Characteristics of Probiotic Preparations and Their Applications
Abstract
:1. Introduction
2. Dosage Forms Containing Probiotics
2.1. Liquids
2.2. Powder
2.3. Capsules
2.4. Microcapsules
2.5. Tablets
2.6. Suppositories
3. The Site of Action of Probiotics and their Corresponding Dosage Forms
3.1. Oral Cavity
3.2. Upper Respiratory Tract
3.3. Gastrointestinal Tract
3.4. Vagina
4. Factors Affecting Probiotic Survival
4.1. Processing Technology
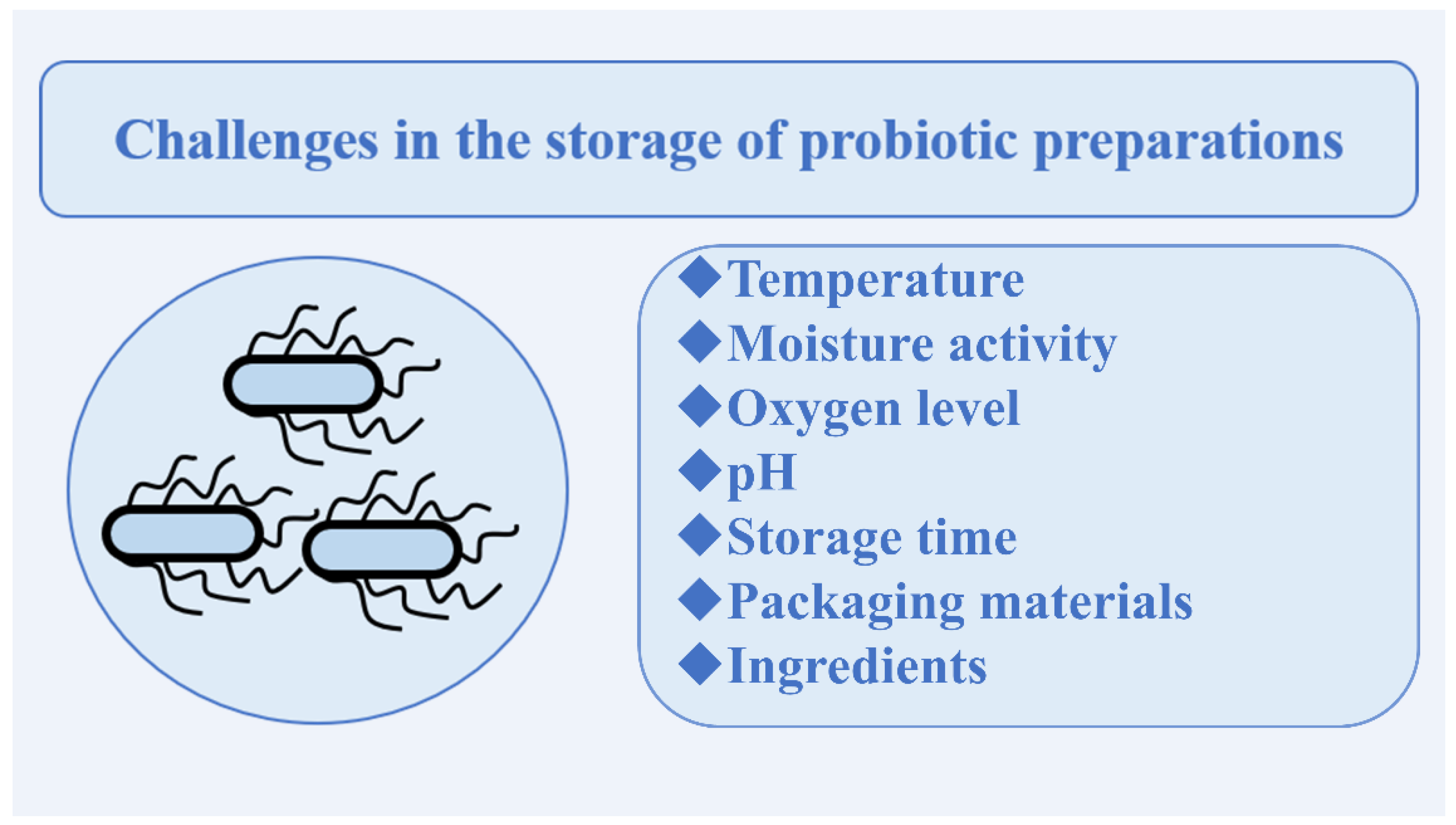
4.2. Storage Conditions
5. Solutions to Increase the Viability of Probiotics
5.1. Common Multifunctional Polymeric Materials
5.2. Nanocarriers
5.3. Lipid Membranes and Biofilms
6. Conclusions
Author Contributions
Funding
Data Availability Statement
Conflicts of Interest
References
- Cunningham, M.; Azcarate-Peril, M.A.; Barnard, A.; Benoit, V.; Grimaldi, R.; Guyonnet, D.; Holscher, H.D.; Hunter, K.; Manurung, S.; Obis, D.; et al. Shaping the Future of Probiotics and Prebiotics. Trends Microbiol. 2021, 29, 667–685. [Google Scholar] [CrossRef] [PubMed]
- Gao, J.; Li, X.; Zhang, G.; Sadiq, F.A.; Simal-Gandara, J.; Xiao, J.; Sang, Y. Probiotics in the Dairy Industry—Advances and Opportunities. Compr. Rev. Food Sci. Food Saf. 2021, 20, 3937–3982. [Google Scholar] [CrossRef] [PubMed]
- Grumet, L.; Tromp, Y.; Stiegelbauer, V. The Development of High-Quality Multispecies Probiotic Formulations: From Bench to Market. Nutrients 2020, 12, 2453. [Google Scholar] [CrossRef]
- Munekata, P.E.S.; Pateiro, M.; Tomasevic, I.; Domínguez, R.; Silva Barretto, A.C.; Santos, E.M.; Lorenzo, J.M. Functional Fermented Meat Products with Probiotics—A Review. J. Appl. Microbiol. 2021, 133, 91–103. [Google Scholar] [CrossRef]
- Han, Y.; Ren, Q. Does Probiotics Work for Bacterial Vaginosis and Vulvovaginal Candidiasis. Curr. Opin. Pharmacol. 2021, 61, 83–90. [Google Scholar] [CrossRef] [PubMed]
- Tripathy, A.; Dash, J.; Kancharla, S.; Kolli, P.; Mahajan, D.; Senapati, S.; Jena, M.K. Probiotics: A Promising Candidate for Management of Colorectal Cancer. Cancers 2021, 13, 3178. [Google Scholar] [CrossRef] [PubMed]
- Badgeley, A.; Anwar, H.; Modi, K.; Murphy, P.; Lakshmikuttyamma, A. Effect of Probiotics and Gut Microbiota on Anti-Cancer Drugs: Mechanistic Perspectives. Biochim. Et Biophys. Acta (BBA) - Rev. Cancer 2021, 1875, 188494. [Google Scholar] [CrossRef]
- Bungau, S.G.; Behl, T.; Singh, A.; Sehgal, A.; Singh, S.; Chigurupati, S.; Vijayabalan, S.; Das, S.; Palanimuthu, V.R. Targeting Probiotics in Rheumatoid Arthritis. Nutrients 2021, 13, 3376. [Google Scholar] [CrossRef]
- Davoodvandi, A.; Marzban, H.; Goleij, P.; Sahebkar, A.; Morshedi, K.; Rezaei, S.; Mahjoubin-Tehran, M.; Tarrahimofrad, H.; Hamblin, M.R.; Mirzaei, H. Effects of Therapeutic Probiotics on Modulation of MicroRNAs. Cell Commun. Signal. 2021, 19, 4. [Google Scholar] [CrossRef]
- Yoha, K.S.; Nida, S.; Dutta, S.; Moses, J.A.; Anandharamakrishnan, C. Targeted Delivery of Probiotics: Perspectives on Research and Commercialization. Probiotics Antimicrob. Proteins 2021, 1–34. [Google Scholar] [CrossRef]
- Amaral, M.; Sousa e Silva, J.; Costa, P.; Gomes, A. Development of Probiotic Dosage Forms. In Probiotic Bacteria; Freitas, A., Ed.; Pan Stanford Publishing: Singapore, 2014; pp. 227–261. [Google Scholar] [CrossRef]
- Zárate, G.; Nader-Macias, M.E. Viability and Biological Properties of Probiotic Vaginal Lactobacilli after Lyophilization and Refrigerated Storage into Gelatin Capsules. Process. Biochem. 2006, 41, 1779–1785. [Google Scholar] [CrossRef]
- Dianawati, D.; Mishra, V.; Shah, N.P. Survival of Microencapsulated Probiotic Bacteria after Processing and during Storage: A Review. Crit. Rev. Food Sci. Nutr. 2016, 56, 1685–1716. [Google Scholar] [CrossRef] [PubMed]
- Kvakova, M.; Bertkova, I.; Stofilova, J.; Savidge, T.C. Co-Encapsulated Synbiotics and Immobilized Probiotics in Human Health and Gut Microbiota Modulation. Foods 2021, 10, 1297. [Google Scholar] [CrossRef] [PubMed]
- Kakiuchi, T.; Mizoe, A.; Yamamoto, K.; Imamura, I.; Hashiguchi, K.; Kawakubo, H.; Yamaguchi, D.; Fujioka, Y.; Nakayama, A.; Okuda, M.; et al. Effect of Probiotics during Vonoprazan-containing Triple Therapy on Gut Microbiota in Helicobacter Pylori Infection: A Randomized Controlled Trial. Helicobacter 2020, 25, e12690. [Google Scholar] [CrossRef]
- Khursheed, R.; Singh, S.K.; Wadhwa, S.; Gulati, M.; Awasthi, A.; Kumar, R.; Ramanunny, A.K.; Kapoor, B.; Kumar, P.; Corrie, L. Exploring Role of Probiotics and Ganoderma Lucidum Extract Powder as Solid Carriers to Solidify Liquid Self-Nanoemulsifying Delivery Systems Loaded with Curcumin. Carbohydr. Polym. 2020, 250, 116996. [Google Scholar] [CrossRef]
- Rasika, D.M.D.; Munasinghe, M.A.D.D.; Vidanarachchi, J.K.; da Cruz, A.G.; Ajlouni, S.; Ranadheera, C.S. Chapter Nine—Probiotics and Prebiotics in Non-Bovine Milk. In Advances in Food and Nutrition Research; da Cruz, A.G., Prudencio, E.S., Esmerino, E.A., da Silva, M.C., Eds.; Probiotic and Prebiotics in Foods: Challenges, Innovations and Advances; Academic Press: Cambridge, MA, USA, 2020; Volume 94, pp. 339–384. [Google Scholar] [CrossRef]
- Sharifi-Rad, J.; Rodrigues, C.F.; Stojanović-Radić, Z.; Dimitrijević, M.; Aleksić, A.; Neffe-Skocińska, K.; Zielińska, D.; Kołożyn-Krajewska, D.; Salehi, B.; Milton Prabu, S.; et al. Probiotics: Versatile Bioactive Components in Promoting Human Health. Medicina 2020, 56, 433. [Google Scholar] [CrossRef]
