Effects of Vibration on Accelerating Orthodontic Tooth Movement in Clinical and In Vivo Studies: A Systematic Review
Abstract
1. Introduction
2. Materials and Methods
- P (Population): Orthodontic patients/animals with an orthodontic force.
- I (Intervention or Exposure): Exposure to high (>30 Hz) or low (≦30 Hz) frequency vibration.
- C (Comparison): Patients/animals who underwent orthodontic treatment with and without vibration stimuli.
- O (Outcomes): OTM by measuring the distance at several points over time intervals.
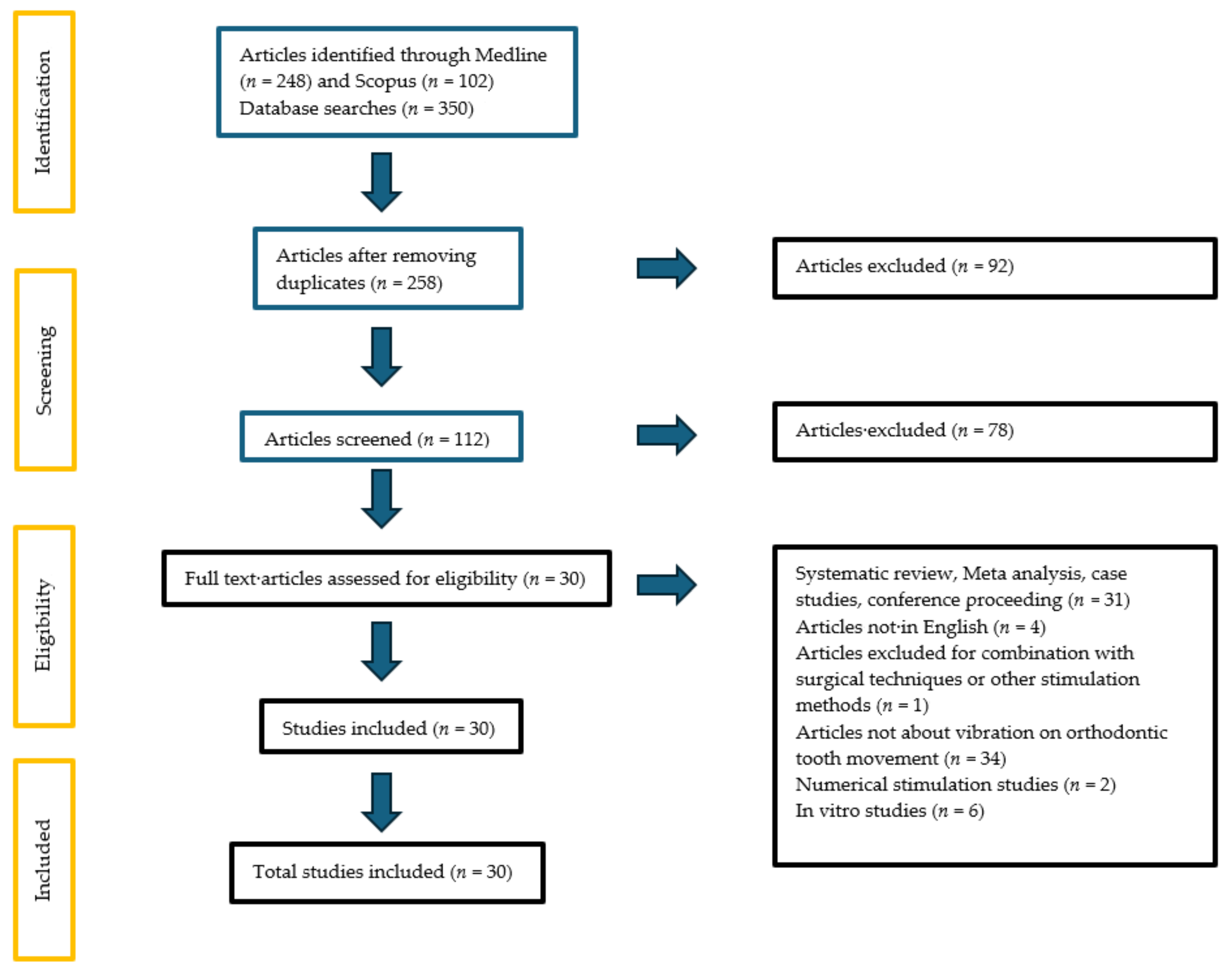
2.1. Research Strategy and Selection Process
2.2. Eligibility Criteria
- Clinical studies and in vivo studies.
- Vibration combined with orthodontic treatment / orthodontic force.
- Orthodontic treatment with aligners and fixed appliance.
- Review or meta-analysis, case studies and conference proceedings.
- In vitro studies.
- Articles not in English.
- Combination of vibration with surgical techniques or other stimulation method.
- Numerical simulation studies.
2.3. Data Collection and Extraction
2.4. Quality Assessment
3. Results
3.1. Search Strategy
3.2. Quality Assessment
3.3. In Vivo Studies
3.4. Clinical Studies
4. Discussion
4.1. Effects of Supplemental Low-Frequency Vibration on Dental Movement in Humans
4.2. Effects of Supplemental High-Frequency Vibration on Dental Movement in Human Patients
4.3. Effects of Supplemental Vibration on Dental Movement in In Vivo Studies
4.4. Limitations and Strengths of the Study
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- El-Angbawi, A.; McIntyre, G.T.; Fleming, P.S.; Bearn, D.R. Non-surgical Adjunctive Interventions for Accelerating Tooth Movement in Patients Undergoing Fixed Orthodontic Treatment. Cochrane Database Syst. Rev. 2015, 2016, CD010887. [Google Scholar] [CrossRef] [PubMed]
- Kacprzak, A.; Strzecki, A. Methods of Accelerating Orthodontic Tooth Movement: A Review of Contemporary Literature. Dent. Med. Probl. 2018, 55, 197–206. [Google Scholar] [CrossRef] [PubMed]
- Jing, D.; Xiao, J.; Li, X.; Li, Y.; Zhao, Z. The Effectiveness of Vibrational Stimulus to Accelerate Orthodontic Tooth Movement: A Systematic Review. BMC Oral Health 2017, 17, 143. [Google Scholar] [CrossRef] [PubMed]
- Andrade, I.; dos Santos Sousa, A.B.; da Silva, G.G. New Therapeutic Modalities to Modulate Orthodontic Tooth Movement. Dent. Press J. Orthod. 2014, 19, 123–133. [Google Scholar] [CrossRef] [PubMed]
- Leethanakul, C.; Suamphan, S.; Jitpukdeebodintra, S.; Thongudomporn, U.; Charoemratrote, C. Vibratory Stimulation Increases Interleukin-1 Beta Secretion during Orthodontic Tooth Movement. Angle Orthod. 2016, 86, 74–80. [Google Scholar] [CrossRef] [PubMed]
- Pascoal, S.; Gonçalves, A.; Brandão, A.; Rocha, D.; Oliveira, S.; Monteiro, F.; Carvalho, Ó.; Coimbra, S.; Pinho, T. Human Interleukin-1β Profile and Self-Reported Pain Monitoring Using Clear Aligners with or without Acceleration Techniques: A Case Report and Investigational Study. Int. J. Dent. 2022, 2022, 8252696. [Google Scholar] [CrossRef]
- Nishimura, M.; Chiba, M.; Ohashi, T.; Sato, M.; Shimizu, Y.; Igarashi, K.; Mitani, H. Periodontal Tissue Activation by Vibration: Intermittent Stimulation by Resonance Vibration Accelerates Experimental Tooth Movement in Rats. Am. J. Orthod. Dentofac. Orthop. 2008, 133, 572–583. [Google Scholar] [CrossRef] [PubMed]
- Siriphan, N.; Leethanakul, C.; Thongudomporn, U. Effects of Two Frequencies of Vibration on the Maxillary Canine Distalization Rate and RANKL and OPG Secretion: A Randomized Controlled Trial. Orthod. Craniofacial Res. 2019, 22, 131–138. [Google Scholar] [CrossRef] [PubMed]
- Benjakul, S.; Leethanakul, C.; Jitpukdeebodintra, S. Low Magnitude High Frequency Vibration Induces RANKL via Cyclooxygenase Pathway in Human Periodontal Ligament Cells in Vitro. J. Oral Biol. Craniofacial Res. 2019, 9, 251–255. [Google Scholar] [CrossRef]
- Alikhani, M.; Lopez, J.A.; Alabdullah, H.; Vongthongleur, T.; Sangsuwon, C.; Alikhani, M.; Alansari, S.; Oliveira, S.M.; Nervina, J.M.; Teixeira, C.C. High-Frequency Acceleration. J. Dent. Res. 2016, 95, 311–318. [Google Scholar] [CrossRef]
- Pascoal, S.; Oliveira, S.; Monteiro, F.; Padrão, J.; Costa, R.; Zille, A.; Catarino, S.O.; Silva, F.S.; Pinho, T.; Carvalho, Ó. Influence of Ultrasound Stimulation on the Viability, Proliferation and Protein Expression of Osteoblasts and Periodontal Ligament Fibroblasts. Biomedicines 2024, 12, 361. [Google Scholar] [CrossRef] [PubMed]
- Gonçalves, A.; Monteiro, F.; Oliveira, S.; Costa, I.; Catarino, S.O.; Carvalho, Ó.; Padrão, J.; Zille, A.; Pinho, T.; Silva, F.S. Optimization of a Photobiomodulation Protocol to Improve the Cell Viability, Proliferation and Protein Expression in Osteoblasts and Periodontal Ligament Fibroblasts for Accelerated Orthodontic Treatment. Biomedicines 2024, 12, 180. [Google Scholar] [CrossRef] [PubMed]
- Mordente, C.M.; Oliveira, D.D.; Palomo, J.M.; Cardoso, P.A.; Assis, M.A.L.; Zenóbio, E.G.; Souki, B.Q.; Soares, R.V. The Effect of Micro-Osteoperforations on the Rate of Maxillary Incisors’ Retraction in Orthodontic Space Closure: A Randomized Controlled Clinical Trial. Prog. Orthod. 2024, 25, 6. [Google Scholar] [CrossRef] [PubMed]
- Uribe, F.; Padala, S.; Allareddy, V.; Nanda, R. Patients’, Parents’, and Orthodontists’ Perceptions of the Need for and Costs of Additional Procedures to Reduce Treatment Time. Am. J. Orthod. Dentofac. Orthop. 2014, 145, S65–S73. [Google Scholar] [CrossRef] [PubMed]
- Bani-Hani, M.; Karami, M.A. Piezoelectric Tooth Aligner for Accelerated Orthodontic Tooth Movement. In Proceedings of the 2018 40th Annual International Conference of the IEEE Engineering in Medicine and Biology Society (EMBC), Honolulu, HI, USA, 18–21 July 2018; pp. 4265–4268. [Google Scholar] [CrossRef]
- Shipley, T.; Farouk, K.; El-Bialy, T. Effect of High-Frequency Vibration on Orthodontic Tooth Movement and Bone Density. J. Orthod. Sci. 2019, 8, 15. [Google Scholar] [CrossRef] [PubMed]
- Shamseer, L.; Moher, D.; Clarke, M.; Ghersi, D.; Liberati, A.; Petticrew, M.; Shekelle, P.; Stewart, L.A.; PRISMA-P Group. Preferred Reporting Items for Systematic Review and Meta-Analysis Protocols (PRISMA-P) 2015: Elaboration and Explanation. BMJ 2015, 349, g7647. [Google Scholar] [CrossRef] [PubMed]
- Jackson, N.; Waters, E. Criteria for the Systematic Review of Health Promotion and Public Health Interventions. Health Promot. Int. 2005, 20, 367–374. [Google Scholar] [CrossRef] [PubMed]
- Sterne, J.A.; Hernán, M.A.; Reeves, B.C.; Savović, J.; Berkman, N.D.; Viswanathan, M.; Henry, D.; Altman, D.G.; Ansari, M.T.; Boutron, I.; et al. ROBINS-I: A Tool for Assessing Risk of Bias in Non-Randomised Studies of Interventions. BMJ 2016, 355, i4919. [Google Scholar] [CrossRef] [PubMed]
