Influence of Direct Coronal Restoration Materials on the Fracture Resistance of Endodontically Treated Premolars: An In Vitro Study
Abstract
:1. Introduction
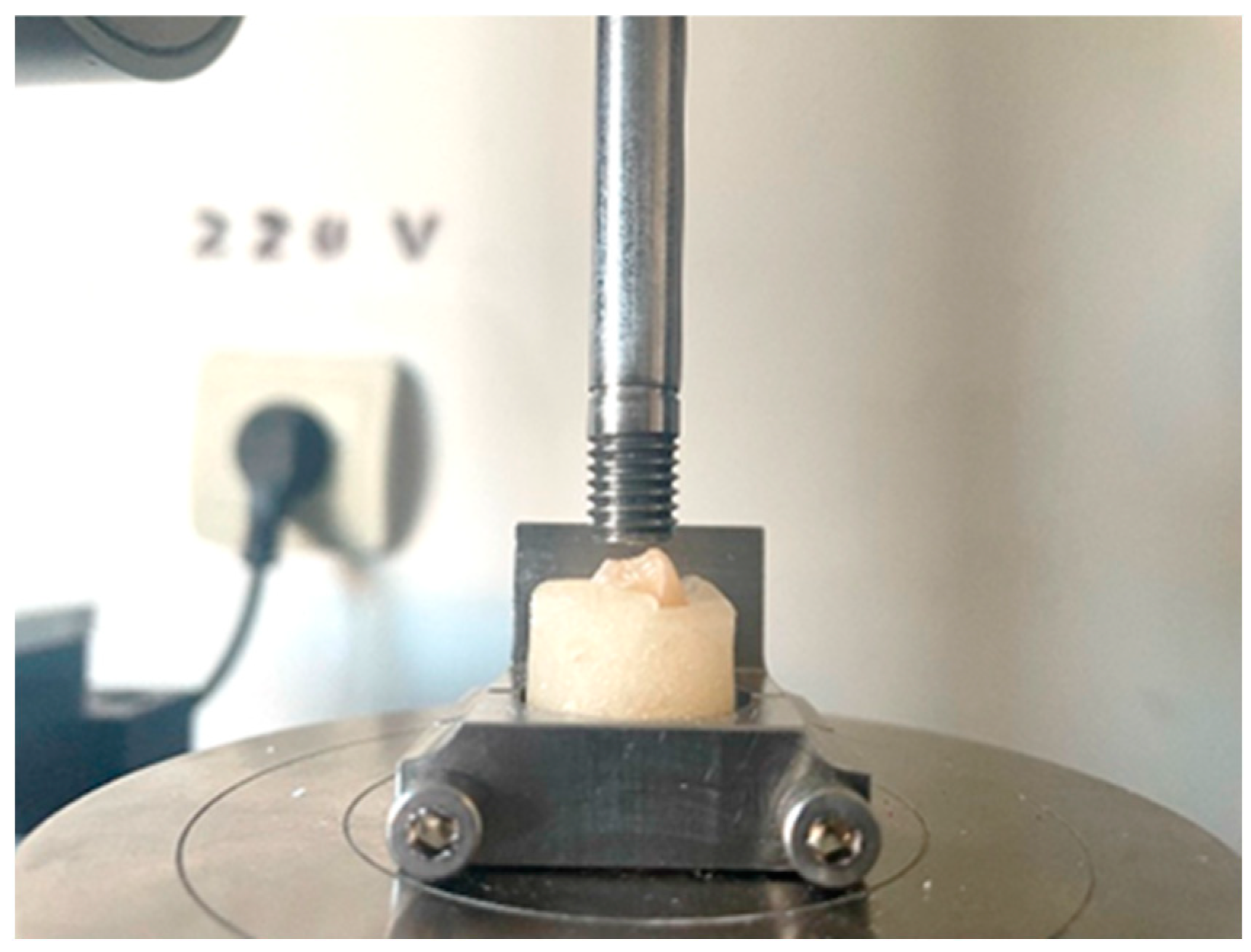
2. Materials and Methods
- Group 1: intact teeth used as negative control;
- Group 2: teeth with MOD cavities and endodontic treatment but left unrestored, used as positive control;
- Group 3: teeth with endodontic treatment and MOD cavities restored with Tetric Power Flow and Tetric EvoCeram. Before every restoration, a SuperMat Adapt Super Cap Matrix system (Kerr Hawe SA, Bioggio, Switzerland) was placed around the tooth structure. An etching gel containing 37% phosphoric acid (Total Etch, Ivoclar Vivadent AG, Schaan, Liechtenstein) was applied on the enamel and subsequently on the dentin and allowed a reaction time of 15 s. Afterwards, the phosphoric acid was thoroughly rinsed off with water spray and the tooth surfaces dried with oil-free air, avoiding excessive drying of the dentin. The cavity walls were bonded with Adhese Universal (Ivoclar Vivadent AC, Liechtenstein). After scrubbing the adhesive onto the tooth surface for 20 s, compressed air was used to disperse it, resulting in a glossy, immobile film layer, that was light-cured for 10 s with Bluephase G4 (Ivoclar Vivadent AG, Liechtenstein). Tetric PowerFlow (Ivoclar Vivadent AG, Liechtenstein) was applied in layers of 4 mm thickness, adapted to the cavity walls with a suitable instrument (probe) then light-cured for 10 s. For the final layer of 2 mm, Tetric EvoCeram was used with a suitable instrument and light-cured for 10 s. At the end, the finishing and polishing procedures were performed under water cooling once the matrix was removed;
