Interfacial Effects Between Dental Impression and Die Materials and Their Role in the Internal Fit of Indirect Resin-Based Composite Restorations
Abstract
:1. Introduction
2. Materials and Methods
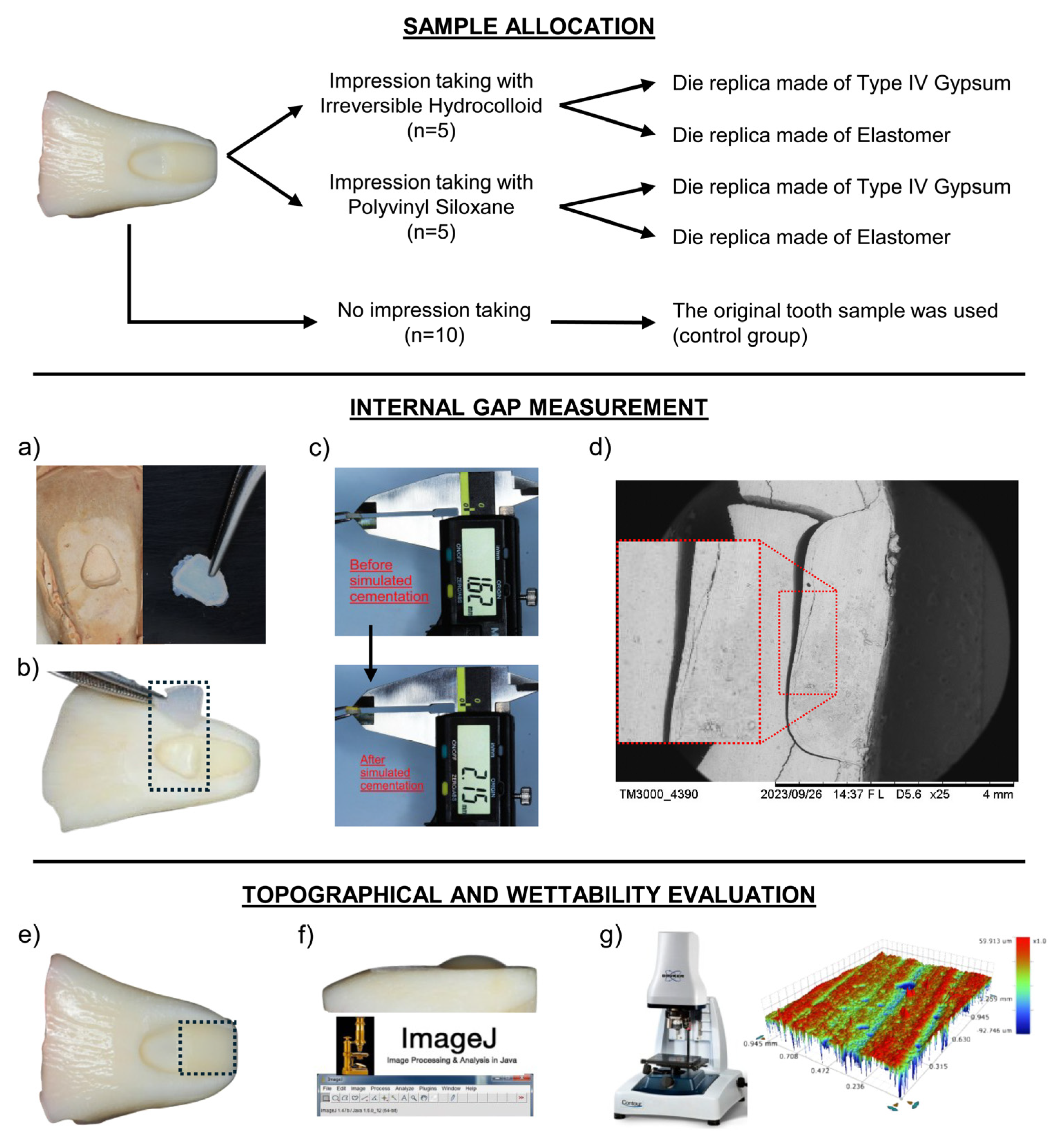
2.1. Sample Size Calculation and Study Design
2.2. Sample Preparation and Group Allocation
2.3. Fabrication of Restorations
2.4. Evaluation of the Internal Adaptation of Restorations
2.5. Scanning Electron Microscopy (SEM) Analysis
2.6. Optical Profilometry Analysis
2.7. Surface Wettability Analysis
2.8. Statistical Analysis
3. Results
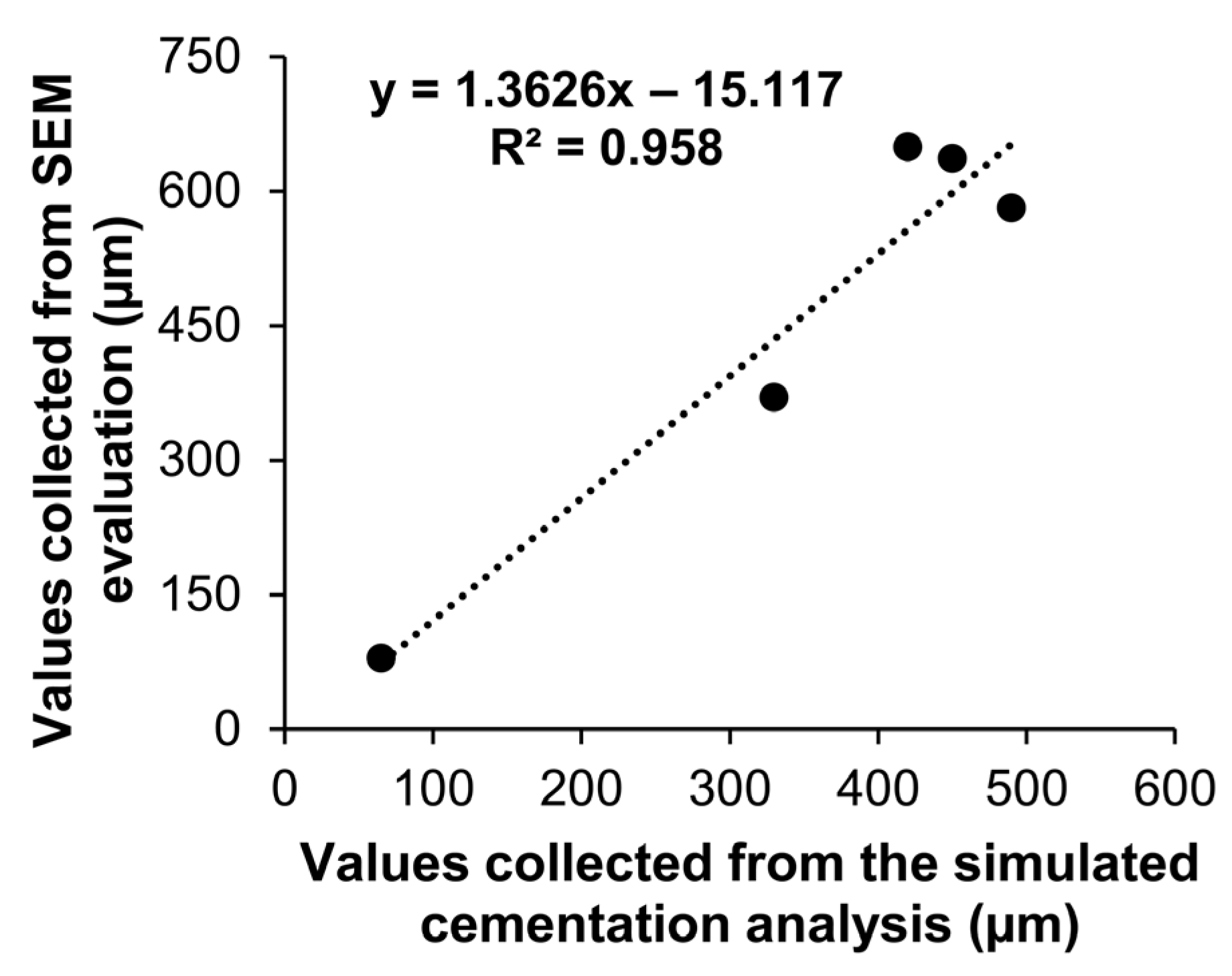
3.1. Validation of the Simulated Cementation Method with SEM
3.2. Internal Fit of Restorations
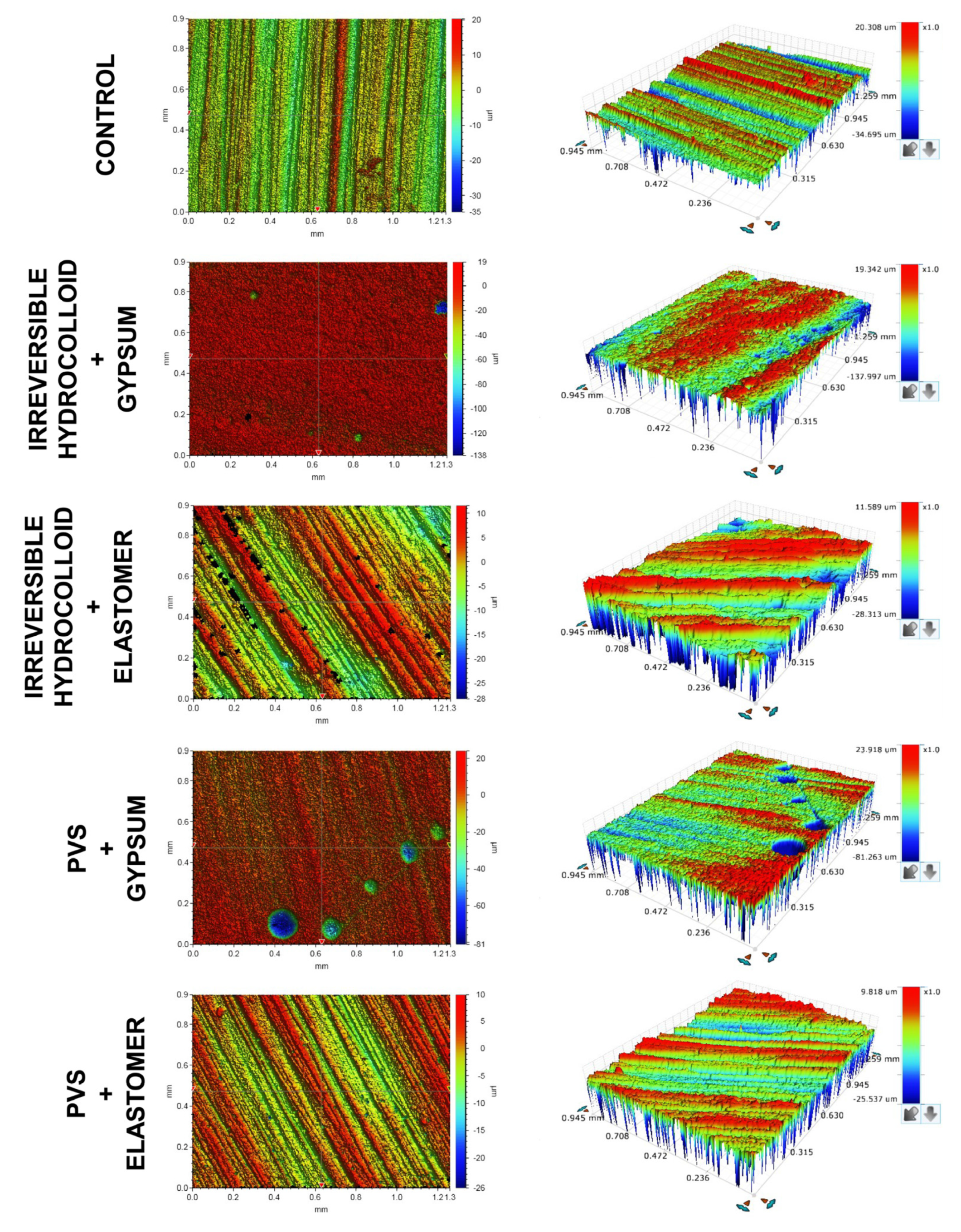
3.3. Surface Reproducibility
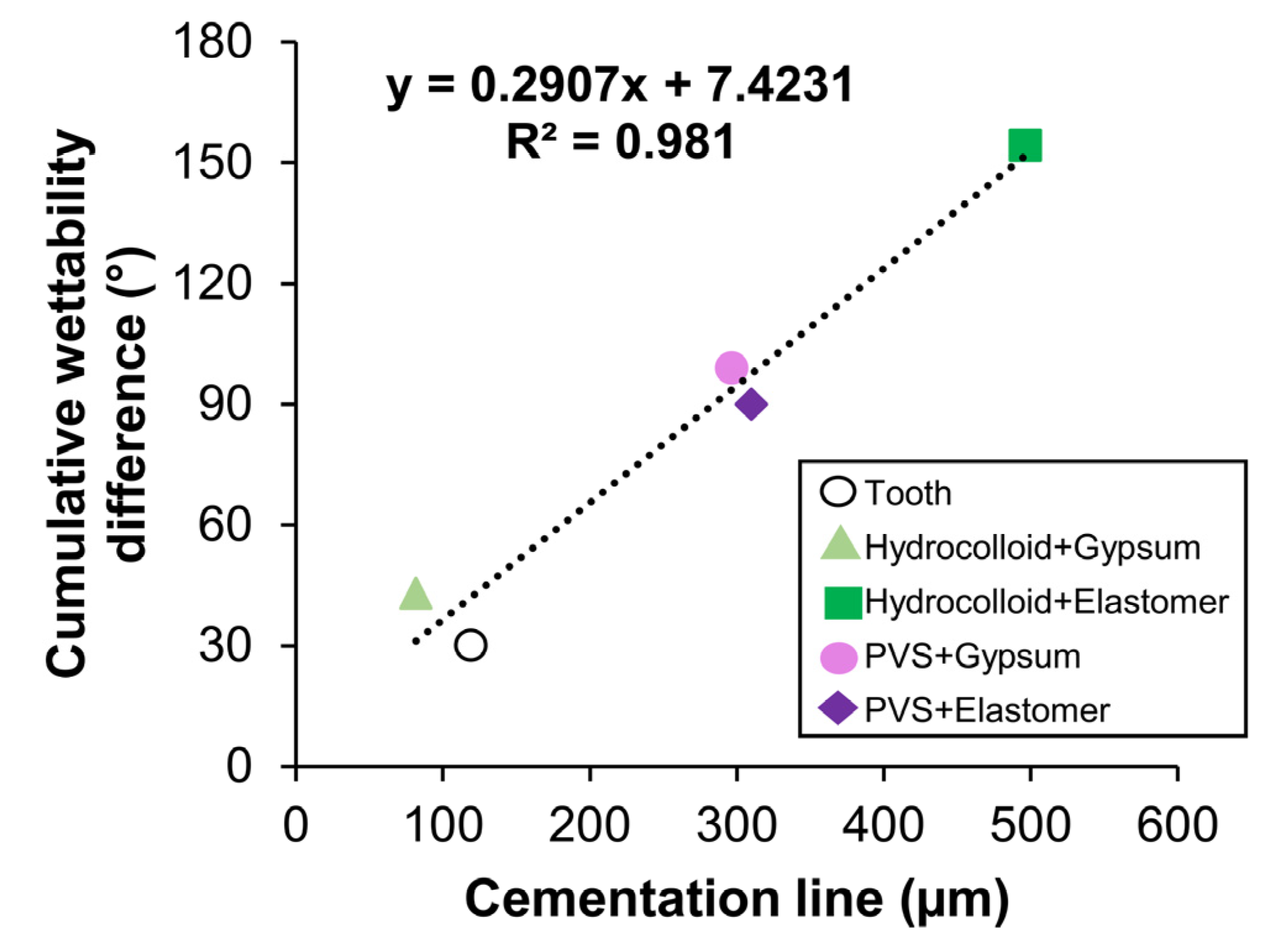
3.4. Wettability Properties
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Tribst, J.P.M.; Dos Santos, A.F.C.; da Cruz Santos, G.; da Silva Leite, L.S.; Lozada, J.C.; Silva-Concílio, L.R.; Baroudi, K.; Amaral, M. Effect of Cement Layer Thickness on the Immediate and Long-Term Bond Strength and Residual Stress between Lithium Disilicate Glass-Ceramic and Human Dentin. Materials 2021, 14, 5153. [Google Scholar] [CrossRef] [PubMed]
- Yassen, G.H.; Platt, J.A.; Hara, A.T. Bovine Teeth as Substitute for Human Teeth in Dental Research: A Review of Literature. J. Oral. Sci. 2011, 53, 273–282. [Google Scholar] [CrossRef] [PubMed]
- Hakmi, A.; Dashash, M. Direct or Indirect Composite for Restoring Permanent First Molars Affected by Molar Incisor Hypomineralisation (MIH): A Randomized Clinical Controlled Trial. BDJ Open 2023, 9, 37. [Google Scholar] [CrossRef] [PubMed]
- Kusugal, P.; Chourasiya, R.S.; Ruttonji, Z.; Astagi, P.; Nayak, A.K.; Patil, A. Surface Detail Reproduction and Dimensional Stability of Contemporary Irreversible Hydrocolloid Alternatives after Immediate and Delayed Pouring. Contemp. Clin. Dent. 2018, 9, 20–25. [Google Scholar] [CrossRef]
