Efficacy of the Sausage Technique in Rebuilding the Crestal Buccal Bone Thickness: A Retrospective Analysis
Abstract
1. Introduction
2. Materials and Methods
2.1. Inclusion Criteria
2.2. Exclusion Criteria
2.3. Clinical Protocol
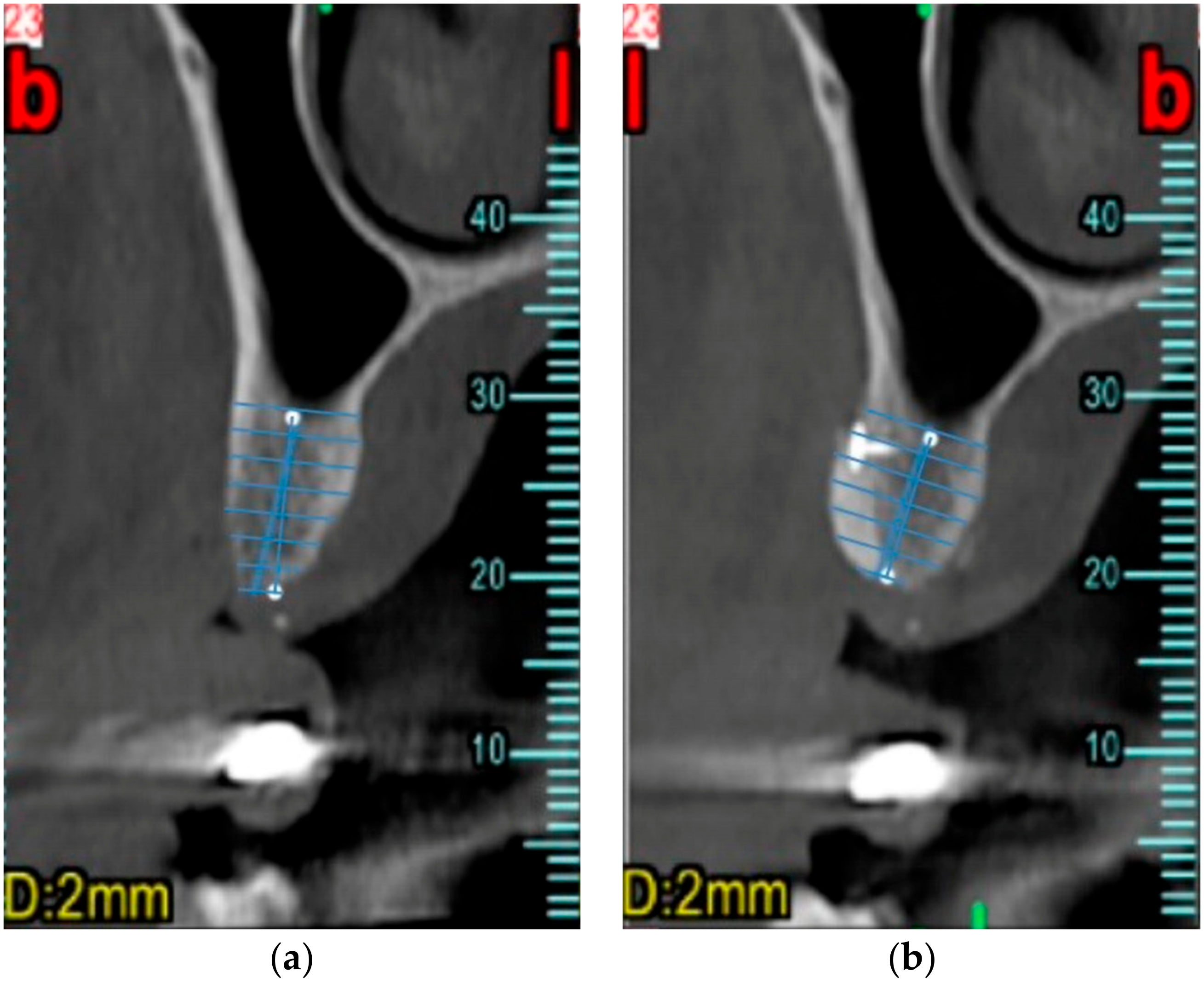
2.4. Data Collection
2.5. Data Analysis
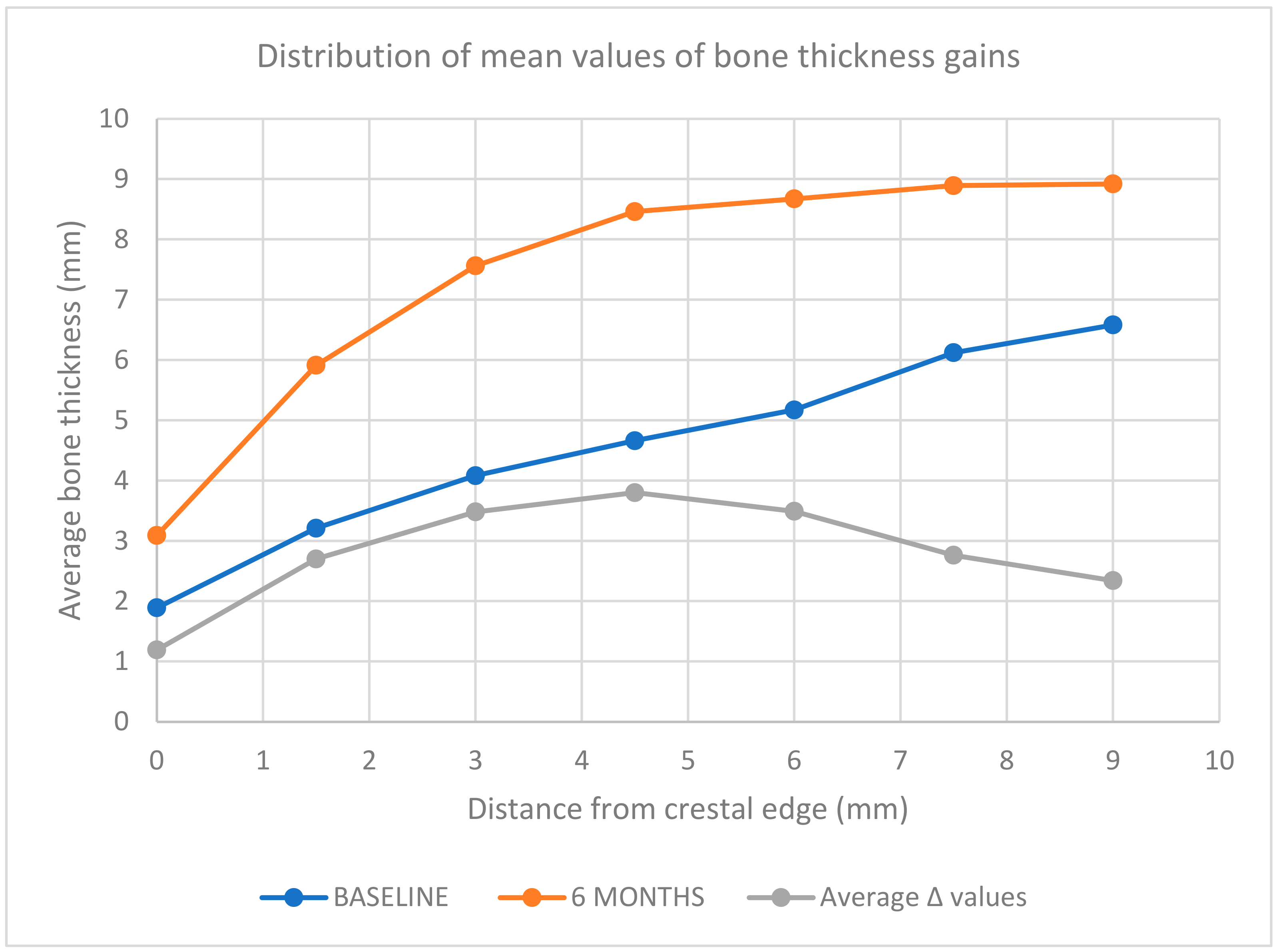
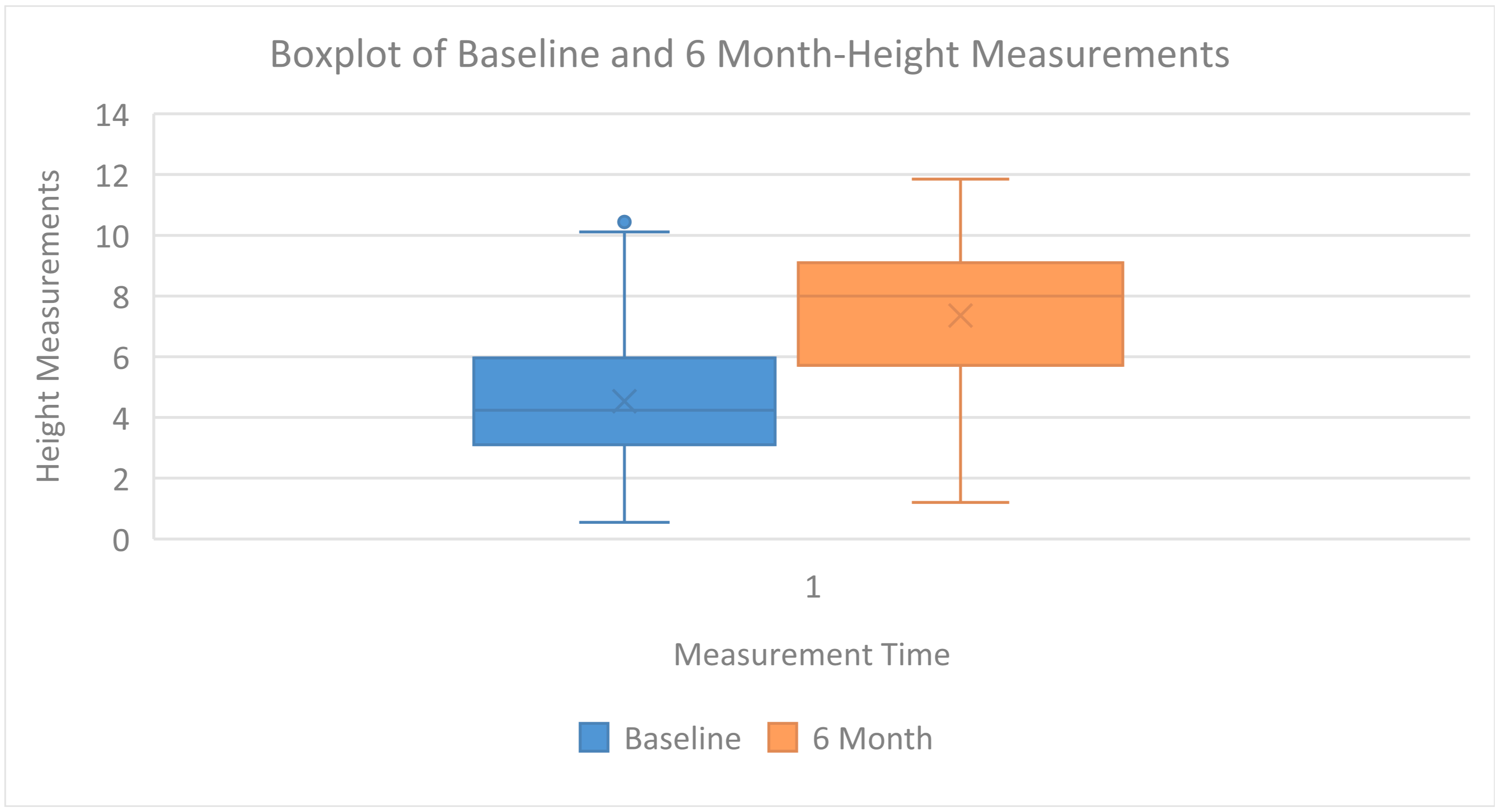
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Albrektsson, T.; Zarb, G.; Worthington, P.; Eriksson, A.R. The long-term efficacy of currently used dental implants: A review and proposed criteria of success. Int. J. Oral Maxillofac. Implants 1986, 1, 11–25. [Google Scholar] [PubMed]
- Oshida, Y.; Tuna, E.B.; Aktören, O.; Gençay, K. Dental implant systems. Int. J. Mol. Sci. 2010, 11, 1580–1678. [Google Scholar] [CrossRef] [PubMed]
- Chackartchi, T.; Romanos, G.E.; Parkanyi, L.; Schwarz, F.; Sculean, A. Reducing errors in guided implant surgery to optimize treatment outcomes. Periodontology 2000 2022, 88, 64–72. [Google Scholar] [CrossRef] [PubMed]
- Brugnami, F.; Caleffi, C. Prosthetically driven implant placement. How to achieve the appropriate implant site development. Keio J. Med. 2005, 54, 172–178. [Google Scholar] [CrossRef]
- Annibali, S.; Bignozzi, I.; La Monaca, G.; Cristalli, M.P. Usefulness of the aesthetic result as a success criterion for implant therapy: A review. Clin. Implant Dent. Relat. Res. 2012, 14, 3–40. [Google Scholar] [CrossRef] [PubMed]
- Morton, D.; Chen, S.T.; Martin, W.C.; Levine, R.A.; Buser, D. Consensus statements and recommended clinical procedures regarding optimizing esthetic outcomes in implant dentistry. Int. J. Oral Maxillofac. Implants 2014, 29, 216–220. [Google Scholar] [CrossRef] [PubMed]
- Buser, D.; Martin, W.; Belser, U.C. Optimizing esthetics for implant restorations in the anterior maxilla: Anatomic and surgical considerations. Int. J. Oral Maxillofac. Implants 2004, 19, 43–61. [Google Scholar] [PubMed]
- Chiapasco, M.; Casentini, P. Horizontal bone-augmentation procedures in implant dentistry: Prosthetically guided regeneration. Periodontology 2000 2018, 77, 213–240. [Google Scholar] [CrossRef] [PubMed]
