Abstract
Background/Objectives: Lately, there has been a greater focus on the function of the dento-mandibular apparatus, specifically on the location of the jaw and occlusion. Given the new potential insights, the current study aimed to comprehensively analyze the published literature on the use of occlusal splints and their effects on exercise performance. Methods: A search was conducted on PubMed, Scopus, and Web of Science for papers published between 2014 and 2024. Starting from the 128 identified records, 28 were finally included for review. Results: The extensive literature review revealed significant diversity in the experimental conditions, suggesting that the occlusal splints may enhance exercise performance and support dental health. Conclusions: The present study highlights the growing interest in occlusal splints research and its impact on sport and exercise science. Mouthguards or occlusal splints should continue to be worn in sports with a considerable risk of orofacial injury. Regardless of how they affect performance, mouthguards or occlusal splints are crucial for athletes in many sports to prevent oral and dental injuries.
1. Introduction
In recent years, there has been a greater focus on the function of the dento-mandibular apparatus, specifically on the location of the jaw and occlusion. In light of the new potential insights, the current study carefully examines the published literature on using occlusal splints (OSs) and how they impact exercise performance [1].
Athletes commonly use mouthguards to prevent oral and dental injuries during training and competition. These injuries are common in contact sports and non-contact activities, including workouts. Although the data are unclear, their use has been advertised to minimize concussion incidence and severity. Mouthguards absorb impact loads, reducing the force on the teeth, bones, cranium, and soft tissue. The benefits outweigh the hazards, justifying the usage of mouthguards throughout training and competition. It is widely acknowledged that protecting against orofacial injuries has numerous benefits [2].
A strong physical condition and coordination are beneficial when participating in any activity, whether sports, business, or leisure [3,4,5]. That also involves good posture. The body’s position that preserves equilibrium under static conditions, including the spatial relationships between its anatomical components, is referred to as human posture [6]. To adapt to ongoing oscillations in the upright position, posture must be continuously adjusted [7]. The central nervous system (CNS) integrates sensory inputs, like visual, vestibular, and proprioceptive signals, from various sensors to control muscle activation [7]. According to earlier research, postural control is influenced by the state of dental occlusion [8,9].
An altered dental occlusion can impact balance stability and mobility [6]. Balance stability can be assessed, among other things, by the equal percentage distribution of body weight on the right and left forefoot and rearfoot and by the movement of the center of pressure (COP) over time; here, shorter distances correspond to more minor fluctuations [10]. Other studies support that an OC influences posture, muscular strength, and performance [11].
Other authors define occlusal splints as follows. The OC is commonly used in dental practice to manage temporomandibular disorders (TMDs), bruxism, and specific occlusal issues. They help stabilize the jaw, reduce muscle strain, and prevent excessive wear on teeth by adjusting the occlusal surface. Some types, like the Michigan splint, improve muscle relaxation and mandibular posture [12].
Occlusal splints are removable dental appliances that protect the teeth by redistributing forces and can treat conditions such as jaw pain, headaches, and joint strain due to TMD or bruxism. They maintain specific mandibular positions and reduce the load on the temporomandibular joint (TMJ) through various designs, like anterior bite planes and posterior bite planes [13]. Dental medicine is crucial for athletes’ health and well-being because up to 18% of sports-related injuries happen in the maxillofacial region. It has been recommended that sports teams should consider hiring a dentist [14].
By changing the jaw relation via a custom-made splint, the effect may be twofold: an improvement in ventilation can be achieved, and the prevailing dysfunctions in the TMJ can be regulated [15,16,17]. An advantage of using an OS is that it helps alleviate muscle pain associated with TMJ disorders by promoting muscle relaxation. A disadvantage, however, is that certain types, like soft splints, can worsen bruxism in some patients due to imbalanced posterior tooth contact [18,19].
Occlusal splints, known as night guards or bite guards, are available in several types based on the design, material, and intended function. We will analyze two main types of occlusal splints in our research, and they serve distinct yet interrelated purposes. The first type is therapeutic and is used in dentistry to manage TMD, bruxism, and other occlusal issues.
The primary types include [13,20] the following:
- Stabilization Splints (Flat Plane Splints): Designed to cover the upper or lower arch, these splints evenly distribute bite forces to reduce muscle activity and protect the teeth. They are commonly used to manage TMD and bruxism.
- Anterior Bite Plane Splints: These cover only the front teeth, disengaging the back teeth to prevent clenching. Due to the possibility of posterior teeth shifting with prolonged use, they are usually advised for short-term use only.
- Repositioning Splints: These alter the jaw’s position to reduce TMJ strain and are often used to treat joint-related issues. However, they can cause permanent bite changes if used for extended periods.
- Soft and Hard Splints: Soft splints are generally more comfortable and suitable for mild bruxism, while rigid splints are more durable and adequate for severe cases. Hybrid splints, with a hard outer layer and soft inner layer, provide a balance of comfort and durability.
These types differ in material and customization options. For example, some are fabricated from acrylic or CAD/CAM technology for precise fitting [20].
The second type, commonly known as mouthguards, is designed for athletes to protect their teeth from impact-related injuries during sports. Athletic mouthguards are categorized into three types: [21,22].
- Stock Mouthguards: These are pre-shaped and available in multiple sizes, making them the most convenient and cost-effective choice. However, their generic fit often results in less comfort and reduced protection. Since they cannot be customized, wearers may need to clench their jaws to keep them securely in position.
- Boil-and-Bite Mouthguards: Made from thermoplastic materials, such as ethylene-vinyl acetate (EVA), these mouthguards soften when exposed to hot water. Once heated, the user bites into the material, shaping it to match the structure of their teeth and gums. This molding process provides a more customized fit than stock mouthguards, improving comfort and protection. However, their effectiveness relies on proper shaping during the fitting process.
