MAMA—Mandibular Advancement Magnetic Appliance: A Digital Workflow and a CAD–CAM Development of a New Mandibular Advancement Device for the Treatment of Obstructive Sleep Apnea Syndrome
Abstract
1. Introduction
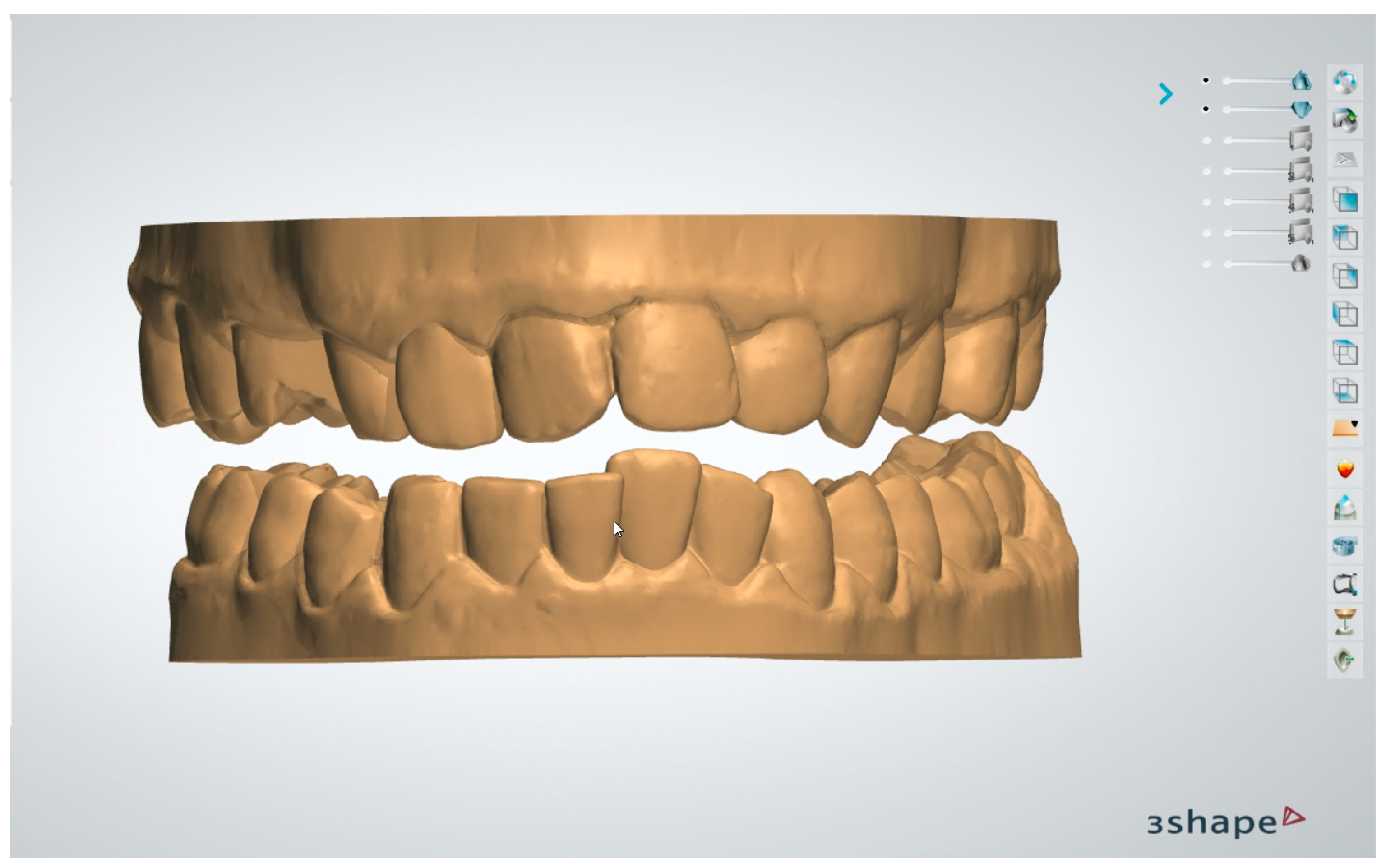
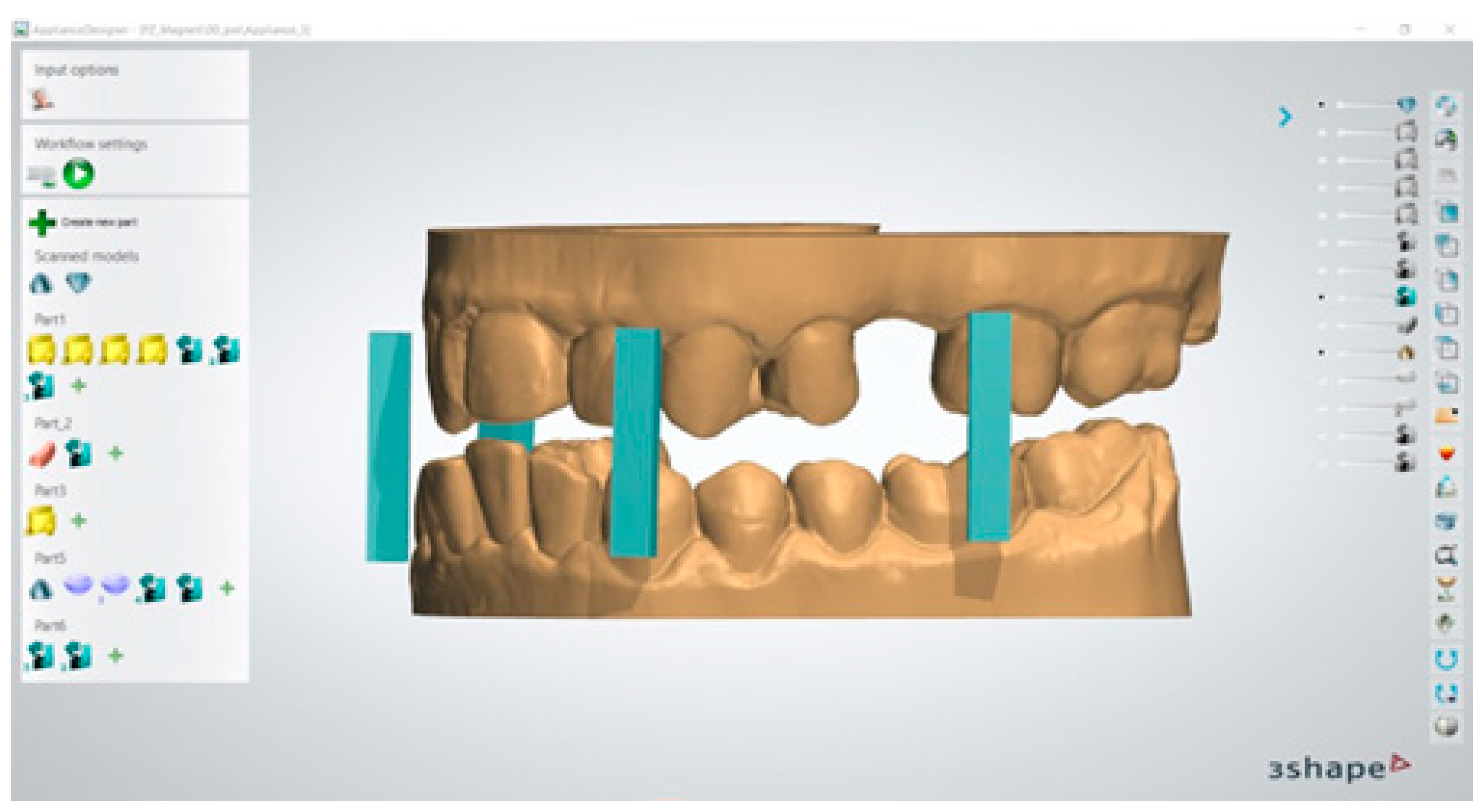
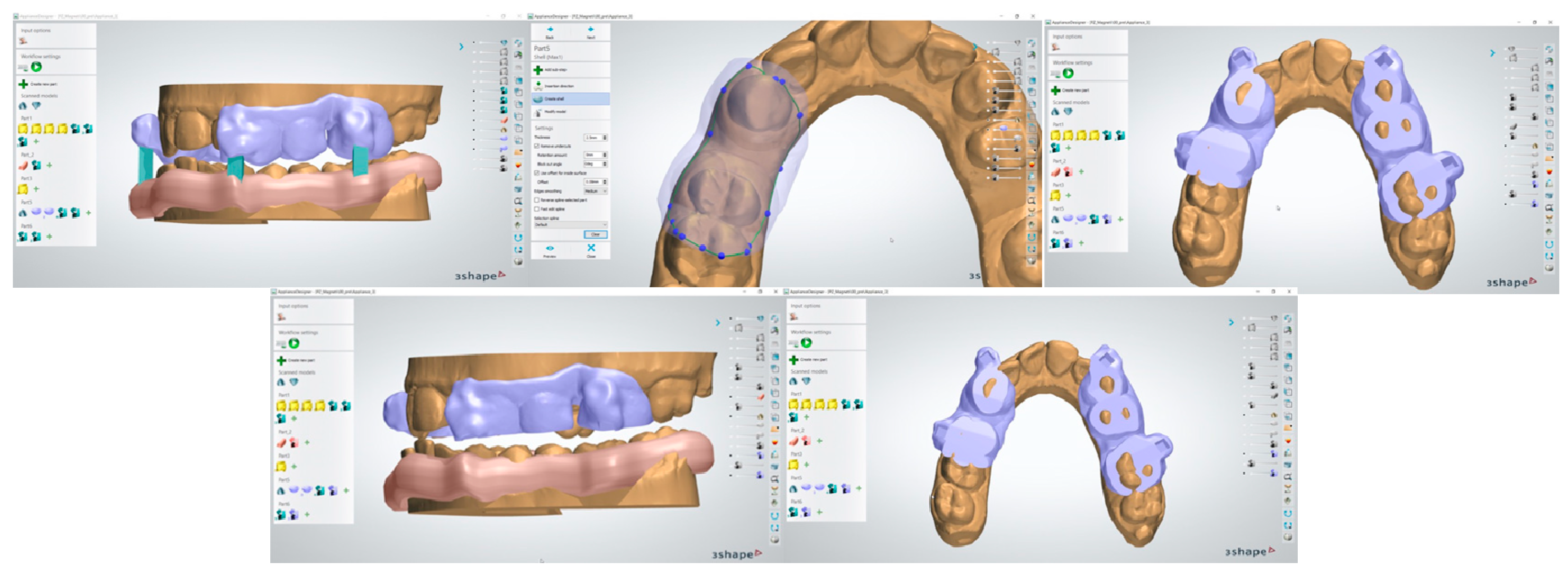
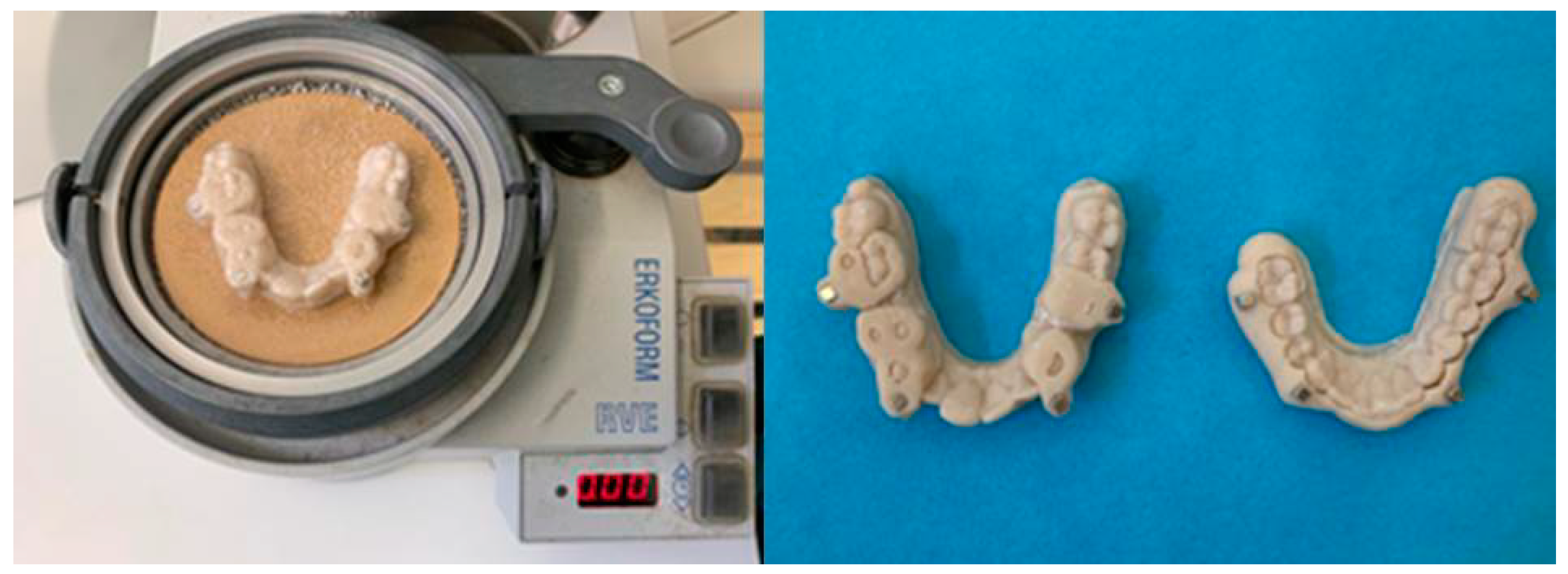
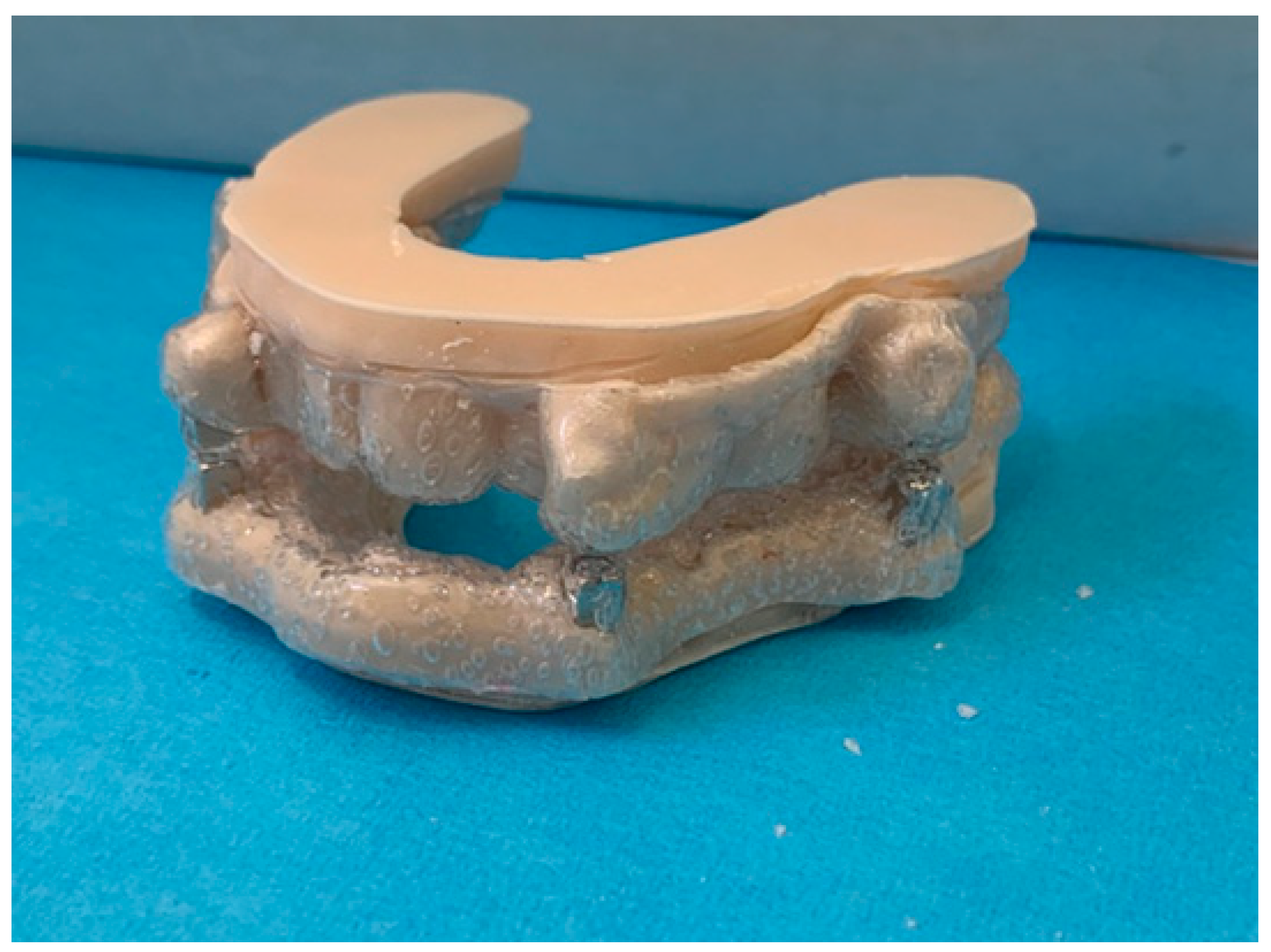
2. Materials and Methods
3. Results
4. Discussion
5. Conclusions
- The digital workflow proposed in this study appears to be effective and efficient for the design of a magnetic advancement device;
- CAD–CAM technology allows us to make an individualized device for each patient with a high degree of precision;
- The original workflow proposed by the authors allows clinicians to develop the apparatus directly in the practice.
6. Patents
Author Contributions
Funding
Data Availability Statement
Conflicts of Interest
References
- Sateia, M.J. International classification of sleep disorders-third edition: Highlights and modification. Chest 2014, 146, 1387–1394. [Google Scholar] [CrossRef]
