The Use of High Frequency Vibration and Clear Aligners in Management of an Adult Patient with Class III Skeletal Malocclusion with Open Bite and Severe Bimaxillary Protrusion: Case Report
Abstract
:1. Introduction
2. Materials and Methods
2.1. Case Presentation
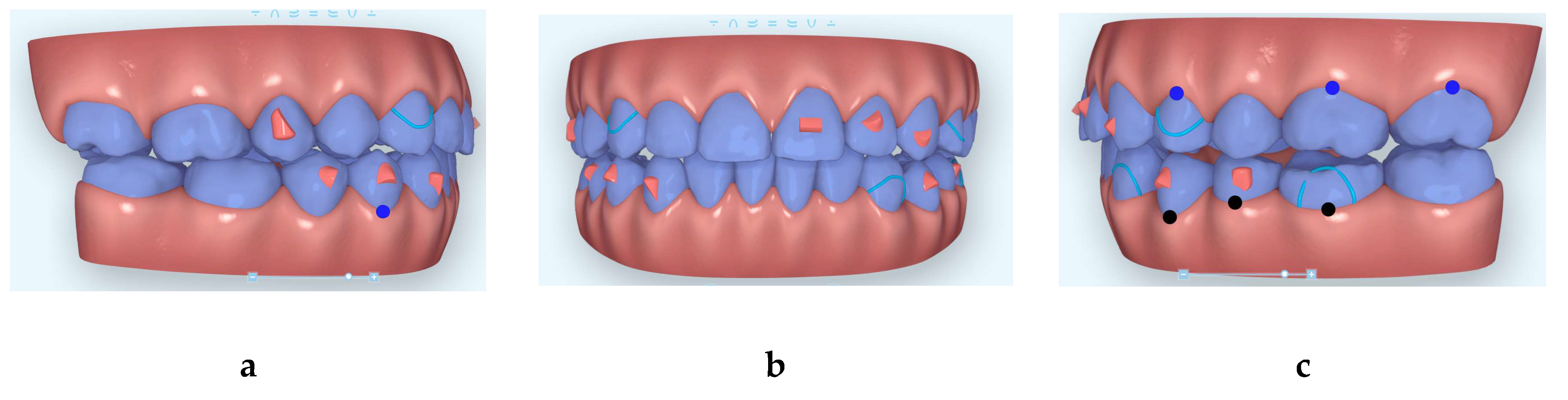
2.2. Treatment Plan and Progress
3. Results
3.1. Clinical Records
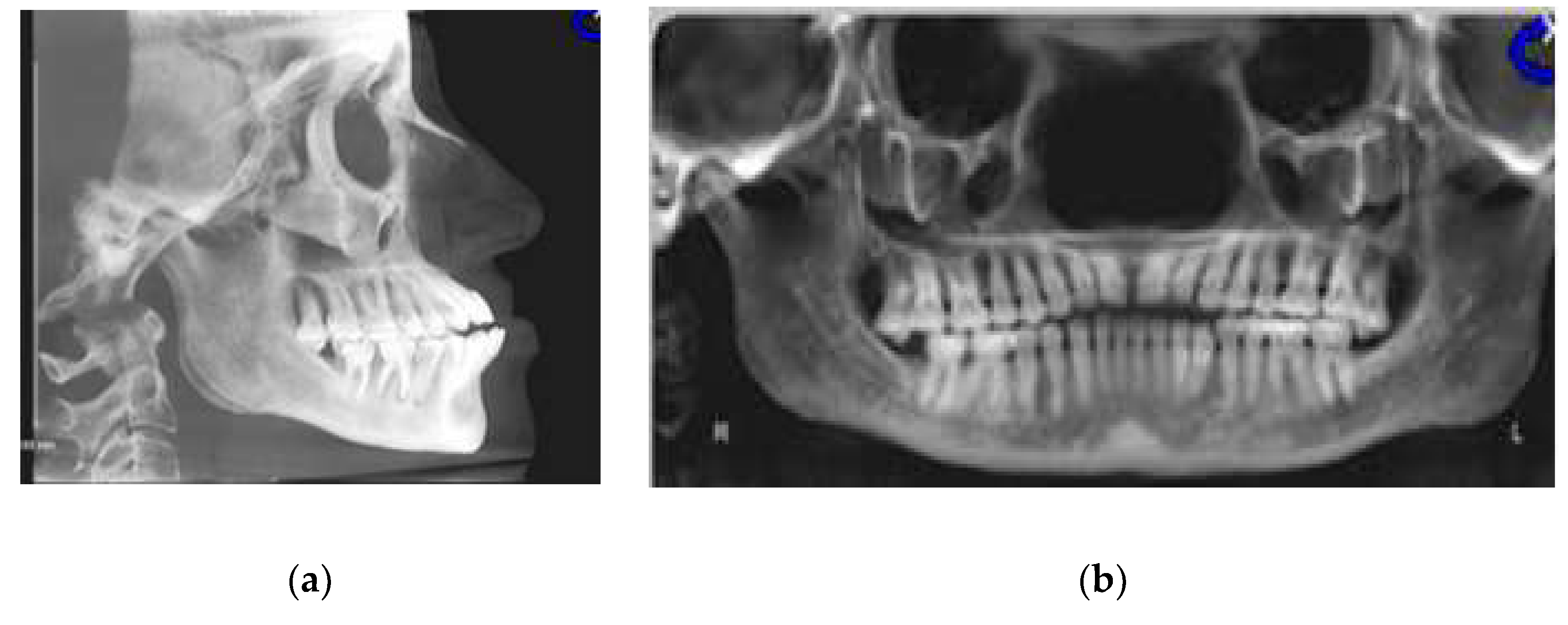
3.2. CBCT-Driven Radiographs
3.2.1. Cephalometric Radiographs and Analysis
3.2.2. Panoramic and Sagittal Screen Radiographs
4. Discussion
5. Conclusions
- The use of multidisciplinary approach in treating similar cases of severe open bite and the coordination between the orthodontist and myofunctional therapist is extremely important to ensure timely treatment and long-term stability.
