Pit and Fissure Sealants—A Comprehensive Review
Abstract
:1. Caries Developments in Recent Decades
2. Caries Prophylaxis
3. Materials for Sealing Pits and Fissures
4. Sealing of Non-Cavitated Lesions
5. Follow-Up Treatment
6. Conclusions
Author Contributions
Conflicts of Interest
References
- Rugg-Gunn, A. Dental caries: Strategies to control this preventable disease. Acta Med. Acad. 2013, 42, 117–130. [Google Scholar] [CrossRef] [PubMed]
- Petersen, P.E. The world oral health report 2003: Continuous improvement of oral health in the 21st century—The approach of the who global oral health programme. Community Dent. Oral Epidemiol. 2003, 31, 3–23. [Google Scholar] [CrossRef] [PubMed]
- Petersen, P.E. World health organization global policy for improvement of oral health—World health assembly 2007. Int. Dent. J. 2008, 58, 115–121. [Google Scholar] [CrossRef] [PubMed]
- Petersen, P.E. Sociobehavioural risk factors in dental caries—International perspectives. Community Dent. Oral Epidemiol. 2005, 33, 274–279. [Google Scholar] [CrossRef] [PubMed]
- Bagramian, R.A.; Garcia-Godoy, F.; Volpe, A.R. The global increase in dental caries. A pending public health crisis. Am. J. Dent. 2009, 22, 3–8. [Google Scholar] [PubMed]
- Dye, B.A.; Tan, S.; Smith, V.; Lewis, B.G.; Barker, L.K.; Thornton-Evans, G.; Eke, P.I.; Beltran-Aguilar, E.D.; Horowitz, A.M.; Li, C.H. Trends in oral health status: United States, 1988–1994 and 1999–2004. Vital Health Stat. 11 2007, 248, 1–92. [Google Scholar]
- Haugejorden, O.; Magne Birkeland, J. Ecological time-trend analysis of caries experience at 12 years of age and caries incidence from age 12 to 18 years: Norway 1985–2004. Acta Odontol. Scand. 2006, 64, 368–375. [Google Scholar] [CrossRef] [PubMed]
- Carvalho, J.C. Caries process on occlusal surfaces: Evolving evidence and understanding. Caries Res. 2014, 48, 339–346. [Google Scholar] [CrossRef] [PubMed]
- Brown, L.J.; Kaste, L.M.; Selwitz, R.H.; Furman, L.J. Dental caries and sealant usage in U.S. Children, 1988–1991: Selected findings from the third national health and nutrition examination survey. J. Am. Dent. Assoc. 1996, 127, 335–343. [Google Scholar] [CrossRef] [PubMed]
- Feigal, R.J.; Donly, K.J. The use of pit and fissure sealants. Pediatr. Dent. 2006, 28, 143–150. [Google Scholar] [PubMed]
- Kotsanos, N.; Darling, A.I. Influence of posteruptive age of enamel on its susceptibility to artificial caries. Caries Res. 1991, 25, 241–250. [Google Scholar] [CrossRef] [PubMed]
- Schulte, A.; Gente, M.; Pieper, K. Posteruptive changes of electrical resistance values in fissure enamel of premolars. Caries Res. 1999, 33, 242–247. [Google Scholar] [CrossRef] [PubMed]