- Xu, M.; Gagné-Bourque, F.; Dumont, M.-J.; Jabaji, S. Encapsulation of Lactobacillus Casei ATCC 393 Cells and Evaluation of Their Survival after Freeze-Drying, Storage and under Gastrointestinal Conditions. J. Food Eng. 2016, 168, 52–59. [Google Scholar] [CrossRef]
- Inic-Kanada, A.; Stojanovic, M.; Marinkovic, E.; Becker, E.; Stein, E.; Lukic, I.; Djokic, R.; Schuerer, N.; Hegemann, J.H.; Barisani-Asenbauer, T. A Probiotic Adjuvant Lactobacillus Rhamnosus Enhances Specific Immune Responses after Ocular Mucosal Immunization with Chlamydial Polymorphic Membrane Protein C. PLoS ONE 2016, 11, e0157875. [Google Scholar] [CrossRef]
- Rodrigues, F.; Maia, M.J.; das Neves, J.; Sarmento, B.; Amaral, M.H.; Oliveira, M.B.P.P. Vaginal Suppositories Containing Lactobacillus Acidophilus: Development and Characterization. Drug Dev. Ind. Pharm. 2015, 41, 1518–1525. [Google Scholar] [CrossRef]
- Sihra, N.; Goodman, A.; Zakri, R.; Sahai, A.; Malde, S. Nonantibiotic Prevention and Management of Recurrent Urinary Tract Infection. Nat. Rev. Urol 2018, 15, 750–776. [Google Scholar] [CrossRef]
- Aryana, K.J.; Olson, D.W. A 100-Year Review: Yogurt and Other Cultured Dairy Products. J. Dairy Sci. 2017, 100, 9987–10013. [Google Scholar] [CrossRef] [PubMed]
- Nyanzi, R.; Jooste, P.J.; Buys, E.M. Invited Review: Probiotic Yogurt Quality Criteria, Regulatory Framework, Clinical Evidence, and Analytical Aspects. J. Dairy Sci. 2021, 104, 1–19. [Google Scholar] [CrossRef] [PubMed]
- Peluzio, M.d.C.G.; de Moura e Dias, M.; Martinez, J.A.; Milagro, F.I. Kefir and Intestinal Microbiota Modulation: Implications in Human Health. Front. Nutr 2021, 8, 638740. [Google Scholar] [CrossRef]
- Nissen, L.; Casciano, F.; Gianotti, A. Volatilome Changes during Probiotic Fermentation of Combined Soy and Rice Drinks. Food Funct. 2021, 12, 3159–3169. [Google Scholar] [CrossRef] [PubMed]
- Caillard, R.; Lapointe, N. In Vitro Gastric Survival of Commercially Available Probiotic Strains and Oral Dosage Forms. Int. J. Pharm. 2017, 519, 125–127. [Google Scholar] [CrossRef] [PubMed]
- Sady, M.; Najgebauer-Lejko, D.; Domagała, J. The Suitability of Different Probiotic Strains for the Production of Fruit-Whey Beverages. Acta Sci. Pol. Technol. Aliment. 2017, 16, 421–429. [Google Scholar] [CrossRef]
- Hashemi, K.; Hosseini, E. The Stabilizing and Prebiotic Potential of Water-Soluble Phase of Bitter Almond Gum Exudate in Probiotic Yogurt Drink. Carbohydr. Polym. 2021, 255, 117395. [Google Scholar] [CrossRef] [PubMed]
- Zielińska, D.; Marciniak-Lukasiak, K.; Karbowiak, M.; Lukasiak, P. Effects of Fructose and Oligofructose Addition on Milk Fermentation Using Novel Lactobacillus Cultures to Obtain High-Quality Yogurt-like Products. Molecules 2021, 26, 5730. [Google Scholar] [CrossRef]
- Wang, A.; Lin, J.; Zhong, Q. Probiotic Powders Prepared by Mixing Suspension of Lactobacillus Salivarius NRRL B-30514 and Spray-Dried Lactose: Physical and Microbiological Properties. Food Res. Int. 2020, 127, 108706. [Google Scholar] [CrossRef]
- Makinen, K.; Berger, B.; Bel-Rhlid, R.; Ananta, E. Science and Technology for the Mastership of Probiotic Applications in Food Products. J. Biotechnol. 2012, 162, 356–365. [Google Scholar] [CrossRef]
- Meng, X.C.; Stanton, C.; Fitzgerald, G.F.; Daly, C.; Ross, R.P. Anhydrobiotics: The Challenges of Drying Probiotic Cultures. Food Chem. 2008, 106, 1406–1416. [Google Scholar] [CrossRef]
- Yoha, K.S.; Moses, J.A.; Anandharamakrishnan, C. Effect of Encapsulation Methods on the Physicochemical Properties and the Stability of Lactobacillus Plantarum (NCIM 2083) in Synbiotic Powders and in-Vitro Digestion Conditions. J. Food Eng. 2020, 283, 110033. [Google Scholar] [CrossRef]
- Arepally, D.; Reddy, R.S.; Goswami, T.K. Encapsulation of Lactobacillus Acidophilus NCDC 016 Cells by Spray Drying: Characterization, Survival after in Vitro Digestion, and Storage Stability. Food Funct. 2020, 11, 8694–8706. [Google Scholar] [CrossRef] [PubMed]
- Kil, B.J.; Yoon, S.J.; Yun, C.-H.; Huh, C.-S. The Effect of Milk Protein on the Biological and Rheological Properties of Probiotic Capsules. J. Microbiol. Biotechnol. 2020, 30, 1870–1875. [Google Scholar] [CrossRef] [PubMed]
- How, Y.-H.; Yeo, S.-K. Oral Probiotic and Its Delivery Carriers to Improve Oral Health: A Review. Microbiology 2021, 167. [Google Scholar] [CrossRef]
- Dodoo, C.C.; Wang, J.; Basit, A.W.; Stapleton, P.; Gaisford, S. Targeted Delivery of Probiotics to Enhance Gastrointestinal Stability and Intestinal Colonisation. Int. J. Pharm. 2017, 530, 224–229. [Google Scholar] [CrossRef]
- Marzorati, M.; Possemiers, S.; Verhelst, A.; Cadé, D.; Madit, N.; Van de Wiele, T. A Novel Hypromellose Capsule, with Acid Resistance Properties, Permits the Targeted Delivery of Acid-Sensitive Products to the Intestine. LWT - Food Sci. Technol. 2015, 60, 544–551. [Google Scholar] [CrossRef]
- Stegemann, S. Capsules as a Delivery System for Modified-Release Products. In Controlled Release in Oral Drug Delivery; Wilson, C.G., Crowley, P.J., Eds.; Springer: Boston, MA, USA, 2011; pp. 277–298. [Google Scholar] [CrossRef]
- Marzorati, M.; Calatayud, M.; Rotsaert, C.; Van Mele, M.; Duysburgh, C.; Durkee, S.; White, T.; Fowler, K.; Jannin, V.; Bellamine, A. Comparison of Protection and Release Behavior of Different Capsule Polymer Combinations Based on L. Acidophilus Survivability and Function and Caffeine Release. Int. J. Pharm. 2021, 607, 120977. [Google Scholar] [CrossRef]