- The use of HFV can be an important treatment adjunctive therapy in similar cases to minimize orthodontic treatment time as well as to help bone formation where gingival recession was initially present due to the severely proclined incisors.
Funding
Acknowledgments
Conflicts of Interest
References
- Park, J.H.; Kim, T.W. Anterior crossbite correction with a series of clear removable appliances: A case report. J. Esthet. Restor. Dent. 2009, 21, 149–159. [Google Scholar] [CrossRef]
- Garnett, B.S.; Mahood, K.; Nguyen, M.; Al-Khateeb, A.; Liu, S.; Boyd, R.; Oh, H. Cephalometric comparison of adult anterior open bite treatment using clear aligners and fixed appliances. Angle Orthod. 2019, 89, 3–9. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pagani, R.; Signorino, F.; Poli, P.P.; Manzini, P.; Panisi, I. The Use of Invisalign® System in the Management of the Orthodontic Treatment before and after Class III Surgical Approach. Case Rep. Dent. 2016, 2016, 9231219. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kook, M.S.; Kim, H.M.; Oh, H.K.; Lee, K.M. Clear Aligner Use Following Surgery-First Mandibular Prognathism Correction. J. Craniofacial Surg. 2019, 30, e544–e547. [Google Scholar] [CrossRef]
- Bawaskar, N.S. Anterior Crossbite and Crowding Correction with a Series of Clear Aligners Involving Lower Incisor Extraction: “The Clear Way” Case Report. Int. J. Orthod. Milwaukee 2015, 26, 29–33. [Google Scholar]
- Staderini, E.; Meuli, S.; Gallenzi, P. Orthodontic treatment of class three malocclusion using clear aligners: A case report. J. Oral Biol. Craniofacial Res. 2019, 9, 360–362. [Google Scholar] [CrossRef]
- Boyd, R.L. Periodontal and restorative considerations with clear aligner treatment to establish a more favorable restorative environment. Compend. Contin. Educ. Dent. 2009, 30, 280–282. [Google Scholar]
- Giancotti, A.; Garino, F.; Mampieri, G. Use of clear aligners in open bite cases: An unexpected treatment option. J. Orthod. 2017, 44, 114–125. [Google Scholar] [CrossRef] [PubMed]
- Taha, K.; Conley, R.S.; Arany, P.; Warunek, S.; Al-Jewair, T. Effects of mechanical vibrations on maxillary canine retraction and perceived pain: A pilot, single-center, randomized-controlled clinical trial. Odontology 2020, 108, 321–330. [Google Scholar] [CrossRef] [PubMed]
- Farouk, K.; Shipley, T.; El-Bialy, T. Effect of the application of high-frequency mechanical vibration on tooth length concurrent with orthodontic treatment using clear aligners: A retrospective study. J. Orthodont. Sci. 2018, 7, 1–5. [Google Scholar]
- Shipley, T. Effects of High Frequency Acceleration Device on Aligner Treatment—A Pilot Study. Dent. J. 2018, 6, 32. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Shipley, T.; Farouk, K.; El-Bialy, T. Effect of high-frequency vibration on orthodontic tooth movement and bone density. J. Orthod. Sci. 2019, 8, 15. [Google Scholar] [PubMed]
- Alikhani, M.; Alikhani, M.; Alansari, S.; Almansour, A.; Hamidaddin, M.A.; Khoo, E.; Lopez, J.A.; Nervina, J.M.; Nho, J.Y.; Oliveira, S.M.; et al. Therapeutic effect of localized vibration on alveolar bone of osteoporotic rats. PLoS ONE 2019, 14, e0211004. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Alikhani, M.; Alansari, S.; Hamidaddin, M.A.; Sangsuwon, C.; Alyami, B.; Thirumoorthy, S.N.; Oliveira, S.M.; Nervina, J.M.; Teixeira, C.C. Vibration paradox in orthodontics: Anabolic and catabolic effects. PLoS ONE 2018, 13, e0196540. [Google Scholar] [CrossRef] [Green Version]