- Group 4: teeth with endodontic treatment and MOD cavities restored with Multicore and Tetric EvoCeram. After etching and bonding, as was conducted in Group 3, MultiCore Flow (Ivoclar Vivadent AG, Liechtenstein) using the intra-oral tip was directly placed into the cavity and light-cured for 10 s. The final layer of 2 mm was filled in the same way as in Group 3, and the final steps were the same as for Group 3;
- Group 5: teeth with endodontic treatment and MOD cavities restored only with MultiCore Flow. The etching and bonding procedures were conducted as for Group 3, then MultiCore Flow filled the entire cavity and was light-cured, with the matrix removal being followed by the polishing procedure.
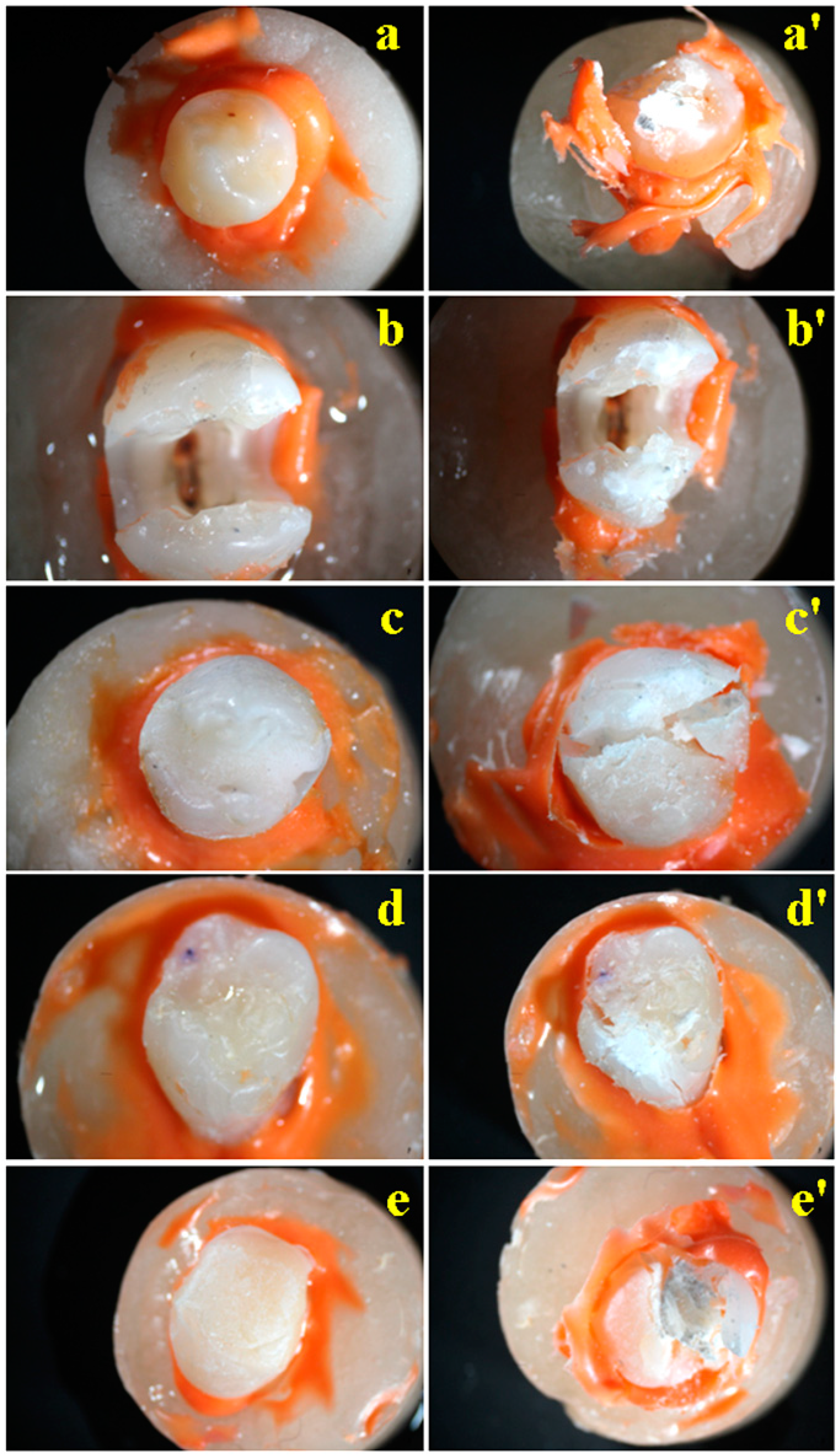
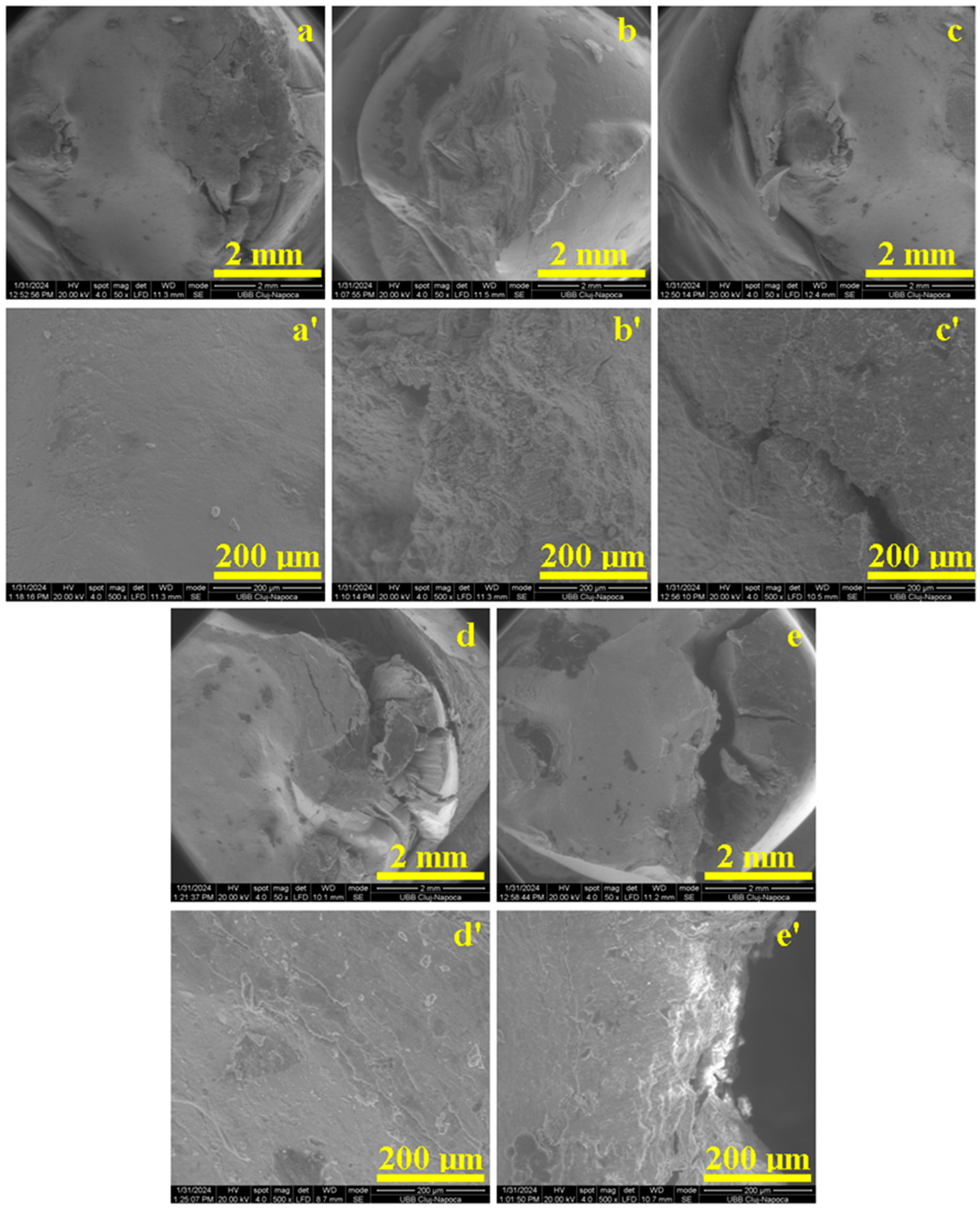
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Burke, F.J. Tooth fracture in vivo and in vitro. J. Dent. 1986, 20, 131–139. [Google Scholar] [CrossRef]
- Santos, J.M.; Palma, P.J.; Ramos, J.C.; Cabrita, A.S.; Friedman, S. Periapical inflammation subsequent to coronal inoculation of dog teeth root filled with resilon/epiphany in 1 or 2 treatment sessions with chlorhexidine medication. J. Endod. 2014, 40, 837–841. [Google Scholar] [CrossRef]
- Plotino, G. (Ed.) Minimally Invasive Approaches in Endodontic Practice; Springer: Cham, Switzerland, 2021; ISBN 978-3-030-45866-9. [Google Scholar]
- Gambarini, G.; Galli, M.; Morese, A.; Abduljabbar, F.; Seracchiani, M.; Stefanelli, L.V.; Giovarruscio, M.; Di Nardo, D.; Testarelli, L. Digital Design of Minimally Invasive Endodontic Access Cavity. Appl. Sci. 2020, 10, 3513. [Google Scholar] [CrossRef]
- Puleio, F.; Lo Giudice, G.; Militi, A.; Bellezza, U.; Lo Giudice, R. Does Low-Taper Root Canal Shaping Decrease the Risk of Root Fracture? A Systematic Review. Dent. J. 2022, 10, 94. [Google Scholar] [CrossRef]