- Ramos, P.E.; Cerqueira, M.A.; Teixeira, J.A.; Vicente, A.A. Physiological Protection of Probiotic Microcapsules by Coatings. Crit. Rev. Food Sci. Nutr. 2018, 58, 1864–1877. [Google Scholar] [CrossRef]
- Heidebach, T.; Först, P.; Kulozik, U. Microencapsulation of Probiotic Cells for Food Applications. Crit. Rev. Food Sci. Nutr. 2012, 52, 291–311. [Google Scholar] [CrossRef]
- Sarao, L.K.; Arora, M. Probiotics, Prebiotics, and Microencapsulation: A Review. Crit. Rev. Food Sci. Nutr. 2017, 57, 344–371. [Google Scholar] [CrossRef] [PubMed]
- Gioumouxouzis, C.I.; Karavasili, C.; Fatouros, D.G. Recent Advances in Pharmaceutical Dosage Forms and Devices Using Additive Manufacturing Technologies. Drug Discov. Today 2019, 24, 636–643. [Google Scholar] [CrossRef] [PubMed]
- Niamah, A.K.; Gddoa Al-Sahlany, S.T.; Ibrahim, S.A.; Verma, D.K.; Thakur, M.; Singh, S.; Patel, A.R.; Aguilar, C.N.; Utama, G.L. Electro-Hydrodynamic Processing for Encapsulation of Probiotics: A Review on Recent Trends, Technological Development, Challenges and Future Prospect. Food Biosci. 2021, 44, 101458. [Google Scholar] [CrossRef]
- Sierra-Vega, N.O.; Romañach, R.J.; Méndez, R. Feed Frame: The Last Processing Step before the Tablet Compaction in Pharmaceutical Manufacturing. Int. J. Pharm. 2019, 572, 118728. [Google Scholar] [CrossRef]
- Vorländer, K.; Kampen, I.; Finke, J.H.; Kwade, A. Along the Process Chain to Probiotic Tablets: Evaluation of Mechanical Impacts on Microbial Viability. Pharmaceutics 2020, 12, 66. [Google Scholar] [CrossRef] [PubMed]
- Byl, E.; Bladt, P.; Lebeer, S.; Kiekens, F. Importance of Pressure Plasticity during Compression of Probiotic Tablet Formulations. Eur. J. Pharm. Biopharm. 2019, 145, 7–11. [Google Scholar] [CrossRef] [PubMed]
- Purohit, T.J.; Hanning, S.M.; Wu, Z. Advances in Rectal Drug Delivery Systems. Pharm. Dev. Technol. 2018, 23, 942–952. [Google Scholar] [CrossRef]
- Kale, V.V.; Trivedi, R.V.; Wate, S.P.; Bhusari, K.P. Development and Evaluation of a Suppository Formulation Containing Lactobacillus and Its Application in Vaginal Diseases. Ann. N. Y. Acad. Sci. 2005, 1056, 359–365. [Google Scholar] [CrossRef]
- Ventolini, G. Vaginal Lactobacillus: Biofilm Formation in Vivo—Clinical Implications. Int. J. Women’s Health 2015, 7, 243–247. [Google Scholar] [CrossRef]
- Verdenelli, M.C.; Cecchini, C.; Coman, M.M.; Silvi, S.; Orpianesi, C.; Coata, G.; Cresci, A.; Di Renzo, G.C. Impact of Probiotic SYNBIO® Administered by Vaginal Suppositories in Promoting Vaginal Health of Apparently Healthy Women. Curr. Microbiol. 2016, 73, 483–490. [Google Scholar] [CrossRef]
- Kadogami, D.; Nakaoka, Y.; Morimoto, Y. Use of a Vaginal Probiotic Suppository and Antibiotics to Influence the Composition of the Endometrial Microbiota. Reprod. Biol. 2020, 20, 307–314. [Google Scholar] [CrossRef] [PubMed]
- Chen, T.; Yu, W.-H.; Izard, J.; Baranova, O.V.; Lakshmanan, A.; Dewhirst, F.E. The Human Oral Microbiome Database: A Web Accessible Resource for Investigating Oral Microbe Taxonomic and Genomic Information. Database 2010, 2010, baq013. [Google Scholar] [CrossRef] [PubMed]
- Hoare, A.; Marsh, P.D.; Diaz, P.I. Ecological Therapeutic Opportunities for Oral Diseases. Microbiol. Spectr. 2017, 5. [Google Scholar] [CrossRef]
- Kolenbrander, P.E.; Andersen, R.N.; Blehert, D.S.; Egland, P.G.; Foster, J.S.; Palmer, R.J., Jr. Communication among Oral Bacteria. Microbiol. Mol. Biol. Rev. 2002, 66, 486–505. [Google Scholar] [CrossRef]
- Routier, A.; Blaizot, A.; Agossa, K.; Dubar, M. What Do We Know about the Mechanisms of Action of Probiotics on Factors Involved in the Pathogenesis of Periodontitis? A Scoping Review of in Vitro Studies. Arch. Oral Biol. 2021, 129, 105196. [Google Scholar] [CrossRef] [PubMed]
- Seminario-Amez, M.; López-López, J.; Estrugo-Devesa, A.; Ayuso-Montero, R.; Jané-Salas, E. Probiotics and Oral Health: A Systematic Review. Med. Oral Patol Oral Cir. Bucal 2017, 22, e282–e288. [Google Scholar] [CrossRef] [PubMed]
- Sang-Ngoen, T.; Czumbel, L.M.; Sadaeng, W.; Mikó, A.; Németh, D.I.; Mátrai, P.; Hegyi, P.; Tóth, B.; Csupor, D.; Kiss, I.; et al. Orally Administered Probiotics Decrease Aggregatibacter Actinomycetemcomitans but Not Other Periodontal Pathogenic Bacteria Counts in the Oral Cavity: A Systematic Review and Meta-Analysis. Front. Pharm. 2021, 12, 682656. [Google Scholar] [CrossRef]
- Kaźmierczyk-Winciorek, M.; Nędzi-Góra, M.; Słotwińska, S.M. The Immunomodulating Role of Probiotics in the Prevention and Treatment of Oral Diseases. Cent. Eur J. Immunol. 2021, 46, 99–104. [Google Scholar] [CrossRef]
- Nguyen, T.; Brody, H.; Radaic, A.; Kapila, Y. Probiotics for Periodontal Health—Current Molecular Findings. Periodontol 2000 2021, 87, 254–267. [Google Scholar] [CrossRef]
- Tobita, K.; Watanabe, I.; Tomokiyo, M.; Saito, M. Effects of Heat-Treated Lactobacillus Crispatus KT-11 Strain Consumption on Improvement of Oral Cavity Environment: A Randomised Double-Blind Clinical Trial. Benef. Microbes 2018, 9, 585–592. [Google Scholar] [CrossRef]
- Alanzi, A.; Honkala, S.; Honkala, E.; Varghese, A.; Tolvanen, M.; Söderling, E. Effect of Lactobacillus Rhamnosus and Bifidobacterium Lactis on Gingival Health, Dental Plaque, and Periodontopathogens in Adolescents: A Randomised Placebo-Controlled Clinical Trial. Benef. Microbes 2018, 9, 593–602. [Google Scholar] [CrossRef] [PubMed]