- Riva, Y.R.; Rahman, S.F. Dental Composite Resin: A Review. AIP Conf. Proc. 2019, 2193, 020011. [Google Scholar]
- de Almeida, C.M.; Piva, E.; Duarte, C.G.; Vieira, H.T.; Isolan, C.P.; Valente, L.L.; Münchow, E.A. Physico-Mechanical Characterization and Fracture Reliability of Dental Resin Composites for Enamel Restoration. J. Braz. Soc. Mech. Sci. Eng. 2019, 41, 398. [Google Scholar] [CrossRef]
- Josic, U.; D’Alessandro, C.; Miletic, V.; Maravic, T.; Mazzitelli, C.; Jacimovic, J.; Sorrentino, R.; Zarone, F.; Mancuso, E.; Delgado, A.H.; et al. Clinical Longevity of Direct and Indirect Posterior Resin Composite Restorations: An Updated Systematic Review and Meta-Analysis. Dent. Mater. 2023, 39, 1085–1094. [Google Scholar] [CrossRef]
- Tiron, B.; Forna, N.C.; Tărăboanță, I.; Stoleriu, S.; Topoliceanu, C.; Sălceanu, M.; Brânzan, R.; Iovan, G. The Evaluation of the Cervical Marginal Sealing of Direct vs. Indirect Composite Resin Restorations in MOD Cavities. Dent. J. 2024, 12, 92. [Google Scholar] [CrossRef]
- Fennis, W.M.; Kuijs, R.H.; Roeters, F.J.; Creugers, N.H.; Kreulen, C.M. Randomized Control Trial of Composite Cuspal Restorations: Five-Year Results. J. Dent. Res. 2014, 93, 36–41. [Google Scholar] [CrossRef]
- Pallesen, U.; Qvist, V. Composite Resin Fillings and Inlays. An 11-Year Evaluation. Clin. Oral Investig. 2003, 7, 71–79. [Google Scholar] [CrossRef]
- Angeletaki, F.; Gkogkos, A.; Papazoglou, E.; Kloukos, D. Direct versus Indirect Inlay/Onlay Composite Restorations in Posterior Teeth: A Systematic Review and Meta-Analysis. J. Dent. 2016, 53, 12–21. [Google Scholar] [CrossRef] [PubMed]
- Tian, Y.; Chen, C.; Xu, X.; Wang, J.; Hou, X.; Li, K.; Lu, X.; Shi, H.; Lee, E.-S.; Jiang, H.B. A Review of 3D Printing in Dentistry: Technologies, Affecting Factors, and Applications. Scanning 2021, 2021, 9950131. [Google Scholar] [CrossRef] [PubMed]