- Tang, W.; Wu, Y.; Smales, R.J. Identifying and reducing risks for potential fractures in endodontically treated teeth. J. Endod. 2010, 36, 609–617. [Google Scholar] [CrossRef]
- Panitvisai, P.; Messer, H.H. Cuspal deflection in molars in relation to endodontic and restorative procedures. J. Endod. 1995, 21, 57–61. [Google Scholar] [CrossRef]
- Smith, J.; Doe, A. Onlays vs. Crowns in MOD Restorations: A Comparative Study. J. Dent. Res. 2024, 12, 345–356. [Google Scholar]
- Fan, J.; Xu, Y.; Si, L.; Li, X.; Fu, B.; Hannig, M. Long-term Clinical Performance of Composite Resin or Ceramic Inlays, Onlays, and Overlays: A Systematic Review and Meta-analysis. Oper. Dent. 2021, 46, 25–44. [Google Scholar] [CrossRef]
- Ozan, G.; Eren, M.M.; Dikmen, B.; Yildiz, E. Fracture Resistance of Endodontically Treated Premolars Restored with CAD-CAM Onlays. Am. J. Dent. 2022, 35, 308–314. [Google Scholar] [PubMed]
- Caussin, E.; Izart, M.; Ceinos, R.; Attal, J.-P.; Beres, F.; François, P. Advanced Material Strategy for Restoring Damaged Endodontically Treated Teeth: A Comprehensive Review. Materials 2024, 17, 3736. [Google Scholar] [CrossRef]
- Kumar, A.; Sarthaj, S. In Vitro Evaluation of Fracture Resistance of Endodontically treated Teeth restored with Bulk-fill, Bulk-fill Flowable, Fiber-reinforced, and Conventional Resin Composite. J. Oper. Dent. Endod. 2018, 3, 12–17. [Google Scholar]
- Mergulhão, V.A.; de Mendonça, L.S.; de Albuquerque, M.S.; Braz, R. Fracture Resistance of Endodontically Treated Maxillary Premolars Restored With Different Methods. Oper. Dent. 2019, 44, E1–E11. [Google Scholar] [CrossRef] [PubMed]
