Oral Health-Related Quality of Life of Hong Kong Kindergarten Children Receiving Silver Diamine Fluoride Therapy
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Clinical Assessment
2.3. Parental Questionnaires
2.4. Statistical Analysis
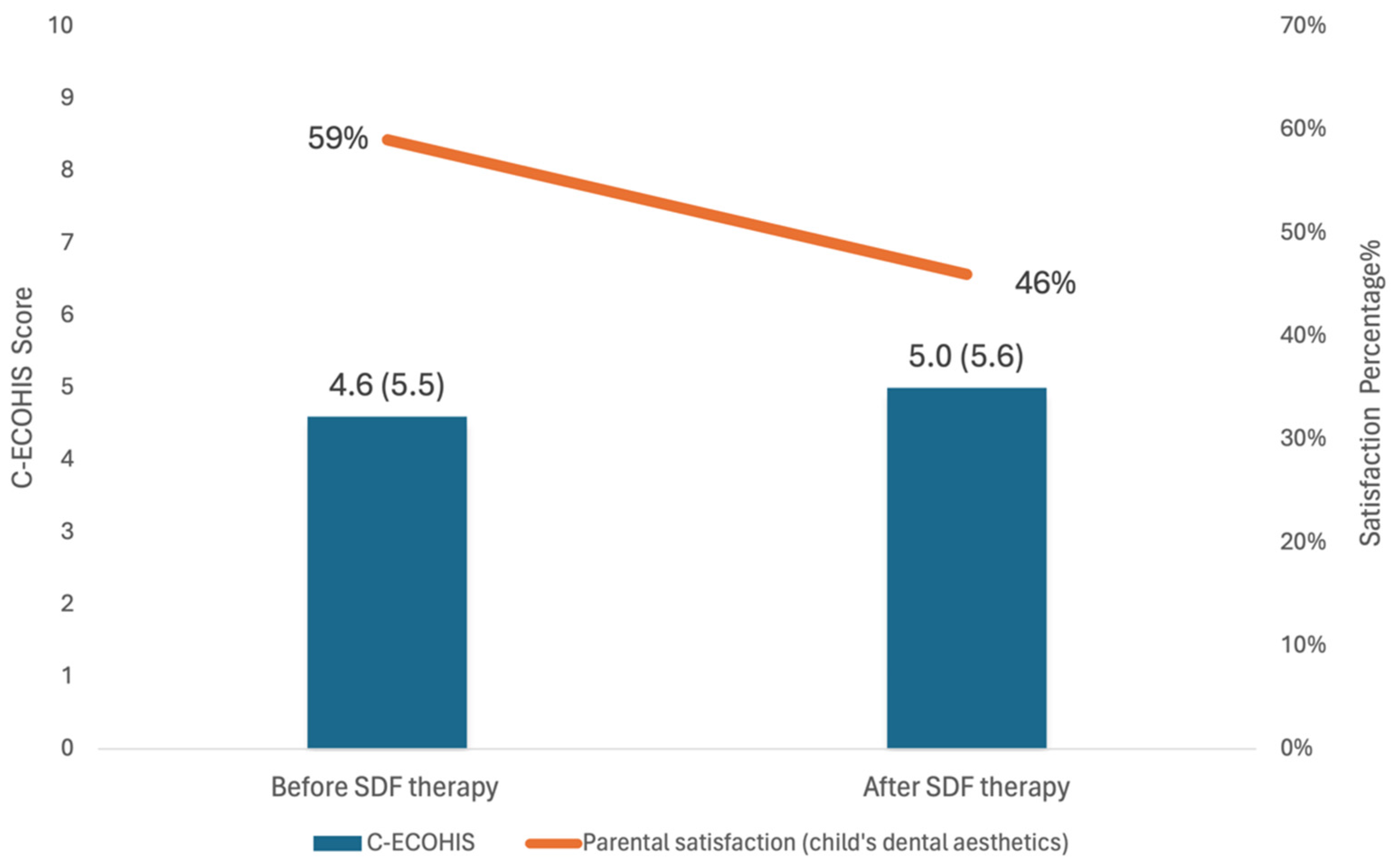
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- American Academy of Pediatric Dentistry. Policy on early childhood caries (ECC): Consequences and preventive strategies. Ref. Man. Pediatr. Dent. Chic. III Am. Acad. Pediatr. Dent. 2021, 81–84. [Google Scholar]
- Uribe, S.E.; Innes, N.; Maldupa, I. The global prevalence of early childhood caries: A systematic review with meta-analysis using the WHO diagnostic criteria. Int. J. Paediatr. Dent. 2021, 31, 817–830. [Google Scholar] [CrossRef]
- Chen, J.; Duangthip, D.; Gao, S.S.; Huang, F.; Anthonappa, R.; Oliveira, B.H.; Turton, B.; Durward, C.; El Tantawi, M.; Attia, D.; et al. Oral Health Policies to Tackle the Burden of Early Childhood Caries: A Review of 14 Countries/Regions. Front. Oral Health 2021, 2, 670154. [Google Scholar] [CrossRef]
- Allen, P.F. Assessment of oral health related quality of life. Health Qual. Life Outcomes 2003, 1, 40. [Google Scholar] [CrossRef]
- Chai, H.H.; Gao, S.S.; Chen, K.J.; Lo, E.C.M.; Duangthip, D.; Chu, C.H. Tools Evaluating Child Oral Health-Related Quality of Life. Int. Dent. J. 2024, 74, 15–24. [Google Scholar] [CrossRef]