- Alikhani, M.; Sangsuwon, C.; Alansari, S.; Nervina, J.M.; Teixeira, C.C. High Frequency Acceleration: A New Tool for Alveolar Bone Regeneration. JSM Dent. Surg. 2017, 2, 1026. [Google Scholar]
- Alikhani, M.; Lopez, J.A.; Alabdullah, H.; Vongthongleur, T.; Sangsuwon, C.; Alikhani, M.; Alansari, S.; Oliveira, S.M.; Nervina, J.M.; Teixeira, C.C. High-Frequency Acceleration: Therapeutic Tool to Preserve Bone following Tooth Extractions. J. Dent. Res. 2016, 95, 311–318. [Google Scholar] [CrossRef]
- Pernet, F.; Vento, C.; Pandis, N.; Kiliaridis, S. Long-term evaluation of lower incisors gingival recessions after orthodontic treatment. Eur. J. Orthod. 2019, 41, 559–564. [Google Scholar] [CrossRef]
- Rana, T.K.; Phogat, M.; Sharma, T.; Prasad, N.; Singh, S. Management of gingival recession associated with orthodontic treatment: A case report. J. Clin. Diagn. Res. 2014, 8, ZD05–ZD07. [Google Scholar]
- Kalia, A.; Mirdehghan, N.; Khandekar, S.; Patil, W. Multi-disciplinary approach for enhancing orthodontic esthetics—Case report. Clin. Cosmet. Investig. Dent. 2015, 7, 83–89. [Google Scholar] [CrossRef] [Green Version]
- Egawa, M.; Inagaki, S.; Tomita, S.; Saito, A. Connective Tissue Graft for Gingival Recession in Mandibular Incisor Area: A Case Report. Bull. Tokyo Dent. Coll. 2016, 58, 155–162. [Google Scholar] [CrossRef] [Green Version]
- Sugawara, Y.; Ishihara, Y.; Takano-Yamamoto, T.; Yamashiro, T.; Kamioka, H. Orthodontic treatment of a patient with unilateral orofacial muscle dysfunction: The efficacy of myofunctional therapy on the treatment outcome. Am. J. Orthod. Dentofac. Orthop. 2016, 150, 167–180. [Google Scholar] [CrossRef] [PubMed]








| Measurement | Initial | Final | Norm |
|---|---|---|---|
| SNA (°) | 86.2 | 86.3 | 82 |
| SNB (°) | 86.7 | 86 | 80.9 |
| SN - MP (°) | 28.9 | 29.8 | 32.9 |
| FMA (MP-FH) (°) | 20.8 | 18.9 | 23.9 |
| ANB (°) | −0.5 | 0.3 | 1.6 |
| U1 - NA (mm) | 7.5 | 4.8 | 4.3 |
| U1 - SN (°) | 119 | 109.9 | 102.8 |
| L1 - NB (mm) | 9.4 | 3.7 | 4 |
| L1 - MP (°) | 106.3 | 87.4 | 95 |
| Lower Lip to E-Plane (mm) | 0.5 | −2.8 | −2 |
| Upper Lip to E-Plane (mm) | −6.8 | −6 | −6 |
© 2020 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
El-Bialy, T. The Use of High Frequency Vibration and Clear Aligners in Management of an Adult Patient with Class III Skeletal Malocclusion with Open Bite and Severe Bimaxillary Protrusion: Case Report. Dent. J. 2020, 8, 75. https://doi.org/10.3390/dj8030075
El-Bialy T. The Use of High Frequency Vibration and Clear Aligners in Management of an Adult Patient with Class III Skeletal Malocclusion with Open Bite and Severe Bimaxillary Protrusion: Case Report. Dentistry Journal. 2020; 8(3):75. https://doi.org/10.3390/dj8030075
Chicago/Turabian StyleEl-Bialy, Tarek. 2020. "The Use of High Frequency Vibration and Clear Aligners in Management of an Adult Patient with Class III Skeletal Malocclusion with Open Bite and Severe Bimaxillary Protrusion: Case Report" Dentistry Journal 8, no. 3: 75. https://doi.org/10.3390/dj8030075
APA StyleEl-Bialy, T. (2020). The Use of High Frequency Vibration and Clear Aligners in Management of an Adult Patient with Class III Skeletal Malocclusion with Open Bite and Severe Bimaxillary Protrusion: Case Report. Dentistry Journal, 8(3), 75. https://doi.org/10.3390/dj8030075