- Kataoka, S.; Sakuma, S.; Wang, J.; Yoshihara, A.; Miyazaki, H. Changes in electrical resistance of sound fissure enamel in first molars for 66 months from eruption. Caries Res. 2007, 41, 161–164. [Google Scholar] [CrossRef] [PubMed]
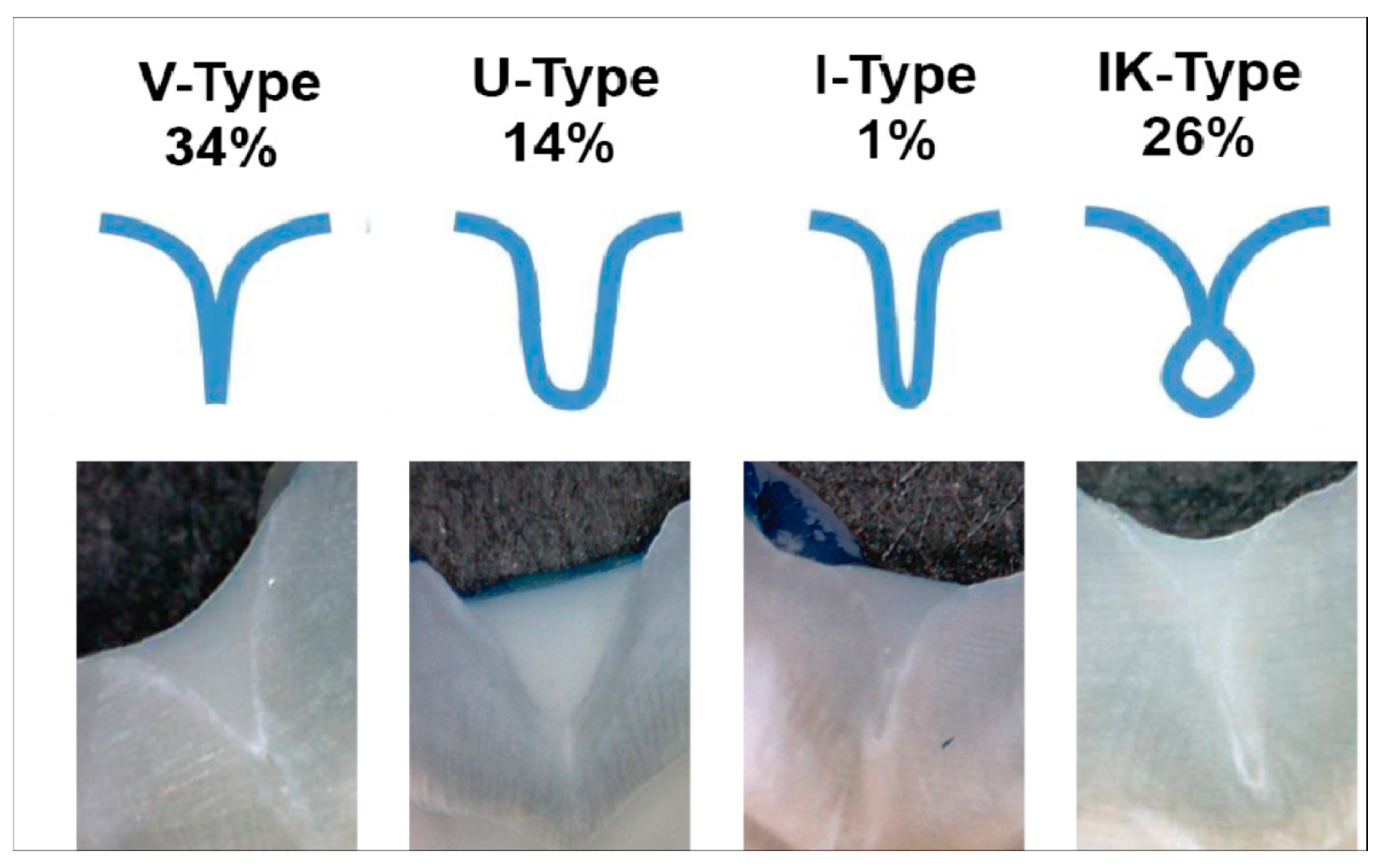
- Muller-Bolla, M.; Courson, F.; Droz, D.; Lupi-Pegurier, L.; Velly, A.M. Definition of at-risk occlusal surfaces of permanent molars—A descriptive study. J. Clin. Pediatr. Dent. 2009, 34, 35–42. [Google Scholar] [CrossRef] [PubMed]
- Yu, F.; Yu, H.; Lin, P.; Dong, Y.; Zhang, L.; Sun, X.; Liu, Z.; Guo, H.; Huang, L.; Chen, J. Effect of an antibacterial monomer on the antibacterial activity of a pit-and-fissure sealant. PLoS ONE 2016, 11, e0162281. [Google Scholar] [CrossRef] [PubMed]
- Ahovuo-Saloranta, A.; Forss, H.; Hiiri, A.; Nordblad, A.; Makela, M. Pit and fissure sealants versus fluoride varnishes for preventing dental decay in the permanent teeth of children and adolescents. Cochrane Database Syst. Rev. 2016. [Google Scholar] [CrossRef] [PubMed]
- Carvalho, J.C.; Dige, I.; Machiulskiene, V.; Qvist, V.; Bakhshandeh, A.; Fatturi-Parolo, C.; Maltz, M. Occlusal caries: Biological approach for its diagnosis and management. Caries Res. 2016, 50, 527–542. [Google Scholar] [CrossRef] [PubMed]
- Marthaler, T.M. Changes in dental caries 1953–2003. Caries Res. 2004, 38, 173–181. [Google Scholar] [CrossRef] [PubMed]
- Petersson, G.H.; Bratthall, D. The caries decline: A review of reviews. Eur. J. Oral Sci. 1996, 104, 436–443. [Google Scholar] [CrossRef] [PubMed]
- Ahovuo-Saloranta, A.; Forss, H.; Walsh, T.; Hiiri, A.; Nordblad, A.; Makela, M.; Worthington, H.V. Sealants for preventing dental decay in the permanent teeth. Cochrane Database Syst. Rev. 2013. [Google Scholar] [CrossRef] [Green Version]
- Ripa, L.W. Sealants revisted: An update of the effectiveness of pit-and-fissure sealants. Caries Res. 1993, 27, 77–82. [Google Scholar] [CrossRef] [PubMed]
- Wright, J.T.; Tampi, M.P.; Graham, L.; Estrich, C.; Crall, J.J.; Fontana, M.; Gillette, E.J.; Novy, B.B.; Dhar, V.; Donly, K.; et al. Sealants for preventing and arresting pit-and-fissure occlusal caries in primary and permanent molars: A systematic review of randomized controlled trials-a report of the American dental association and the American academy of pediatric dentistry. J. Am. Dent. Assoc. 2016, 147, 631–645.e18. [Google Scholar] [CrossRef] [PubMed]
- Shellis, R.P.; Duckworth, R.M. Studies on the cariostatic mechanisms of fluoride. Int. Dent. J. 1994, 44, 263–273. [Google Scholar] [PubMed]
- Ten Cate, J.M. Review on fluoride, with special emphasis on calcium fluoride mechanisms in caries prevention. Eur. J. Oral Sci. 1997, 105, 461–465. [Google Scholar] [CrossRef] [PubMed]
