48 | 8.48 | ||||
| III | 10 | 8.48 | 0 | 8.48 | 8.48 | 8.48 | 8.48 | 8.48 | ||||
| IV | 10 | 8.48 | 0 | 8.48 | 8.48 | 8.48 | 8.48 | 8.48 | ||||
| 48 h | I | 10 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 37.26 | <0.001 * | |
| II | 10 | 1.14 | 0.26 | 0.85 | 1.60 | 0.98 | 1.00 | 1.35 | ||||
| III | 10 | 3.33 | 0.46 | 2.30 | 3.90 | 3.00 | 3.48 | 3.65 | ||||
| IV | 10 | 6.03 | 0.69 | 5.00 | 6.78 | 5.30 | 6.30 | 6.60 | ||||
| 7 day | I | 10 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 37.34 | <0.001 * | |
| II | 10 | 1.14 | 0.19 | 1.00 | 1.48 | 1.00 | 1.00 | 1.30 | ||||
| III | 10 | 3.22 | 0.68 | 2.00 | 3.78 | 2.75 | 3.48 | 3.65 | ||||
| IV | 10 | 5.89 | 0.47 | 5.48 | 6.78 | 5.48 | 5.74 | 6.15 | ||||
| Smooth Ti discs | Baseline | I | 10 | 8.48 | 0 | 8.48 | 8.48 | 8.48 | 8.48 | 8.48 | 0 | 1.00 (NS) |
| II | 10 | 8.48 | 0 | 8.48 | 8.48 | 8.48 | 8.48 | 8.48 | ||||
| III | 10 | 8.48 | 0 | 8.48 | 8.48 | 8.48 | 8.48 | 8.48 | ||||
| IV | 10 | 8.48 | 0 | 8.48 | 8.48 | 8.48 | 8.48 | 8.48 | ||||
| 48 h | I | 10 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 30.04 | <0.001 * | |
| II | 10 | 0.75 | 0.69 | 0 | 1.78 | 0 | 0.95 | 1.35 | ||||
| III | 10 | 2.23 | 0.44 | 1.48 | 3.00 | 2.00 | 2.15 | 2.55 | ||||
| IV | 10 | 4.68 | 1.90 | 0 | 6.78 | 4.18 | 5.15 | 5.78 | ||||
| 7 day | I | 10 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 30.39 | <0.001 * | |
| II | 10 | 0.62 | 0.54 | 0 | 1.30 | 0 | 0.95 | 1.00 | ||||
| III | 10 | 2.35 | 0.34 | 2 | 2.95 | 2.00 | 2.39 | 2.60 | ||||
| IV | 10 | 4.57 | 1.73 | 0 | 5.60 | 4.45 | 5.00 | 5.60 | ||||
| Groups | Rough Ti Discs | Smooth Ti Discs | |||
|---|---|---|---|---|---|
| U Statistic | p-Value | U Statistic | p-Value | ||
| Baseline | I vs. II | 50 | 1.00 (NS) | 50 | 1.00 (NS) |
| I vs. III | 50 | 1.00 (NS) | 50 | 1.00 (NS) | |
| I vs. IV | 50 | 1.00 (NS) | 50 | 1.00 (NS) | |
| II vs. III | 50 | 1.00 (NS) | 50 | 1.00 (NS) | |
| II vs. IV | 50 | 1.00 (NS) | 50 | 1.00 (NS) | |
| III vs. IV | 50 | 1.00 (NS) | 50 | 1.00 (NS) | |
| 48 h | I vs. II | 0 | <0.001 * | 20 | 0.03 * |
| I vs. III | 0 | <0.001 * | 0 | <0.001 * | |
| I vs. IV | 0 | <0.001 * | 5 | <0.001 * | |
| II vs. III | 0 | <0.001 * | 1.5 | <0.001 * | |
| II vs. IV | 0 | <0.001 * | 8 | 0.006 * | |
| III vs. IV | 0 | <0.001 * | 10 | 0.012 * | |
| 7 day | I vs. II | 0 | <0.001 * | 20 | 0.03 * |
| I vs. III | 0 | <0.001 * | 0 | <0.001 * | |
| I vs. IV | 0 | <0.001 * | 5 | <0.001 * | |
| II vs. III | 0 | <0.001 * | 0 | <0.001 * | |
| II vs. IV | 0 | <0.001 * | 8 | 0.006 * | |
| III vs. IV | 0 | <0.001 * | 10 | 0.012 * | |
| Group | 48 h—Baseline | Day 7—Baseline | Day 7—48 h | ||
|---|---|---|---|---|---|
| Rough Ti discs | I | Z | −3.16 | −3.16 | 0 |
| p-value | 0.006 * | 0.006 * | 1.00 (NS) | ||
| II | Z | −2.82 | −2.88 | −0.14 | |
| p-value | 0.02 * | 0.01 * | 0.89 (NS) | ||
| III | Z | −2.81 | −2.82 * | −0.24 | |
| p-value | 0.02 * | 0.02 * | 0.81 (NS) | ||
| IV | Z | −2.82 | −2.81 | −0.67 | |
| p-value | 0.02 * | 0.02 * | 0.51 (NS) | ||
| Smooth Ti discs | I | Z | −3.16 | −3.16 | 0 |
| p-value | 0.006 * | 0.006 * | 1.00 (NS) | ||
| II | Z | −2.82 | −2.84 | −1.75 | |
| p-value | 0.02 * | 0.02 * | 0.08 (NS) | ||
| III | Z | −2.82 | −2.83 | −0.85 | |
| p-value | 0.02 * | 0.02 * | 0.40 (NS) | ||
| IV | Z | −2.81 | −2.83 | −0.30 | |
| p-value | 0.02 * | 0.02 * | 0.77 (NS) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Varghese, J.; Ramenzoni, L.L.; Shenoy, P.A.; Schmidlin, P.R.; Mehrotra, S.; Kamath, V. Injectable Platelet-Rich Fibrin and Advanced Platelet-Rich Fibrin Demonstrate Enhanced Anti-Biofilm Effect Compared to Enamel Matrix Derivatives on Decontaminated Titanium Surfaces. Dent. J. 2024, 12, 175. https://doi.org/10.3390/dj12060175
Varghese J, Ramenzoni LL, Shenoy PA, Schmidlin PR, Mehrotra S, Kamath V. Injectable Platelet-Rich Fibrin and Advanced Platelet-Rich Fibrin Demonstrate Enhanced Anti-Biofilm Effect Compared to Enamel Matrix Derivatives on Decontaminated Titanium Surfaces. Dentistry Journal. 2024; 12(6):175. https://doi.org/10.3390/dj12060175
Chicago/Turabian StyleVarghese, Jothi, Liza L. Ramenzoni, Padmaja A. Shenoy, Patrick R. Schmidlin, Shubhankar Mehrotra, and Vinayak Kamath. 2024. "Injectable Platelet-Rich Fibrin and Advanced Platelet-Rich Fibrin Demonstrate Enhanced Anti-Biofilm Effect Compared to Enamel Matrix Derivatives on Decontaminated Titanium Surfaces" Dentistry Journal 12, no. 6: 175. https://doi.org/10.3390/dj12060175
APA StyleVarghese, J., Ramenzoni, L. L., Shenoy, P. A., Schmidlin, P. R., Mehrotra, S., & Kamath, V. (2024). Injectable Platelet-Rich Fibrin and Advanced Platelet-Rich Fibrin Demonstrate Enhanced Anti-Biofilm Effect Compared to Enamel Matrix Derivatives on Decontaminated Titanium Surfaces. Dentistry Journal, 12(6), 175. https://doi.org/10.3390/dj12060175