- Abualsaud, R.; Alalawi, H. Fit, Precision, and Trueness of 3D-Printed Zirconia Crowns Compared to Milled Counterparts. Dent. J. 2022, 10, 215. [Google Scholar] [CrossRef] [PubMed]
- Cervino, G.; Fiorillo, L.; Herford, A.S.; Laino, L.; Troiano, G.; Amoroso, G.; Crimi, S.; Matarese, M.; D’Amico, C.; Siniscalchi, E.N.; et al. Alginate Materials and Dental Impression Technique: A Current State of the Art and Application to Dental Practice. Drug Mater. 2018, 17, 18. [Google Scholar] [CrossRef]
- Schelb, E.; Mazzocco, C.V.; Jones, J.D.; Prihoda, T. Compatibility of Type IV Dental Stones with Polyvinyl Siloxane Impression Materials. J. Prosthet. Dent. 1987, 58, 19–22. [Google Scholar] [CrossRef]
- Patel, R.D.; Kattadiyil, M.T.; Goodcare, C.J.; Winer, M.S. An In Vitro Investigation into the Physical Properties of Irreversible Hydrocolloid Alternatives. J. Prosthet. Dent. 2010, 104, 325–332. [Google Scholar] [CrossRef]
- de Abreu, J.L.; Katz, S.; Sbardelotto, C.; Mijares, D.; Witek, L.; Coelho, P.G.; Hirata, R. Comparative Analysis of Elastomeric Die Materials for Semidirect Composite Restorations. Int. J. Esthet. Dent. 2020, 15, 344–354. [Google Scholar]
- Lorren, R.A.; Salter, D.J.; Fairhurst, C.W. The Contact Angles of Die Stone on Impression Materials. J. Prosthet. Dent. 1976, 36, 176–180. [Google Scholar] [CrossRef]
- Balkenhol, M.; Eichhorn, M.; Wostmann, B. Contact Angles of Contemporary Type 3 Impression Materials. Int. J. Prosthodont. 2009, 22, 396–398. [Google Scholar]
- Kugel, G.; Klettke, T.; Goldberg, J.A.; Benchimol, J.; Perry, R.D.; Sharma, S. Investigation of a New Approach to Measuring Contact Angles for Hydrophilic Impression Materials. J. Prosthodont. 2007, 16, 84–92. [Google Scholar] [CrossRef]
- Liu, X.; Cameron, A.B.; Haugli, K.H.; Mougios, A.A.; Heng, N.C.K.; Choi, J.J.E. Influence of CAD/CAM Diamond Bur Wear on the Accuracy and Surface Roughness of Dental Ceramic Restorations: A Systematic Review. J. Mech. Behav. Biomed. Mater. 2025, 161, 106813. [Google Scholar] [CrossRef]