- Maspero, C.; Giannini, L.; Galbiati, G.; Rosso, G.; Farronato, G. Obstructive sleep apnea syndrome: A literature review. Minerva Stomatol. 2015, 64, 97–109. [Google Scholar] [PubMed]
- Young, T.; Evans, L.; Finn, L.; Palta, M. Estimation of the clinically diagnosed proportion of sleep apnea syndrome in middle-aged men and women. Sleep 1997, 20, 705–706. [Google Scholar] [CrossRef] [PubMed]
- Marcus, C.L.; Brooks, L.J.; Draper, K.A. Diagnosis and management of childhood obstructive sleep apnea syndrome. Pediatrics 2012, 130, 576–584. [Google Scholar] [CrossRef]
- Xu, T.; You, D.; Chen, X. Non-surgical treatment of obstructive sleep apnea syndrome. Eur. Arch. Otorhinolaryngol. 2018, 275, 335–346. [Google Scholar]
- Loução-de-Amorim, I.; Bentes, C.; Peralta, A.R. Men and women with chronic insomnia disorder and OSAS: Different responses to CPAP. Sleep. Sci. 2019, 12, 190–195. [Google Scholar] [CrossRef]
- Serra Torres, S.; Bellott Arcis, C.; Montiel Company, J.L.; Marco Algarra, J.; Almerich Silla, J.M. Effectiveness of mandibular advancement appliances in treating obstructive sleep apnea syndrome: A systematic review. Laryngoscope 2016, 126, 507–514. [Google Scholar] [CrossRef]