- Bennadi, D.; Reddy, C.V. Oral health related quality of life. J. Int. Soc. Prev. Community Dent. 2013, 3, 1–6. [Google Scholar] [CrossRef]
- McGrath, C.; Broder, H.; Wilson-Genderson, M. Assessing the impact of oral health on the life quality of children: Implications for research and practice. Community Dent. Oral. Epidemiol. 2004, 32, 81–85. [Google Scholar] [CrossRef]
- Eiser, C.; Mohay, H.; Morse, R. The measurement of quality of life in young children. Child. Care Health Dev. 2000, 26, 401–414. [Google Scholar] [CrossRef]
- Pahel, B.T.; Rozier, R.G.; Slade, G.D. Parental perceptions of children’s oral health: The Early Childhood Oral Health Impact Scale (ECOHIS). Health Qual. Life Outcomes 2007, 5, 6. [Google Scholar] [CrossRef]
- Lee, G.H.; McGrath, C.; Yiu, C.K.; King, N.M. Translation and validation of a Chinese language version of the Early Childhood Oral Health Impact Scale (ECOHIS). Int. J. Paediatr. Dent. 2009, 19, 399–405. [Google Scholar] [CrossRef]
- Oral Health Education Division; Department of Health; The Government of the Hong Kong Special Administration Regio. Brighter Smiles Playland. Available online: https://www.toothclub.gov.hk/en/en_play_instruction.html (accessed on 8 June 2024).