- AlJarboua, R.T.; Alshihry, R.A.; Alkhaldi, H.O.; Al Marar, F.H.; Aljaffary, M.A.; Almana, M.L.; Balhaddad, A.A.; Alkhateeb, O. Effect of Fiber-Reinforced Composite Placement Site on Fracture Resistance of Premolar Teeth: An in vitro Study. Clin. Cosmet. Investig. Dent. 2024, 16, 255–266. [Google Scholar] [CrossRef]
- Chen, Y.; Chen, D.; Ding, H.; Meng, X. Fatigue Behavior of Endodontically Treated Maxillary Premolars with MOD Defects under Different Minimally Invasive Restorations. Clin. Oral Investig. 2022, 26, 197–206. [Google Scholar] [CrossRef]
- Moosavi, H.; Zeynali, M.; Pour, Z.H. Fracture Resistance of Premolars Restored by Various Types and Placements Techniques of Resin Composites. Int. J. Dent. 2012, 2012, 973641. [Google Scholar] [CrossRef]
- Atiyah, A.H.; Baban, L.M. Fracture resistance of endodontically treated premolars with extensive MOD cavities restored with different composite restorations. An In Vitro study. J. Baghdad Coll. Dent. 2014, 26, 7–15. [Google Scholar] [CrossRef]
- Forster, A.; Braunitzer, G.; Tóth, M.; Szabó, B.P.; Fráter, M. In Vitro fracture resistance of adhesively restored molar teeth with different MOD cavity dimensions. J. Prosthodont. 2019, 28, e325–e331. [Google Scholar] [CrossRef]
- Sharma, A.; Amirtharaj, L.V.; Sanjeev, K.; Mahalaxmi, S. Fracture resistance of Endodontically treated Premolars restored with Flowable Short Fibre-Reinforced Resin Composite—An In Vitro Study. Eur. Endod. J. 2022, 7, 161. [Google Scholar]
- Sarabi, N.; Taji, H.; Jalayer, J.; Ghaffari, N.; Forghani, M. Fracture resistance and failure mode of endodontically treated premolars restored with different adhesive restorations. J. Dent. Mater. Tech. 2015, 4, 13–20. [Google Scholar]
- Santos, M.J.; Bezerra, R.B. Fracture resistance of maxillary premolars restored with direct and indirect adhesive techniques. J. Can. Dent. Assoc. 2005, 71, 585. [Google Scholar]