- Kapur, V.; Auckley, D.H.; Chowdhuri, S.; Kuhlmann, D.; Mehra, R.; Ramar, K.; Harrod, C.G. Clinical Practice Guideline for Diagnostic Testing for Adult Obstructive Sleep Apnea: An American Academy of Sleep Medicine Clinical Practice Guideline. J. Clin. Sleep. Med. 2017, 13, 479–504. [Google Scholar] [CrossRef]
- Ping, L.; Xiao-Hui, N.; Hua, L.; Ning, Z.; Yan-Feng, G.; Fen, P. Continuous positive airway pressure versus mandibular advancement device in the treatment of obstructive sleep apnea: A systematic review and meta-analysis. Sleep. Med. 2020, 72, 5–11. [Google Scholar]
- Jindal, P.; Juneja, M.; Siena, F.; Bajaj, D.; Breedon, P. Mechanical and geometric properties of thermoformed and 3D printed clear dental aligners. Am. J. Orthod. Dentofac. Orthop. 2019, 156, 694–701. [Google Scholar] [CrossRef]
- Casavola, C.; Pappalettera, G.; Pappalettere, C.; Patronelli, M.; Renna, G.; Laurenziello, M.; Ciavarella, D. A full-field DIC analysis of the mechanical-deformation behavior of polyethylene terephthalate glycol (PET-G) aligners. J. Mech. Behav. Biomed. Mater. 2022, 134, 105391. [Google Scholar] [CrossRef]