- Lövgren, N.; Roxner, R.; Klemendz, S.; Larsson, C. Effect of Production Method on Surface Roughness, Marginal and Internal Fit, and Retention of Cobalt-Chromium Single Crowns. J. Prosthet. Dent. 2017, 118, 95–101. [Google Scholar] [CrossRef] [PubMed]
- Vohra, F.; Alsaif, R.; Khan, R.; Bukhari, I.A. Comparison of Misfit and Roughness of CAD-CAM ZrO, Selective Laser Sintered CoCr and Preformed Ti Implant Abutment Crowns. BMC Oral Health 2024, 24, 999. [Google Scholar] [CrossRef]
- Bakhsh, T.A.; Altouki, N.H.; Baeesa, L.S.; Baamer, R.A.; Alshebany, R.M.; Natto, Z.; Nasir, A.; Turkistani, A.; Hasanain, F.; Naguib, G.H. Effect of Self-Etch Adhesives on the Internal Adaptation of Composite Restoration: A CP-OCT Study. Odontology 2019, 107, 165–173. [Google Scholar] [CrossRef]
- Bilgili Can, D.; Özarslan, M. 3D-2D Microleakage Assessment of Preheated Bulk-Fill Composite Resin Applied with Different Parameters: A Micro-CT Analysis. Odontology 2023, 111, 942–952. [Google Scholar] [CrossRef]
- Sampaio, C.S.; Garcés, G.A.; Kolakarnprasert, N.; Atria, P.J.; Giannini, M.; Hirata, R. External Marginal Gap Evaluation of Different Resin-Filling Techniques for Class II Restorations-A Micro-CT and SEM Analysis. Oper. Dent. 2020, 45, E167–E175. [Google Scholar] [CrossRef]
- AlQussier, A.; Awliya, W. Effect of Erbium, Chromium-Doped: Yttrium, Scandium, Gallium and Garnet Laser Tooth Preparation on Gap Formation of Universal Adhesive Bonded to Enamel and Dentin: A Micro-CT and SEM Study. J. Lasers Med. Sci. 2022, 13, e14. [Google Scholar] [CrossRef]
- Tosco, V.; Vitiello, F.; Furlani, M.; Gatto, M.L.; Monterubbianesi, R.; Giuliani, A.; Orsini, G.; Putignano, A. Microleakage Analysis of Different Bulk-Filling Techniques for Class II Restorations: Μ-CT, SEM and EDS Evaluations. Materials 2020, 14, 31. [Google Scholar] [CrossRef]
- Donmez, M.B.; Okutan, Y. Marginal Gap and Fracture Resistance of Implant-Supported 3D-Printed Definitive Crowns: An In Vitro Study. J. Dent. 2022, 124, 104216. [Google Scholar] [CrossRef]