- Custom-Fitted Mouthguards: These mouthguards are custom-made by dental professionals using precise impressions of the wearer’s teeth. They offer the best possible fit, comfort, and protection, but they also come at a higher cost. Due to their exceptional performance, they are especially recommended for athletes participating in high-contact sports.
While both devices serve protective functions, occlusal splints are primarily used for medical treatment, whereas mouthguards provide physical protection in high-risk activities.
Physical effort refers to the physiological and psychological energy to perform a given task, particularly in physical activities or exercises. It involves a combination of muscle contraction, cardiovascular activity, and neural coordination, requiring a measurable amount of metabolic energy [23]. Athletic performance refers to the ability of an individual to perform physical activities, particularly in sports, including strength, speed, agility, balance, and coordination. High-intensity functional training greatly impacts the development of athletes’ speed and balance [24].
Scientific research on physical effort has shown that it is closely linked to the body’s capacity to sustain and recover from activity, directly influencing performance [25]. In this context, performance is the ability to achieve a desired outcome in a physical task, often measured through speed, strength, endurance, and precision. The link between effort and performance is modulated by training intensity, individual fitness levels, and environmental factors (e.g., temperature and altitude) [26].
Understanding physical effort and performance requires an interdisciplinary approach, integrating physiology, biomechanics, psychology, nutrition, and, in this case, the dento-mandibular apparatus, to grasp how these elements combine to impact both daily activities and elite sports outcomes. The results indicated that dental occlusion differentially contributed to the dynamic stability, with an improvement when the dental occlusion was set in the correct position, disregarding the dominant and non-dominant lower limb [27]. Also, other authors agree with the fact that for both men and women, the wearing of a splint that keeps the jaw close to the centric relation improves their balance stability and increases the ROM (range of motion) of the cervical spine [1,10,28,29]. Women may have marginally different basic balance stability strategies than men regarding bipedal and unipedal standing. There were barely any differences between the two sexes in adaptation when wearing a splint. Thus, changing the jaw relation between men and women can favor and support movement potentials [10].
Sports dentistry is a developing field with an immense potential to decrease sports injuries and boost efficiency [14]. Dentists should actively assess athletes’ health status [30] because there is a correlation between the stomatognathic and musculoskeletal systems [29]. Dental health may significantly influence sports performance; thus, proper preventive measures could enable athletes to sustain their training and competition schedules without disruptions caused by dental discomforts [30]. Consequently, enhancing dental state evaluations is strongly advised in the medical monitoring of athletes [31].
Prior research indicates that the oral occlusion status affects postural control [6,25,26]. Dental occlusion and the relative position of each tooth also determine the mandible posture [27]. However, oral health is also an essential component of overall health in athletes. Poor oral health can induce systemic inflammatory responses, affect athletes’ physical fitness, and even negatively influence their athletic performance and balance [32].
Because tooth occlusion may impact muscle strength somewhere else in the body, splints have also been used for better athletic results [14,33,34]. In healthy patients, occlusal splints worn in a centric relation position have an ergogenic effect by enhancing shoulder strength and muscular activation. Splints are vital for sports where upper-body strength is essential for performance (like boxing) [14]. However, the athlete and the potential intervention to improve performance in high-level sports should always be regarded individually [35].
Dancers’ general efficiency and neuro-muscular synergy were enhanced using a customized dental apparatus for six months, during which electromyography (EMG) data and balancing tests were obtained. The orthotic could improve postural balance and classical ballet performance when applied to participants exhibiting asymmetrical muscle activation [26]. The EMG was successfully used to diagnose TMD in basketball athletes. According to the results, EMG has a high degree of discriminative power, especially regarding cases of muscular TMD. Asymmetry metrics are vital for diagnosis when paired with clinical examination, and key indicators like overall scores, such as: percent overlap coefficient between masseter muscles and anterior temporalis (POC-TA), torsional attitude of the mandibula in horizontal position (TORS), asymmetry (ASIM), and anterior temporalis activity offer insightful information. The diagnostic accuracy is improved using latent EMG variables, especially when identifying borderline cases. Furthermore, healthy athletes had more consistent and higher SCORE values, making it easier to identify using EMG [36].
The fascial system is also essential because it comprises mechanical receptors and has an autonomous contractile ability that affects the tension of the fasciae; in addition to its ability to passively distribute stress in the body muscles when mechanically triggered [29]. The posture of the body appears to be impacted by these tensions [29]. At the same time, research about the influence of occlusion splints on the rate of force development (RFD) and maximal strength tests was confirmed. Individualized splints increase performance in jumping and strength tests [37].
Research on physical performance analysis and the dento-mandibular apparatus has made significant progress, as proven by recent publications. This study aims to thoroughly assess the literature on occlusal splints and athletic performance, considering new possible insights.
2. Materials and Methods
2.1. Protocol and Registration
This systematic review was conducted according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA). The PICO question was used to determine the eligibility requirements, which addressed the following guidelines: does dental occlusion affect athletes’ performance?
P—patients—athletes;
I—dental occlusion interferes with athletes’ performance;
C—normal occlusion and dental anomalies;
O—evaluation.
The main goal was to explore how dental occlusion relates to sports performance and if splints can benefit athletes.
2.2. Search Processing
A search was conducted on PubMed, Scopus, and Web of Science for papers published between 1 January 2014 and 1 May 2024 to identify research that assesses the usage of occlusal splints in physical activity and its implications on sports performance. Boolean keywords were used in the search strategy: (“dental occlusion”) AND (“sport performance”) AND (“occlusal splints”) AND (“sports dentistry”). We chose key terms that closely coincided with our study’s purpose, which aimed to investigate the role of dental occlusion in sports performance. (Table 1).

Table 1.
Database search indicators.
2.3. Eligibility Criteria and Study Selection
The selection process consisted of two stages: evaluating the abstract, title, and the entire material. Inclusion criteria included open-access studies on dental occlusion and sports performance, reviews, English-language publications, and full-text articles. Documents that were not compatible with the required specifications were not included.