- Spray, J.R.; Black, C.G.; Morris, H.F.; Ochi, S. The influence of bone thickness on facial marginal bone response: Stage 1 placement through stage 2 uncovering. Ann. Periodontol. 2000, 5, 119–128. [Google Scholar] [CrossRef] [PubMed]
- Yoda, N.; Zheng, K.; Chen, J.; Li, W.; Swain, M.; Sasaki, K.; Li, Q. Bone morphological effects on post-implantation remodeling of maxillary anterior buccal bone: A clinical and biomechanical study. J. Prosthodont. Res. 2017, 61, 393–402. [Google Scholar] [CrossRef]
- Viña-Almunia, J.; Candel-Martí, M.E.; Cervera-Ballester, J.; García-Mira, B.; Calvo-Guirado, J.L.; Peñarrocha-Oltra, D.; Peñarrocha-Diago, M. Buccal bone crest dynamics after immediate implant placement and ridge preservation techniques: Review of morphometric studies in animals. Implant Dent. 2013, 22, 155–160. [Google Scholar] [CrossRef] [PubMed]
- Farronato, D.; Pasini, P.M.; Orsina, A.A.; Manfredini, M.; Azzi, L.; Farronato, M. Correlation between Buccal Bone Thickness at Implant Placement in Healed Sites and Buccal Soft Tissue Maturation Pattern: A Prospective Three-Year Study. Materials 2020, 13, 511. [Google Scholar] [CrossRef] [PubMed]
- Cawood, J.I.; Howell, R.A. A classification of the edentulous jaws. Int. J. Oral Maxillofac. Surg. 1988, 17, 232–236. [Google Scholar] [CrossRef] [PubMed]
- Cawood, J.I.; Howell, R.A. Reconstructive preprosthetic surgery. I. Anatomical considerations. Int. J. Oral Maxillofac. Surg. 1991, 20, 75–82. [Google Scholar] [CrossRef] [PubMed]
- Aghaloo, T.L.; Moy, P.K. Which hard tissue augmentation techniques are the most successful in furnishing bony support for implant placement? Int. J. Oral Maxillofac. Implants 2007, 22, 49–70, Erratum in Int. J. Oral Maxillofac. Implants 2008, 23, 56. [Google Scholar]
- Chiapasco, M.; Casentini, P.; Zaniboni, M. Bone augmentation procedures in implant dentistry. Int. J. Oral Maxillofac. Implants 2009, 24, 237–259. [Google Scholar]
- Sanz-Sánchez, I.; Ortiz-Vigon, A.; Sanz-Martín, I.; Figuero, E.; Sanz, M. Effectiveness of lateral bone augmentation on the alveolar crest dimension: A systematic review and meta-analysis. J. Dent. Res. 2015, 94, 128S–142S. [Google Scholar] [CrossRef] [PubMed]