- Iliadi, A.; Koletsi, D.; Eliades, T. Forces and moments generated by aligner-type appliances for orthodontic tooth movement: A systematic review and meta-analysis. Orthod. Craniofac Res. 2019, 22, 248–258. [Google Scholar] [CrossRef] [PubMed]
- Shirey, N.; Mendonca, G.; Groth, C.; Berman, H. Comparison of mechanical properties of 3-dimensional printed and thermoformed orthodontic aligners. Am. J. Orthod. Dentofac. Orthop. 2023, 163, 720–728. [Google Scholar] [CrossRef] [PubMed]
- Zinelis, S.; Panayi, N.; Polychronis, G.; Papageorgiou, S.; Eliades, T. Comparative analysis of mechanical properties of orthodontic aligners produced by different contemporary 3D printers. Orthod. Craniofac Res. 2022, 25, 336–341. [Google Scholar] [CrossRef] [PubMed]
- Lombardo, L.; Martines, E.; Mazzanti, V.; Arreghini, A.; Mollica, F.; Siciliani, G. Stress relaxation properties of four orthodontic aligner materials: A 24-hour in vitro study. Angle Orthod. 2017, 87, 11–18. [Google Scholar] [CrossRef]
- Skaik, A.; Wei, X.; Abusamak, I.; Iddi, I. Effects of time and clear aligner removal frequency on the force delivered by different polyethylene terephthalate glycol-modified materials determined with thin-film pressure sensors. Am. J. Orthod. Dentofac. Orthop. 2019, 155, 98–107. [Google Scholar] [CrossRef]