- Raadal, M.; Laegreid, O.; Laegreid, K.V.; Hveem, H.; Korsgaard, E.K.; Wangen, K. Fissure sealing of permanent first molars in children receiving a high standard of prophylactic care. Community Dent. Oral Epidemiol. 1984, 12, 65–68. [Google Scholar] [CrossRef] [PubMed]
- Liu, B.Y.; Lo, E.C.; Chu, C.H.; Lin, H.C. Randomized trial on fluorides and sealants for fissure caries prevention. J. Dent. Res. 2012, 91, 753–758. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bravo, M.; Montero, J.; Bravo, J.J.; Baca, P.; Llodra, J.C. Sealant and fluoride varnish in caries: A randomized trial. J. Dent. Res. 2005, 84, 1138–1143. [Google Scholar] [CrossRef] [PubMed]
- Llodra, J.C.; Bravo, M.; Delgado-Rodriguez, M.; Baca, P.; Galvez, R. Factors influencing the effectiveness of sealants—A meta-analysis. Community Dent. Oral Epidemiol. 1993, 21, 261–268. [Google Scholar] [CrossRef] [PubMed]
- Mejare, I.; Lingstrom, P.; Petersson, L.G.; Holm, A.K.; Twetman, S.; Kallestal, C.; Nordenram, G.; Lagerlof, F.; Soder, B.; Norlund, A.; et al. Caries-preventive effect of fissure sealants: A systematic review. Acta Odontol. Scand. 2003, 61, 321–330. [Google Scholar] [CrossRef] [PubMed]
- Lalloo, R.; Turton, M.S. Fissure sealants on permanent first molars—Consequences of a one-year delay. Community Dent. Health 2008, 25, 191–192. [Google Scholar] [PubMed]
- Brown, L.J.; Wall, T.P.; Lazar, V. Trends in untreated caries in permanent teeth of children 6 to 18 years old. J. Am. Dent. Assoc. 1999, 130, 1637–1644. [Google Scholar] [CrossRef] [PubMed]
- Brown, L.J.; Wall, T.P.; Lazar, V. Trends in total caries experience: Permanent and primary teeth. J. Am. Dent. Assoc. 2000, 131, 223–231. [Google Scholar] [CrossRef] [PubMed]
- Brown, L.J.; Wall, T.P.; Lazar, V. Trends in untreated caries in primary teeth of children 2 to 10 years old. J. Am. Dent. Assoc. 2000, 131, 93–100. [Google Scholar] [CrossRef] [PubMed]
- Kaste, L.M.; Selwitz, R.H.; Oldakowski, R.J.; Brunelle, J.A.; Winn, D.M.; Brown, L.J. Coronal caries in the primary and permanent dentition of children and adolescents 1–17 years of age: United States, 1988–1991. J. Dent. Res. 1996, 75, 631–641. [Google Scholar] [CrossRef] [PubMed]
- Heller, K.E.; Reed, S.G.; Bruner, F.W.; Eklund, S.A.; Burt, B.A. Longitudinal evaluation of sealing molars with and without incipient dental caries in a public health program. J. Public Health Dent. 1995, 55, 148–153. [Google Scholar] [CrossRef] [PubMed]
- Bhuridej, P.; Damiano, P.C.; Kuthy, R.A.; Flach, S.D.; Kanellis, M.J.; Heller, K.E.; Dawson, D.V. Natural history of treatment outcomes of permanent first molars: A study of sealant effectiveness. J. Am. Dent. Assoc. 2005, 136, 1265–1272. [Google Scholar] [CrossRef] [PubMed]
- Handelman, S.L.; Buonocore, M.G.; Heseck, D.J. A preliminary report on the effect of fissure sealant on bacteria in dental caries. J. Prosthet. Dent. 1972, 27, 390–392. [Google Scholar] [CrossRef]