- Jensen, S.S.; Terheyden, H. Bone augmentation procedures in localized defects in the alveolar ridge: Clinical results with different bone grafts and bone-substitute materials. Int. J. Oral Maxillofac. Implants 2009, 24, 218–236. [Google Scholar] [PubMed]
- Esposito, M.; Grusovin, M.G.; Coulthard, P.; Worthington, H.V. The efficacy of various bone augmentation procedures for dental implants: A Cochrane systematic review of randomized controlled clinical trials. Int. J. Oral Maxillofac. Implants 2006, 21, 696–710. [Google Scholar] [PubMed]
- Al-Aroomi, O.A.; Sakran, K.A.; Al-Aroomi, M.A.; Mashrah, M.A.; Ashour, S.H.; Al-Attab, R.; Yin, L. Immediate implant placement with simultaneous bone augmentation versus delayed implant placement following alveolar ridge preservation: A clinical and radiographic study. J. Stomatol. Oral Maxillofac. Surg. 2023, 124, 101291. [Google Scholar] [CrossRef] [PubMed]
- Slagter, K.W.; Meijer, H.J.A.; Hentenaar, D.F.M.; Vissink, A.; Raghoebar, G.M. Immediate single-tooth implant placement with simultaneous bone augmentation versus delayed implant placement after alveolar ridge preservation in bony defect sites in the esthetic region: A 5-year randomized controlled trial. J. Periodontol. 2021, 92, 1738–1748. [Google Scholar] [CrossRef] [PubMed]
- Tolstunov, L.; Hamrick, J.F.E.; Broumand, V.; Shilo, D.; Rachmiel, A. Bone Augmentation Techniques for Horizontal and Vertical Alveolar Ridge Deficiency in Oral Implantology. Oral. Maxillofac. Surg. Clin. N. Am. 2019, 31, 163–191. [Google Scholar] [CrossRef] [PubMed]
- von Arx, T.; Buser, D. Horizontal ridge augmentation using autogenous block grafts and the guided bone regeneration technique with collagen membranes: A clinical study with 42 patients. Clin. Oral Implants Res. 2006, 17, 359–366. [Google Scholar] [CrossRef] [PubMed]
- Smeets, R.; Matthies, L.; Windisch, P.; Gosau, M.; Jung, R.; Brodala, N.; Stefanini, M.; Kleinheinz, J.; Payer, M.; Henningsen, A.; et al. Horizontal augmentation techniques in the mandible: A systematic review. Int. J. Implant Dent. 2022, 8, 23. [Google Scholar] [CrossRef] [PubMed]