- Ahn, H.; Lee, S.; Yu, H.; Park, J.; Kim, K.; Kim, S. Force Distribution of a Novel Core-Reinforced Multilayered Mandibular Advancement Device. Sensors 2021, 21, 3383. [Google Scholar] [CrossRef]
- Elkholy, F.; Schmidt, S.; Schmidt, F.; Amirkhani, M.; Lapatki, B. Force decay of polyethylene terephthalate glycol aligner materials during simulation of typical clinical loading/unloading scenarios. J. Orofac. Orthop. 2023, 84, 189–201. [Google Scholar] [CrossRef] [PubMed]
- Nicita, F.; D’Amico, C.; Filardi, V.; Spadaro, D.; Aquilio, E.; Mancini, M.; Fiorillo, L. Chemical-Physical Characterization of PET-G-Based Material for Orthodontic Use: Preliminary Evaluation of micro-Raman Analysis. Eur. J. Dent. 2024, 18, 228–235. [Google Scholar] [CrossRef] [PubMed]
- Ihssen, B.; Willmann, J.; Nimer, A.; Drescher, D. Effect of in vitro aging by water immersion and thermocycling on the mechanical properties of PETG aligner material. J. Orofac. Orthop. 2019, 80, 292–303. [Google Scholar] [CrossRef]
- Bernard, G.; Rompré, P.; Tavares, J.R.; Montpetit, A. Colorimetric and spectrophotometric measurements of orthodontic thermoplastic aligners exposed to various staining sources and cleaning methods. Head. Face Med. 2020, 16, 2. [Google Scholar] [CrossRef] [PubMed]