Excluded papers included research methodologies, conference presentations, in vitro or animal experiments, meta-analyses, and those lacking original data and full text. The initial search yielded relevant titles and abstracts. Complete articles from relevant research were gathered for analysis. Two reviewers (P.C. and A.M.) evaluated the retrieved studies for inclusion based on the abovementioned criteria.
2.4. Data Processing
Based on the selection criteria, two reviewers (P.C. and A.M.) separately accessed the databases to collect the studies and provide a quality grade. During the screening process, publications that did not correspond with the examined themes may have been excluded due to disagreements. After determining that the publications met the predetermined inclusion criteria, the entire text of each was read.
3. Results
3.1. Selection and Characteristics of Study
A total of 128 publications were found using the electronic database search (Web of Science = 36, PubMed = 65, and Scopus = 28)
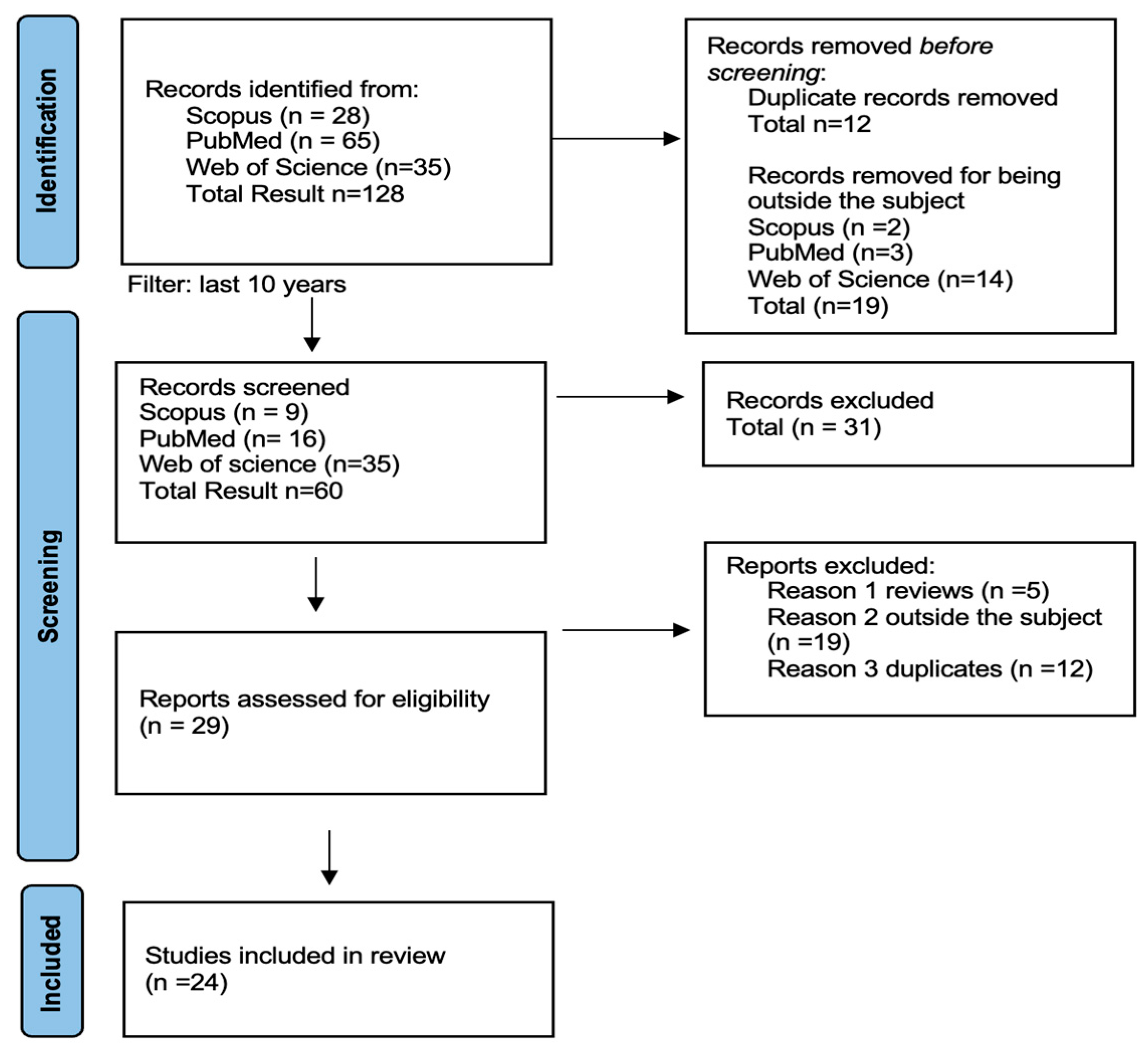
The first search yielded 128 studies. Only articles published within the last ten years were included using the inclusion and exclusion criteria. A total of 64 remained. After an additional examination, only human studies were chosen, and after removing duplicates from the tree databases, articles were manually picked, resulting in 24 papers at the end of the research (see Figure 1).

Figure 1.
Prisma flow diagram [38].
3.2. Synthesis of Results
The search results are organized in the following table (see Table 2) into parts based on the many characteristics of exercise performance examined in the included research (see Table 2).

Table 2.
Data analysis of included studies.
The included studies tested many aspects of physical performance, including aerobic and anaerobic capacity, maximum and explosive power, force, and strength, as well as evaluated other indicators, all related to occlusal splints.