- Cucchi, A.; Vignudelli, E.; Napolitano, A.; Marchetti, C.; Corinaldesi, G. Evaluation of complication rates and vertical bone gain after guided bone regeneration with non-resorbable membranes versus titanium meshes and resorbable membranes. A randomized clinical trial. Clin. Implant Dent. Relat. Res. 2017, 19, 821–832. [Google Scholar] [CrossRef] [PubMed]
- Chiapasco, M.; Casentini, P.; Tommasato, G.; Dellavia, C.; Del Fabbro, M. Customized CAD/CAM titanium meshes for the guided bone regeneration of severe alveolar ridge defects: Preliminary results of a retrospective clinical study in humans. Clin. Oral Implants Res. 2021, 32, 498–510. [Google Scholar] [CrossRef] [PubMed]
- Berger, S.; Hakl, P.; Sutter, W.; Meier, M.; Roland, H.; Bandura, P.; Turhani, D. Interantral alveolar ridge splitting for maxillary horizontal expansion and simultaneous dental implant insertion: A case report. Ann. Med. Surg. 2019, 48, 83–87. [Google Scholar] [CrossRef] [PubMed]
- Elnayef, B.; Monje, A.; Lin, G.H.; Gargallo-Albiol, J.; Chan, H.L.; Wang, H.L.; Hernández-Alfaro, F. Alveolar ridge split on horizontal bone augmentation: A systematic review. Int. J. Oral Maxillofac. Implants 2015, 30, 596–606. [Google Scholar] [CrossRef] [PubMed]
- Crespi, R.; Toti, P.; Covani, U.; Crespi, G.; Menchini-Fabris, G.B. Maxillary and mandibular split crest technique with immediate implant placement: A 5-year cone beam retrospective study. Int. J. Oral Maxillofac. Implants 2021, 36, 999–1007. [Google Scholar] [CrossRef] [PubMed]
- Artzi, Z. Lateral augmentation of the jaw by the split expansion ridge technique. A critical review. Periodontology 2000 2023, 93, 205–220. [Google Scholar] [CrossRef] [PubMed]
- Cordaro, L.; Amadé, D.S.; Cordaro, M. Clinical results of alveolar ridge augmentation with mandibular block bone grafts in partially edentulous patients prior to implant placement. Clin. Oral Implants Res. 2002, 13, 103–111. [Google Scholar] [CrossRef]
- Chappuis, V.; Cavusoglu, Y.; Buser, D.; von Arx, T. Lateral Ridge Augmentation Using Autogenous Block Grafts and Guided Bone Regeneration: A 10-Year Prospective Case Series Study. Clin. Implant Dent. Relat. Res. 2017, 19, 85–96. [Google Scholar] [CrossRef] [PubMed]