- Mincik, J.; Urban, D.; Timkova, S.; Urban, R. Fracture resistance of endodontically treated maxillary premolars restored by various direct filling materials: An in vitro study. Int. J. Biomater. 2016, 2016, 9138945. [Google Scholar] [CrossRef] [PubMed]
- Naik, A.; de Ataide, I.D.; Fernandes, M. Fracture resistance of Endodontically treated premolars using Nanohybrid Composite, Fiber-Reinforced Composite, Horizontal Glass Fiber posts, and ceramic inlays: An In Vitro Study. J. Endod. 2023, 49, 1739–1746. [Google Scholar] [CrossRef] [PubMed]
- Abdel-Maksoud, H.B.; Eid, B.M.; Hamdy, M. Optimizing fracture resistance of endodontically treated maxillary premolars restored with preheated thermos-viscous composite post-thermocycling, a comparative study. Part I. BMC Oral Health 2024, 24, 295. [Google Scholar] [CrossRef]
- Spinhayer, L.; Bui, A.T.B.; Leprince, J.G.; Hardy, C.M.F. Core build-up resin composites: An in-vitro comparative study. Biomater. Investig. Dent. 2020, 7, 159–166. [Google Scholar] [CrossRef]
- Kumar, G.; Shivrayan, A. Comparative study of mechanical properties of direct core build-up materials. Contemp. Clin. Dent. 2015, 6, 16–20. [Google Scholar]
- Nakade, P.; Bangar, B.R.; Thaore, S.; Jankar, A.S.; Wadhwani, M.; Joteppa, V. Comparative Evaluation of Fracture Toughness and Flexural Strength of Four Different Core Build up Materials an In Vitro Study. J. Res. Med. Dent. Sci. 2023, 11, 099–104. [Google Scholar]
- Isufi, A.; Plotino, G.; Grande, N.; Ioppolo, P.; Testarelli, L.; Bedini, R.; Al-Sudani, D.; Gambarini, G. Fracture resistance of endodontically treated teeth restored with a bulkfill flowable material and a resin composite. Ann. Stomatol. 2016, 7, 4–10. [Google Scholar] [CrossRef]