- Fisher, M.; Feuerstein, G.; Howells, D.W.; Hurn, P.D.; Kent, T.A.; Savitz, S.I.; Lo, E.H. Update of the Stroke Therapy Academic Industry Roundtable Preclinical Recommendations. Stroke 2009, 40, 2244–2250. [Google Scholar] [CrossRef]
- Kalajzic, Z.; Peluso, E.B.; Utreja, A.; Dyment, N.; Nihara, J.; Xu, M.; Chen, J.; Uribe, F.; Wadhwa, S. Effect of Cyclical Forces on the Periodontal Ligament and Alveolar Bone Remodeling during Orthodontic Tooth Movement. Angle Orthod. 2014, 84, 297–303. [Google Scholar] [CrossRef]
- Yadav, S.; Dobie, T.; Assefnia, A.; Gupta, H.; Kalajzic, Z.; Nanda, R. Effect of Low-Frequency Mechanical Vibration on Orthodontic Tooth Movement. Am. J. Orthod. Dentofac. Orthop. 2015, 148, 440–449. [Google Scholar] [CrossRef] [PubMed]
- Takano-Yamamoto, T.; Sasaki, K.; Fatemeh, G.; Fukunaga, T.; Seiryu, M.; Daimaruya, T.; Takeshita, N.; Kamioka, H.; Adachi, T.; Ida, H.; et al. Synergistic Acceleration of Experimental Tooth Movement by Supplementary High-Frequency Vibration Applied with a Static Force in Rats. Sci. Rep. 2017, 7, 13969. [Google Scholar] [CrossRef] [PubMed]
- Alikhani, M.; Alansari, S.; Hamidaddin, M.A.; Sangsuwon, C.; Alyami, B.; Thirumoorthy, S.N.; Oliveira, S.M.; Nervina, J.M.; Teixeira, C.C. Vibration Paradox in Orthodontics: Anabolic and Catabolic Effects. PLoS ONE 2018, 13, e0196540. [Google Scholar] [CrossRef] [PubMed]
- Azeem, M.; Afzal, A.; Jawa, S.A.; Haq, A.U.; Khan, M.; Akram, H. Effectiveness of Electric Toothbrush as Vibration Method on Orthodontic Tooth Movement: A Split-Mouth Study. Dent. Press J. Orthod. 2019, 24, 49–55. [Google Scholar] [CrossRef] [PubMed]
- Reiss, S.; Chouinard, M.C.; Landa, D.F.; Nanda, R.; Chandhoke, T.; Sobue, T.; Allareddy, V.; Kuo, C.-L.; Mu, J.; Uribe, F. Biomarkers of Orthodontic Tooth Movement with Fixed Appliances and Vibration Appliance Therapy: A Pilot Study. Eur. J. Orthod. 2020, 42, 378–386. [Google Scholar] [CrossRef] [PubMed]
- Miles, P.; Smith, H.; Weyant, R.; Rinchuse, D.J. The Effects of a Vibrational Appliance on Tooth Movement and Patient Discomfort: A Prospective Randomised Clinical Trial. Aust. Orthod. J. 2012, 28, 213–218. [Google Scholar] [CrossRef] [PubMed]
- Khera, A.K.; Raghav, P.; Mehra, V.; Wadhawan, A.; Gupta, N.; Phull, T.S. Effect of Customized Vibratory Device on Orthodontic Tooth Movement: A Prospective Randomized Control Trial. J. Orthod. Sci. 2022, 11, 18. [Google Scholar] [CrossRef] [PubMed]
- Woodhouse, N.R.; DiBiase, A.T.; Papageorgiou, S.N.; Johnson, N.; Slipper, C.; Grant, J.; Alsaleh, M.; Cobourne, M.T. Supplemental Vibrational Force Does Not Reduce Pain Experience during Initial Alignment with Fixed Orthodontic Appliances: A Multicenter Randomized Clinical Trial. Sci. Rep. 2015, 5, 17224. [Google Scholar] [CrossRef]
- Liao, Z.; Elekdag-Turk, S.; Turk, T.; Grove, J.; Dalci, O.; Chen, J.; Zheng, K.; Darendeliler, M.A.; Swain, M.; Li, Q. Computational and Clinical Investigation on the Role of Mechanical Vibration on Orthodontic Tooth Movement. J. Biomech. 2017, 60, 57–64. [Google Scholar] [CrossRef]
- Katchooi, M.; Cohanim, B.; Tai, S.; Bayirli, B.; Spiekerman, C.; Huang, G. Effect of Supplemental Vibration on Orthodontic Treatment with Aligners: A Randomized Trial. Am. J. Orthod. Dentofac. Orthop. 2018, 153, 336–346. [Google Scholar] [CrossRef]
- Miles, P. Does Microvibration Accelerate Leveling and Alignment? A Randomized Controlled Trial. J. Clin. Orthod. 2018, 52, 342–345. [Google Scholar]
- Kumar, V.; Batra, P.; Sharma, K.; Raghavan, S.; Srivastava, A. Comparative Assessment of the Rate of Orthodontic Tooth Movement in Adolescent Patients Undergoing Treatment by First Bicuspid Extraction and En Mass Retraction, Associated with Low-Frequency Mechanical Vibrations in Passive Self-Ligating and Conventional Brackets: A Randomized Controlled Trial. Int. Orthod. 2020, 18, 696–705. [Google Scholar] [CrossRef] [PubMed]
- Telatar, B.C.; Gungor, A.Y. Effectiveness of Vibrational Forces on Orthodontic Treatment. J. Orofac. Orthop. Fortschritte Kieferorthopädie 2021, 82, 288–294. [Google Scholar] [CrossRef] [PubMed]
- Lombardo, L.; Arreghini, A.; Ghislanzoni, L.T.H.; Siciliani, G. Does Low-Frequency Vibration Have an Effect on Aligner Treatment? A Single-Centre, Randomized Controlled Trial. Eur. J. Orthod. 2019, 41, 434–443. [Google Scholar] [CrossRef] [PubMed]
- DiBiase, A.T.; Woodhouse, N.R.; Papageorgiou, S.N.; Johnson, N.; Slipper, C.; Grant, J.; Alsaleh, M.; Khaja, Y.; Cobourne, M.T. Effects of Supplemental Vibrational Force on Space Closure, Treatment Duration, and Occlusal Outcome: A Multicenter Randomized Clinical Trial. Am. J. Orthod. Dentofac. Orthop. 2018, 153, 469–480. [Google Scholar] [CrossRef] [PubMed]
- Taha, K.; Conley, R.S.; Arany, P.; Warunek, S.; Al-Jewair, T. Effects of Mechanical Vibrations on Maxillary Canine Retraction and Perceived Pain: A Pilot, Single-Center, Randomized-Controlled Clinical Trial. Odontology 2020, 108, 321–330. [Google Scholar] [CrossRef]
- Mayama, A.; Seiryu, M.; Takano-Yamamoto, T. Effect of Vibration on Orthodontic Tooth Movement in a Double Blind Prospective Randomized Controlled Trial. Sci. Rep. 2022, 12, 1288. [Google Scholar] [CrossRef] [PubMed]
- Yildiz, O.; Yagci, A.; Hashimli, N. Effect of Applying Intermittent Force with and without Vibration on Orthodontic Tooth Movement. J. Orofac. Orthop. Fortschritte Kieferorthopädie 2023, 1–10. [Google Scholar] [CrossRef] [PubMed]
- ElMotaleb, M.A.A.; El-Beialy, A.R.; El-Sharaby, F.A.; ElDakroury, A.E.; Eid, A.A. Effectiveness of Low Frequency Vibration on the Rate of Canine Retraction: A Randomized Controlled Clinical Trial. Sci. Rep. 2024, 14, 7952. [Google Scholar] [CrossRef] [PubMed]
- Akbar, A.; Rehman, A.U.; Fatima, M. Effects of Vibrations Induced by Electric Tooth Brush on Amount of Canine Retraction: A Cross Sectional Study Done at University of Lahore. J. Pak. Med. Assoc. 2022, 72, 1740–1745. [Google Scholar] [CrossRef]
- Bowman, S.J. The Effect of Vibration on the Rate of Leveling and Alignment. J. Clin. Orthod. 2014, 48, 678–688. [Google Scholar] [PubMed]
- Orton-Gibbs, S.; Kim, N.Y. Clinical Experience with the Use of Pulsatile Forces to Accelerate Treatment. J. Clin. Orthod. 2015, 49, 557–573. [Google Scholar] [PubMed]
- Bowman, S.J. The Effect of Vibration on Molar Distalization. J. Clin. Orthod. 2016, 50, 683–693. [Google Scholar] [PubMed]
- Shipley, T.S. Effects of High Frequency Acceleration Device on Aligner Treatment—A Pilot Study. Dent. J. 2018, 6, 32. [Google Scholar] [CrossRef] [PubMed]
- Bilello, G.; Fazio, M.; Currò, G.; Scardina, G.A.; Pizzo, G. The Effects of Low-Frequency Vibration on Aligner Treatment Duration: A Clinical Trial. J. Int. Soc. Prev. Community Dent. 2022, 12, 345–352. [Google Scholar] [CrossRef]