- Zupancic, K.; Kriksic, V.; Kovacevic, I.; Kovacevic, D. Influence of Oral Probiotic Streptococcus Salivarius K12 on Ear and Oral Cavity Health in Humans: Systematic Review. Probiotics Antimicro. Prot. 2017, 9, 102–110. [Google Scholar] [CrossRef] [PubMed]
- Cosseau, C.; Devine, D.A.; Dullaghan, E.; Gardy, J.L.; Chikatamarla, A.; Gellatly, S.; Yu, L.L.; Pistolic, J.; Falsafi, R.; Tagg, J.; et al. The Commensal Streptococcus Salivarius K12 Downregulates the Innate Immune Responses of Human Epithelial Cells and Promotes Host-Microbe Homeostasis. Infect. Immun. 2008, 76, 4163–4175. [Google Scholar] [CrossRef] [PubMed]
- Hoffmann, A.; Daniels, R. Ultra–Fast Disintegrating ODTs Comprising Viable Probiotic Bacteria and HPMC as a Mucoadhesive. Eur. J. Pharm. Biopharm. 2019, 139, 240–245. [Google Scholar] [CrossRef]
- Hoffmann, A.; Fischer, J.T.; Daniels, R. Development of Probiotic Orodispersible Tablets Using Mucoadhesive Polymers for Buccal Mucoadhesion. Drug Dev. Ind. Pharm. 2020, 46, 1753–1762. [Google Scholar] [CrossRef]
- Rawls, M.; Ellis, A.K. The Microbiome of the Nose. Ann. Allergy Asthma Immunol. 2019, 122, 17–24. [Google Scholar] [CrossRef]
- De Rudder, C.; Garcia-Tímermans, C.; De Boeck, I.; Lebeer, S.; Van de Wiele, T.; Calatayud Arroyo, M. Lacticaseibacillus Casei AMBR2 Modulates the Epithelial Barrier Function and Immune Response in a Donor-Derived Nasal Microbiota Manner. Sci. Rep. 2020, 10, 16939. [Google Scholar] [CrossRef]
- Lee, J.T.; Kim, C.M.; Ramakrishnan, V. Microbiome and Disease in the Upper Airway. Curr. Opin. Allergy Clin. Immunol. 2019, 19, 1–6. [Google Scholar] [CrossRef]
- Cabana, M.D.; McKean, M.; Caughey, A.B.; Fong, L.; Lynch, S.; Wong, A.; Leong, R.; Boushey, H.A.; Hilton, J.F. Early Probiotic Supplementation for Eczema and Asthma Prevention: A Randomized Controlled Trial. Pediatrics 2017, 140, e20163000. [Google Scholar] [CrossRef]
- Du, X.; Wang, L.; Wu, S.; Yuan, L.; Tang, S.; Xiang, Y.; Qu, X.; Liu, H.; Qin, X.; Liu, C. Efficacy of Probiotic Supplementary Therapy for Asthma, Allergic Rhinitis, and Wheeze: A Meta-Analysis of Randomized Controlled Trials. Allergy Asthma Proc. 2019, 40, 250–260. [Google Scholar] [CrossRef]
- Kim, W.-G.; Kang, G.-D.; Kim, H.I.; Han, M.J.; Kim, D.-H. Bifidobacterium Longum IM55 and Lactobacillus Plantarum IM76 Alleviate Allergic Rhinitis in Mice by Restoring Th2/Treg Imbalance and Gut Microbiota Disturbance. Benef. Microbes 2019, 10, 55–67. [Google Scholar] [CrossRef] [PubMed]
- Zeng, X.-H.; Yang, G.; Liu, J.-Q.; Geng, X.-R.; Cheng, B.-H.; Liu, Z.-Q.; Yang, P.-C. Nasal Instillation of Probiotic Extracts Inhibits Experimental Allergic Rhinitis. Immunotherapy 2019, 11, 1315–1323. [Google Scholar] [CrossRef] [PubMed]
- Passali, D.; Passali, G.C.; Vesperini, E.; Cocca, S.; Visconti, I.C.; Ralli, M.; Bellussi, L.M. The Efficacy and Tolerability of Streptococcus Salivarius 24SMB and Streptococcus Oralis 89a Administered as Nasal Spray in the Treatment of Recurrent Upper Respiratory Tract Infections in Children. Eur Rev. Med. Pharm. Sci 2019, 23, 67–72. [Google Scholar] [CrossRef]
- Santagati, M.; Scillato, M.; Muscaridola, N.; Metoldo, V.; La Mantia, I.; Stefani, S. Colonization, Safety, and Tolerability Study of the Streptococcus Salivarius 24SMBc Nasal Spray for Its Application in Upper Respiratory Tract Infections. Eur. J. Clin. Microbiol. Infect. Dis 2015, 34, 2075–2080. [Google Scholar] [CrossRef] [PubMed]
- Jokicevic, K.; Kiekens, S.; Byl, E.; De Boeck, I.; Cauwenberghs, E.; Lebeer, S.; Kiekens, F. Probiotic Nasal Spray Development by Spray Drying. Eur. J. Pharm. Biopharm. 2021, 159, 211–220. [Google Scholar] [CrossRef] [PubMed]
- Ashaolu, T.J. Immune Boosting Functional Foods and Their Mechanisms: A Critical Evaluation of Probiotics and Prebiotics. Biomed. Pharmacother. 2020, 130, 110625. [Google Scholar] [CrossRef]
- Dong, L.; Xie, J.; Wang, Y.; Zuo, D. Gut Microbiota and Immune Responses. In Gut Microbiota and Pathogenesis of Organ Injury; Chen, P., Ed.; Advances in Experimental Medicine and Biology; Springer: Singapore, 2020; pp. 165–193. [Google Scholar] [CrossRef]
- Gupta, A.; Saha, S.; Khanna, S. Therapies to Modulate Gut Microbiota: Past, Present and Future. World J. Gastroenterol. 2020, 26, 777–788. [Google Scholar] [CrossRef] [PubMed]
- Sevrin, G.; Massier, S.; Chassaing, B.; Agus, A.; Delmas, J.; Denizot, J.; Billard, E.; Barnich, N. Adaptation of Adherent-Invasive E. Coli to Gut Environment: Impact on Flagellum Expression and Bacterial Colonization Ability. Gut Microbes 2020, 11, 364–380. [Google Scholar] [CrossRef]
- Ding, L.; Xiao, X.-H. Gut Microbiota: Closely Tied to the Regulation of Circadian Clock in the Development of Type 2 Diabetes Mellitus. Chin. Med. J. 2020, 133, 817–825. [Google Scholar] [CrossRef]
- Liu, B.-N.; Liu, X.-T.; Liang, Z.-H.; Wang, J.-H. Gut Microbiota in Obesity. World J. Gastroenterol. 2021, 27, 3837–3850. [Google Scholar] [CrossRef]
- Monteagudo-Mera, A.; Rastall, R.A.; Gibson, G.R.; Charalampopoulos, D.; Chatzifragkou, A. Adhesion Mechanisms Mediated by Probiotics and Prebiotics and Their Potential Impact on Human Health. Appl. Microbiol. Biotechnol. 2019, 103, 6463–6472. [Google Scholar] [CrossRef] [PubMed]