- Gao, S.S.; Chen, K.J.; Duangthip, D.; Lo, E.C.M.; Chu, C.H. Oral Health Care in Hong Kong. Healthcare 2018, 6, 45. [Google Scholar] [CrossRef]
- Duangthip, D.; Chen, K.J.; Gao, S.S.; Lo, E.C.M.; Chu, C.H. Early childhood caries among 3- to 5-year-old children in Hong Kong. Int. Dent. J. 2019, 69, 230–236. [Google Scholar] [CrossRef]
- Zheng, F.M.; Yan, I.G.; Duangthip, D.; Gao, S.; Lo, E.C.M.; Chu, C.H. Silver diamine fluoride therapy for dental care. Jpn. Dent. Sci. Rev. 2022, 58, 249–257. [Google Scholar] [CrossRef]
- Anant, N.; Rai, N.; Nr, S.; Amaltas, P.; Kalambe, M.; Emmanuel, A. Assessing the Effects and Acceptance of Silver Diamine Fluoride Treatment in Early Childhood Caries. Cureus 2024, 16, e55767. [Google Scholar] [CrossRef]
- Chai, H.H.; Gao, S.S.; Chen, K.; Duangthip, D.; Lo, E.C.M.; Chu, C.H. A Kindergarten-Based Oral Health Preventive Approach for Hong Kong Preschool Children. Healthcare 2020, 8, 545. [Google Scholar] [CrossRef]
- Alazmah, A. Early Childhood Caries: A Review. J. Contemp. Dent. Pract. 2017, 18, 732–737. [Google Scholar] [CrossRef]
- Magno, M.; Silva, L.; Ferreira, D.; Barja-Fidalgo, F.; Gonçalves, A. Aesthetic perception, acceptability and satisfaction in the treatment of caries lesions with silver diamine fluoride: A scoping review. Int. J. Paediatr. Dent. 2019, 29, 257–266. [Google Scholar] [CrossRef]
- Rutherford, A. ANOVA and ANCOVA: A GLM Approach; John Wiley & Sons: Hoboken, NJ, USA, 2011. [Google Scholar]
- Weinberg, S.L.; Abramowitz, S.K. Statistics Using SPSS: An Integrative Approach; Cambridge University Press: Cambridge, UK, 2008. [Google Scholar]
- Duangthip, D.; Gao, S.S.; Chen, K.J.; Lo, E.C.M.; Chu, C.H. Oral health-related quality of life and caries experience of Hong Kong preschool children. Int. Dent. J. 2020, 70, 100–107. [Google Scholar] [CrossRef]
- Duangthip, D.; Gao, S.; Chen, K.J.; Lo, E.C.M.; Chu, C.H. Oral health-related quality of life of preschool children receiving silver diamine fluoride therapy: A prospective 6-month study. J. Dent. 2019, 81, 27–32. [Google Scholar] [CrossRef]
- Sihra, R.; Schroth, R.J.; Bertone, M.; Martin, H.; Patterson, B.; Mittermuller, B.A.; Lee, V.; Patterson, B.; Moffatt, M.E.; Klus, B.; et al. The Effectiveness of Silver Diamine Fluoride and Fluoride Varnish in Arresting Caries in Young Children and Associated Oral Health-Related Quality of Life. J. Can. Dent. Assoc. 2020, 86, k9. [Google Scholar]
- Ruff, R.R.; Whittemore, R.; Grochecki, M.; Bateson, J.; Barry Godín, T.J. Silver diamine fluoride and oral health-related quality of life: A review and network meta-analysis. PLoS ONE 2022, 17, e0261627. [Google Scholar] [CrossRef] [PubMed]
- Almarwan, M.; Almawash, A.; AlBrekan, A.; Albluwi, S. Parental Acceptance for the Use of Silver Diamine Fluoride on Their Special Health Care-Needs Child’s Primary and Permanent Teeth. Clin. Cosmet. Investig. Dent. 2021, 13, 195–200. [Google Scholar] [CrossRef]
- Crystal, Y.; Kreider, B.; Raveis, V. Parental Expressed Concerns about Silver Diamine Fluoride (SDF) Treatment. J. Clin. Pediatr. Dent. 2019, 43, 155–160. [Google Scholar] [CrossRef] [PubMed]
- Crystal, Y.O.; Marghalani, A.A.; Ureles, S.D.; Wright, J.T.; Sulyanto, R.; Divaris, K.; Fontana, M.; Graham, L. Use of Silver Diamine Fluoride for Dental Caries Management in Children and Adolescents, Including Those with Special Health Care Needs. Pediatr. Dent. 2017, 39, 135–145. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization Model List of Essential Medicines—22nd List, 2021; World Health Organization: Geneva, Switzerland, 2021.