- Woodhouse, N.R.; DiBiase, A.T.; Johnson, N.; Slipper, C.; Grant, J.; Alsaleh, M.; Donaldson, A.N.A.; Cobourne, M.T. Supplemental Vibrational Force during Orthodontic Alignment: A Randomized Trial. J. Dent. Res. 2015, 94, 682–689. [Google Scholar] [CrossRef]
- Akbari, A.; Wang, D.; Chen, J. Peak Loads on Teeth from a Generic Mouthpiece of a Vibration Device for Accelerating Tooth Movement. Am. J. Orthod. Dentofac. Orthop. 2022, 162, 229–237. [Google Scholar] [CrossRef]
| Sample Size Calculation | Inclusion and Exclusion Criteria | Randomization | Allocation Concealment | Reporting of Animals Excluded from Analysis | Blinded Assessment of Outcome | Reporting Potential Conflicts of Interest and Study Funding | |
|---|---|---|---|---|---|---|---|
| Nishimura et al. (2008) [7] | Moderate | Weak | Weak | Weak | NA | Weak | Moderate |
| Kalajzic et al. (2014) [21] | Moderate | Weak | Weak | Weak | NA | Weak | Moderate |
| Yadav et al. (2015) [22] | Moderate | Weak | Strong | Weak | NA | Weak | Moderate |
| Takano-Yamamoto et al. (2017) [23] | Weak | Weak | Strong | Weak | NA | Moderate | Strong |
| Alikhani et al. (2018) [24] | Weak | Weak | Weak | Weak | Moderate | Strong | Moderate |
| Selection Biais | Study Design | Confounders | Blinding | Data Collection Method | Withdrawals and Dropouts | Final Decision | |
|---|---|---|---|---|---|---|---|
| Leethanakul et al., (2016) [5] | Moderate | Strong | Strong | Moderate | Strong | Strong | Strong |
| Azeem et al., (2019) [25] | Strong | Strong | Strong | Moderate | Strong | Strong | Strong |
| Reiss et al., (2020) [26] | Strong | Strong | Strong | Moderate | Strong | Strong | Strong |
| Miles et al., (2012) [27] | Moderate | Strong | Strong | Moderate | Strong | Strong | Strong |
| Khera et al., (2022) [28] | Strong | Strong | Strong | Moderate | Strong | Strong | Strong |
| Woodhouse et al., (2015) [29] | Strong | Strong | Strong | Moderate | Strong | Strong | Strong |
| Liao et al., (2017) [30] | Strong | Strong | Strong | Weak | Strong | Strong | Moderate |
| Katchooi et al., (2018) [31] | Strong | Strong | Strong | Strong | Strong | Strong | Strong |
| Miles, (2018) [32] | Strong | Strong | Strong | Weak | Strong | Strong | Moderate |
| Siriphan et al., (2019) [8] | Strong | Strong | Strong | Moderate | Strong | Strong | Strong |
| Kumar et al., (2020) [33] | Strong | Strong | Strong | Moderate | Strong | Strong | Strong |
| Teletar et al., (2021) [34] | Strong | Strong | Strong | Weak | Strong | Strong | Moderate |
| Lombardo et al., (2019) [35] | Strong | Strong | Strong | Moderate | Strong | Strong | Strong |
| DiBiase et al., (2018) [36] | Strong | Strong | Strong | Moderate | Strong | Strong | Strong |
| Taha et al., (2020) [37] | Strong | Strong | Strong | Weak | Strong | Strong | Moderate |
| Mayama et al., (2022) [38] | Strong | Strong | Strong | Moderate | Strong | Strong | Strong |
| Yildiz et al., (2023) [39] | Strong | Strong | Moderate | Moderate | Strong | Strong | Strong |
| ElMotaleb et al., (2024) [40] | Strong | Strong | Strong | Moderate | Strong | Strong | Strong |
| Bias Arising from the Randomization Process | Bias Caused by Deviations from Intended Interventions | Bias Caused by Missing Outcome Data | Bias in Measurement of the Outcome | Bias in Selection of the Reported Results | Overall Bias | |
|---|---|---|---|---|---|---|
| Akbar et al., (2022) [41] | Low | Low | Low | Some concerns | Low | Some concerns |
| Bowman, (2014) [42] | Low | High | High | Low | Low | High |
| Orton-Gibbs et al., (2015) [43] | High | High | High | High | High | High |
| Bowman, (2016) [44] | Low | Low | Low | Low | Low | Low |
| Shipley, (2018) [45] | Low | Low | Low | Low | Low | Low |
| Shipley et al., (2019) [16] | Low | Some concerns | Low | Low | Low | Some concerns |
| Bilello et al., (2022) [46] | Low | Low | Low | Low | Low | Low |
| Author (Year) | Population | Orthodontic Appliance | Treatment Objectives | Vibration Parameters | Results | Conclusion |
|---|---|---|---|---|---|---|
| Nishimura et al. (2008) [7] | N = 12 ♂ 6-week-old Wistar Rats. Groups: - CG: expansive spring to move the upper first molars - EG: additional vibration stimulation applied to the first molars | Fixed appliances: standardized expansive spring made of 0.012-in nickel–titanium wire. | Effects of mechanical stimulation by resonance vibration on tooth movement. | Mean additional vibrational stimulation of 61.02 ± 8.375 Hz, during 8 min on days 0, 7, and 14 during 21 days using an expansive spring | - Mean displacement in resonance was 0.0014 ± 0.002 mm and the average velocity was 0.27 ± 0.018 mm/s. EG: ↑Extent of tooth movement on day 21 (15%) and ↑Osteoclasts - RANKL-positive cells were found in the PDL of both groups. RANKL expression was stronger on the compression side (compared to the tension side). - Root resorption: observed on the root surface of the compression side (both groups). | Application of resonance vibration: might accelerate orthodontic tooth movement. Enhances RANKL expression in the PDL. No additional damage (to periodontal tissues) such as root resorption. |
| Kalajzic et al. (2014) [21] | N = 26 ♀ Sprague-Dawley rats 7 weeks old Groups: - CG 1: unloaded - CG 2: only vibration - CG 3: only orthodontic spring - EG: orthodontic spring and additional vibrational stimulus | Fixed appliances: nickel–titanium coil spring (25 g of force). | Effect of cyclical force, vibratory, on tooth movement, on the structural integrity of the periodontal ligament, and remodelling of alveolar bone. | Forces at 0.4 N and 30 Hz. 2x/week for 10 min | Statistically significant difference in tooth movement measurements between molars: CG3 (mean of 0.486 ± 0.178 mm) compared to the CG1, CG2, and EG, and when EG (mean of 0.242 ± 0.139 mm) was compared to the CG2 and CG3 groups. It was found at smaller intermolar distances in EG, suggesting that 30 Hz cyclical force inhibited tooth movement. In CG1 and CG2, fewer osteoclasts were found on the alveolar bone and almost no osteoclasts in the periodontal ligament, but a statistical significance in the osteoclast number was found in CG3 (mean: 7.50 ± 1.98) compared to CG1 (1.75 ± 2.06) and CG2 (1.75 ± 1.50). Significant bone volume fraction decrease in CG3 compared to CG1 and CG2. Collagen fibers: tightly thicker morphology in CG2 than CG1. In CG3, collagen fibers were thick and smooth. The EG had a disrupted morphology compared to the CG3. | Cyclical forces significantly inhibited the amount of tooth movement. There was also a disorganization of the collagen fibril structure of the periodontal ligament during dental movement. |