- Nkenke, E.; Schultze-Mosgau, S.; Radespiel-Tröger, M.; Kloss, F.; Neukam, F.W. Morbidity of harvesting of chin grafts: A prospective study. Clin. Oral Implants Res. 2001, 12, 495–502. [Google Scholar] [CrossRef] [PubMed]
- Nkenke, E.; Weisbach, V.; Winckler, E.; Kessler, P.; Schultze-Mosgau, S.; Wiltfang, J.; Neukam, F.W. Morbidity of harvesting of bone grafts from the iliac crest for preprosthetic augmentation procedures: A prospective study. Int. J. Oral Maxillofac. Surg. 2004, 33, 157–163. [Google Scholar] [CrossRef] [PubMed]
- Raghoebar, G.M.; Louwerse, C.; Kalk, W.W.; Vissink, A. Morbidity of chin bone harvesting. Clin. Oral Implants Res. 2001, 12, 503–507. [Google Scholar] [CrossRef] [PubMed]
- Cricchio, G.; Lundgren, S. Donor Site Morbidity in Two Different Approaches to Anterior Iliac Crest Bone Harvesting. Clin. Implant Dent. Relat. Res. 2003, 5, 161–169. [Google Scholar] [CrossRef] [PubMed]
- Reissmann, D.R.; Poxleitner, P.; Heydecke, G. Location, intensity, and experience of pain after intra-oral versus extra-oral bone graft harvesting for dental implants. J. Dent. 2018, 79, 102–106. [Google Scholar] [CrossRef] [PubMed]
- Reissmann, D.R.; Dietze, B.; Vogeler, M.; Schmelzeisen, R.; Heydecke, G. Impact of donor site for bone graft harvesting for dental implants on health-related and oral health-related quality of life. Clin. Oral Implant Res. 2012, 24, 698–705. [Google Scholar] [CrossRef] [PubMed]
- Maiorana, C.; Beretta, M.; Salina, S.; Santoro, F. Reduction of autogenous bone graft resorption by means of bio-oss coverage: A prospective study. Int. J. Periodontics Restor. Dent. 2005, 25, 19–25. [Google Scholar]
- Hämmerle, C.H.F.; Karring, T. Guided bone regeneration at oral implant sites. Periodontology 2000 1998, 17, 151–175. [Google Scholar] [CrossRef] [PubMed]
- Elgali, I.; Omar, O.; Dahlin, C.; Thomsen, P. Guided bone regeneration: Materials and biological mechanisms revisited. Eur. J. Oral Sci. 2017, 125, 315–337. [Google Scholar] [CrossRef] [PubMed]
- Jung, R.E.; Fenner, N.; Hämmerle, C.H.; Zitzmann, N.U. Long-term outcome of implants placed with guided bone regeneration (GBR) using resorbable and non-resorbable membranes after 12–14 years. Clin. Oral Implants Res. 2013, 24, 1065–1073. [Google Scholar] [CrossRef] [PubMed]