4. Discussion
Dental occlusion or mouthguards are essential for athletes in numerous sports to protect against oral and dental injuries, independent of their impact on performance. Orofacial injuries occur in 39.1% of athletes who participate in contact sports, with injury types varying based on the nature of the activity, competitive level, age, group sex, and additional influencing factors [54]. For example, among professional handball players, 49% experienced head and/or facial injuries, while 22% reported dental trauma, with 76% leading to complications [55]. Another study of 169 ice hockey players in Canada found that 45.6% never wore a mouthguard, 23.1% always wore one, 14.8% occasionally wore one, and 16.5% only wore one when required. Additionally, 57.7% of players were hit by a stick, 46.2% by a puck, and 25% experienced a body check from an opponent. These findings highlight the importance of improving mouthguard designs to enhance protection, comfort, and player compliance [55]. Goud et al. advocate using occlusal splints to reduce the risk of sport-associated dental trauma [56].
Mouthguards are essential for protecting dentition and mouth face tissues, but their application has been constrained by various drawbacks and restrictions [53]. Utilizing a mouthguard to adjust jaw positioning for enhanced performance is not new. A previous study [57] showed positive effects on the isometric strength in the neck and head. Since medicine evolved, neuromuscular dentistry techniques have become more advanced. A survey of male college athletes performing sports like basketball, wrestling, mixed martial arts, and lacrosse emphasized that using a mouthguard can influence athletic performance in the peak power and consistent power output [58].
An improvement while using the occlusal splint was observed in professional basket players, mainly the force of the quadriceps muscle [59]. Using a splint to keep the mandible near the centric relation improves the balance, stability, and range of motion (ROM) in the cervical spine for both male and female participants. Women could experience slightly alternative balance firmness methods than male participants for two-legged and one-leg standing. Both sexes adjust similarly to using a brace. Altering the jaw alignment in healthy individuals may help release movement potentials, simplifying everyday activities and sports motions. Göttfert et al. [10] found in their study that for both men and women, wearing a splint that retains the mandibula, bringing the jaw closer to the centric relation, enhances balance stability and increases the cervical range of motion
Women may employ slightly varied fundamental strategies for balance and stability compared to men during bipedal and unipedal standing. However, the differences in splint adaptation between genders were minimal. Thus, modifying the jaw relationship in men and women may favor and support movement potentials. An improvement in the body posture of pilots was observed [60]. Minor adjustments in the positioning of the lower jaw can influence muscle activation, resulting in a better-balanced force production [61,62].
Prior studies [41,63,64] have proven the effect of occlusion factors on muscular chains. Improved balance, upright posture, and symmetrical walking patterns have been observed. These movements typically require minimal muscular activity. In maximal strength testing, muscles are engaged to produce maximum force and power. Minor adjustments in the positioning of the lower jaw can influence muscle activation, resulting in better-balanced force production [41,63,64]. The use of customized splints was evaluated on triathletes over four months, and enhancements in balance and biting function were found, though were not necessarily aligned with improvements in sports performance [65].
Dias et al., examining the impact of dental occlusion on shoulder strength, indicated that an OS provides a beneficial ergogenic effect on shoulder and arm strength in healthy individuals compared to a condition without a splint. These findings could have implications for sports and physical activities that require significant upper-body strength, particularly in the arms and shoulders [14]. However, Baum et al. [66] determined that the use of a dental splint does not significantly impact the rehabilitation of the glenohumeral internal rotation deficit in female volleyball players.
If an athlete has a malocclusion, they should undergo clinical and instrumental examinations to determine the benefits of using an oral splint for their discipline [67].
The most common reasons for not wearing a mouthguard are discomfort and challenges with breathing, speaking, and swallowing during physical activities [68,69]. Athletes in another study also experienced pain and problems breathing, which were caused by the continual masticatory force necessary to keep mouthguards in position due to insufficient retention [70]. In the study performed by Biagi R. et al. [71] the primary reasons for not wearing a mouthguard among athletes were lack of interest (12%) and insufficient information (9%). Additionally, 2% believed a mouthguard could not be used during ongoing orthodontic treatment, while 1% avoided it for esthetic reasons. Furthermore, 5% stated that they refrained from using a mouthguard because it negatively impacted their sports performance, and 3% reported experiencing breathing difficulties. However, in kickboxing, the use of a mouthguard is mandatory.
Vertical jump testing and the countermovement jump (VSJ and CMVJ) are commonly utilized to evaluate explosive power in the lower limbs [72]. Some studies have found enhancements in jump performance after the implementation of OSs for the VJ and CMVJ [45,70,73], while others observed improvement in lower body power for men, [74], or no significant differences [75].
Militi A et al. concluded that the application of an occlusal splint should be assessed across various sports, as athlete’s occlusion, temporomandibular joint conditions, and physical exertion levels vary [67].
Oral health plays a crucial role in physical and sports performance, and occlusal splints can enhance athletic performance. Cesanelli et al. emphasized that oral splints should be used to improve oral health in athletes and as a possible tool to enhance sports performance. They also recommend teamwork between medical staff, athletes, and coaches to establish each athlete’s peculiarities, focus on sports performance only, and consider the occlusal splints. Greater attention should be directed to athletes’ oral health to enhance their overall well-being and quality of life and potentially improve their sports performance [1].
Additionally, coaches, sports clubs, and federations need to recognize the significance of implementing oral health prevention programs for athletes [28], as well as the impact of occlusion on posture and the relationship between occlusal variations and changes in balance [28,29,30]. The mandible position influences physical performance [29], even if the OS is custom-made or commercial [1].
5. Conclusions
This study underscores the critical role of occlusal splints in maintaining and improving oral health by addressing issues such as bite misalignment, bruxism, and TMD. Occlusal splints also act as a preventive measure against dental wear and potential long-term complications. Regular dental check-ups and assessments are essential to determine the appropriateness and effectiveness of occlusal splints for individual patients, ensuring personalized treatment plans that optimize their therapeutic benefits.
In contrast, mouthguards are primarily designed to protect athletes’ teeth and oral structures from impact-related injuries. Their mandatory implementation in high-risk sports remains crucial to injury prevention strategies. While distinct in their primary function—occlusal splints focusing on therapeutic intervention and mouthguards on injury prevention—both devices contribute to overall oral stability and influence jaw positioning.