| Yadav et al. (2015) [22] | N = 64 ♂ CD1 mice 12 weeks old. Groups: - CGs: baseline; no spring + 5 Hz; no spring + 10 Hz; no spring + 20 Hz. - EGs: spring + no vibration; spring + 5 Hz; spring + 10 Hz; spring + 20 Hz. | Nickel-titanium coil springs: 10 g of force, 2 weeks. | To study the effect of low frequencies of vibration on the rate of movement of the teeth, on the BVF, on the tissue density, and on the integrity of the PDL. | LFMV: 5, 10, or 20 Hz. 15 min. | LFMV did not increase the rate of orthodontic tooth movement. Microfocus X-ray computed tomography analysis showed increases in bone volume fractions and tissue densities with applications of LFMV. Sclerostin expression was decreased with 10 and 20 Hz vibrations in both the control and experimental groups. Additionally, the picrosirius staining showed that LFMV helped in maintaining the thickness and integrity of collagen fibers in the periodontal ligament. | There was no significant increase in tooth movement by applying LFMV when compared with the control groups (spring 1 no vibration). LFMV (5, 10, 20 Hz) had no deleterious effect on the integrity of the PDL. However, LFMV maintains the thickness and integrity of the PDL. |
| Takano- Yamamoto et al. (2017) [23] | N = 70 ♂ 25-week-old Wistar rats (410 g). Groups: - C control group - TM: tooth movement by activated Ni-Ti appliance - V: vibration only - TMV: Ni-Ti appliance and vibration | Continuous static force bent 0.014-inch nickel-titanium wires to the upper right first molar to move it palatally. | To investigate whether the additional application of a vibration device can accelerate orthodontic movement. Searching for the smallest magnitude, the smallest number of applications, and the shortest exposure. | New vibration device with automatic changes: frequency of vibration: 3 gf at 70 Hz, 21 days. EG1 for 3 min, EG2 for 6 min, EG3 for 10 min, EG4 for 30 min. | EG3-Optimal conditions to accelerate orthodontic tooth movement (maxillary molar of adult rats): 3 gf at 70 Hz for 3 min per week (one-week intervals). Optimum magnitude high-frequency vibration, with static force accelerates tooth movement. - Acceleration of experimental tooth movement (by supplemental vibration) did not correlate with the duration of the vibration’s exposure. - Vibration did not produce a directional force that moved the teeth. Thus, vibration alone does not cause tooth movement. - Optimum-magnitude high-frequency vibration with static force did not affect root resorption. - Supplementary vibration with a force synergistically stimulated the activation in osteoblasts, osteoclasts and osteocytes. - During the experimental group: vibration and static force increased the size of the tooth sockets around the periodontal ligament by osteoclastic bone resorption. | The most effective level of supplementary vibration to accelerate tooth movement stimulated by a continuous static force was 3 gf at 70 Hz for 3 min once a week. Furthermore, at this optimum-magnitude, high-frequency vibration could synergistically enhance osteoclastogenesis, leading to alveolar bone resorption and finally, accelerated tooth movement, but only when a static force was continuously applied to the teeth. |
| Alikhani et al. (2018) [24] | N = 206 ♂ adult Sprague Dawley rats Average weight of 400 g, 120 days of age. Groups: - CG1: animals not received spring nor HFV. - CG2: spring with no activation. - CG3 (orthodontic tooth movement only) - EG: same orthodontic forces and different HFA regimens. | Fixed appliances: Sentalloy closing coils 10 cN or 25 cN of force 1 mm activation | To study the effect of high-frequency acceleration on the rate of movement of teeth and alveolar bone, and to investigate the mechanism by which high-frequency acceleration affects movement. | Acceleration: 0.01 g, 0.05 g or 0.1 g. Frequency: 30 Hz, 60 Hz or 120 Hz. Duration 5 or 10 min. | Increase in acceleration increased the rate of tooth movement Effect of frequency and time on rat of tooth movement is not linear Effects of HFA on the rate of tooth movement are similar to orthodontic forces: Both are PDL-dependent and enhance cytokine release HFA increased osteoclast activity and bone resorption during orthodontic tooth movement | HFA can be used to improve the rate of tooth movement during the catabolic phase of treatment, and can then be used in the anabolic remodelling phase to improve retention. Compared to control groups, 30 Hz demonstrates an increase in the rate of tooth movement Frequencies of 60 Hz and 120 Hz caused an increase in the rate of tooth movement, compared with both control and 30 Hz |
| Author (Year) | Type of Study | Population | Orthodontic Appliance | Treatment Objectives/Methods | Vibration Parameters | Results | Conclusion |
|---|---|---|---|---|---|---|---|
| Miles et al., (2012) [27] | Randomized clinical trial | N = 66 Aged 11 and 15 years old. Groups: - CG: without stimulation - EG: Tooth Masseuse® | Fixed appliances. | Rate of tooth movement and patient discomfort. Irregularity at 4 time points: start of treatment T0, 5 weeks T1, 8 weeks T2, 10 weeks T3. Level of discomfort at 5 times: after initial brackets and wire placement, 6–8 h after, 1 day after, 3 days after, and 7 days after appliances were placed. | Vibrational frequency of 111 Hz and 0.06 N minimum of 20 min per day. | CG: - Irregularity mean: T0 4.9 mm; T3: 1.6 mm. - Mean irregularity difference: T0–T2: 3.1 mm T0–T3: 3.4 mm EG: - Irregularity mean: T0 6.2 mm; T3: 2.1 mm. - Mean irregularity difference: T0–T3: 4.0 mm | No significant differences in the levels of irregularity or pain between the two groups. |
| Bowman (2014) [42] | Non-randomized clinical trial | N = 117 ♂47 ♀70 Groups: - EG: AcceleDent® vibration group - CG1: Fixed appliance only - CG2: Patients who were treated prior to the initiation of a separate pro- spective examination of the effects of vibration on molar distalization | Fixed appliances. | Effects of vibrational device on the time required for lower arch levelling and alignment on Class II non-extraction patients who underwent upper molar distalization. | AcceleDent® device. Low-frequency vibration 30 Hz, 0.25 N, for 20 min per day. | - Mean time period required to attain alignment of the lower arch dentition was shorter in the EG groups than in the CGs (respectively 93 < 120 < 131 days). - The following arch wire (0.017” × 0.025”) was placed in the EG group earlier than in the CGs: 27 days earlier than CG1 patients and 38 days earlier than in the CG2 group (respectively, 29% and 40% faster). - Levelling took approximately 5 months in EG and 7 months in CGs. | AcceleDent®: ↓amount of time needed to achieve dental alignment and levelling in Class II non extraction patients. ↑30% tooth movement during levelling of the lower arch dentition. |
