The Strange Case of a Broken Periodontal Instrument Tip
Abstract
:1. Introduction
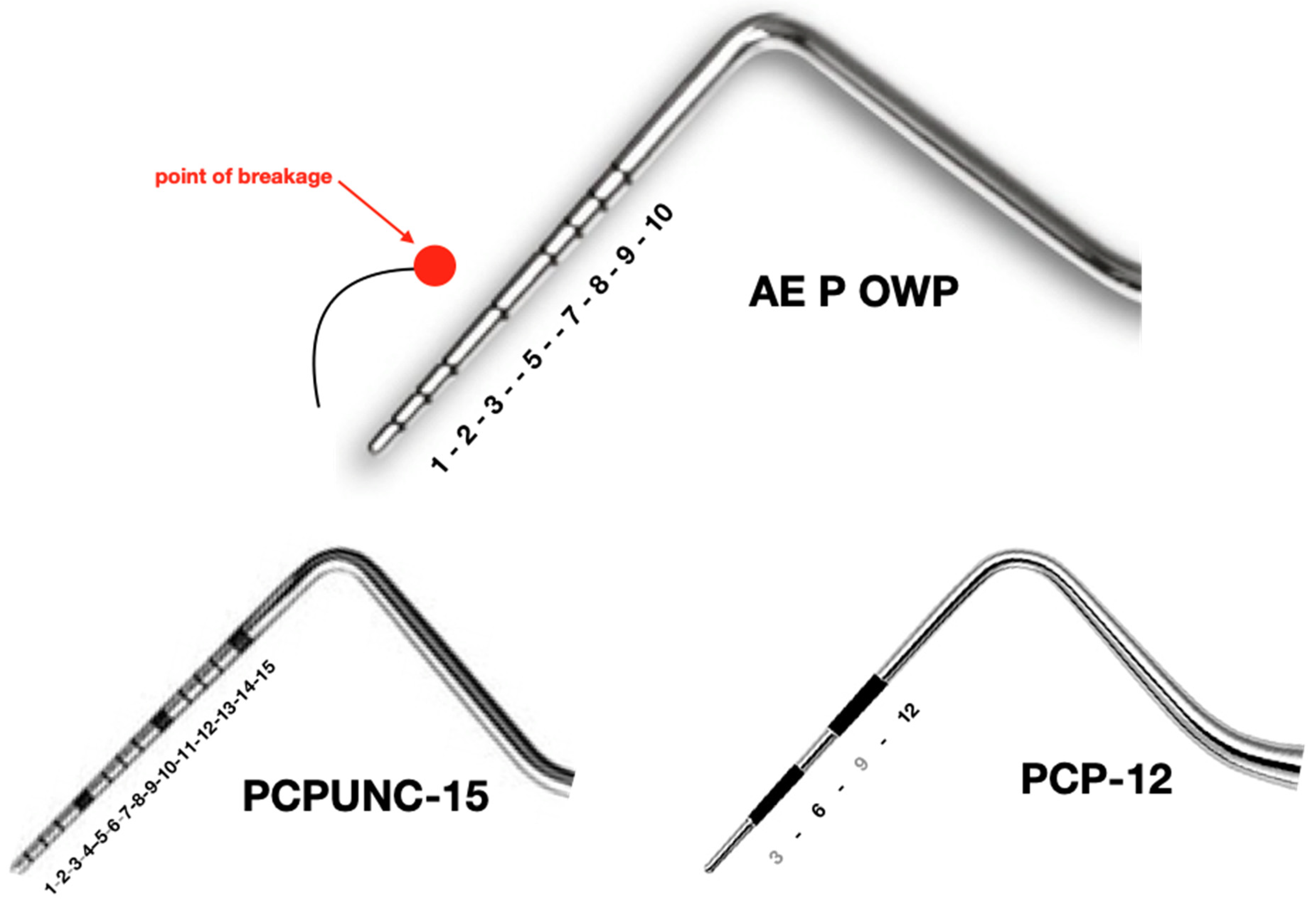
2. Case Report
2.1. Orthopantomography (OPT)
2.2. Digital Volume Tomography (DVT)
2.3. X-ray
3. Diagnosis
4. Therapy
5. Discussion
- Knowledge of instruments (shape, region of use, force, material) is crucial
- Breakage of instruments may occur but must always be communicated by the clinician to the patient
- Removal of a broken instrument is not always indicated depending on the region and contamination of the instrument
- If removal of a broken instrument is indicated, the region should be carefully assessed, if necessary radiographically
6. Conclusions
Supplementary Materials
Author Contributions
Funding
Conflicts of Interest
Ethics Approval and Consent to Participate
Consent for Publication
References
- Rajaran, J.R.; Nazimi, A.J.; Rajandram, R.K. Iatrogenic displacement of high-speed bur during third molar removal. BMJ Case Rep. 2017, 2017. [Google Scholar] [CrossRef] [PubMed]
- Yalcin, S.; Aktas, I.; Emes, Y.; Atalay, B. Accidental displacement of a high-speed handpiece bur during mandibular third molar surgery: A case report. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endodontology 2008, 105, e29–e31. [Google Scholar] [CrossRef] [PubMed]
- Noy, A.F.; Shapira, J. A percutaneous injury by a contaminated instrument is a human bite equivalent. Int. J. Paediatr. Dent. 2010, 21, 74–76. [Google Scholar] [CrossRef]
- Ali, A.; Cunliffe, D.R.; Watt-Smith, S.R. Surgical emphysema and pneumomediastinum complicating dental extraction. Br. Dent. J. 2000, 188, 589–590. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pierro, V.S.D.S.; De Morais, A.P.; Granado, L.; Maia, L.C. An unusual accident during a primary molar extraction. J. Clin. Pediatr. Dent. 2010, 34, 193–195. [Google Scholar] [CrossRef] [PubMed]
- Suter, B. Separated Root Canal Instruments—An overview of incidence, localisation, treatment strategies and outcome. Swiss Dent. J. 2017, 127, 233–237. [Google Scholar]
- Kwon, O.-J.; Lee, J.-K.; Chang, B.-S.; Um, H.-S. Study on broken periodontal curets. J. Korean Acad. Periodontol. 2008, 38, 23. [Google Scholar] [CrossRef] [Green Version]
- Kluess, D.; Zenk, K.; Mittelmeier, W. Reportable incidents with surgical instruments in orthopedic surgery. Orthopade 2014, 43, 561–567. [Google Scholar] [CrossRef]