The findings from this study emphasize the need for standardized research methodologies to assess the full impact of occlusal splints on oral health, neuromuscular function, and sports performance. Future investigations should optimize design features, improve material properties, and refine clinical recommendations to enhance their effectiveness for therapeutic and protective purposes.
Author Contributions
Conceptualization, C.P. and I.R.B.; methodology, I.R.B., A.D.I. and F.I.; software, G.D. and A.M.I.; validation, C.P., G.D. and I.R.B.; formal analysis, C.P.; investigation, F.I. and G.D.; resources, A.D.I. and A.L.M.; data curation, C.P.; writing—original draft preparation, G.D.; writing—review and editing, A.M.I. and A.D.I.; visualization, I.R.B.; supervision, I.R.B. and A.L.M.; project administration, A.L.M.; funding acquisition, F.I. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Cesanelli, L.; Cesaretti, G.; Ylaitė, B.; Iovane, A.; Bianco, A.; Messina, G. Occlusal Splints and Exercise Performance: A Systematic Review of Current Evidence. Int. J. Environ. Res. Public Health 2021, 18, 10338. [Google Scholar] [CrossRef] [PubMed]
- ADA Council on Access; Prevention and Interprofessional Relations; ADA Council on Scientific Affairs. Using mouthguards to reduce the incidence and severity of sports-related oral injuries. J. Am. Dent. Assoc. 2006, 137, 1712–1720. [Google Scholar] [CrossRef] [PubMed]
- Wanke, E.M.; Schreiter, J.; Groneberg, D.A.; Weisser, B. Muscular imbalances and balance capability in dance. J. Occup. Med. Toxicol. 2018, 13, 36. [Google Scholar] [CrossRef] [PubMed]
- Wanke, E.M.; Gabrys, L.; Leslie-Spinks, J.; Ohlendorf, D.; Groneberg, D.A. Functional muscle asymmetries and laterality in Latin American formation dancers. J. Back Musculoskelet. Rehabil. 2018, 31, 931–938. [Google Scholar] [CrossRef]
- Wanke, E.M.; Mill, H.; Arendt, M.; Wanke, A.; Koch, F.; Groneberg, D.A. Occupational accidents in professional dancers with regard to different professional dance styles. Work 2014, 49, 597–606. [Google Scholar] [CrossRef] [PubMed]
- Dias, A.; Redinha, L.A.; Silva, L.M.; and Pezarat-Correia, P.C. Effects of Dental Occlusion on Body Sway, Upper Body Muscle Activity and Shooting Performance in Pistol Shooters. Appl. Bionics Biomech. 2018, 2018, 9360103. [Google Scholar] [CrossRef] [PubMed]
- Kandel, E.; Schwartz, J.; Jessell, T.; Sielgelbaum, S.; Hudspeth, A. (Eds.) Principles of Neural Science; McGraw-Hill: New York, NY, USA, 2013; pp. 943–947. [Google Scholar]
- Baldini, A.; Nota, A.; Tripodi, D.; Longoni, S.; Cozza, P. Evaluation of the correlation between dental occlusion and posture using a force platform. Clinics 2013, 68, 45–49. [Google Scholar] [CrossRef] [PubMed]
- Huggare, J.A.; Raustia, A.M.; Makofsky, H.W. Head posture and cervicovertebral and craniofacial morphology in patients with craniomandibular dysfunction. CRANIO® 1992, 10, 173–179. [Google Scholar] [CrossRef]
- Göttfert, F.; Herzog, J.; Maurer-Grubinger, C.; Oremek, G.; Holzgreve, F.; Groneberg, D.A.; Ohlendorf, D. Balance Stability and Cervical Spine Range of Motion While Wearing a Custom-Made Mandibular Splint with Special Consideration of the Sex. Appl. Sci. 2022, 12, 11856. [Google Scholar] [CrossRef]
- Moon, H.J.; Lee, Y.K. The relationship between dental occlusion/-temporomandibular joint status and general body health: Part 1. Dental occlusion and TMJ status exert an influence on general body health. J. Altern. Complement. Med. 2011, 17, 995–1000. [Google Scholar] [CrossRef]
- Kui, A.; Pop, S.; Buduru, S.; Neguciociu, M. The use of Occlusal Splints in Temporomandibular disorders—An overview. Acta Stomatol. Marisiensis J. 2020, 3, 3–8. [Google Scholar] [CrossRef]
- Alqutaibi, A.Y.; Aboalrejal, A.N. Types of Occlusal Splint in Management of Temporomandibular Disorders (TMD). J. Arthritis 2015, 4, 176. [Google Scholar] [CrossRef]
- Dias, A.; Redinha, L.; Vaz, J.R.; Cordeiro, N.; Silva, L.; Pezarat–Correia, P. Effects of occlusal splints on shoulder strength and activation. Ann. Med. 2019, 51, 15–21. [Google Scholar] [CrossRef] [PubMed]
- Leroux, E.; Leroux, S.; Maton, F.; Ravalec, X.; Sorel, O. Influence of dental occlusion on the athletic performance of young elite rowers: A pilot study. Clinics 2018, 73, 453. [Google Scholar] [CrossRef]
- Grosdent, S.; O’Thanh, R.; Domken, O.; Lamy, M.; Croisier, J.L. Dental Occlusion Influences Knee Muscular Performances in Asymptomatic Females. J. Strength Cond. Res. 2014, 28, 492–498. [Google Scholar] [CrossRef]