- Primosch, R.E.; Barr, E.S. Sealant use and placement techniques among pediatric dentists. J. Am. Dent. Assoc. 2001, 132, 1442–1451. [Google Scholar] [CrossRef] [PubMed]
- Jodkowska, E. Efficacy of pit and fissure sealing: Long-term clinical observations. Quintessence Int. 2008, 39, 593–602. [Google Scholar] [PubMed]
- Nicholson, J.W. Polyacid-modified composite resins (“compomers”) and their use in clinical dentistry. Dent. Mater. 2007, 23, 615–622. [Google Scholar] [CrossRef] [PubMed]
- Ruse, N.D. What is a “compomers”? J. Can. Dent. Assoc. 1999, 65, 500–504. [Google Scholar] [PubMed]
- Kantovitz, K.R.; Pascon, F.M.; Alonso, R.C.; Nobre-dos-Santos, M.; Rontani, R.M. Marginal adaptation of pit and fissure sealants after thermal and chemical stress. A SEM study. Am. J. Dent. 2008, 21, 377–382. [Google Scholar] [PubMed]
- Mehrabkhani, M.; Mazhari, F.; Sadeghi, S.; Ebrahimi, M. Effects of sealant, viscosity, and bonding agents on microleakage of fissure sealants: An in vitro study. Eur. J. Dent. 2015, 9, 558–563. [Google Scholar] [PubMed]
- Beauchamp, J.; Caufield, P.W.; Crall, J.J.; Donly, K.; Feigal, R.; Gooch, B.; Ismail, A.; Kohn, W.; Siegal, M.; Simonsen, R.; et al. Evidence-based clinical recommendations for the use of pit-and-fissure sealants: A report of the American dental association council on scientific affairs. J. Am. Dent. Assoc. 2008, 139, 257–268. [Google Scholar] [CrossRef] [PubMed]
- Ahovuo-Saloranta, A.; Forss, H.; Walsh, T.; Nordblad, A.; Makela, M.; Worthington, H.V. Pit and fissure sealants for preventing dental decay in permanent teeth. Cochrane Database Syst. Rev. 2017, 7. [Google Scholar] [CrossRef] [PubMed]
- Naaman, R.; El-Housseiny, A.A.; Alamoudi, N. The use of pit and fissure sealants—A literature review. Dent. J. (Basel) 2017, 5, 34. [Google Scholar] [CrossRef] [PubMed]
- Kantovitz, K.R.; Moreira, K.M.; Pascon, F.M.; Nociti, F.H., Jr.; Machado Tabchoury, C.P.; Puppin-Rontani, R.M. Penetration of filled and unfilled resin sealants on different enamel substrates. Pediatr. Dent. 2016, 38, 472–476. [Google Scholar] [PubMed]
- Erbas Unverdi, G.; Atac, S.A.; Cehreli, Z.C. Effectiveness of pit and fissure sealants bonded with different adhesive systems: A prospective randomized controlled trial. Clin. Oral Investig. 2017, 21, 2235–2243. [Google Scholar] [CrossRef] [PubMed]
- Khare, M.; Suprabha, B.S.; Shenoy, R.; Rao, A. Evaluation of pit-and-fissure sealants placed with four different bonding protocols: A randomized clinical trial. Int. J. Paediatr. Dent. 2017, 27, 444–453. [Google Scholar] [CrossRef] [PubMed]
- Rechmann, P.; Sherathiya, K.; Kinsel, R.; Vaderhobli, R.; Rechmann, B.M. Influence of irradiation by a novel CO2 9.3-μm short-pulsed laser on sealant bond strength. Lasers Med. Sci. 2017, 32, 609–620. [Google Scholar] [CrossRef] [PubMed]
