Abstract
Huangshan Maofeng green tea (HMGT) is one of the most well-known green teas consumed for a thousand years in China. Research has demonstrated that consumption of green tea effectively improves metabolic disorders. However, the underlying mechanisms of obesity prevention are still not well understood. This study investigated the preventive effect and mechanism of long-term intervention of Huangshan Maofeng green tea water extract (HTE) on obesity-associated metabolic disorders in leptin receptor knockout (Lepr−/−) rats by using gut microbiota and hepatic lipidomics data. The Lepr−/− rats were administered with 700 mg/kg HTE for 24 weeks. Our results showed that HTE supplementation remarkably reduced excessive fat accumulation, as well as ameliorated hyperlipidemia and hepatic steatosis in Lepr−/− rats. In addition, HTE increased gut microbiota diversity and restored the relative abundance of the microbiota responsible for producing short chain fatty acids, including Ruminococcaceae, Faecalibaculum, Veillonellaceae, etc. Hepatic lipidomics analysis found that HTE significantly recovered glycerolipid and glycerophospholipid classes in the liver of Lepr−/− rats. Furthermore, nineteen lipid species, mainly from phosphatidylcholines (PCs), phosphatidylethanolamines (PEs), and triglycerides (TGs), were significantly restored increases, while nine lipid species from TGs and diglycerides (DGs) were remarkably recovered decreases by HTE in the liver of Lepr−/− rats. Our results indicated that prevention of obesity complication by HTE may be possible through maintaining homeostasis of gut microbiota and certain hepatic lipid classes.
1. Introduction
Obesity is becoming an important public health issue around the world, and it is a cluster of the dangerous risk factors linked to metabolic syndrome, type 2 diabetes, hypertension, and cardiovascular disease [1,2,3]. Recent studies have shown that obese individuals are more likely to develop COVID–19 [4,5]. According to the definition of obesity by the World Health Organization (WHO), the ranges of body mass index (BMI, in kg/m2) ≥ 25 are overweight, and BMI ≥ 30 are obesity. Right now, 1.9 billion adults are overweight, over 650 million of them are obese, and the prevalence of obesity is expected to rise in the future [6,7]. Apparently, there is a desperate need for effective management of obesity. However, treating obesity with medicines is commonly associated with a variety of side effects [8,9,10], such as gastrointestinal dysfunction, hepatotoxicity, statin–related myotoxicity, etc. Interestingly, studies have shown that foods and their functional ingredients can prevent obesity and other metabolic diseases with fewer side effects [11,12,13]. Thus, the investigation of dietary interventions in the prevention of obesity and their potential mechanisms is of important significance to public health. The development of obesity may be a result of a combination of genetic and environmental factors [7,14], such as unhealthy eating habits and lifestyle. Recent researches have shown that the composition and metabolic functions of gut microbiota play a crucial role in obesity development [15,16]. Emerging evidence has revealed that foods and their functional components can affect the metabolism of lipids and prevent obesity through altering gut microbiota composition [17,18,19], which indicates that gut microbiota may serve as a potential new target for obesity prevention.
Tea is one of the most popular drinks in the world, and contains a wide variety of bioactive compounds [20], such as catechins, theanine, caffeine, polysaccharides, etc. Previous research has indicated that drinking tea or consuming tea ingredients has health benefits to the public, such as reducing body weight, alleviating metabolic syndrome, preventing cardiovascular diseases and cancer, and improving cognitive ability [17,21,22,23]. Recent studies reported that consuming tea could modulate gut microbiota to improve host metabolism, indicating a possible role of microbiota in regulating health benefits related to tea drinking, such as hypoglycemia and weight loss [23,24,25]. Liu et al. reported that Fuzhuan brick tea attenuates obesity by altering gut bacteria in high-fat diet-induced mice [26]. Chen et al. also reported that tea polyphenols lower blood glucose levels by changing gut microbiota in db/db mice [27]. Our previous studies found that large yellow tea ameliorated metabolic disorders by reducing lipogenesis and altering microbiota in leptin receptor knockout rats [28]. Huangshan Maofeng green tea (HMGT) is one of the most famous green teas, which has been produced and consumed for a thousand years in China [29]. The tea trees used for making HMGT grow at altitudes above 700 m around Huangshan Mountain in Anhui province, China [30]. Cui et al. reported that HMGT extract protected mice from CCl4–induced liver damage [31]. Our previous studies proved that HMGT supplementation prevented hypertension induced by desoxycorticosterone acetate and salt in old C57BL/6 mice [32]. However, the effect and mechanism of HSMF in preventing obesity complication are not well understood. Notably, potential roles of gut microbiota and lipidomic classes regulated by HMGT in obesity prevention remains unclear.