| Woodhouse et al., (2015) [29] | Randomized controlled trial. | N = 81 ♂ 40 ♀41 Mean age of 14.1 years. Groups: - EG 1: fixed appliance treatment with AcceleDent® - CG 1: fixed appliance treatment with identical non-functional device (sham) - CG 2: fixed appliance only. | Fixed appliances. | Effect of additional vibration force on the rate of orthodontic alignment of teeth with fixed appliances. | AcceleDent® device. Low-frequency vibration 30 Hz, 0.25 N, for 20 min per day. | - Mean irregularity index at baseline for the total sample: 8.5 mm (±3.8) with no significant difference among groups. - Mean irregularity index at initial alignment for the total sample: 2.7 mm (±2.8) with no significant difference among groups. - Mean time from initial to final alignment: 150 days (±62.5). - Mean time from baseline to final alignment: 209 days (±65). There were no significant differences among groups. - For each mm of irregularity, initial rate, initial rate of alignment increased by 0.01 mm/day, and overall rate increased by 0.004 mm/day. | No evidence that the additional vibratory force increases the rate of initial tooth movement or reduces the time required to achieve final alignment. |
| Orton-Gibbs et al., (2015) [43] | Non-randomized clinical trial | N = 117 Mean age of 31 years. 76% adults ♀66% ♂ 44% Groups: Group with fixed appliance: - EG: fixed appliances and AcceleDent® - CG: fixed appliances only Group with aligners: - EG: aligners and AcceleDent® - CG: aligners only | Ceramic brackets (N = 52) Metal brackets (N = 19) Lingual brackets (N = 19) Clear aligners (N = 16) Removable expansion appliances (N = 11) | Study the processing time with the AcceleDent® experiment. | AcceleDent® device. Low-frequency vibration 30 Hz, 0.25 N, for 20 min per day. | Group with fixed appliances: In the group with patients with fixed appliances and using AcceleDent®, treatment took an average 12.4 months: 38.2% faster than the predicted time (20.0 months). In the group with patients without AcceleDent®, predicted treatment time was accurate to within an average of 1.6 months. Predicted times were between 18 and 24 months. Group with aligners: - Patients with aligners and AcceleDent® had to change aligners as they became passive (7 to 10 days): treatment time was an average 37.2% faster than the conservative estimate, with a range of 5–55% faster. | AcceleDent® in patients with fixed appliances or aligners ↓treatment time. |
| Bowman (2016) [44] | Non-randomized clinical trial | N = 30 Mean age: EG 13.1 years, CG 2.9 years ♂13 ♀17 in each group. Groups: - EG: AcceleDent® throughout orthodontic treatment - CG: orthodontic treatment only | Fixed appliances | Study the effects of vibration on molar distalization. | AcceleDent® device. Low-frequency vibration 30 Hz, 0.25 N, for 20 min per day. | - Significant difference between EG and CG with respect to 2nd-molar eruption status. - No statistically significant differences between groups with respect to upper 1st molar tipping, intrusion, crown distalization, number of days required to achieve a super-Class I molar relationship. - EG 27% greater rate of crown movement (1.1 mm/month vs. 0.9 mm/month). Also, 71% more movement of the molar root apex (2.9 mm/month vs. 1.7 mm/month). | ↑30% of the mandibular arch levelling rate ↑almost 3 × the tooth movement per month typically reported of 1 mm in the maxillary arch ↑150–200% reduction in time required. |
| Leethanakul et al., (2016) [5] | Randomized controlled trial. | N = 15 Mean age 22.9 years. Groups: - EG: one side with light force of 60 g applied to the canine for three months + vibratory stimuli - CG: Contralateral canine: only orthodontic force. | Fixed appliances. | Effects of vibratory stimuli applied with an electric toothbrush on interleukin IL-1 secretion during upper canine distalization. | Electric toothbrush Battery-powered Colgate® Motion-Multi Action. 125 Hz. 15 min per day for 2 months. Time points: T0 before starting canine retraction T1 after canine retraction for one month T2 after canine retraction for two months without and with vibration T3 after canine retraction for three months without and with vibration. | - Patterns of fluctuation in the GCF’s volumes were similar at the pressure and tension sites of experimental and control canine. - IL-1β level at the pressure site of control teeth: higher for experimental teeth than for control teeth. IL-1β level for experimental teeth, after one month of vibration, did not reduce at T2 and stayed like levels at T1 and then elevated significantly at T3. - IL-1β level at the tension site of control teeth: no fluctuations observed. - IL-1β level at the tension site of experimental teeth: increased after vibration at T2 and T3 time points. At T3, a significant difference in the IL-1β levels were observed between the tension sites of experimental teeth. - IL-1β levels of experimental teeth were higher at the pressure site after retraction and after one month of vibration. IL-1β levels of control teeth were higher at the pressure site after retraction. - Within T0 and T1, the amount of canine movement was equal for experimental and control teeth. At T2 and T3, the amount was higher for experimental teeth compared to control teeth. After T2, the amount of movement doubled for the experimental teeth. - Within T2 and T3, the amount of tooth movement reduced for the experimental teeth but remained higher than control teeth. | Vibratory stimuli, in combination with orthodontic force: ↑secretion of IL-1β in GCF ↑bone resorption activity and acceleration of tooth movement. |
| Liao et al., (2017) [30] | Randomized controlled trial. | N = 13 patients Mean age:13.6 years. Patients were randomly assigned a vibration and a non-vibration side on the buccal surface of upper canine. | Orthodontic fixed appliances: brackets. | Examine the biomechanics of orthodontic movements when subjected to a single tooth vibration with a conventional orthodontic force. Distal retraction of maxillary canines. | Oral B® Hamming Bird Vibrating device with a frequency of 50 Hz and a force of 0.2 N, 10 min per day. | - Amount of total space closure on canine distalization is higher with vibration (compared to non-vibration). - Harmonic vibration in conjunction with orthodontic force: amplify the VHS of the PDL. - 50 Hz vibration: increased the VHS of canine PDL (9.2% for the mesio-distally and 10.8% for the linguo-buccally). - Highest amplification induced by the vibration of 50 Hz was recorded with lateral incisor with mesio-distal vibration and 1st premolar with linguo-buccally vibration. - General enlargements of tissue responses: ranging from 7.3% to 13.5% - Higher amplifications for 1st and 2nd premolars and canine for linguo-buccal vibration. | The amount of total space closure ↑with vibration and the amount of distalization of the canine ↑on the vibration side. |