- Yasa, B.; Arslan, H.; Yasa, E.; Akcay, M.; Hatirli, H. Effect of novel restorative materials and retention slots on fracture resistance of endodontically-treated teeth. Acta Odontol. Scand. 2016, 74, 96–102. [Google Scholar] [CrossRef]
- Alaa, H.; Abbas, Z.; Abdulameer, M. Effect of Different Restoration Designs on Fracture Strength of Endodontically Treated Teeth Weakened with MOD Cavities. J. Res. Med. Dent. Sci. 2021, 9, 190–196. [Google Scholar]
- Habekost, L.V.; Camacho, G.B.; Azevedo, E.C.; Demarco, F.F. Fracture resistance of thermal cycled and endodontically treated premolars with adhesive restorations. J. Prosthet. Dent. 2007, 98, 186–192. [Google Scholar] [CrossRef] [PubMed]
- Karzoun, W.; Abdulkarim, A.; Samran, A.; Kern, M. Fracture strength of endodontically treated maxillary premolars supported by a horizontal glass fiber post: An in vitro study. J. Endod. 2015, 41, 907–912. [Google Scholar] [CrossRef]
- Rohym, S.; Badra, H.; Nassar, H. Comparative Evaluation of Marginal Adaptation and Fatigue Resistance of Endodontically Treated Premolars Restored with Direct and Indirect Coronal Restorations: An in vitro Study. BMC Oral Health 2024, 24, 696. [Google Scholar] [CrossRef]

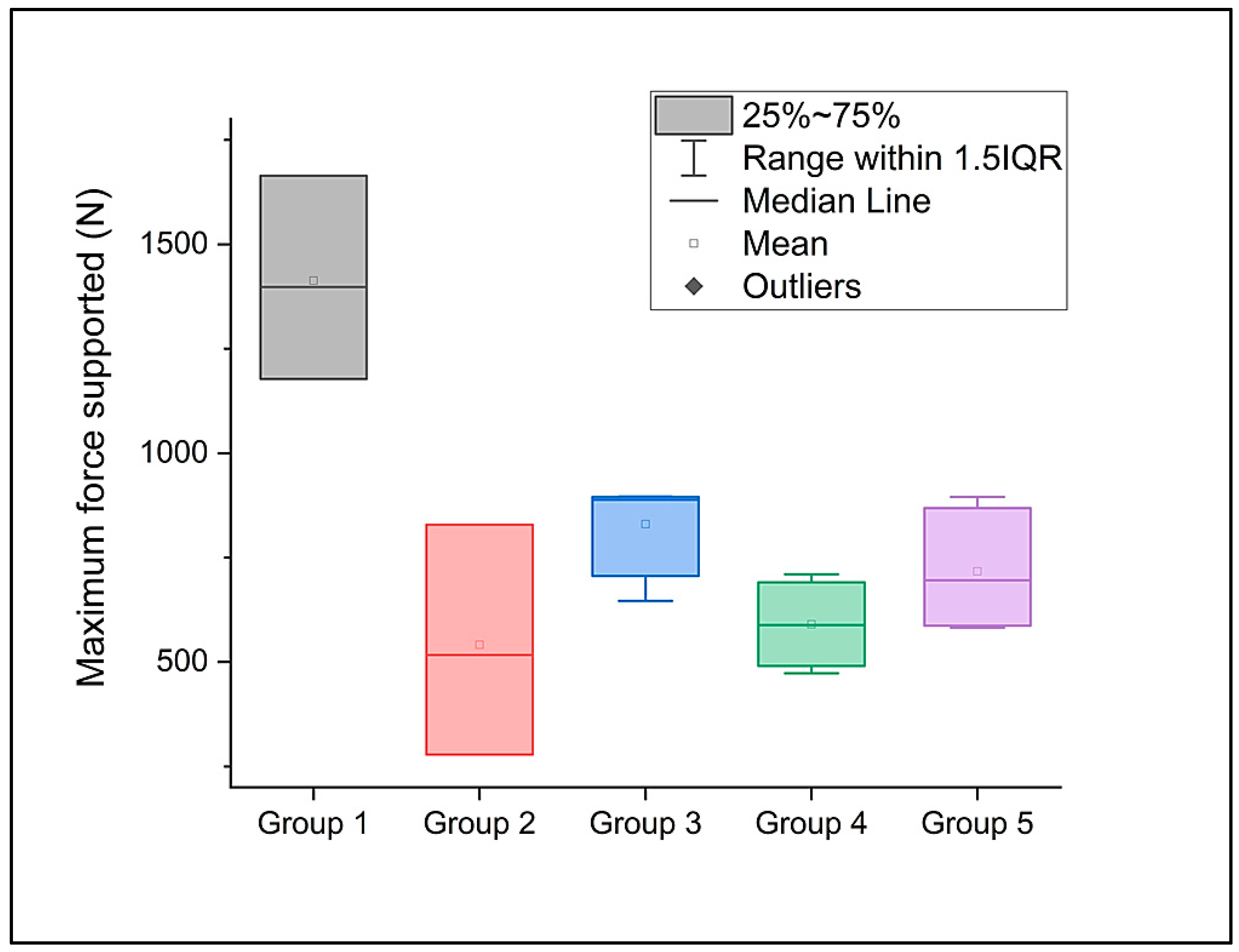
| Group | Compressive Strength (MPa) | Maximum Force Supported (N) | |
|---|---|---|---|
| 1 | Mean | 25.23273 | 1413.03281 |
| Standard deviation | 4.35149 | 243.68338 | |
| 2 | Mean | 15.77553 | 541.34753 |
| Standard deviation | 3.56558 | 276.01193 | |
| 3 | Mean | 276.01193 | 829.9073 |
| Standard deviation | 276.01193 | 122.60253 | |
| 4 | Mean | 122.60253 | 590.00804 |
| Standard deviation | 2.28742 | 103.32499 | |
| 5 | Mean | 13.47568 | 717.00178 |
| Standard deviation | 2.32245 | 150.90633 | |
| Sum of Squares | Mean Square | F Value | Prob > F | |