- Bhushan, U.; Goswami, M. Evaluation of retention of pit and fissure sealants placed with and without air abrasion pretreatment in 6–8 year old children—An in vivo study. J. Clin. Exp. Dent. 2017, 9, e211–e217. [Google Scholar] [CrossRef] [PubMed]
- Borges, B.C.; de Assuncao, I.V.; de Aquino, C.A.; de Melo Monteiro, G.Q.; Gomes, A.S. Marginal and internal analysis of preheated dental fissure-sealing materials using optical coherence tomography. Int. Dent. J. 2016, 66, 23–28. [Google Scholar] [CrossRef] [PubMed]
- Akinlotan, M.; Chen, B.; Fontanilla, T.M.; Chen, A.; Fan, V.Y. Economic evaluation of dental sealants: A systematic literature review. Community Dent. Oral Epidemiol. 2018, 46, 38–46. [Google Scholar] [CrossRef] [PubMed]
- Twetman, S. Caries risk assessment in children: How accurate are we? Eur. Arch. Paediatr. Dent. 2016, 17, 27–32. [Google Scholar] [CrossRef] [PubMed]
- Mejare, I.; Axelsson, S.; Dahlen, G.; Espelid, I.; Norlund, A.; Tranaeus, S.; Twetman, S. Caries risk assessment. A systematic review. Acta Odontol. Scand. 2014, 72, 81–91. [Google Scholar] [CrossRef] [PubMed]
- Weerheijm, K.L.; van Amerongen, W.E.; Eggink, C.O. The clinical diagnosis of occlusal caries: A problem. ASDC J. Dent. Child. 1989, 56, 196–200. [Google Scholar] [PubMed]
- De Assuncao, I.V.; da Costa Gde, F.; Borges, B.C. Systematic review of noninvasive treatments to arrest dentin non-cavitated caries lesions. World J. Clin. Cases 2014, 2, 137–141. [Google Scholar] [CrossRef] [PubMed]
- Borges, B.C.; de Souza Borges, J.; de Araujo, L.S.; Machado, C.T.; Dos Santos, A.J.; de Assuncao Pinheiro, I.V. Update on nonsurgical, ultraconservative approaches to treat effectively non-cavitated caries lesions in permanent teeth. Eur. J. Dent. 2011, 5, 229–236. [Google Scholar] [PubMed]
- Bakhshandeh, A.; Qvist, V.; Ekstrand, K.R. Sealing occlusal caries lesions in adults referred for restorative treatment: 2–3 years of follow-up. Clin. Oral Investig. 2012, 16, 521–529. [Google Scholar] [CrossRef] [PubMed]
- Borges, B.C.; Campos, G.B.; da Silveira, A.D.; de Lima, K.C.; Pinheiro, I.V. Efficacy of a pit and fissure sealant in arresting dentin non-cavitated caries: A 1-year follow-up, randomized, single-blind, controlled clinical trial. Am. J. Dent. 2010, 23, 311–316. [Google Scholar] [PubMed]
- Borges, B.C.; de Souza Borges, J.; Braz, R.; Montes, M.A.; de Assuncao Pinheiro, I.V. Arrest of non-cavitated dentinal occlusal caries by sealing pits and fissures: A 36-month, randomised controlled clinical trial. Int. Dent. J. 2012, 62, 251–255. [Google Scholar] [CrossRef] [PubMed]