The liver is an important organ that regulates nutrition metabolism along with energy balance [33]. Dysregulation of hepatic lipid metabolism can result in hepatic steatosis, obesity, and other comorbidities [28,34,35]. However, traditional biochemical data cannot provide detailed information on which classes of lipids or lipidomic pathways are compromised with obesity complication. Lipidomics has recently emerged as a new way of measuring lipid classes and identifying biomarkers associated with lipid metabolism [36]. Shon et al. studied the obesity-prevention effect of Chrysanthemum morifolium Ramat leaves using plasma lipidomics [37]. In addition, Nam et al. reported that green tea ethanol extracts improved lipid profiles in mice fed a high-fat diet using lipidomics analysis [38]. So far, few studies have utilized lipidomics to explore how green tea alters the profiles of hepatic lipid metabolism.
The Lepr−/− rat is a newly developed leptin receptor knockout rat model characterized by obesity, glucose intolerance, and dyslipidemia, which is proven to be a suitable animal model to study obesity complication [28,39,40]. In this study, the combination of both gut microbiota and hepatic lipid profiles data were applied to investigate the preventive mechanism of obesity-associated metabolic disorders by long term intervention of Huangshan Maofeng green tea water extracts (HTE) in Lepr−/− rats model.
2. Materials and Methods
2.1. Chemical Analysis of Huangshan Maofeng Green Tea Water Extracts
HSMF samples were obtained from the Huangshan Maofeng Tea Group Company (Anhui, China). HSMF was powdered and extracted three times by boiled water with ultrasound assistance according to our previous method [12]. Afterwards, the extractions were concentrated under vacuum and lyophilized, yielding HSMF water extracts (HTE) which were stored at minus 80 °C. Table 1 lists the main ingredients in HTE determined by our previous method [28].

Table 1.
Contents of catechins, polysaccharide, caffeine, and amino acid in lyophilized powder of tea water extracts.
2.2. Animals Experiment
Leptin receptor knockout (Lepr−/−) rats (Sprague-Dawley background) were obtained from the Chinese Academy of Medical Sciences (Beijing, China). The rats were free to drink and eat and were kept in the specific pathogen free laboratory animal center (temperature 22 ± 1 °C, relative humidity 50 ± 5% with 12 h light−dark cycle). At the age of seven weeks, Lepr−/− rats were randomly divided into the Lepr−/− control group (KO) (n = 6) and the Lepr−/− with HTE intervention group (KH) (n = 6). Wild type littermates are considered as the WT control group (WT) (n = 6). The rats in the KH group were given 700 mg/kg HTE by oral gavage once every day for a total of 24 weeks, and the rats in the control group were administered the same amount of water. The HTE was prepared freshly every day at the concentration of 100 mg/mL just before administration. The ethical protocol for animal study was approved on 4 April 2019 by the Institutional Animal Care and Use Committee of the Anhui Agricultural University (ethical code: AHAU 2019–034).
The TP23512 diet for rats was purchased from Trophic Animal Feed Co., Ltd. (Nantong, China, Table S1). Fat mass and lean mass were determined as body composition analysis by using minispec LF90II Analyzer (Bruker, Germany) according to our previous method [41]. At the end of the experiment, rats were sacrificed after being anesthetized with pentobarbital sodium following a fast of 12 h. The blood, liver, inguinal, and epididymal adipose tissues were collected for further study. The formula for calculating Lee’s index is as follows: Lee’s index = body weight (g) ^ (1/3) × 1000/body length (cm) [42].
2.3. Serum Biochemical Analysis
The levels of triglyceride (TG), total cholesterol (T-CHO), low–density lipoprotein cholesterol (LDL-C) in serum and liver tissue, as well as serum aspartate transaminase (AST) and alanine aminotransferase (ALT) levels were determined using activity assay kits (Jiancheng Biotech, Nanjing, China). In addition, the levels of free fatty acid (FFA) were determined using enzyme linked immunosorbent assay (ELISA) kits (Jianglai Biotech, Shanghai, China) according to operating instructions.
2.4. Histopathological Analysis
Histopathological analysis was carried out according to the previous method [43]. Briefly, formalin-fixed liver and adipose tissue samples were paraffin-embedded, sectioned at 5 μm, and stained with hematoxylin and eosin (H & E) for histological analysis. In addition, formalin-fixed liver tissue samples were sectioned at 10 μm and stained with Oil red O (ORO) staining. Images were taken by microscope at 100× or 400× magnification. The area of the white adipocytes and the hepatic lipid were determined using Image-J software (NIH, Bethesda, MD, USA).