| Lombardo et al., (2019) [35] | Randomized controlled trial. | N = 45 Mean age of 27.1 ♀ 25 ♂ 20 Groups: - CG: Group A: 15 patients, conventional protocol with aligners replaced every 14 days. - EG: Group B: 15 patients with aligners substituted every 14 days + AcceleDent® - EG: Group C: 15 patients with aligners substituted every 7 days + AcceleDent® | Aligners | Differences in the accuracy of tooth movement in patients who are treated with a low-frequency vibratory aligner AND reducing OR reducing the interval of aligner replacement compared to a conventional protocol. | AcceleDent® device. Low-frequency vibration 30 Hz, 0.25 N, for 20 min per day. | - Rotation of the upper incisors: group B is significantly more accurate than group A. (0.72 > 0.62) - Vestibulo-lingual tipping of the upper canines: group B significantly more accurate than group C. (0.67 > 0.54) - Mésio-distal tipping of the upper canines: group B significantly more accurate than group C. (0.65 > 0.49) - Vestibulo-lingual tipping of the upper molars: group B significantly more accurate than group C. (0.71 > 0.55) | No difference in accuracy between the aligners (replacing every 7 days) with low-frequency and aligners (replacing every 14 days) without vibration. |
| Katchooi et al., (2018) [31] | Randomized controlled trial. | N = 27 Mean age of 33 years. ♂ 12 ♀ 15 Groups: - EG: N = 14 AcceleDent® and aligners - CG: N = 13 Sham AcceleDent® and aligners | Aligners | Effects of AcceleDent® when used in conjunction with Invisalign® (clear aligners). | AcceleDent® device. Low-frequency vibration 30 Hz, 0.25 N, for 20 min per day. | - Both groups were compliant with usage of AcceleDent® and there was no significant difference between completers and non-completers of the 1-week change regimen. - No significant difference in rates between EG and the CG (77% and 85% respectively). - T-tests indicated no difference in the irregularity index between the EG and the CG. - Pain levels lower in the group with active AcceleDent®. But the differences were significantly different at day 3 of the first set of aligners. | No evidence that AcceleDent® completes a series of alignments (weekly change) or final alignment obtained in the 27 patients. No significant effects on pain reduction or quality of life when AcceleDent® is used with Invisalign® |
| DiBiase et al., (2018) [36] | Randomized clinical trial. | N = 61 Mean age 13.9 ♂ 30 ♀ 31 Groups: - EG: AcceleDent® With fixed appliance - CG: Fixed appliances only | Fixed appliances. | Study the effect of an additional vibratory force on space closure and the results on patients with fixed appliances | AcceleDent® device. Low-frequency vibration 30 Hz, 0.25 N, for 20 min per day. | - Initial rate of mandibular arch space closure: median of 0.89 mm/month with no significant differences among groups. - No significant differences among groups for any secondary outcomes, -overall treatment duration (median 18.57 months) - overall rate of mandibular arch space closure (median 0.74 mm/month) - number of visits (median 12 visits) - number of breakages (median 2 breakages) - absolute (median 28 points) - % of improvement in PAR score (median 90.0%) - final PAR score (3 points). | There is no benefit with vibration in the rate of mandibular space closure, in the duration of treatment and in the result. Furthermore, the use of additional vibratory forces with fixed devices is not associated with increased device breakage |
| Miles, (2018) [32] | Randomized controlled trial. | N = 40 Mean age of 12.8 years. ♀ 26 ♂ 14 Groups: - EG: AcceleDent Aura® with fixed appliances - CG: fixed appliances only | Fixed appliances. | Difference in time to reach the working wire stage with the AcceleDent® device compared to the control group. | AcceleDent® device. Low-frequency vibration 30 Hz, 0.25 N, for 20 min per day. | - Upper arch: AcceleDent® group took a median 139 days and the control group took 132 days. - Lower arch: AcceleDent® group took a median 143 days and the control group took 139 days. | In the upper arch, the difference in treatment time for the AcceleDent® group and the control group is not significant. The same is true for the lower arch. |
| Shipley, (2018) [45] | Non-randomized clinical trial | N = 16 EG: 27.6 years; CG age: 18.9 years. ♀ 11 ♂ 5 Groups: - EG with aligner treatment + use of the HFA device. Exchanged aligners every 5 days. - CG: aligner treatment, exchange aligners every 14 days. | Aligners | Effect of an HFA on clear aligners exchange intervals + treatment time needed to achieve prescribed tooth movements. | VPro5® device 120 Hz, 5 min per day. | - Lower and upper crowding were at 0.0 mm for all patients in EG and CG at post-treatment. - Prescribed number of aligners was not significantly different between groups (14 days), but the number used in EG was lower than among controls (approximately 5 days and 14 respectively). This equates to a 66% reduction. - Estimated treatment durations between groups did not differ significantly. Treatment duration for EG was significantly shorter than CG. EG duration was significantly shorter than estimated and CG duration was significantly longer than estimated. | VPro5®: ↑66% aligners exchange ↓number of aligners to complete treatment |
| Azeem et al., (2019) [25] | Randomized controlled trial. | N = 28 Mean age of 20.8 years. ♀ 18 ♂ 10 Groups: - EG: vibration-side with a light force of 100 g applied to the canine for 90 days + vibratory stimuli - CG: non-vibration-side with only orthodontic force applied to the canine | Fixed appliances. | Effect of an electric toothbrush (vibratory stimuli) on the speed of orthodontic tooth movement during maxillary canine retraction | Orthodontic brush head Oral-B Triumph® 125 Hz. 20 min per day. | - First month of canine retraction: amount of canine movement equal for the vibration side and non-vibration side. - Second and third months: also similar for the canines on the vibration side and non-vibration side. - Plaque accumulation: minimal during the study. No statistically significant difference between the vibration and the non-vibration sides. - No reported discomfort. | Application of supplemental vibratory stimuli (electric toothbrush) in combination with light orthodontic force do not accelerate tooth movement. |