- Caballé-Serrano, J.; Munar-Frau, A.; Ortiz-Puigpelat, O.; Soto-Penaloza, D.; Peñarrocha, M.; Hernández-Alfaro, F. On the search of the ideal barrier membrane for guided bone regeneration. J. Clin. Exp. Dent. 2018, 10, e477–e483. [Google Scholar] [CrossRef] [PubMed]
- Retzepi, M.; Donos, N. Guided Bone Regeneration: Biological principle and therapeutic applications. Clin. Oral Implants Res. 2010, 21, 567–576. [Google Scholar] [CrossRef] [PubMed]
- Jung, R.E.; Brügger, L.V.; Bienz, S.P.; Hüsler, J.; Hämmerle, C.H.F.; Zitzmann, N.U. Clinical and radiographical performance of implants placed with simultaneous guided bone regeneration using resorbable and nonresorbable membranes after 22–24 years, a prospective, controlled clinical trial. Clin. Oral Implants Res. 2021, 32, 1455–1465. [Google Scholar] [CrossRef] [PubMed]
- Hammerle, C.H.F.; Jung, R.E.; Yaman, D.; Lang, N.P. Ridge augmentation by applying bioresorbable membranes and deproteinized bovine bone mineral: A report of twelve consecutive cases. Clin. Oral Implants Res. 2008, 19, 19–25. [Google Scholar] [CrossRef] [PubMed]
- Soldatos, N.K.; Stylianou, P.; Koidou, V.P.; Angelov, N.; Yukna, R.; Romanos, G.E. Limitations and options using resorbable versus nonresorbable membranes for successful guided bone regeneration. Quintessence Int. 2017, 48, 131–147. [Google Scholar] [CrossRef] [PubMed]
- Sbricoli, L.; Guazzo, R.; Annunziata, M.; Gobbato, L.; Bressan, E.; Nastri, L. Selection of Collagen Membranes for Bone Regeneration: A Literature Review. Materials 2020, 13, 786. [Google Scholar] [CrossRef] [PubMed]
- Urban, I.A.; Nagursky, H.; Lozada, J.L. Horizontal ridge augmentation with a resorbable membrane and particulated autogenous bone with or without anorganic bovine bone-derived mineral: A prospective case series in 22 patients. Int. J. Oral Maxillofac. Implant 2011, 26, 404–414. [Google Scholar]
- Urban, I.A.; Nagursky, H.; Lozada, J.L.; Nagy, K. Horizontal ridge augmentation with a collagen membrane and a combination of particulated autogenous bone and anorganic bovine bone-derived mineral: A prospective case series in 25 patients. Int. J. Periodontics Restor. 2013, 33, 299–307. [Google Scholar] [CrossRef] [PubMed]
