The Influence of Posterior Class II Composite Restoration Location and Techniques on Marginal Sealing
Abstract
1. Introduction
2. Materials and Methods
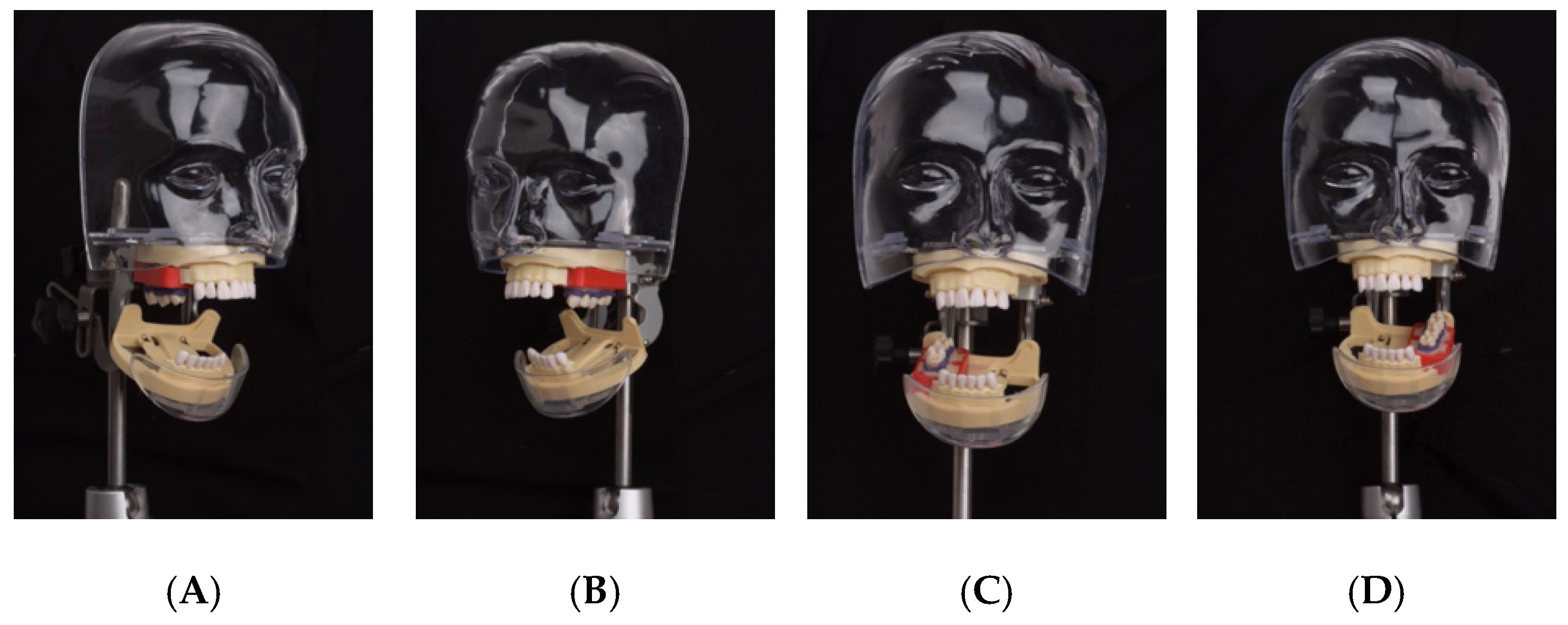
Teeth Holder
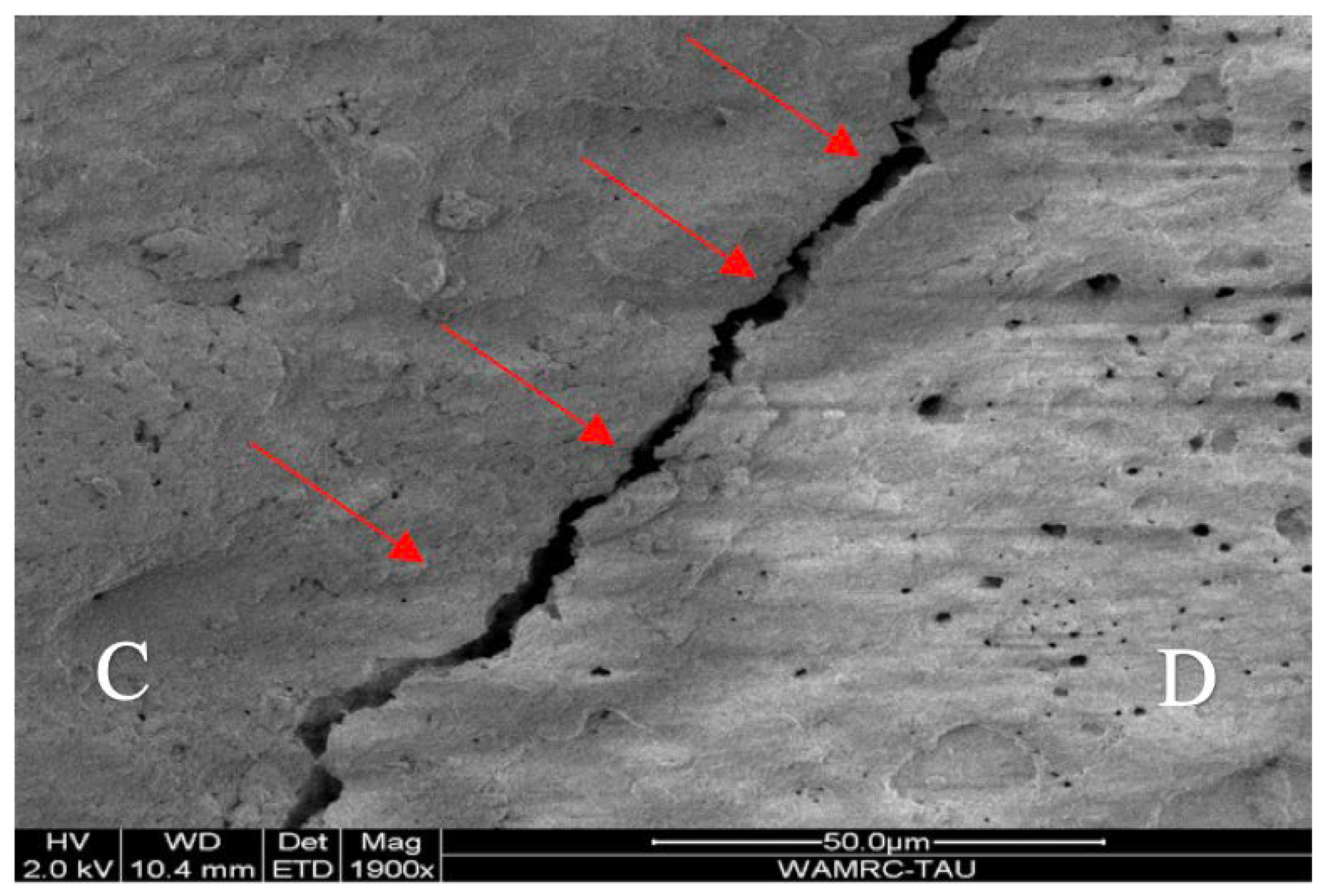
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Bohaty, B.S.; Ye, Q.; Misra, A.; Sene, F.; Spencer, P. Posterior composite restoration update: Focus on factors influencing form and function. Clin. Cosmet. Investig. Dent. 2013, 5, 33–42. [Google Scholar] [CrossRef] [PubMed]
- Manhart, J.; Kunzelmann, K.H.; Chen, H.Y.; Hickel, R. Mechanical properties of new composite restorative materials. J. Biomed. Mater. Res. 2000, 53, 353–361. [Google Scholar] [CrossRef]
- Türkün, L.S.; Türkün, M.; Ozata, F. Two-year clinical evaluation of a packable resin-based composites. J. Am. Dent. Assoc. 2003, 134, 1205–1212. [Google Scholar] [CrossRef] [PubMed]
- Qamar, Z.; Fatima, T. Comparative review of various flowable composites. J. Pak. Dent. Assoc. 2014, 23, 11–14. [Google Scholar]
- Attar, N.; Tam, L.E.; McComb, D. Flow, strength, stiffness and radiopacity of flowable resin composites. J. Can. Dent. Assoc. 2003, 69, 516–521. [Google Scholar] [PubMed]
- Baroudi, K.; Rodrigues, J.C. Flowable Resin Composites: A systematic review and clinical considerations. J. Clin. Diagn. Res. 2015, 9, ZE18–ZE24. [Google Scholar] [CrossRef] [PubMed]
- Bayne, S.C.; Thompson, J.Y.; Swift, E.J., Jr.; Stamatiades, P.; Wilkerson, M. A characterization of first-generation flowable composites. J. Am. Dent. Assoc. 1998, 129, 567–577. [Google Scholar] [CrossRef]
- Reddy, S.N.; Jayashankar, D.N.; Nainan, M.; Shivanna, V. The effect of flowable composite lining thickness with various curing techniques on microleakage in class II composite restorations: An in vitro study. J. Contemp. Dent. Pract. 2013, 14, 56–60. [Google Scholar] [CrossRef]