- Garner, D.P.; Lamira, J. Respiratory outcomes with the use of a lower custom fit genioglossal-effecting oral appliance. Clin. Exp. Dent. Res. 2019, 6, 100–106. [Google Scholar] [CrossRef] [PubMed]
- Grondin, F.; Hall, T.; Ella, B.; Laurentoye, M.; Ella, B. Upper cervical range of motion is impaired in patients with temporomandibular disorders. Cranio 2014, 33, 91–99. [Google Scholar] [CrossRef] [PubMed]
- Subachanya, R.; Saravana, P.G.L. Oclussal splints therapy in TMD pain management: A review. J. Glob. Oral Health 2022, 5, 102–106. [Google Scholar] [CrossRef]
- Ainoosah, S.; Farghal, A.E.; Alzemei, M.S.; Saini, R.S.; Gurumurthy, V.; Quadri, S.A.; Okshah, A.; Mosaddad, S.A.; Heboyan, A. Comparative analysis of different types of occlusal splints for the management of sleep bruxism: A systematic review. BMC Oral Health 2024, 24, 29. [Google Scholar] [CrossRef]
- Sakshi, N.; Sneha, S.M.; Abhilasha, B. Comparing Boil and Bite with Customized Mouthguard Based on Subjective Experience of Boxers—A Pilot Study. Int. J. Health Sci. Res. 2021, 11, 358–366. [Google Scholar] [CrossRef]
- Patrick, D.G.; Van Noort, R.; Found, M.S. Scale of protection and the various types of sports mouthguard. Br. J. Sports Med. 2005, 39, 278–281. [Google Scholar] [CrossRef] [PubMed]
- Borg, G.A. Psychophysical bases of perceived exertion. Med. Sci. Sports Exerc. 1982, 14, 377–381. [Google Scholar] [CrossRef] [PubMed]
- Wang, X.; Soh, K.G.; Samsudin, S.; Deng, N.; Liu, X.; Zhao, Y.; Akbar, S. Effects of high-intensity functional training on physical fitness and sport-specific performance among the athletes: A systematic review with meta-analysis. PLoS ONE 2023, 18, e0295531. [Google Scholar] [CrossRef]
- Wilmore, J.H.; Costill, D.L. Physiology of Sport and Exercise, 3rd ed.; Human Kinetics: New York, NY, USA, 2004; pp. 78–80. [Google Scholar]
- Noakes, T.D. Lore of Running, 4th ed.; Human Kinetics: Cape Town, South Africa, 2001; pp. 23–26. [Google Scholar]
- Julià-Sánchez, S.; Álvarez-Herms, J.; Cirer-Sastre, R.; Corbi, F.; Burtscher, M. The Influence of Dental Occlusion on Dynamic Balance and Muscular Tone. Front. Physiol. 2020, 10, 1626. [Google Scholar] [CrossRef] [PubMed]
- Didier, H.; Assandri, F.; Gaffuri, F.; Cavagnetto, D.; Abate, A.; Villanova, M.; Maiorana, C. The Role of Dental Occlusion and Neuromuscular Behavior in Professional Ballet Dancers’ Performance: A Pilot Study. Healthcare 2021, 9, 251. [Google Scholar] [CrossRef]
- Patti, A.; Bianco, A.; Messina, G.; Bellafiore, M.; Battaglia, G.; Iovane, A.; Traina, M.; Palma, A. The influence of the stomatognathic system on explosive strength: A pilot study. J. Phys. Ther. Sci. 2016, 28, 72–75. [Google Scholar] [CrossRef]
- de la Parte, A.; Monticelli, F.; Toro-Román, V.; Pradas, F. Differences in Oral Health Status in Elite Athletes According to Sport Modalities. Sustainability 2021, 13, 7282. [Google Scholar] [CrossRef]
- Minty, M.; Canceill, T.; Lê, S.; Dubois, P.; Amestoy, O.; Loubieres, P.; Christensen, J.E.; Champion, C.; Azalbert, V.; Grasset, E.; et al. Oral health and microbiota status in professional rugby players: A case-control study. J. Dent. 2018, 79, 53–60. [Google Scholar] [CrossRef]
- Ayadi, H.; Ben Saad, H.; Talbi, M.; Boughzela, A.; Moalla, W.; Granacher, U.; Chaouachi, A. Effects of wearing fixed orthodontic appliance on dynamic balance, reaction time, and pain perception in adolescents and young adult elite athletes. Somatosens. Mot. Res. 2023, 41, 230–237. [Google Scholar] [CrossRef]
- Klineberg, I.; Jagger, R.G. Occlusion and Clinical Practice: An Evidence-Based Approach. Br. Dent. J. 2004, 197, 106–107. [Google Scholar]
- Verban, E.M.; Groppel, J.L.; Pfautsch, E.W.; Ramseyer, G.C. The Effects of a Mandibular Orthopedic Repositioning Appliance on Shoulder Strength. J. Craniomandib. Pract. 1984, 2, 232–237. [Google Scholar] [CrossRef] [PubMed]
- Ringhof, S.; Hellmann, D.; Meier, F.; Etz, E.; Schindler, H.J.; Stein, T. The effect of oral motor activity on the athletic performance of professional golfers. Front. Psychol. 2015, 6, 750. [Google Scholar] [CrossRef]
- Valenti, C.; Di Pasquale, F.; Pancrazi, G.P.; Falocci, N.; Nanussi, A.; Biscarini, A.; Pagano, S. Evaluation of different electromyographic parameters of temporomandibular dysfunction in athletes. J. Bodyw. Mov. Ther. 2024, 42, 56–63. [Google Scholar] [CrossRef]
- Maurer, C.; Heller, S.; Sure, J.-J.; Fuchs, D.; Mickel, C.; Wanke, E.M.; Groneberg, D.A.; Ohlendorf, D. Strength improvements through occlusal splints? The effects of different lower jaw positions on maximal isometric force production and performance in different jumping types. PLoS ONE 2018, 13, e0193540. [Google Scholar] [CrossRef] [PubMed]