| Siriphan et al., (2019) [8] | Randomized controlled trial. | N = 60 Mean age 21.5 years ♀ 47 ♂ 13 Groups: - EG 1: canine combined with 60 cN continuous distalization force and 30 Hz vibration - EG 2: canine combined with 60 cN continuous distalization force and 60 Hz vibration - CG: canine combined with 60 cN continuous distalization force only | Fixed appliances. | Effects of a vibratory stimulus on canine distalization and OPG and RANKL secretion. | 30 Hz vibration or 60 Hz vibration produced by modified electric toothbrushes, for 20 min per day Timepoints: T1: Before initiation of distalization. T2: 24 h after initiation of distalization. T3: 48 after initiation of distalization. T4: 7 days after initiation of distalization. | - Compression side in the group control: RANKL is significantly different between time points. - RANKL at T1 is significantly lower than T2, T3, or T4 - RANKL, OPG, and RANKL/OPG ratio: not significantly different within or between groups. - Rates of canine movement: not significantly different between the 30 Hz (0.82 mm/month), 60 Hz (0.87 mm/month), and control groups (0.83 mm/month). - Rates of molar movement and tipping and canine rotation and tipping: not significantly different between groups. | 30 Hz and 60 Hz vibrations have no additive effect on rate of canine distalization, OPG, and RANKL secretion or RANKL/OPG ratio. |
| Shipley et al., (2019) [16] | Non-randomized clinical trial | N = 30 ♀ 19 ♂ 11 Groups: - EG: VPro5® with aligners - CG: only aligners | Aligners | Effects of HFV on tooth movement and post-treatment bone density at initiation of retention. | VPro5® device 120 Hz, 5 min per day. | - Patients with adjunctive HFV exchanged aligners faster than the CG. They also finished the treatment faster. EG average clear aligners exchange interval was 5.2 ± 2.2 days whereas for the control group it was 8.7 ± 1.2 days. EG average total treatment time was 135 ± 27 days whereas for the control group it was 252 ± 59 days. A substantial increase in bone density in the alveolar bone around teeth in the maxilla and mandible was observed in the EG, but not in the CG at the beginning of the retention phase. | VPro5® ↑aligner change ↑tooth movement ↑bone density |
| Kumar et al., (2020) [33] | N = 65 Mean age of 17.1 years. ♀ 35 ♂ 30 Groups: - EG 1: passive self-ligating brackets treated + low-frequency vibrations - EG 2: Conventional MBT brackets + low-frequency vibrations - CG: conventional MBT brackets only | Fixed appliances: conventional MBT brackets and passive self-ligating brakets | Effectiveness of frequent low-frequency vibration on orthodontic movements in patients with passive self-ligating brackets and conventional brackets. | 30 Hz vibration, 20 min per day | - Rate of space closure in EG 1: 0.61 mm/month (maxillary right side), 0.61 mm/month (maxillary left side), 0.51 mm/month (mandibular right side), 0.51 mm/month (mandibular left side). - Rate of space closure in EG 2: 0.54 mm/month (maxillary right side), 0.54 mm/month (maxillary left side), 0.46 mm/month (mandibular right side), 0.46 mm/month (mandibular left side). - Rate of space closure in CG: 0.57 mm/month (maxillary right side), 0.61 mm/month (maxillary left side), 0.53 mm/month (mandibular right side), 0.53 mm/month (mandibular left side). | Low frequency does not increase in a statistically significant way the orthodontic tooth movement. | |
| Taha et al., (2020) [37] | Randomized- controlled trial | N = 21 Mean age of 15.48 years. ♀ 14 ♂ 7 Groups: - EG: mechanical vibration device with fixed appliance - CG: fixed appliance only | Fixed Appliances | Retraction of maxillary canines under the effect of a mechanical vibration simulation, and perception of pain in patients undergoing complete orthodontic treatment with extraction. | AcceleDent® device. Low-frequency vibration 30 Hz, 0.25 N, for 20 min per day. Timepoints: T0: day of initial canine retraction T1: 4 weeks after initiation canine retraction T2: 8 weeks after initiation canine retraction T3: 12 weeks after initiation canine retraction | Amount of tooth movement in CG vs. EG: 1.12 ± 0.22 mm vs. 1.39 ± 0.36 mm at T1. 2.59 ± 0.38 mm vs. 2.49 ± 0.76 mm at T2. 3.54 ± 0.24 mm vs. 3.37 ± 1.38 mm at T3. Rate of tooth movement: Overall tooth movement rate of 1.21 ± 0.32 mm/month for CG and 1.12 ± 0.20 mm/month for EG. 1.12 ± 0.22 mm/month (control) vs. 1.39 ± 0.36 mm/month (experimental) at T1. 1.47 ± 0.37 mm/month (control) vs. 0.93 ± 0.59 mm/month (experimental) at T2. 1.01 ± 0.31 mm/month (control) vs. 1.05 ± 0.71 mm/month (experimental) at T3. Level of pain: - Slightly higher in the EG on the 1st day. - Day 2: similar in the two groups. - Day 3: started to stay higher in the EG until day 6 (started to reduce to similar levels). | There were no statistically significant differences between the groups in the rate of retraction of the maxillary canines or in the pain perceived with the use of the mechanical vibration stimulation device. |
| Reiss et al., (2020) [26] | Randomized controlled trial | N = 40 Mean age 20.4 years. ♀ 20 ♂ 20 Groups: - EG: supplemental use of vibrational device with fixed appliances - CG: fixed appliances only | Fixed Appliances | Effect of additional vibratory force, in patients with fixed appliances, on biomarkers of bone remodelling, to study the RMAA and to study compliance with a vibrating appliance. | AcceleDent® device. Low-frequency vibration 30 Hz, 0.25 N, for 20 min per day. Timepoints: T0: baseline measurements T1: 4–6 weeks later T2: 10–12 weeks later T3: 15–18 weeks later | Mean first quartile and third quartile of irregularity and biomarkers including RANK/OPG ratio in the AcceleDent® and control group: - 7.24 at T0 vs. 8.96 at T0 - 4.26 at T1 vs. 5.24 at T1 - 2.33 at T2 vs. 2.96 at T2 - 0.97 at T3 vs. 1.22 at T3 The change did not significantly differ between groups. In the CG: Biomarkers level increased (remained similar in the EG). | No difference in the changes in salivary biomarkers of bone remodelling and no correlation was found between changes in irregularity and biomarker level. No association between RMAA and compliance with additional vibratory force. |
| Telatar et al., (2021) [34] | Randomized, controlled trial. | N = 20 ♀ 10 ♂ 10 Groups: - EG: AcceleDent® device with fixed appliances - CG: fixed appliances only | Fixed appliances | Evaluate the application of vibrational forces on the rate of canine distalization. | AcceleDent® device. Low-frequency vibration 30 Hz, 0.25 N, for 20 min per day. | In the EG, the average rate of tooth movement for the lower canines was 1.09 mm per month and 1.24 mm per month for the upper canines. In the CG, the average rate of tooth movement for the lower canines was 1.06 mm per month and 1.06 mm per month for the upper canines. Canine retraction rates were not different between groups. | No statistical difference between groups in the rate of canine retraction. |