- Roulet, J.F. Marginal integrity: Clinical significance. J. Dent. 1994, 22 (Suppl. S1), S9–S12. [Google Scholar] [CrossRef] [PubMed]
- Rodrigues Junior, S.A.; Pin, L.F.; Machado, G.; Della Bona, A.; Demarco, F.F. Influence of different restorative techniques on marginal seal of class II composite restorations. J. Appl. Oral Sci. 2010, 18, 37–43. [Google Scholar] [CrossRef] [PubMed]
- Muliyar, S.; Shameem, K.A.; Thankachan, R.P.; Francis, P.G.; Jayapalan, C.S.; Hafiz, K.A. Microleakage in endodontics. J. Int. Oral Health 2014, 6, 99–104. [Google Scholar] [PubMed]
- Chuang, S.F.; Jin, Y.T.; Liu, J.K.; Chang, C.H.; Shieh, D.B. Influence of flowable composite lining thickness on Class II composite restorations. Oper. Dent. 2004, 29, 301–308. [Google Scholar] [PubMed]
- Bore Gowda, V.; Sreenivasa Murthy, B.V.; Hegde, S.; Venkataramanaswamy, S.D.; Pai, V.S.; Krishna, R. Evaluation of gingival microleakage in Class II composite restorations with different lining techniques: An in vitro study. Scientifica 2015, 1, 896507. [Google Scholar] [CrossRef] [PubMed]
- Cavalcanti, A.N.; Mitsui, F.H.; Silva, F.; Peris, A.R.; Bedran-Russo, A.; Marchi, G.M. Effect of cyclic loading on the bond strength of class II restorations with different composite materials. Oper. Dent. 2008, 33, 163–168. [Google Scholar] [CrossRef] [PubMed]
- Kermanshah, H.; Yasini, E.; Hoseinifar, R. Effect of cyclic loading on microleakage of silorane based composite compared with low shrinkage methacrylate-based composites. Dent. Res. J. 2016, 13, 264–271. [Google Scholar] [CrossRef]
- Jang, K.T.; Chung, D.H.; Shin, D.; García-Godoy, F. Effect of eccentric load cycling on microleakage of Class V flowable and packable composite resin restorations. Oper. Dent. 2001, 26, 603–608. [Google Scholar]