- Arnal, H.M.; Angioni, C.D.; Gaultier, F.; Urbinelli, R.; Urban, I.A. Horizontal guided bone regeneration on knife-edge ridges: A retrospective case-control pilot study comparing two surgical techniques. Clin. Implant Dent. Relat. Res. 2022, 24, 211–221. [Google Scholar] [CrossRef] [PubMed]
- Kim, K.M.; Choi, S.Y.; Park, J.H.; Kim, H.Y.; Kim, S.J.; Kim, J.W. Six-month stability following extensive alveolar bone augmentation by sausage technique. Maxillofac. Plast. Reconstr. Surg. 2023, 45, 16. [Google Scholar] [CrossRef]
- Meloni, S.M.; Jovanovic, S.A.; Urban, I.; Baldoni, E.; Pisano, M.; Tallarico, M. Horizontal ridge augmentation using GBR with a native collagen membrane and 1:1 ratio of particulate xenograft and autologous bone: A 3-year after final loading prospective clinical study. Clin. Implant Dent. Relat. Res. 2019, 21, 669–677. [Google Scholar] [CrossRef] [PubMed]
- Meloni, S.M.; Jovanovic, S.A.; Urban, I.; Canullo, L.; Pisano, M.; Tallarico, M. Horizontal Ridge Augmentation using GBR with a Native Collagen Membrane and 1:1 Ratio of Particulated Xenograft and Autologous Bone: A 1-Year Prospective Clinical Study. Clin. Implant Dent. Relat. Res. 2017, 19, 38–45. [Google Scholar] [CrossRef] [PubMed]
- Dewilde, F.; Hindryckx, M.; Younes, F.; De Bruyckere, T.; Cosyn, J. Lateral bone augmentation with a composite graft covered with a stretched and pinned collagen membrane: A retrospective case series using cone-beam computed tomography. Clin. Implant Dent. Relat. Res. 2024. Early View. [Google Scholar] [CrossRef]
- Adibrad, M.; Shahabuei, M.; Sahabi, M. Significance of the width of keratinized mucosa on the health status of the supporting tissue around implants supporting overdentures. J. Oral Implantol. 2009, 35, 232–237. [Google Scholar] [CrossRef] [PubMed]
| Category | Total | Details |
|---|---|---|
| Patients treated | 5 | Two women and three men, average age 54.4 years |
| Regeneration areas | 6 | 5 in the maxilla, 1 in the mandible |
| Measurement sites | 10 | Distributed across the 6 surgical sites |
| Dental implants inserted | 10 | Distributed across the measurement sites |
| Sextant | Number of Implants |
|---|---|
| I | 2 |