- Hutton, B.; Salanti, G.; Caldwell, D.M.; Chaimani, A.; Schmid, C.H.; Cameron, C.; Ioannidis, J.P.A.; Straus, S.; Thorlund, K.; Jansen, J.P.; et al. The PRISMA Extension Statement for Reporting of Systematic Reviews Incorporating Network Meta-analyses of Health Care Interventions: Checklist and Explanations. Ann. Intern. Med. 2015, 162, 777–784. [Google Scholar] [CrossRef]
- Allen, C.R.; Dabbs, N.C.; Zachary, C.S.; Garner, J.C. The Acute Effect of a Commercial Bite-Aligning Mouthpiece on Strength and Power in Recreationally Trained Men. J. Strength Cond. Res. 2014, 28, 499–503. [Google Scholar] [CrossRef] [PubMed]
- Golem, D.L.; Arent, S.M. Effects of Over-the-Counter Jaw-Repositioning Mouth Guards on Dynamic Balance, Flexibility, Agility, Strength, and Power in College-Aged Male Athletes. J. Strength Cond. Res. 2015, 29, 500–512. [Google Scholar] [CrossRef] [PubMed]
- Maurer, C.; Stief, F.; Jonas, A.; Kovac, A.; Groneberg, D.A.; Meurer, A.; Ohlendorf, D. Influence of the Lower Jaw Position on the Running Pattern. PLoS ONE 2015, 10, e0135712. [Google Scholar] [CrossRef]
- Battaglia, G.; Giustino, V.; Iovane, A.; Bellafiore, M.; Martines, F.; Patti, A.; Traina, M.; Messina, G.; Palma, A. Influence of occlusal vertical dimension on cervical spine mobility in sports subjects. Acta Medica Mediterr. 2016, 32, 1589–1595. [Google Scholar] [CrossRef]
- Buscà, B.; Morales, J.; Solana-Tramunt, M.; Miró, A.; García, M. Effects of Jaw Clenching While Wearing a Customized Bite-Aligning Mouthpiece on Strength in Healthy Young Men. J. Strength Cond. Res. 2016, 30, 1102–1110. [Google Scholar] [CrossRef]
- Ringhof, S.; Stein, T.; Hellmann, D.; Schindler, H.J.; Potthast, W. Effect of Jaw Clenching on Balance Recovery: Dynamic Stability and Lower Extremity Joint Kinematics after Forward Loss of Balance. Front. Psychol. 2016, 7, 291. [Google Scholar] [CrossRef] [PubMed]
- Fischer, H.; Weber, D.; Beneke, R. No Improvement in Sprint Performance With a Neuromuscular Fitted Dental Splint. Int. J. Sports Physiol. Perform. 2017, 12, 414–417. [Google Scholar] [CrossRef]
- Golem, D.L.; Davitt, P.M.; Arent, S.M. The effects of over-the-counter jaw-repositioning mouthguards on aerobic performance. J. Sports Med. Phys. Fit. 2017, 57, 865–871. [Google Scholar] [CrossRef]
- Kinjo, R.; Wada, T.; Churei, H.; Ohmi, T.; Hayashi, K.; Yagishita, K.; Uo, M.; Ueno, T. Development of a Wearable Mouth Guard Device for Monitoring Teeth Clenching during Exercise. Sensors 2021, 21, 1503. [Google Scholar] [CrossRef]
- Carbonari, B.; Balducci, F.; Cesaretti, G.; Cesanelli, L.; Botticelli, D.; Messina, G. Performance, balance and posture variations with Occlusal Splint and Taopatch® devices: A retrospettive cross-over study. J. Sports Med. Phys. Fit. 2021, 61, 317–323. [Google Scholar] [CrossRef] [PubMed]
- Cardoso, F.; Monteiro, A.S.; Vilas-Boas, J.P.; Pinho, J.C.; Pyne, D.B.; Fernandes, R.J. Effects of Wearing a 50% Lower Jaw Advancement Splint on Biophysical and Perceptual Responses at Low to Severe Running Intensities. Life 2022, 12, 253. [Google Scholar] [CrossRef] [PubMed]
- Inchingolo, A.D.; Pezzolla, C.; Patano, A.; Ceci, S.; Ciocia, A.M.; Marinelli, G.; Malcangi, G.; Montenegro, V.; Cardarelli, F.; Piras, F.; et al. Experimental Analysis of the Use of Cranial Electromyography in Athletes and Clinical Implications. Int. J. Environ. Res. Public Health 2022, 19, 7975. [Google Scholar] [CrossRef] [PubMed]
- Parrini, S.; Rossini, G.; Nebiolo, B.; Airale, M.; Franceschi, A.; Cugliari, G.; Deregibus, A.; Castroflorio, T. Variations in athletic performance with occlusal splint in track and field athletes: A randomized clinical trial. J. Sports Med. Phys. Fit. 2022, 62, 375–381. [Google Scholar] [CrossRef] [PubMed]
- Dias, A.; Redinha, L.; Tavares, F.; Silva, L.; Malaquias, F.; Pezarat-Correia, P. The effect of a controlled mandible position mouthguard on upper body strength and power in trained rugby athletes—A randomized within subject study. Injury 2021, 53, 457–462. [Google Scholar] [CrossRef]
- Kalman, L.; Piva, A.M.d.O.D.; de Queiroz, T.S.; Tribst, J.P.M. Biomechanical Behavior Evaluation of a Novel Hybrid Occlusal Splint-Mouthguard for Contact Sports: 3D-FEA. Dent. J. 2021, 10, 3. [Google Scholar] [CrossRef] [PubMed]
- Sanchez-Avila, M.B.; Gutmann, J.L.; Navas-Barrantes, E.; Leal-Fernandez, M.C.; Mejia-Morales, S. Management of external replacement root resorption in a tooth with a history of avulsion. Endod. Pract. Today 2020, 14, 145–150. [Google Scholar]
- Sarao, S.K.; Rattai, J.; Levin, L. Dental Trauma Among Hockey Players: Preventive Measures, Compliance and Injury Types. J. Can. Dent. Assoc. 2021, 87, l8. [Google Scholar]