- Scotti, N.; Comba, A.; Gambino, A.; Paolino, D.S.; Alovisi, M.; Pasqualini, D.; Berutti, E. Microleakage at enamel and dentin margins with a bulk fills flowable resin. Eur. J. Dent. 2014, 8, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Peutzfeldt, A.; Mühlebach, S.; Lussi, A.; Flury, S. Marginal Gap formation in approximal “bulk fill” resin composite restorations after artificial ageing. Oper. Dent. 2018, 43, 180–189. [Google Scholar] [CrossRef] [PubMed]
- Demarco, F.F.; Corrêa, M.B.; Cenci, M.S.; Moraes, R.R.; Opdam, N.J. Longevity of posterior composite restorations: Not only a matter of materials. Dent. Mater. 2012, 28, 87–101. [Google Scholar] [CrossRef]
- Amaral, F.L.; Colucci, V.; Palma-Dibb, R.G.; Corona, S.A. Assessment of in vitro methods used to promote adhesive interface degradation: A critical review. J. Esthet. Restor. Dent. 2007, 19, 340–354. [Google Scholar] [CrossRef] [PubMed]
- Papia, E.; Larsson, C.; du Toit, M.; Vult von Steyern, P. Bonding between oxide ceramics and adhesive cement systems: A systematic review. J. Biomed. Mater. Res. Part B Appl. Biomater. 2014, 102, 395–413. [Google Scholar] [CrossRef] [PubMed]
- Da Rosa Rodolpho, P.A.; Donassollo, T.A.; Cenci, M.S.; Loguércio, A.D.; Moraes, R.R.; Bronkhorst, E.M.; Opdam, N.J.; Demarco, F.F. 22-Year clinical evaluation of the performance of two posterior composites with different filler characteristics. Dent. Mater. 2011, 27, 955–963. [Google Scholar] [CrossRef]
- Pallesen, U.; van Dijken, J.W.; Halken, J.; Hallonsten, A.L.; Höigaard, R. Longevity of posterior resin composite restorations in permanent teeth in Public Dental Health Service: A prospective 8 years follow up. J. Dent. 2013, 41, 297–306. [Google Scholar] [CrossRef]