2.5. RNA Isolation and Real-Time PCR Analysis
Real-time PCR analysis was performed according to our previous method [44]. To measure the expression of hepatic lipogenic gene in the liver samples, total RNA was extracted by RNA-easy Isolation Reagent (Vazyme, Nanjing, China). cDNA was synthesized using HiScript II cDNA Synthesis kit (Vazyme, Nanjing, China). Quantitative real-time PCR (qRT-PCR) was conducted using AceQ qPCR SYBR Green kit (Vazyme, Nanjing, China). The relative quantification was performed using the 2−ΔΔCt method. The primer sequences are listed in Table S2 of the Supplementary Materials.
2.6. Analysis of Liver Lipidomics
Each sample preparation used 30 mg of liver tissue. The tissue sample was pulverized in liquid nitrogen. Then, 300 μL of PBS was added to liver tissue powder and vortexed to mix well. Next, 429 μL of methyl tert–butyl ether, 342 μL of methanol, and 429 μL of H2O was added and vortexed for 1 min, followed by centrifugation at 2000× g at 4 °C for 5 min. After that, the supernatant was evaporated at −20 °C, and then 100 μL isopropanol was added to the dried mixture, which was vortexed for 3 min. The mixture samples were centrifuged again at 12,000× g for 15 min. The supernatant was collected in a glass vial for analysis.
Lipidomic analysis was accomplished using Ultimate HPLC system (ThermoFisher Scientific, Waltham, MA, USA) equipped with XBridge BEH HILIC (100 mm × 2.1 mm, 2.5 μm; Waters, Milford, MA, USA). MS detection was executed on an Q Exactive Focus Oribitrap MS/MS system (Thermo Fisher Scientific, Waltham, MA, USA). Mass spectra and chromatograms were acquired and processed with Xcalibur. The Automated Identification Engine for Lipidomics Version 4.0 software was used to determine the chemical formula for product and precursor ions. Univariate and multivariate analysis were conducted by metaboanalyst 5.0. The data analysis for the study was conducted according to previous methods [45].
2.7. Analysis of Gut Microbiota
Colon content samples were collected and frozen in liquid nitrogen immediately after the rats were sacrificed, and then stored at −80 °C until use. Total DNA in colon content samples was isolated, amplified, and constructed using SMRT Bell library according to our previous methods [28]. The colonic microbiota composition was assessed by the PacBio RS II platform and QIIME package was used for obtaining high–quality sequences. For precise operational taxonomic unit (OTU) analysis, the high–quality sequences with similarity > 97% were classified into OTU through UCLUST. Based upon an 80% confidence threshold, the OTU representative sequences were taxonomized using the Ribosomal Database Project II database.
2.8. Quantification of Fecal Short–Chain Fatty Acids
The samples of rat feces were collected and frozen in liquid nitrogen, and then stored at −80 °C until analysis was performed. The level of short–chain fatty acids (SCFAs) in the feces was extracted and measured using a gas chromatography method according to a previous study [46]. Determination of fecal SCFAs was performed by gas chromatography equipped with a flame ionization detector (Agilent 5977, Santa Clara, CA, USA). The concentrations of fecal SCFAs were quantified using external calibration curves.
2.9. Statistical Analysis
Results are presented as mean ± SEM. Student’s t–test was used to assess the significance of the statistical difference between the two groups, and multiple group comparisons were performed by one–way ANOVA. Using GraphPad Prism, we first ascertained whether data showed normal distribution. Then, equal normality test was performed. Parametric analysis was performed using one-way ANOVA followed by Tukey’s test. This reaches statistical significance when the p-value was less than 0.05.
3. Results
3.1. Main Chemical Compounds in Huangshan Maofeng Green Tea Water Extract
The major catechins, polysaccharide, caffeine, and amino acid in HTE were determined and shown in Table 1. According to the results, total catechins (381.84 ± 4.56 mg/g), polysaccharide (153.89 ± 1.36 mg/g), and caffeine (106.92 ± 0.93 mg/g) are the main chemical components in HTE. Large yellow tea is one of the most famous traditional yellow teas in China, which is known to prevent metabolic syndrome significantly [12,28]. Comparing the main chemical compounds in large yellow tea extracts (LTE), the HTE contained a higher concentration of total catechins, total amino acid, and (−)-epigallocatechin gallate (EGCG) (p < 0.05). However, the content of (−)-gallocatechin gallate (GCG), (−)-gallocatechin gallate (GC), polysaccharide, and caffeine in HTE was evidently lower than that of LTE (p < 0.05).