|---|---|---|---|---|
| Model | 312.70978 | 78.17744 | 10.04156 | 6.24644 × 10−4 |
| Error | 101.21002 | 7.78539 | ||
| Total | 413.9198 |
| Sum of Squares | Mean Square | F Value | Prob > F | |
|---|---|---|---|---|
| Model | 1,535,643.58363 | 383,910.89591 | 11.98083 | 2.66559 × 10−4 |
| Error | 416,568.81433 | 32,043.75495 | ||
| Total | 1,952,212.39795 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gheorghe, G.F.; Țâncu, A.M.C.; Amza, O.E.; Suciu, I.; Iosif, L.; Cuc, S.; Petean, I.; Moldovan, M.; Dimitriu, B. Influence of Direct Coronal Restoration Materials on the Fracture Resistance of Endodontically Treated Premolars: An In Vitro Study. Dent. J. 2024, 12, 294. https://doi.org/10.3390/dj12090294
Gheorghe GF, Țâncu AMC, Amza OE, Suciu I, Iosif L, Cuc S, Petean I, Moldovan M, Dimitriu B. Influence of Direct Coronal Restoration Materials on the Fracture Resistance of Endodontically Treated Premolars: An In Vitro Study. Dentistry Journal. 2024; 12(9):294. https://doi.org/10.3390/dj12090294
Chicago/Turabian StyleGheorghe, Georgiana Florentina, Ana Maria Cristina Țâncu, Oana Elena Amza, Ioana Suciu, Laura Iosif, Stanca Cuc, Ioan Petean, Marioara Moldovan, and Bogdan Dimitriu. 2024. "Influence of Direct Coronal Restoration Materials on the Fracture Resistance of Endodontically Treated Premolars: An In Vitro Study" Dentistry Journal 12, no. 9: 294. https://doi.org/10.3390/dj12090294
APA StyleGheorghe, G. F., Țâncu, A. M. C., Amza, O. E., Suciu, I., Iosif, L., Cuc, S., Petean, I., Moldovan, M., & Dimitriu, B. (2024). Influence of Direct Coronal Restoration Materials on the Fracture Resistance of Endodontically Treated Premolars: An In Vitro Study. Dentistry Journal, 12(9), 294. https://doi.org/10.3390/dj12090294