- Nelson, C.A. Material selection indices for design of surgical instruments with long tubular shafts. J. Med. Eng. Technol. 2013, 37, 102–108. [Google Scholar] [CrossRef]
- Brophy, T.; Srodon, P.; Briggs, C.; Barry, P.; Steatham, J.; Birch, M. Quality of surgical instruments. Ann. R. Coll. Surg. Engl. 2006, 88, 390–393. [Google Scholar] [CrossRef] [Green Version]
- Bhutta, M.F. Fair trade for surgical instruments. BMJ 2006, 333, 297–299. [Google Scholar] [CrossRef] [Green Version]
- Bhutta, M.F. Quality of surgical instruments. Ann. R. Coll. Surg. Engl. 2007, 89, 190. [Google Scholar] [CrossRef] [Green Version]
- Ruprecht, A.; Ross, A. Location of broken instrument fragments. J. Can. Dent. Assoc. 1981, 47, 245. [Google Scholar]
- Balaji, S.M. Burried broken extraction instrument fragment. Ann. Maxillofac. Surg. 2013, 3, 93–94. [Google Scholar] [CrossRef]
- Eggers, G.; Welzel, T.; Mukhamadiev, D.; Wörtche, R.; Hassfeld, S.; Mühling, J. X-ray–based volumetric imaging of foreign bodies: A comparison of computed tomography and digital volume tomography. J. Oral Maxillofac. Surg. 2007, 65, 1880–1885. [Google Scholar] [CrossRef]
- Ramis-Alario, A.; Tarazona-Alvarez, B.; Cervera-Ballester, J.; Soto-Peñaloza, D.; Peñarrocha-Diago, M.; Peñarrocha-Oltra, D.; Peñarrocha-Diago, M. Comparison of diagnostic accuracy between periapical and panoramic radiographs and cone beam computed tomography in measuring the periapical area of teeth scheduled for periapical surgery. A cross-sectional study. J. Clin. Exp. Dent. 2019, 11, e732–e738. [Google Scholar] [CrossRef]
- Dutra-Horstmann, K.L.; Haas, L.; Porporatti, A.L.; Mir, C.F.; Santos, J.N.; Mezzomo, L.A.; Corrêa, M.; Canto, G.D.L. Diagnostic accuracy of cone-beam computed tomography and conventional radiography on apical periodontitis: A systematic review and meta-analysis. J. Endod. 2016, 42, 356–364. [Google Scholar] [CrossRef]
- Sisera, M.; Hofer, D.; Sener, B.; Attin, R.; Schmidlin, P.R. In vitro evaluation of three curettes with edge retention technology after extended use. Schweizer Monatsschrift für Zahnmedizin 2009, 119, 1200–1208. [Google Scholar]
- Moore, U.; Fanibunda, K.; Gross, M. The use of a metal detector for localisation of a metallic foreign body in the floor of the mouth. Br. J. Oral Maxillofac. Surg. 1993, 31, 191–192. [Google Scholar] [CrossRef]