| Mayama et al., (2022) [38] | Randomized controlled trial. | N = 25 Mean age 20.2 years. ♀ 21 ♂ 4 Groups: - EG: vibration with fixed appliance on one side of the upper arch - CG: fixed appliance on the other side of the upper arch | Fixed appliances. | Evaluate the effect and safety of supplementary vibrations on orthodontic movements. | Frequency of vibration 102.2 ± 2.6 Hz Force of 5.2 ± 0.5 g. 3 min per day. | - Mean amount of canine movement at each visit: 0.89 mm ± 0.55 mm in the CG group and 1.21 mm ± 0.60 mm in EG (significant difference). - Number of estimated visits for space closure: 6.38 ± 3.10 in CG and 4.61 ± 2.15 in EG. Number of visits in the EG was significantly less than in the CG. The difference between the two groups was 1.77 ± 4.65. - No patients complained of any pain during 3 min of vibration (supplemental) with static orthodontic force. - Evaluation of the VAS: no significant difference between the two groups. - Crown root ratio at the start of canine retraction was 0.59 ± 0.02 in the CG and 0.58 ± 0.02 in the EG. - Crown root ratio at the end of canine retraction was 0.59 ± 0.02 in the CG and 0.59 ± 0.02 in the EG. No significant difference was observed. | No statistically significant differences in pain, discomfort, and root resorption. Static orthodontic force with additional vibration ↑tooth movement (canine retraction), ↓number of visits |
| Akbar et al., (2022) [41] | Non-randomized clinical trial | N = 30 ♀ 20 ♂ 10 Groups: - EG: left side in the upper arch with vibration with fixed appliance - CG: right side in the upper arch only with fixed appliance | Fixed appliances. | Effect of localized vibration on the degree of retraction of the canines and evaluate the loss of anchorage. | Vibration by Oral B® electric toothbrush 240 Hz. 15 min per day. | - No discomfort was reported. - After 12 weeks of canine retraction: no difference in the amount of canine retraction between the groups. - Anchorage loss in the form of molar mesialization: present in both groups but with a difference insignificant. - Difference between the anchorage loss in the form of maxillary canine and 1sr molar rotation: statistically insignificant. | No statistically significant differences in the amount of canine movement; no difference in anchorage loss. |
| Bilello et al., (2022) [46] | Non-randomized Clinical trial | N = 20 Mean age 35 years. ♀ 75% Groups: - EG: 7-day aligner change regimen + AcceleDent® - CG: 14-day aligner change regimen, no supplemental vibration. | Aligners. | Investigate the effectiveness of AcceleDent® device when used during a clear aligner treatment. | AcceleDent® device. Low-frequency vibration 30 Hz, 0.25 N, for 20 min per day. | EG needed 41.1 ± 22.4 aligners on average. CG needed 33.1 ± 15.5 aligners. Difference between the two groups was not statistically significant. Treatment duration EG: 366 ± 187.4 days. Treatment duration CG: 509.3 ± 243.5 days. To complete the treatment, EG wore each aligner 9.0 ± 1 days and CG wore each aligner 15.4 ± 1.2 days. There is an average difference of 6.4 days per aligners, the difference is statistically significant. Pain perception: EG reported a VAS mean value of 2.4 ± 1 and CG a VAS mean value of 4.4 ± 1.4. | Using AcceleDent® device during a clear aligner treatment led to a successful, fast, and comfortable treatment, with reduction in pain perception, although they did not understand if the acceleration of treatment time could be attributed to the use of AcceleDent® or to the change regimen of the aligners. |
| Khera et al., (2022) [28] | Randomized controlled trial | N = 30 Aged between 18–25 years. Groups: - EG: Vibration side with fixed appliances - CG: fixed appliances only | Fixed appliances. | Investigate the effect of low-frequency vibration on the rate of canine retraction. | Customized vibratory device. Frequency of 30 Hz and force of 0.25 N. 20 min per day. Timepoints: T0: baseline. T1: 1st month. T2: 2nd month. T3: 3rd month. T4: 4th month. | This study showed a statistically non-significant difference between groups in the rate of canine retraction. | Low-frequency vibratory stimulation of 30 Hz with fixed orthodontic treatment did not significantly accelerate the rate of canine retraction. |
| Yildiz et al., (2023) [39] | Randomized controlled trial | N = 24 ♀ 8 ♂ 16 Mean age 15.07 Groups: CG: orthodontic force (split-mouth: one side with an activation only force, and the other side with an intermittent activation-deactivation-activation force) EG: orthodontic force (split-mouth) with AcceleDent® device | Fixed appliance with Hycon device | To achieve a synergistic effect between Hycon and AcceleDent® on the accelerating orthodontic tooth movement with the least possible root resorption. | AcceleDent® device. Low-frequency vibration 30 Hz, 0.25 N, for 20 min per day. | Intermittent force provided more effective and rapid canine distalization (statistically significant difference on both groups with or without vibration). Comparing the same activating protocol with vibration on the speed of tooth movement the results showed no significant difference. | The intermittent force was very effective in closing spaces. Vibration did not significantly affect orthodontic tooth movement rate. |
| ElMotaleb et al., (2024) [40] | Randomized controlled trial | N = 32 (64 canines) ♀ Age 15–21 years Groups: CG: fixed appliance only EG: fixed appliance and vibration device | Fixed appliance | Investigate the effectiveness of AcceleDent® vibrating device on the rate of canine retraction. | AcceleDent® device. Low-frequency vibration 30 Hz, 0.25 N, for 20 min per day. 4 months | No statistically significant difference between both groups regarding the total distance of canine retraction. No statistically significant difference between both groups regarding the rate of canine retraction per month. No statistically significant difference between both groups regarding pain level. Root condition was the same for both groups. | No evidence that AcceleDent® had any effect on acceleration of tooth movement. Pain level could not be reduced. Root condition was not affected. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pascoal, S.; Oliveira, S.; Ascione, M.; Pereira, J.; Carvalho, Ó.; Pinho, T. Effects of Vibration on Accelerating Orthodontic Tooth Movement in Clinical and In Vivo Studies: A Systematic Review. Dent. J. 2024, 12, 243. https://doi.org/10.3390/dj12080243
Pascoal S, Oliveira S, Ascione M, Pereira J, Carvalho Ó, Pinho T. Effects of Vibration on Accelerating Orthodontic Tooth Movement in Clinical and In Vivo Studies: A Systematic Review. Dentistry Journal. 2024; 12(8):243. https://doi.org/10.3390/dj12080243
Chicago/Turabian StylePascoal, Selma, Sofia Oliveira, Margaux Ascione, Jorge Pereira, Óscar Carvalho, and Teresa Pinho. 2024. "Effects of Vibration on Accelerating Orthodontic Tooth Movement in Clinical and In Vivo Studies: A Systematic Review" Dentistry Journal 12, no. 8: 243. https://doi.org/10.3390/dj12080243
APA StylePascoal, S., Oliveira, S., Ascione, M., Pereira, J., Carvalho, Ó., & Pinho, T. (2024). Effects of Vibration on Accelerating Orthodontic Tooth Movement in Clinical and In Vivo Studies: A Systematic Review. Dentistry Journal, 12(8), 243. https://doi.org/10.3390/dj12080243