- Porojan, L.; Vasiliu, R.; Porojan, S.; Bîrdeanu, M. Surface Quality Evaluation of Removable Thermoplastic Dental Appliances Related to Staining Beverages and Cleaning Agents. Polymers 2020, 12, 1736. [Google Scholar] [CrossRef]
- Vardimon, A.D.; Graber, T.M.; Voss, L.R.; Muller, T.P. Functional orthopedic magnetic appliance (FOMA) III--modus operandi. Am. J. Orthod. Dentofac. Orthop. 1990, 97, 135–148. [Google Scholar] [CrossRef]
- Nalabothu, P.; Verna, C.; Steineck, M.; Mueller, A.A.; Dalstra, M. The biomechanical evaluation of magnetic forces to drive osteogenesis in newborn’s with cleft lip and palate. J. Mater. Sci. Mater. Med. 2020, 31, 79. [Google Scholar] [CrossRef] [PubMed]




Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Nucera, R.; Nastro Siniscalchi, E.; Consolo, G.; Calabrese, L.; Caccamo, D.; Bellocchio, A.M.; Portelli, M. MAMA—Mandibular Advancement Magnetic Appliance: A Digital Workflow and a CAD–CAM Development of a New Mandibular Advancement Device for the Treatment of Obstructive Sleep Apnea Syndrome. Dent. J. 2025, 13, 104. https://doi.org/10.3390/dj13030104