- Palotie, U.; Eronen, A.K.; Vehkalahti, K.; Vehkalahti, M.M. Longevity of 2- and 3-surface restorations in posterior teeth of 25- to 30-year-olds attending Public Dental Service-A 13-year observation. J. Dent. 2017, 62, 13–17. [Google Scholar] [CrossRef] [PubMed]
- van de Sande, F.H.; Moraes, R.R.; Elias, R.V.; Montagner, A.F.; Rodolpho, P.A.; Demarco, F.F.; Cenci, M.S. Is composite repair suitable for anterior restorations? A long-term practice-based clinical study. Clin. Oral Investig. 2019, 23, 2795–2803. [Google Scholar] [CrossRef]
- Lucarotti, P.S.; Holder, R.L.; Burke, F.J. Outcome of direct restorations placed within the general dental services in England and Wales (Part 1): Variation by type of restoration and re-intervention. J. Dent. 2005, 33, 805–815. [Google Scholar] [CrossRef] [PubMed]
- Mobarak, E.; El-Deeb, H.; Daifalla, L.E.; Ghaly, M.; Mustafa, M.; Sabry, D.; Fatah, H.; Mulder, J.; Creugers, N.H.J.; Frencken, J.E. Survival of multiple-surface ART restorations using a zinc-reinforced glass-ionomer restorative after 2 years: A randomized triple-blind clinical trial. Dent. Mater. 2019, 35, e185–e192. [Google Scholar] [CrossRef]
- Pedram, P.; Hooshmand, T.; Heidari, S. Effect of Different Cavity Lining Techniques on Marginal Sealing of Class II Resin Composite Restorations In Vitro. Int. J. Periodontics Restor. Dent. 2018, 38, 895–901. [Google Scholar] [CrossRef] [PubMed]
- Nair, B.G.; Rao, S.S. The effect of flowable composite lining thickness with various curing techniques on internal voids in Class II composite restorations—An Invitro Study. Ann. Essences Dent. 2011, 3, 22–26. [Google Scholar]