- Bi, L.; Yan, B.; Yang, Q.; Li, M.; Cui, H. Probiotic Strategies to Prevent Necrotizing Enterocolitis in Preterm Infants: A Meta-Analysis. Pediatr. Surg. Int. 2019, 35, 1143–1162. [Google Scholar] [CrossRef]
- Martoni, C.J.; Evans, M.; Chow, C.T.; Chan, L.S.; Leyer, G. Impact of a Probiotic Product on Bowel Habits and Microbial Profile in Participants with Functional Constipation: A Randomized Controlled Trial. J. Dig. Dis. 2019, 20, 435–446. [Google Scholar] [CrossRef] [PubMed]
- Nanri, A.; Miyaji, N.; Kochi, T.; Eguchi, M.; Kabe, I.; Mizoue, T. Eating Speed and Risk of Metabolic Syndrome among Japanese Workers: The Furukawa Nutrition and Health Study. Nutrition 2020, 78, 110962. [Google Scholar] [CrossRef] [PubMed]
- Kassaian, N.; Feizi, A.; Aminorroaya, A.; Amini, M. Probiotic and Synbiotic Supplementation Could Improve Metabolic Syndrome in Prediabetic Adults: A Randomized Controlled Trial. Diabetes Metab. Syndr. Clin. Res. Rev. 2019, 13, 2991–2996. [Google Scholar] [CrossRef]
- Kijmanawat, A.; Panburana, P.; Reutrakul, S.; Tangshewinsirikul, C. Effects of Probiotic Supplements on Insulin Resistance in Gestational Diabetes Mellitus: A Double-blind Randomized Controlled Trial. J. Diabetes Investig. 2019, 10, 163–170. [Google Scholar] [CrossRef]
- Palacios, T.; Vitetta, L.; Coulson, S.; Madigan, C.D.; Denyer, G.S.; Caterson, I.D. The Effect of a Novel Probiotic on Metabolic Biomarkers in Adults with Prediabetes and Recently Diagnosed Type 2 Diabetes Mellitus: Study Protocol for a Randomized Controlled Trial. Trials 2017, 18, 7. [Google Scholar] [CrossRef]
- Rezazadeh, L.; Alipour, B.; Jafarabadi, M.A.; Behrooz, M.; Gargari, B.P. Daily Consumption Effects of Probiotic Yogurt Containing Lactobacillus Acidophilus La5 and Bifidobacterium Lactis Bb12 on Oxidative Stress in Metabolic Syndrome Patients. Clin. Nutr. ESPEN 2021, 41, 136–142. [Google Scholar] [CrossRef]
- Rudzki, L.; Ostrowska, L.; Pawlak, D.; Małus, A.; Pawlak, K.; Waszkiewicz, N.; Szulc, A. Probiotic Lactobacillus Plantarum 299v Decreases Kynurenine Concentration and Improves Cognitive Functions in Patients with Major Depression: A Double-Blind, Randomized, Placebo Controlled Study. Psychoneuroendocrinology 2019, 100, 213–222. [Google Scholar] [CrossRef]
- Zeng, C.; Yang, P.; Cao, T.; Gu, Y.; Li, N.; Zhang, B.; Xu, P.; Liu, Y.; Luo, Z.; Cai, H. Gut Microbiota: An Intermediary between Metabolic Syndrome and Cognitive Deficits in Schizophrenia. Prog. Neuro-Psychopharmacol. Biol. Psychiatry 2021, 106, 110097. [Google Scholar] [CrossRef]
- Mastromarino, P.; Vitali, B.; Mosca, L. Bacterial Vaginosis: A Review on Clinical Trials with Probiotics. New Microbiol. 2013, 36, 229–238. [Google Scholar] [PubMed]
- van de Wijgert, J.H.H.M.; Borgdorff, H.; Verhelst, R.; Crucitti, T.; Francis, S.; Verstraelen, H.; Jespers, V. The Vaginal Microbiota: What Have We Learned after a Decade of Molecular Characterization? PLoS ONE 2014, 9, e105998. [Google Scholar] [CrossRef] [PubMed]
- Bohbot, J.M.; Daraï, E.; Bretelle, F.; Brami, G.; Daniel, C.; Cardot, J.M. Efficacy and Safety of Vaginally Administered Lyophilized Lactobacillus Crispatus IP 174178 in the Prevention of Bacterial Vaginosis Recurrence. J. Gynecol. Obstet. Hum. Reprod. 2018, 47, 81–86. [Google Scholar] [CrossRef] [PubMed]
- Buckner, M.M.C.; Ciusa, M.L.; Meek, R.W.; Moorey, A.R.; McCallum, G.E.; Prentice, E.L.; Reid, J.P.; Alderwick, L.J.; Di Maio, A.; Piddock, L.J.V. HIV Drugs Inhibit Transfer of Plasmids Carrying Extended-Spectrum β-Lactamase and Carbapenemase Genes. mBio 2020, 11, e03355-19. [Google Scholar] [CrossRef]
- Almeida, M.O.; do Carmo, F.L.R.; Gala-Garcia, A.; Kato, R.; Gomide, A.C.; Drummond, R.M.N.; Drumond, M.M.; Agresti, P.M.; Barh, D.; Brening, B.; et al. Lactobacillus Crispatus Protects against Bacterial Vaginosis. Genet. Mol. Res. 2019, 18, gmr18475. [Google Scholar] [CrossRef]
- Sánchez, M.T.; Ruiz, M.A.; Castán, H.; Morales, M.E. A Novel Double-Layer Mucoadhesive Tablet Containing Probiotic Strain for Vaginal Administration: Design, Development and Technological Evaluation. Eur. J. Pharm. Sci. 2018, 112, 63–70. [Google Scholar] [CrossRef]
- Laue, C.; Papazova, E.; Liesegang, A.; Pannenbeckers, A.; Arendarski, P.; Linnerth, B.; Domig, K.J.; Kneifel, W.; Petricevic, L.; Schrezenmeir, J. Effect of a Yoghurt Drink Containing Lactobacillus Strains on Bacterial Vaginosis in Women—A Double-Blind, Randomised, Controlled Clinical Pilot Trial. Benef. Microbes 2018, 9, 35–50. [Google Scholar] [CrossRef]
- Vujic, G.; Jajac Knez, A.; Despot Stefanovic, V.; Kuzmic Vrbanovic, V. Efficacy of Orally Applied Probiotic Capsules for Bacterial Vaginosis and Other Vaginal Infections: A Double-Blind, Randomized, Placebo-Controlled Study. Eur. J. Obstet. Gynecol. Reprod. Biol. 2013, 168, 75–79. [Google Scholar] [CrossRef]
- Marcial-Coba, M.S.; Knøchel, S.; Nielsen, D.S. Low-Moisture Food Matrices as Probiotic Carriers. FEMS Microbiol. Lett. 2019, 366, fnz006. [Google Scholar] [CrossRef]
- Savedboworn, W.; Noisumdang, C.; Arunyakanon, C.; Kongcharoen, P.; Phungamngoen, C.; Rittisak, S.; Charoen, R.; Phattayakorn, K. Potential of Protein-Prebiotic as Protective Matrices on the Storage Stability of Vacuum-Dried Probiotic Lactobacillus Casei. LWT 2020, 131, 109578. [Google Scholar] [CrossRef]
- Rajam, R.; Subramanian, P. Encapsulation of Probiotics: Past, Present and Future. Beni-Suef Univ. J. Basic Appl. Sci. 2022, 11, 46. [Google Scholar] [CrossRef]