- Kakinuma, H.; Izumita, K.; Yoda, N.; Egusa, H.; Sasaki, K. Comparison of the Accuracy of Resin-Composite Crowns Fabricated by Three-Dimensional Printing and Milling Methods. Dent. Mater. J. 2022, 41, 808–815. [Google Scholar] [CrossRef]
- Haddadi, Y.; Ranjkesh, B.; Isidor, F.; Bahrami, G. Marginal and Internal Fit of Crowns Based on Additive or Subtractive Manufacturing. Biomater. Investig. Dent. 2021, 8, 87–91. [Google Scholar] [CrossRef] [PubMed]
- Lim, Y.A.; Kim, J.M.; Choi, Y.; Park, S. Evaluation of Fitness and Accuracy of Milled and Three-Dimensionally Printed Inlays. Eur. J. Dent. 2023, 17, 1029–1036. [Google Scholar] [CrossRef] [PubMed]
- Fahl, N., Jr. Direct-Indirect Class V Restorations: A Novel Approach for Treating Noncarious Cervical Lesions. J. Esthet. Restor. Dent. 2015, 27, 267–284. [Google Scholar] [CrossRef] [PubMed]
- Valente, L.L.; Silva, M.F.; Fonseca, A.S.; Münchow, E.A.; Isolan, C.P.; Moraes, R.R. Effect of Diamond Bur Grit Size on Composite Repair. J. Adhes. Dent. 2015, 17, 257–263. [Google Scholar] [CrossRef]
- Segerstrom, S.; Wiking-Lima de Faria, J.; Braian, M.; Ameri, A.; Ahlgren, C. A Validation Study of the Impression Replica Technique. J. Prosthodont. 2019, 28, e609–e616. [Google Scholar] [CrossRef]
- Gardner, F.M. Margins of Complete Crowns—Literature Review. J. Prosthet. Dent. 1982, 48, 396–400. [Google Scholar] [CrossRef]
- McLean, J.W.; von Fraunhofer, J.A. The Estimation of Cement Film Thickness by an in Vivo Technique. Br. Dent. J. 1971, 131, 107–111. [Google Scholar] [CrossRef]
- Vieira, T.I.; de Sousa Andrade, K.M.; Cabral, L.M.; Valença, A.M.G.; Maia, L.C.; Batista, A.U.D. Linear and Areal Surface Roughness Assessments for the Study of Tooth Wear in Human Enamel. Clin. Oral Investig. 2023, 27, 329–338. [Google Scholar] [CrossRef]
- Rodriguez, J.M.; Curtis, R.V.; Bartlett, D.W. Surface Roughness of Impression and Dental Stones Scanned by Non-Contacting Laser Profilometry. Dent. Mater. 2009, 25, 500–505. [Google Scholar] [CrossRef]