Nucera R, Nastro Siniscalchi E, Consolo G, Calabrese L, Caccamo D, Bellocchio AM, Portelli M. MAMA—Mandibular Advancement Magnetic Appliance: A Digital Workflow and a CAD–CAM Development of a New Mandibular Advancement Device for the Treatment of Obstructive Sleep Apnea Syndrome. Dentistry Journal. 2025; 13(3):104. https://doi.org/10.3390/dj13030104
Chicago/Turabian StyleNucera, Riccardo, Enrico Nastro Siniscalchi, Giancarlo Consolo, Luigi Calabrese, Daniela Caccamo, Angela Mirea Bellocchio, and Marco Portelli. 2025. "MAMA—Mandibular Advancement Magnetic Appliance: A Digital Workflow and a CAD–CAM Development of a New Mandibular Advancement Device for the Treatment of Obstructive Sleep Apnea Syndrome" Dentistry Journal 13, no. 3: 104. https://doi.org/10.3390/dj13030104
APA StyleNucera, R., Nastro Siniscalchi, E., Consolo, G., Calabrese, L., Caccamo, D., Bellocchio, A. M., & Portelli, M. (2025). MAMA—Mandibular Advancement Magnetic Appliance: A Digital Workflow and a CAD–CAM Development of a New Mandibular Advancement Device for the Treatment of Obstructive Sleep Apnea Syndrome. Dentistry Journal, 13(3), 104. https://doi.org/10.3390/dj13030104