- Braga, R.R.; Hilton, T.J.; Ferracane, J.L. Contraction stress of flowable composite materials and their efficacy as stress-relieving layers. J. Am. Dent. Assoc. 2003, 134, 721–728. [Google Scholar] [CrossRef] [PubMed]
- Moosavi, H.; Maleknejad, F.; Forghani, M.; Afshari, E. Evaluating resin-dentin bond by microtensile bond strength test: Effects of various resin composites and placement techniques. Open Dent. J. 2015, 9, 409–413. [Google Scholar] [CrossRef] [PubMed]
- Silva, P.F.D.; Oliveira, L.R.S.; Braga, S.S.L.; Signori, C.; Armstrong, S.R.; Soares, C.J.; Cenci, M.S.; Faria-E-Silva, A.L. Effect of selective carious tissue removal on biomechanical behavior of class II bulk-fill dental composite restorations. Dent. Mater. 2018, 34, 1289–1298. [Google Scholar] [CrossRef]
- Brosh, T.; Davidovitch, M.; Berg, A.; Shenhav, A.; Pilo, R.; Matalon, S. Influence of practitioner-related placement variables on the compressive properties of Bulk-Fill composite resins—An in vitro clinical simulation Study. Materials 2022, 15, 4305. [Google Scholar] [CrossRef] [PubMed]
- Wahab, F.K.; Shaini, F.J. Evaluation of the microleakage at the proximal walls of Class II cavities restored using resin composite and precured composite inserts. Quintessence Int. 2003, 34, 600–606. [Google Scholar]
- Lucarotti, P.S.; Holder, R.L.; Burke, F.J. Outcome of direct restorations placed within the general dental services in England and Wales (Part 3): Variation by dentist factors. J. Dent. 2005, 33, 827–835. [Google Scholar] [CrossRef]
- Khalil Elgohary, M.; Abdulrazek, H.; Haggag, K.M. Effect of Monolithic Zirconia vs. Gold Alloy on the Wear of Human Enamel: An in vitro study. Al-Azhar J. Dent. Sci. 2018, 21, 253–260. [Google Scholar] [CrossRef]