| II | 6 |
| III | 0 |
| IV | 2 |
| V | 0 |
| VI | 0 |
| Height Measurement | Average Value | DS | Median | Interquartile Range |
|---|---|---|---|---|
| 0 | 1.89 | 1.17 | 1.52 | 1.09 |
| 1.5 | 3.21 | 1.25 | 3.38 | 1.54 |
| 3 | 4.08 | 1.46 | 4.22 | 1.53 |
| 4.5 | 4.66 | 1.54 | 4.78 | 2.16 |
| 6 | 5.17 | 1.64 | 5.23 | 2.86 |
| 7.5 | 6.12 | 2.38 | 5.94 | 3.27 |
| 9 | 6.58 | 2.64 | 6.11 | 3.95 |
| Height Measurement | Average Value | DS | Median | Interquartile Range |
|---|---|---|---|---|
| 0 | 3.09 | 1.48 | 2.98 | 1.60 |
| 1.5 | 5.91 | 1.56 | 6.05 | 1.86 |
| 3 | 7.56 | 1.76 | 7.57 | 1.78 |
| 4.5 | 8.46 | 1.64 | 8.43 | 2.35 |
| 6 | 8.67 | 1.38 | 9.03 | 1.48 |
| 7.5 | 8.89 | 1.17 | 9.00 | 1.17 |
| 9 | 8.92 | 1.54 | 8.89 | 1.85 |
| Height Measurement | Average Value | DS | Median | Interquartile Range |
|---|---|---|---|---|
| 0 | 1.19 | 1.66 | 0.77 | 1.12 |
| 1.5 | 2.70 | 1.59 | 2.43 | 0.96 |
| 3 | 3.48 | 1.74 | 2.63 | 2.31 |
| 4.5 | 3.80 | 1.51 | 3.18 | 2.01 |
| 6 | 3.49 | 1.06 | 3.41 | 1.60 |
| 7.5 | 2.76 | 2.30 | 1.96 | 3.69 |
| 9 | 2.34 | 2.69 | 1.42 | 4.36 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pieroni, S.; Miceli, B.; Giboli, L.; Romano, L.; Azzi, L.; Farronato, D. Efficacy of the Sausage Technique in Rebuilding the Crestal Buccal Bone Thickness: A Retrospective Analysis. Dent. J. 2024, 12, 180. https://doi.org/10.3390/dj12060180
Pieroni S, Miceli B, Giboli L, Romano L, Azzi L, Farronato D. Efficacy of the Sausage Technique in Rebuilding the Crestal Buccal Bone Thickness: A Retrospective Analysis. Dentistry Journal. 2024; 12(6):180. https://doi.org/10.3390/dj12060180
Chicago/Turabian StylePieroni, Stefano, Benedetta Miceli, Luca Giboli, Leonardo Romano, Lorenzo Azzi, and Davide Farronato. 2024. "Efficacy of the Sausage Technique in Rebuilding the Crestal Buccal Bone Thickness: A Retrospective Analysis" Dentistry Journal 12, no. 6: 180. https://doi.org/10.3390/dj12060180
APA StylePieroni, S., Miceli, B., Giboli, L., Romano, L., Azzi, L., & Farronato, D. (2024). Efficacy of the Sausage Technique in Rebuilding the Crestal Buccal Bone Thickness: A Retrospective Analysis. Dentistry Journal, 12(6), 180. https://doi.org/10.3390/dj12060180