- Gould, T.E.; Piland, S.G.; Caswell, S.V.; Ranalli, D.; Mills, S.; Ferrara, M.S.; Courson, R. National Athletic Trainers’ Association Position Statement: Preventing and Managing Sport-Related Dental and Oral Injuries. J. Athl. Train. 2016, 51, 821–839. [Google Scholar] [CrossRef]
- Gelb, H.; Mehta, N.R.; Forgione, A.G. The Relationship Between Jaw Posture and Muscular Strength in Sports Dentistry: A Reappraisal. Cranio® 1996, 14, 320–325. [Google Scholar] [CrossRef] [PubMed]
- Arent, S.M.; McKenna, J.; Golem, D.L. Effects of a neuromuscular dentistry-designed mouthguard on muscular endurance and anaerobic power. Comp. Exerc. Physiol. 2010, 7, 73–79. [Google Scholar] [CrossRef]
- Baldini, A.; Beraldi, A.; Nota, A.; Danelon, F.; Ballanti, F.; Longoni, S. Gnathological postural treatment in a professional basketball player: A case report and an overview of the role of dental occlusion on performance. Ann. Stomatol. 2012, 3, 51–58. [Google Scholar]
- Baldini, A.; Nota, A.; Cravino, G.; Cioffi, C.; Rinaldi, A.; Cozza, P. Influence of Vision and Dental Occlusion on Body Posture in Pilots. Aviat. Space Environ. Med. 2013, 84, 823–827. [Google Scholar] [CrossRef]
- Bracco, P.; Deregibus, A.; Piscetta, R. Effects of different jaw relations on postural stability in human subjects. Neurosci. Lett. 2004, 356, 228–230. [Google Scholar] [CrossRef] [PubMed]
- Hellmann, D.; Giannakopoulos, N.N.; Blaser, R.; Eberhard, L.; Schindler, H.J. The effect of various jaw motor tasks on body sway. J. Oral Rehabil. 2011, 38, 729–736. [Google Scholar] [CrossRef]
- D’Ermes, V.; Basile, M.; Rampello, A.; Di Paolo, C. Influence of occlusal splint on competitive athletes performances. Ann. Di Stomatol. 2012, 3, 113–118. [Google Scholar]
- Ebben, W.P.; Flanagan, E.P.; Jensen, R.L. Jaw Clenching Results in Concurrent Activation Potentiation During the Countermovement Jump. J. Strength Cond. Res. 2008, 22, 1850–1854. [Google Scholar] [CrossRef] [PubMed]
- D’attilio, M.; Bondi, D.; Castellani, M.; Verratti, V.; Pietrangelo, T. Sports performance adaptations through occlusal splint: Case reports of triathlon athletes. Cranio® 2021, 41, 556–564. [Google Scholar] [CrossRef] [PubMed]
- Baum, S.; van Kampen, H.; Ballenberger, N.; von Piekartz, H. Einfluss dentaler Okklusionsveränderungen auf die Rehabilitation eines glenohumeralen Innenrotationsdefizits (GIRD) bei Profivolleyballern. Sportverletz. Sportschaden 2019, 33, 160–171. [Google Scholar] [CrossRef]
- Militi, A.; Cicciù, M.; Sambataro, S.; Bocchieri, S.; Cervino, G.; De Stefano, R.; Fiorillo, L. Dental occlusion and sport performance. Minerva Dent. Oral Sci. 2020, 69, 112–118. [Google Scholar] [CrossRef]
- Ono, Y.; Tanaka, Y.; Sako, K.; Tanaka, M.; Fujimoto, J. Association between Sports-Related Concussion and Mouthguard Use among College Sports Players: A Case-Control Study Based on Propensity Score Matching. Int. J. Environ. Res. Public Health 2020, 17, 4493. [Google Scholar] [CrossRef]
- Paterson, N.T.; Gorham, D.A.; Matela, R.; Moffatt, J.E.; Greasley, A. A finite element study of the mechanics of sports mouthguards. Sports Eng. 2004, 7, 182–195. [Google Scholar]
- Mojarad, F.; Farhadian, M.; Torkaman, S. The Prevalence of Sports-related Dental Injuries and the Rate of Awareness of Mouthguard Use among Child Athletes. J. Pediatr. Res. 2020, 7, 358–364. [Google Scholar] [CrossRef]
- Biagi, R.; Mirelli, C.; Ventimiglia, R.; Ceraulo, S. Traumatic Dental Injuries: Prevalence, First Aid, and Mouthguard Use in a Sample of Italian Kickboxing Athletes. Dent. J. 2024, 12, 310. [Google Scholar] [CrossRef] [PubMed]
- Mackala, K.; Stodółka, J.; Siemienski, A.; Ćoh, M. Biomechanical Analysis of Squat Jump and Countermovement Jump From Varying Starting Positions. J. Strength Cond. Res. 2013, 27, 2650–2661. [Google Scholar] [CrossRef] [PubMed]
- Haughey, J.P.; Fine, P. Effects of the lower jaw position on athletic performance of elite athletes. BMJ Open Sport Exerc. Med. 2020, 6, e000886. [Google Scholar] [CrossRef] [PubMed]
- Schulze, A.; Kwast, S.; Busse, M. Influence of Mouthguards on Physiological Responses in Rugby. Sports Med. Int. Open 2019, 3, 25–31. [Google Scholar] [CrossRef] [PubMed]
- Dunn-Lewis, C.; Luk, H.-Y.; Comstock, B.A.; Szivak, T.K.; Hooper, D.R.; Kupchak, B.R.; Watts, A.M.; Putney, B.J.; Hydren, J.R.; Volek, J.S.; et al. The Effects of a Customized Over-the-Counter Mouth Guard on Neuromuscular Force and Power Production in Trained Men and Women. J. Strength Cond. Res. 2012, 26, 1085–1093. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).