- Baumann, J.M.; Adam, M.S.; Wood, J.D. Engineering Advances in Spray Drying for Pharmaceuticals. Annu. Rev. Chem. Biomol. Eng. 2021, 12, 217–240. [Google Scholar] [CrossRef]
- Assadpour, E.; Jafari, S.M. Advances in Spray-Drying Encapsulation of Food Bioactive Ingredients: From Microcapsules to Nanocapsules. Annu. Rev. Food Sci. Technol. 2019, 10, 103–131. [Google Scholar] [CrossRef] [PubMed]
- Broeckx, G.; Vandenheuvel, D.; Claes, I.J.J.; Lebeer, S.; Kiekens, F. Drying Techniques of Probiotic Bacteria as an Important Step towards the Development of Novel Pharmabiotics. Int. J. Pharm. 2016, 505, 303–318. [Google Scholar] [CrossRef] [PubMed]
- Jeantet, R.; Jan, G. Improving the Drying of Propionibacterium Freudenreichii Starter Cultures. Appl. Microbiol. Biotechnol. 2021, 105, 3485–3494. [Google Scholar] [CrossRef] [PubMed]
- Huang, S.; Vignolles, M.-L.; Chen, X.D.; Le Loir, Y.; Jan, G.; Schuck, P.; Jeantet, R. Spray Drying of Probiotics and Other Food-Grade Bacteria: A Review. Trends Food Sci. Technol. 2017, 63, 1–17. [Google Scholar] [CrossRef]
- Jakubowska, E.; Lulek, J. The Application of Freeze-Drying as a Production Method of Drug Nanocrystals and Solid Dispersions—A Review. J. Drug Deliv. Sci. Technol. 2021, 62, 102357. [Google Scholar] [CrossRef]
- da Silva Guedes, J.; Pimentel, T.C.; Diniz-Silva, H.T.; Tayse da Cruz Almeida, E.; Tavares, J.F.; Leite de Souza, E.; Garcia, E.F.; Magnani, M. Protective Effects of β-Glucan Extracted from Spent Brewer Yeast during Freeze-Drying, Storage and Exposure to Simulated Gastrointestinal Conditions of Probiotic Lactobacilli. LWT 2019, 116, 108496. [Google Scholar] [CrossRef]
- Haindl, R.; Neumayr, A.; Frey, A.; Kulozik, U. Impact of Cultivation Strategy, Freeze-Drying Process, and Storage Conditions on Survival, Membrane Integrity, and Inactivation Kinetics of Bifidobacterium Longum. Folia Microbiol. 2020, 65, 1039–1050. [Google Scholar] [CrossRef]
- Estilarte, M.L.; Tymczyszyn, E.E.; de los ÁngelesSerradell, M.; Carasi, P. Freeze-Drying of Enterococcus Durans: Effect on Their Probiotics and Biopreservative Properties. LWT 2021, 137, 110496. [Google Scholar] [CrossRef]
- Gul, O.; Atalar, I. Different Stress Tolerance of Spray and Freeze Dried Lactobacillus Casei Shirota Microcapsules with Different Encapsulating Agents. Food Sci. Biotechnol. 2018, 28, 807–816. [Google Scholar] [CrossRef]
- Gaucher, F.; Rabah, H.; Kponouglo, K.; Bonnassie, S.; Pottier, S.; Dolivet, A.; Marchand, P.; Jeantet, R.; Blanc, P.; Jan, G. Intracellular Osmoprotectant Concentrations Determine Propionibacterium Freudenreichii Survival during Drying. Appl. Microbiol. Biotechnol. 2020, 104, 3145–3156. [Google Scholar] [CrossRef] [PubMed]
- Thoorens, G.; Krier, F.; Leclercq, B.; Carlin, B.; Evrard, B. Microcrystalline Cellulose, a Direct Compression Binder in a Quality by Design Environment—A Review. Int. J. Pharm. 2014, 473, 64–72. [Google Scholar] [CrossRef] [PubMed]
- Klayraung, S.; Viernstein, H.; Okonogi, S. Development of Tablets Containing Probiotics: Effects of Formulation and Processing Parameters on Bacterial Viability. Int. J. Pharm. 2009, 370, 54–60. [Google Scholar] [CrossRef]
- Allouche, R.; Dupont, S.; Charriau, A.; Gervais, P.; Beney, L.; Chambin, O. Optimized Tableting for Extremely Oxygen-Sensitive Probiotics Using Direct Compression. Int. J. Pharm. 2018, 538, 14–20. [Google Scholar] [CrossRef] [PubMed]
- Byl, E.; Jokicevic, K.; Kiekens, S.; Lebeer, S.; Kiekens, F. Strain-Specific Differences in Behaviour among Lacticaseibacillus Rhamnosus Cell Wall Mutants during Direct Compression. Int. J. Pharm. 2020, 588, 119755. [Google Scholar] [CrossRef] [PubMed]
- Terpou, A.; Papadaki, A.; Lappa, I.K.; Kachrimanidou, V.; Bosnea, L.A.; Kopsahelis, N. Probiotics in Food Systems: Significance and Emerging Strategies Towards Improved Viability and Delivery of Enhanced Beneficial Value. Nutrients 2019, 11, 1591. [Google Scholar] [CrossRef]
- Vesterlund, S.; Salminen, K.; Salminen, S. Water Activity in Dry Foods Containing Live Probiotic Bacteria Should Be Carefully Considered: A Case Study with Lactobacillus Rhamnosus GG in Flaxseed. Int. J. Food Microbiol. 2012, 157, 319–321. [Google Scholar] [CrossRef]
- Norouzbeigi, S.; Vahid-Dastjerdi, L.; Yekta, R.; Farhoodi, M.; Mortazavian, A.M. Effects of Using Different O2 Scavengers on the Qualitative Attributes of Bifidus Yogurt during Refrigerated Storage. Food Res. Int. 2021, 140, 109953. [Google Scholar] [CrossRef]
- Asgari, S.; Pourjavadi, A.; Licht, T.R.; Boisen, A.; Ajalloueian, F. Polymeric Carriers for Enhanced Delivery of Probiotics. Adv. Drug Deliv. Rev. 2020, 161, 1–21. [Google Scholar] [CrossRef]
- González-Ferrero, C.; Irache, J.M.; González-Navarro, C.J. Soybean Protein-Based Microparticles for Oral Delivery of Probiotics with Improved Stability during Storage and Gut Resistance. Food Chem. 2018, 239, 879–888. [Google Scholar] [CrossRef] [PubMed]
- Gheorghita, R.; Anchidin-Norocel, L.; Filip, R.; Dimian, M.; Covasa, M. Applications of Biopolymers for Drugs and Probiotics Delivery. Polymers 2021, 13, 2729. [Google Scholar] [CrossRef] [PubMed]
- Tan, L.L.; Sampathkumar, K.; Wong, J.H.; Loo, S.C.J. Divalent Cations Are Antagonistic to Survivability of Freeze-Dried Probiotics Encapsulated in Cross-Linked Alginate. Food Bioprod. Processing 2020, 124, 369–377. [Google Scholar] [CrossRef]