- DeLong, R.; Pintado, M.R.; Ko, C.C.; Hodges, J.S.; Douglas, W.H. Factors Influencing Optical 3D Scanning of Vinyl Polysiloxane Impression Materials. J. Prosthodont. 2001, 10, 78–85. [Google Scholar] [CrossRef]
- Mondon, M.; Ziegler, C. Changes in Water Contact Angles during the First Phase of Setting of Dental Impression Materials. Int. J. Prosthodont. 2003, 16, 49–53. [Google Scholar]
- Ding, M.; Zhao, D.; Wei, R.; Duan, Z.; Zhao, Y.; Li, Z.; Lin, T.; Li, C. Multifunctional Elastomeric Composites Based on 3D Graphene Porous Materials. Exploration 2023, 4, 20230057. [Google Scholar] [CrossRef]

| Material | Category (Application in Study) | Manufacturer | Composition | Application Technique |
|---|---|---|---|---|
| Algi-Gel Type II | Irreversible hydrocolloid (impression taking) | Maquira (Maringá, PR, Brazil) | Diatomite, potassium alginate, calcium sulfate, magnesium oxide, sodium pyrophosphate, potassium fluortitanate, polyethylene glycol, and flavoring | Vigorous spatulation of the powder-liquid ratio in rubber mixing bowl; after homogenization, the material was inserted into a tray and positioned on the tooth sample until setting as suggested by the manufacturer. |
| Scan Light | Polyvinyl siloxane (impression taking) | Yller Biomaterials (Pelotas, RS, Brazil) | Base: polyvinylsiloxane, polydimethyl-methylhydrogen siloxane, hydrocarbons, silica, and pigments Catalyst paste: vinyl polysiloxane, hydrocarbons, silica, and platinum complex | A dispensing gun was used to incorporate the material, inserting the material onto the tray with the help of a mixing tip. Working and setting times followed in accordance with the product manual. |
| Durone IV | Type IV gypsum (die fabrication) | Dentsply Sirona (São Paulo, SP, Brazil) | Calcium sulfate, alpha hemihydrate, and dye | The powder-liquid ratio was applied to a plaster vibrator (under vacuum) and applied to the mold until the entire surface was filled, obtaining a thickness similar to that of a tooth. |