- Wu, A.W.; McCay, L.; Levinson, W.; Iedema, R.; Wallace, G.G.; Boyle, D.J.; McDonald, T.B.; Bismark, M.; Kraman, S.S.; Forbes, E.; et al. Disclosing adverse events to patients: International norms and trends. J. Patient Saf. 2017, 13, 43–49. [Google Scholar] [CrossRef]
- Hammami, M.M.; Al Gaai, E.; Al-Jawarneh, Y.; Amer, H.A.; Hammami, M.B.; Eissa, A.; Al Qadire, M. Patients’ perceived purpose of clinical informed consent: Mill’s individual autonomy model is preferred. BMC Med. Ethics 2014, 15, 2. [Google Scholar] [CrossRef] [Green Version]
- Hammami, M.M.; Al-Jawarneh, Y.; Hammami, M.B.; Al Qadire, M. Information disclosure in clinical informed consent: “reasonable” patient’s perception of norm in high-context communication culture. BMC Med. Ethics 2014, 15, 3. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Turillazzi, E.; Neri, M. Medical error disclosure: From the therapeutic alliance to risk management: The vision of the new Italian code of medical ethics. BMC Med. Ethics 2014, 15, 57. [Google Scholar] [CrossRef] [Green Version]
- Maio, G. The dentist between medicine and cosmetology. Ethical shortcomings of the esthetics boom in dentistry. Schweizer Monatsschrift für Zahnmedizin 2009, 119, 47–56. [Google Scholar]
- O’Toole, B. Promoting access to oral health care: More than professional ethics is needed. J. Dent. Educ. 2006, 70, 1217–1220. [Google Scholar]
- Schwartz, M. The prevention and management of the broken curet. Compend. Contin. Educ. Dent. (Jamesburg N. J. 1995) 1998, 19, 418–420. [Google Scholar]





© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kaufmann, M.E.; Solderer, A.; Hofer, D.; Schmidlin, P.R. The Strange Case of a Broken Periodontal Instrument Tip. Dent. J. 2020, 8, 55. https://doi.org/10.3390/dj8020055
Kaufmann ME, Solderer A, Hofer D, Schmidlin PR. The Strange Case of a Broken Periodontal Instrument Tip. Dentistry Journal. 2020; 8(2):55. https://doi.org/10.3390/dj8020055
Chicago/Turabian StyleKaufmann, Manuela E., Alex Solderer, Deborah Hofer, and Patrick R. Schmidlin. 2020. "The Strange Case of a Broken Periodontal Instrument Tip" Dentistry Journal 8, no. 2: 55. https://doi.org/10.3390/dj8020055
APA StyleKaufmann, M. E., Solderer, A., Hofer, D., & Schmidlin, P. R. (2020). The Strange Case of a Broken Periodontal Instrument Tip. Dentistry Journal, 8(2), 55. https://doi.org/10.3390/dj8020055