- Yan, W.; Jia, X.; Zhang, Q.; Chen, H.; Zhu, Q.; Yin, L. Interpenetrating Polymer Network Hydrogels of Soy Protein Isolate and Sugar Beet Pectin as a Potential Carrier for Probiotics. Food Hydrocoll. 2021, 113, 106453. [Google Scholar] [CrossRef]
- Qi, X.; Simsek, S.; Chen, B.; Rao, J. Alginate-Based Double-Network Hydrogel Improves the Viability of Encapsulated Probiotics during Simulated Sequential Gastrointestinal Digestion: Effect of Biopolymer Type and Concentrations. Int. J. Biol. Macromol. 2020, 165, 1675–1685. [Google Scholar] [CrossRef]
- Mei, L.; He, F.; Zhou, R.-Q.; Wu, C.-D.; Liang, R.; Xie, R.; Ju, X.-J.; Wang, W.; Chu, L.-Y. Novel Intestinal-Targeted Ca-Alginate-Based Carrier for PH-Responsive Protection and Release of Lactic Acid Bacteria. ACS Appl. Mater. Interfaces 2014, 6, 5962–5970. [Google Scholar] [CrossRef]
- Chang, Y.; Yang, Y.; Xu, N.; Mu, H.; Zhang, H.; Duan, J. Improved Viability of Akkermansia Muciniphila by Encapsulation in Spray Dried Succinate-Grafted Alginate Doped with Epigallocatechin-3-Gallate. Int. J. Biol. Macromol. 2020, 159, 373–382. [Google Scholar] [CrossRef]
- Yilmaz, M.T.; Taylan, O.; Karakas, C.Y.; Dertli, E. An Alternative Way to Encapsulate Probiotics within Electrospun Alginate Nanofibers as Monitored under Simulated Gastrointestinal Conditions and in Kefir. Carbohydr. Polym. 2020, 244, 116447. [Google Scholar] [CrossRef]
- Zaeim, D.; Sarabi-Jamab, M.; Ghorani, B.; Kadkhodaee, R.; Liu, W.; Tromp, R.H. Microencapsulation of Probiotics in Multi-Polysaccharide Microcapsules by Electro-Hydrodynamic Atomization and Incorporation into Ice-Cream Formulation. Food Struct. 2020, 25, 100147. [Google Scholar] [CrossRef]
- Zhao, M.; Huang, X.; Zhang, H.; Zhang, Y.; Gänzle, M.; Yang, N.; Nishinari, K.; Fang, Y. Probiotic Encapsulation in Water-in-Water Emulsion via Heteroprotein Complex Coacervation of Type-A Gelatin/Sodium Caseinate. Food Hydrocoll. 2020, 105, 105790. [Google Scholar] [CrossRef]
- Tasch Holkem, A.; Favaro-Trindade, C.S. Potential of Solid Lipid Microparticles Covered by the Protein-Polysaccharide Complex for Protection of Probiotics and Proanthocyanidin-Rich Cinnamon Extract. Food Res. Int. 2020, 136, 109520. [Google Scholar] [CrossRef] [PubMed]
- de Araújo Etchepare, M.; Nunes, G.L.; Nicoloso, B.R.; Barin, J.S.; Moraes Flores, E.M.; de Oliveira Mello, R.; Ragagnin de Menezes, C. Improvement of the Viability of Encapsulated Probiotics Using Whey Proteins. LWT 2020, 117, 108601. [Google Scholar] [CrossRef]
- Xiao, Y.; Lu, C.; Liu, Y.; Kong, L.; Bai, H.; Mu, H.; Li, Z.; Geng, H.; Duan, J. Encapsulation of Lactobacillus Rhamnosus in Hyaluronic Acid-Based Hydrogel for Pathogen-Targeted Delivery to Ameliorate Enteritis. ACS Appl. Mater. Interfaces 2020, 12, 36967–36977. [Google Scholar] [CrossRef] [PubMed]
- Vanden Braber, N.L.; Díaz Vergara, L.I.; Rossi, Y.E.; Aminahuel, C.A.; Mauri, A.N.; Cavaglieri, L.R.; Montenegro, M.A. Effect of Microencapsulation in Whey Protein and Water-Soluble Chitosan Derivative on the Viability of the Probiotic Kluyveromyces Marxianus VM004 during Storage and in Simulated Gastrointestinal Conditions. LWT 2020, 118, 108844. [Google Scholar] [CrossRef]
- Maleki, O.; Khaledabad, M.A.; Amiri, S.; Asl, A.K.; Makouie, S. Microencapsulation of Lactobacillus Rhamnosus ATCC 7469 in Whey Protein Isolate-Crystalline Nanocellulose-Inulin Composite Enhanced Gastrointestinal Survivability. LWT 2020, 126, 109224. [Google Scholar] [CrossRef]
- Niamah, A.K.; Al-Manhel, A.J.; Al-Sahlany, S.T.G. Effect microencapsulation of Saccharomyces boulardii on viability of yeast in vitro and ice cream. Carpathian J. Food Sci. Technol. 2018, 10, 100–107. [Google Scholar]
- Pinpimai, K.; Rodkhum, C.; Chansue, N.; Katagiri, T.; Maita, M.; Pirarat, N. The Study on the Candidate Probiotic Properties of Encapsulated Yeast, Saccharomyces Cerevisiae JCM 7255, in Nile Tilapia (Oreochromis Niloticus). Res. Vet. Sci. 2015, 102, 103–111. [Google Scholar] [CrossRef]
- Sampathkumar, K.; Tan, K.X.; Loo, S.C.J. Developing Nano-Delivery Systems for Agriculture and Food Applications with Nature-Derived Polymers. iScience 2020, 23, 101055. [Google Scholar] [CrossRef]
- McClements, D.J. Nanotechnology Approaches for Improving the Healthiness and Sustainability of the Modern Food Supply. ACS Omega 2020, 5, 29623–29630. [Google Scholar] [CrossRef]
- Barhoum, A.; Pal, K.; Rahier, H.; Uludag, H.; Kim, I.S.; Bechelany, M. Nanofibers as New-Generation Materials: From Spinning and Nano-Spinning Fabrication Techniques to Emerging Applications. Appl. Mater. Today 2019, 17, 1–35. [Google Scholar] [CrossRef]
- Balusamy, B.; Celebioglu, A.; Senthamizhan, A.; Uyar, T. Progress in the Design and Development of “Fast-Dissolving” Electrospun Nanofibers Based Drug Delivery Systems—A Systematic Review. J. Control. Release 2020, 326, 482–509. [Google Scholar] [CrossRef] [PubMed]
- Feng, K.; Zhai, M.-Y.; Zhang, Y.; Linhardt, R.J.; Zong, M.-H.; Li, L.; Wu, H. Improved Viability and Thermal Stability of the Probiotics Encapsulated in a Novel Electrospun Fiber Mat. J. Agric. Food Chem. 2018, 66, 10890–10897. [Google Scholar] [CrossRef] [PubMed]
- Jayani, T.; Sanjeev, B.; Marimuthu, S.; Uthandi, S. Bacterial Cellulose Nano Fiber (BCNF) as Carrier Support for the Immobilization of Probiotic, Lactobacillus Acidophilus 016. Carbohydr. Polym. 2020, 250, 116965. [Google Scholar] [CrossRef] [PubMed]