- Chai, H.H.; Chen, K.J.; Duangthip, D.; Lo, E.C.M.; Chu, C.H.; Gao, S.S. Parental perspectives on the use of silver diamine fluoride therapy to arrest early childhood caries in kindergarten outreach dental services: A qualitative study. J. Dent. 2022, 125, 104250. [Google Scholar] [CrossRef]
- Amalia, R.; Schaub, R.M.H.; Stewart, R.E.; Widyanti, N.; Groothoff, J.W. Impact of school-based dental program performance on the oral health-related quality of life in children. J. Investig. Clin. Dent. 2017, 8, e12179. [Google Scholar] [CrossRef]
| Social Demographic Background | No. (%) | Mean C-ECOHIS (SD) | p Value 1 |
|---|---|---|---|
| Age | 0.202 | ||
| 3 years old | 93 (44) | 3.9 (4.8) | |
| 4 years old | 118 (56) | 5.2 (6.0) | |
| Sex | 0.692 | ||
| Female | 101 (48) | 4.4 (5.7) | |
| Male | 110 (52) | 4.8 (5.5) | |
| Mother had tertiary education | 0.789 | ||
| Yes | 87 (41) | 4.2 (4.9) | |
| No | 124 (59) | 4.9 (6.0) | |
| Father had tertiary education | 0.970 | ||
| Yes | 86 (41) | 4.4 (5.0) | |
| No | 125 (59) | 4.8 (5.9) | |
| Family income above the median | 0.452 | ||
| Yes | 114 (54) | 4.3 (5.2) | |
| No | 97 (46) | 5.0 (5.9) | |
| Oral health habits | No. (%) | Mean C-ECOHIS (SD) | p Value 1 |
| Daily tooth brushing habits | 0.283 | ||
| <2 times/day | 91 (43) | 4.2 (5.0) | |
| ≥2 times/day | 120 (57) | 5.0 (6.0) | |
| Daily snacking habits | 0.007 | ||
| Yes | 169 (80) | 5.0 (5.7) | |
| No | 42 (20) | 3.0 (4.5) | |
| Bottle-feeding habits | 0.627 | ||
| Yes | 65 (31) | 4.5 (5.7) | |
| No | 146 (69) | 4.7 (5.5) | |
| Oral health status | Mean (SD) | Spearman’s rank correlation coefficient | p Value 2 |
| Caries experience (dmft) | 3.9 (3.0) | 0.289 | <0.001 |
| Oral hygiene (VPI) | 0.5 (0.2) | −0.085 | 0.220 |
| Items | Incidence Rate Ratio | 95% CI | p Value |
|---|---|---|---|
| Daily snacking habits | |||
| Yes | 1.66 | 0.96–2.85 | 0.069 |
| No a | |||
| Caries experience (dmft) | 1.12 | 1.07–1.18 | <0.001 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chai, H.H.; Sun, I.G.; Duangthip, D.; Gao, S.S.; Lo, E.C.M.; Chu, C.H. Oral Health-Related Quality of Life of Hong Kong Kindergarten Children Receiving Silver Diamine Fluoride Therapy. Dent. J. 2024, 12, 248. https://doi.org/10.3390/dj12080248
Chai HH, Sun IG, Duangthip D, Gao SS, Lo ECM, Chu CH. Oral Health-Related Quality of Life of Hong Kong Kindergarten Children Receiving Silver Diamine Fluoride Therapy. Dentistry Journal. 2024; 12(8):248. https://doi.org/10.3390/dj12080248
Chicago/Turabian StyleChai, Hollis Haotian, Ivy Guofang Sun, Duangporn Duangthip, Sherry Shiqian Gao, Edward Chin Man Lo, and Chun Hung Chu. 2024. "Oral Health-Related Quality of Life of Hong Kong Kindergarten Children Receiving Silver Diamine Fluoride Therapy" Dentistry Journal 12, no. 8: 248. https://doi.org/10.3390/dj12080248
APA StyleChai, H. H., Sun, I. G., Duangthip, D., Gao, S. S., Lo, E. C. M., & Chu, C. H. (2024). Oral Health-Related Quality of Life of Hong Kong Kindergarten Children Receiving Silver Diamine Fluoride Therapy. Dentistry Journal, 12(8), 248. https://doi.org/10.3390/dj12080248