| Scan Die | Polyvinyl siloxane (die fabrication) | Yller Biomaterials (Pelotas, RS, Brazil) | Base: polyvinylsiloxane, polydimethylmethylhydrogen siloxane, hydrocarbons, silica, and pigments Catalyst paste: vinyl polysiloxane, hydrocarbons, silica, and platinum complex | Applied with a dispensing gun, inserting it over the molds until the entire surface is filled, obtaining a thickness like that of tooth. When used on the polyvinyl siloxane mold, an insulator was applied, which was sprayed onto the mold and allowed to dry. |
| Opus Bulk Fill | Resin-based composite (fabrication of restorations) | FGM (Joinville, SC, Brazil) | Urethan dimethacrylic monomers, coinitiator, photoinitiator, stabilizers | One increment of up to 2 mm thick was added to the tooth samples and cavities replicated in the dies, followed by light activation for 40 s. |
| Futura AD | Polyvinyl siloxane (cement material used in the simulation technique) | DFL (Rio de Janeiro, RJ, Brazil) | Polymethyl siloxane, and sílica | A dispensing gun was used to incorporate the material and to apply it into the tooth cavity with the help of a mixing tip. The restoration was then applied to the cavity, and pressure was applied using a metallic spatula. Working and setting times followed the instructions of the manufacturer. |
| Yflow SA | Self-adhesive resin-based composite (cement material used for permanent cementation of restorations) | Yller Biomaterials (Pelotas, RS, Brazil) | Inorganic fillers, acid monomers (methacryloyloxydecyl-di-hidrogen phosphate and glycerol phosphate dimethacrylate), methacrylate monomers, pigments, initiators, and stabilizers | The material was applied into the tooth cavity using the automatic tip of the product, followed by positioning of the restoration and light activation for 40 s. |
| Parameter | Impression Material | Die Material | Control (Tooth) | |