- Feng, P.; Cao, Z.; Wang, X.; Li, J.; Liu, J. On-Demand Bacterial Reactivation by Restraining within a Triggerable Nanocoating. Adv. Mater. 2020, 32, 2002406. [Google Scholar] [CrossRef] [PubMed]
- Tawfeek, H.M.; Abdellatif, A.A.H.; Dennison, T.J.; Mohammed, A.R.; Sadiq, Y.; Saleem, I.Y. Colonic Delivery of Indometacin Loaded PGA-Co-PDL Microparticles Coated with Eudragit L100-55 from Fast Disintegrating Tablets. Int. J. Pharm. 2017, 531, 80–89. [Google Scholar] [CrossRef] [PubMed]
- Cao, Z.; Wang, X.; Pang, Y.; Cheng, S.; Liu, J. Biointerfacial Self-Assembly Generates Lipid Membrane Coated Bacteria for Enhanced Oral Delivery and Treatment. Nat. Commun. 2019, 10, 5783. [Google Scholar] [CrossRef]
- Tolker-Nielsen, T. Biofilm Development. Microbiol. Spectr. 2015, 3. [Google Scholar] [CrossRef]
- Wang, X.; Cao, Z.; Zhang, M.; Meng, L.; Ming, Z.; Liu, J. Bioinspired Oral Delivery of Gut Microbiota by Self-Coating with Biofilms. Sci. Adv. 2020, 6, eabb1952. [Google Scholar] [CrossRef]
| Polymer | Form | Survival Rate and Stability of the Strains | Reference | |
|---|---|---|---|---|
| Lacticaseibacillus paracasei KS-199 | Alginate | Electrospun nanofiber | The survival rate of the strain after electrostatic spinning was 85.87%. Under simulated gastrointestinal conditions, the survival rate of the encapsulated strain increased from 51.8% to 70.8%. | [132] |
| L. plantarum | Ca-alginate and chitosan | Microcapsule | The viability of the strains mixed with inulin was 7.23 ± 0.21 and 9.15 ± 0.33 log CFU/g at 25 °C and 4 °C storage, respectively. The viability of the strains mixed with inulin or resistant starch after 90 days of storage was 7.37 ± 0.12 and 7.82 ± 0.39 log CFU/g, respectively. | [133] |
| Limosilactobacillus reuteri | Type-A gelatin/sodium caseinate (GE/Cas), type-A gelatin/gum arabic (GE/GA) | Microcapsule | The survival of the strains decreased in the order GE/Cas > Cas > GE/GA > GE after simulated digestion, heating and ambient storage. | [134] |
| Bifidobacterium animalis subsp. lactis BLC1 | Proanthocyanidin-rich cinnamon extract (PRCE) | Microparticle | The encapsulation rate of probiotics with the combination of BLC1 and 5% PRCE was 98.59 ± 0.45%. After 120 days of storage at 7 °C, the viability of BLC1 was 9.30 ± 0.16 log CFU/g. | [135] |
| L.paracasei LS14 | Soy protein isolate (SPI) and sugar beet pectin (SBP) | Hydrogel | The survival rate of probiotics encapsulated in an SPI/SBP hydrogel in simulated gastric juice was greater than 96.4%. The greatest storage stability was seen for the probiotic wrapped in an interpenetrating polymer network hydrogel containing 10% SPI, 3.5% SBP and 10 U laccase. | [128] |
| L. acidophilus La-14 | Calcium alginate, whey proteins and sodium alginate | Microparticle | The multilayer calcium alginate particles were encapsulated with greater than 80% efficiency and had high strain viability when exposed to simulated gastrointestinal and thermal treatment conditions. The combination of whey protein and one layer of sodium alginate coating was optimal. | [136] |
| L.rhamnosus | Hyaluronic acid | Microcapsule | The hydrogel was most stable at a concentration of 4% (w/v). The viability under a simulated gastrointestinal tract and the storage stability of the strains were enhanced after microencapsulation. | [137] |
| Kluyveromyces marxianus VM004 | Whey protein concentrate (WPC) and water-soluble chitosan (WSCh) | Microcapsule | After spray drying, the probiotic powder had a viability of 8.38 log CFU/g. At 30% (w/v) solids (29:1 WPC:WSCh), the survival rate of the strain after a gastrointestinal tolerance test was up to 95%. | [138] |
| L. rhamnosus ATCC 7469 | Whey protein isolate, crystalline nanocellulose and inulin | Microcapsule | The probiotic bacteria encapsulated in the microcapsules remained active up to 3.2 × 105 CFU/g after being exposed to simulated gastric fluid at 37 °C for 60 min and then exposed to 0.6% bile salt at pH 7.34 for 120 min. | [139] |
| Saccharomyces boulardii ATCC MYA-796 | Alginate and alginate–chitosan | Microcapsule | The survival rates of alginate- and alginate–chitosan-microencapsulated yeast were 80% and 90% after 240 h of treatment with simulated gastric fluid and 80% and 85% after 240 h of treatment with simulated intestinal fluid. | [140] |
| Saccharomyces cerevisiae JCM 7255 | Alginate and skim milk | Microcapsule | The survival rates of encapsulated yeast under simulated gastric and bile conditions were significantly higher and remained high after 14 days of storage at 25 °C. | [141] |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wang, G.; Chen, Y.; Xia, Y.; Song, X.; Ai, L. Characteristics of Probiotic Preparations and Their Applications. Foods 2022, 11, 2472. https://doi.org/10.3390/foods11162472
Wang G, Chen Y, Xia Y, Song X, Ai L. Characteristics of Probiotic Preparations and Their Applications. Foods. 2022; 11(16):2472. https://doi.org/10.3390/foods11162472
Chicago/Turabian StyleWang, Guangqiang, Yunhui Chen, Yongjun Xia, Xin Song, and Lianzhong Ai. 2022. "Characteristics of Probiotic Preparations and Their Applications" Foods 11, no. 16: 2472. https://doi.org/10.3390/foods11162472
APA StyleWang, G., Chen, Y., Xia, Y., Song, X., & Ai, L. (2022). Characteristics of Probiotic Preparations and Their Applications. Foods, 11(16), 2472. https://doi.org/10.3390/foods11162472