- Alvarez-Arenal, A.; Gonzalez-Gonzalez, I.; deLlanos-Lanchares, H.; Brizuela-Velasco, A.; Pinés-Hueso, J.; Ellakuria-Echebarria, J. Retention strength after compressive cyclic loading of five luting agents used in implant-supported prostheses. BioMed Res. Int. 2016, 2016, 2107027. [Google Scholar] [CrossRef] [PubMed]
- Dietschi, D.; Argente, A.; Krejci, I.; Mandikos, M. In vitro performance of Class I and II composite restorations: A literature review on nondestructive laboratory trials-part I. Oper. Dent. 2013, 38, E166–E181. [Google Scholar] [CrossRef]


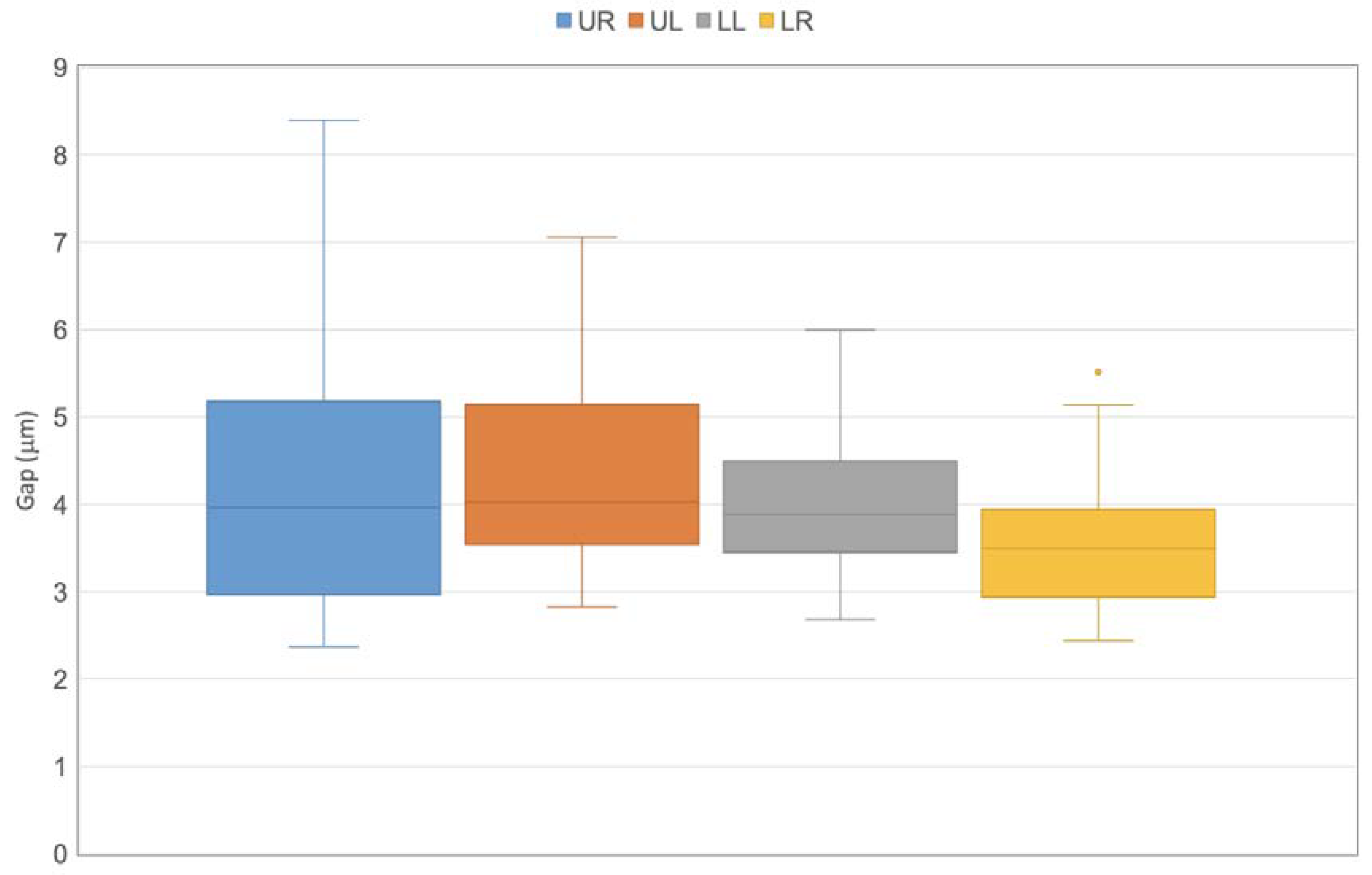
|
|
|
|
|
|
|
|
|
| Method | N | Mean (µm) | Std. Deviation (µm) | p |
|---|---|---|---|---|
| Pre-cure | 47 | 4.197 | 1.838 | >0.212 |
| Co-cure | 45 | 4.035 | 1.503 | |
| Mesial | 47 | 4.098 | 1.479 | >0.443 |
| Distal | 45 | 4.140 | 1.890 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Haddad, M.; Lugassy, D.; Barhum, M.; Brosh, T.; Matalon, S. The Influence of Posterior Class II Composite Restoration Location and Techniques on Marginal Sealing. Dent. J. 2025, 13, 39. https://doi.org/10.3390/dj13010039
Haddad M, Lugassy D, Barhum M, Brosh T, Matalon S. The Influence of Posterior Class II Composite Restoration Location and Techniques on Marginal Sealing. Dentistry Journal. 2025; 13(1):39. https://doi.org/10.3390/dj13010039
Chicago/Turabian StyleHaddad, Mishel, Diva Lugassy, Mohana Barhum, Tamar Brosh, and Shlomo Matalon. 2025. "The Influence of Posterior Class II Composite Restoration Location and Techniques on Marginal Sealing" Dentistry Journal 13, no. 1: 39. https://doi.org/10.3390/dj13010039
APA StyleHaddad, M., Lugassy, D., Barhum, M., Brosh, T., & Matalon, S. (2025). The Influence of Posterior Class II Composite Restoration Location and Techniques on Marginal Sealing. Dentistry Journal, 13(1), 39. https://doi.org/10.3390/dj13010039