|---|---|---|---|---|
| Gypsum | Elastomeric | |||
| Internal gap (µm) | Irreversible Hydrocolloid | 81.7 (42.5) B, b | 496.7 (23.6) A, a | 119.2 (132.9) |
| PVS | 296.7 (71.1) A, a | 310.0 (168.9) B, a | ||
| Parameter | Impression Material | Die Material | Control (Tooth) | |
|---|---|---|---|---|
| Gypsum | Elastomeric | |||
| Sa (µm) | Irreversible Hydrocolloid | 4.23 (0.73) A, a | 3.15 (0.21) A, a | 2.80 (0.73) |
| PVS | 3.67 (0.73) A, a | 2.19 (0.03) A, b | ||
| Sq (µm) | Irreversible Hydrocolloid | 8.02 (2.50) A, a | 4.40 (0.89) A, b | 3.85 (1.15) |
| PVS | 5.15 (1.46) A, a | 2.78 (0.11) A, b | ||
| Sz (µm) | Irreversible Hydrocolloid | 120.5 (34.5) A, a | 72.3 (47.9) A, a | 69.7 (16.8) |
| PVS | 75.5 (13.7) A, a | 42.1 (1.6) A, a | ||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Weissheimer, M.; Foly, J.C.S.N.; Carvalho, F.G.; Münchow, E.A. Interfacial Effects Between Dental Impression and Die Materials and Their Role in the Internal Fit of Indirect Resin-Based Composite Restorations. Dent. J. 2025, 13, 155. https://doi.org/10.3390/dj13040155
Weissheimer M, Foly JCSN, Carvalho FG, Münchow EA. Interfacial Effects Between Dental Impression and Die Materials and Their Role in the Internal Fit of Indirect Resin-Based Composite Restorations. Dentistry Journal. 2025; 13(4):155. https://doi.org/10.3390/dj13040155
Chicago/Turabian StyleWeissheimer, Murillo, João Carlos S. N. Foly, Fabíola G. Carvalho, and Eliseu A. Münchow. 2025. "Interfacial Effects Between Dental Impression and Die Materials and Their Role in the Internal Fit of Indirect Resin-Based Composite Restorations" Dentistry Journal 13, no. 4: 155. https://doi.org/10.3390/dj13040155
APA StyleWeissheimer, M., Foly, J. C. S. N., Carvalho, F. G., & Münchow, E. A. (2025). Interfacial Effects Between Dental Impression and Die Materials and Their Role in the Internal Fit of Indirect Resin-Based Composite Restorations. Dentistry Journal, 13(4), 155. https://doi.org/10.3390/dj13040155