- Borges, B.C.; De Souza Bezerra Araujo, R.F.; Dantas, R.F.; De Araujo Lucena, A.; De Assuncao Pinheiro, I.V. Efficacy of a non-drilling approach to manage non-cavitated dentin occlusal caries in primary molars: A 12-month randomized controlled clinical trial. Int. J. Paediatr. Dent. 2012, 22, 44–51. [Google Scholar] [CrossRef] [PubMed]
- Da Silveira, A.D.; Borges, B.C.; de Almeida Varela, H.; de Lima, K.C.; Pinheiro, I.V. Progression of non-cavitated lesions in dentin through a nonsurgical approach: A preliminary 12-month clinical observation. Eur. J. Dent. 2012, 6, 34–42. [Google Scholar] [PubMed]
- Zandona, A.F.; Swift, E.J., Jr. Critical appraisal. Evidence for sealing versus restoration of early caries lesions. J. Esthet. Restor. Dent. 2015, 27, 55–58. [Google Scholar] [CrossRef] [PubMed]
- Schwendicke, F.; Jager, A.M.; Paris, S.; Hsu, L.Y.; Tu, Y.K. Treating pit-and-fissure caries: A systematic review and network meta-analysis. J. Dent. Res. 2015, 94, 522–533. [Google Scholar] [CrossRef] [PubMed]
- Tagliaferro, E.P.; Pardi, V.; Ambrosano, G.M.; Meneghim Mde, C.; da Silva, S.R.; Pereira, A.C. Occlusal caries prevention in high and low risk schoolchildren. A clinical trial. Am. J. Dent. 2011, 24, 109–114. [Google Scholar] [PubMed]
- Arenholt-Bindslev, D.; Breinholt, V.; Preiss, A.; Schmalz, G. Time-related bisphenol-A content and estrogenic activity in saliva samples collected in relation to placement of fissure sealants. Clin. Oral Investig. 1999, 3, 120–125. [Google Scholar] [CrossRef] [PubMed]
- Schmalz, G.; Preiss, A.; Arenholt-Bindslev, D. Bisphenol-A content of resin monomers and related degradation products. Clin. Oral Investig. 1999, 3, 114–119. [Google Scholar] [CrossRef] [PubMed]
- Fleisch, A.F.; Sheffield, P.E.; Chinn, C.; Edelstein, B.L.; Landrigan, P.J. Bisphenol A and related compounds in dental materials. Pediatrics 2010, 126, 760–768. [Google Scholar] [CrossRef] [PubMed]
- Azarpazhooh, A.; Main, P.A. Is there a risk of harm or toxicity in the placement of pit and fissure sealant materials? A systematic review. J. Can. Dent. Assoc. 2008, 74, 179–183. [Google Scholar] [PubMed]

© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cvikl, B.; Moritz, A.; Bekes, K. Pit and Fissure Sealants—A Comprehensive Review. Dent. J. 2018, 6, 18. https://doi.org/10.3390/dj6020018
Cvikl B, Moritz A, Bekes K. Pit and Fissure Sealants—A Comprehensive Review. Dentistry Journal. 2018; 6(2):18. https://doi.org/10.3390/dj6020018
Chicago/Turabian StyleCvikl, Barbara, Andreas Moritz, and Katrin Bekes. 2018. "Pit and Fissure Sealants—A Comprehensive Review" Dentistry Journal 6, no. 2: 18. https://doi.org/10.3390/dj6020018
APA StyleCvikl, B., Moritz, A., & Bekes, K. (2018). Pit and Fissure Sealants—A Comprehensive Review. Dentistry Journal, 6(2), 18. https://doi.org/10.3390/dj6020018