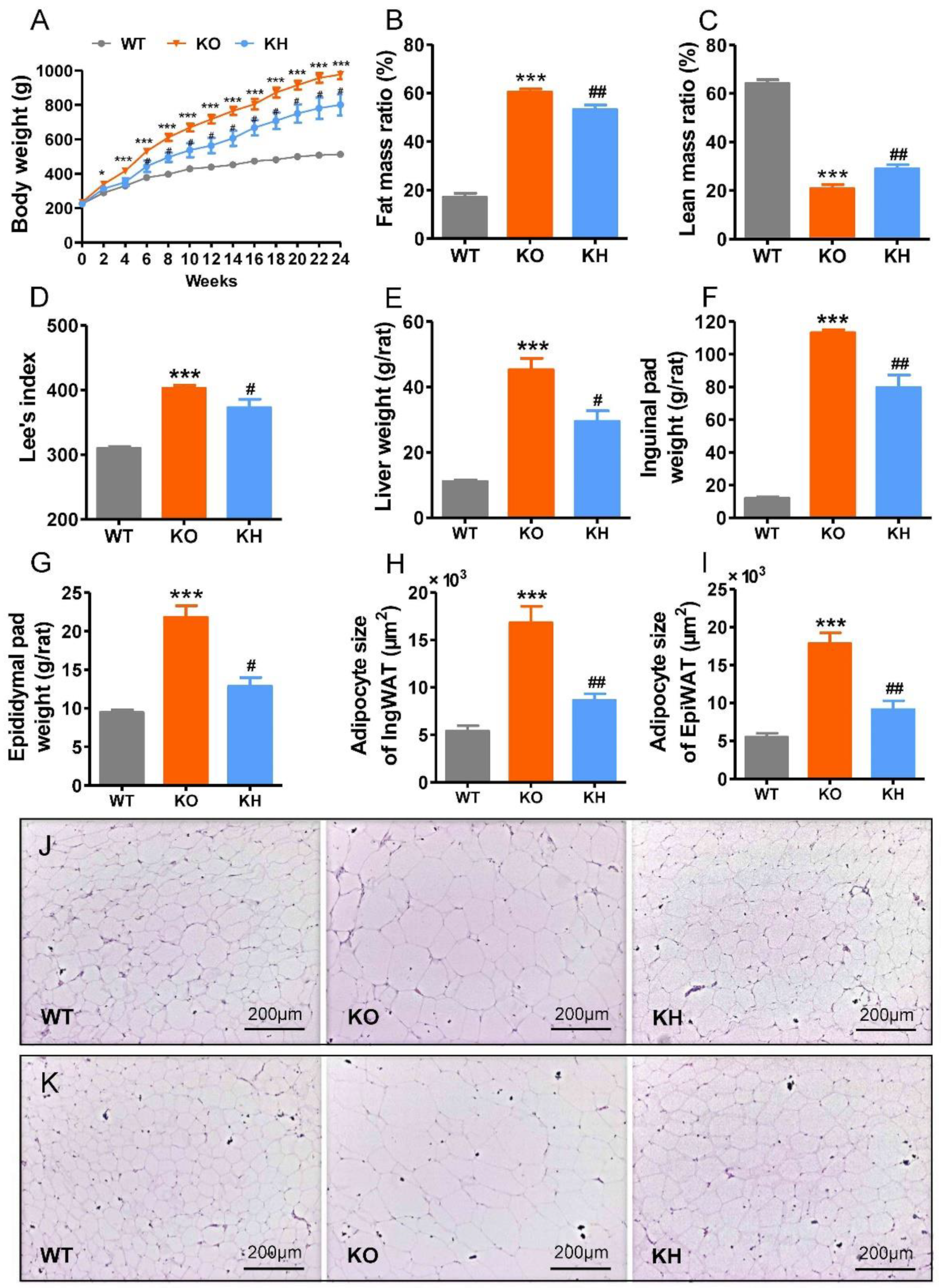
3.2. HTE Attenuated Phenotypes of Obesity in Lepr−/− Rats
The Lepr−/− rat is characterized by obesity and dyslipidemia. To evaluate the effect of HTE on obesity in Lepr−/− rats, we administered 700 mg HTE per kg body weight to rats for 24 weeks. As shown in Figure 1A, the Lepr−/− rats showed rapid weight gain compared to WT rats. After 6 weeks of intervention, the HTE group showed significantly lower body weights compared to the Lepr−/− control group (p < 0.05), and this preventive effect persisted until to the end of 24-week intervention. An analysis of body composition revealed a significant reduction of fat mass gain and an increase of lean mass loss in Lepr−/− rats following HTE intervention (Figure 1B,C). Lee’s index is an effective parameter in evaluating the obesity degree of rats. Compared to WT rats, the Lee’s index of Lepr−/− rats showed a significant increase. However, HTE supplementation obviously decreased the Lee’s index of Lepr−/− rats (Figure 1D). In addition, weights of liver and adipose tissues, including inguinal and epididymal fat, were remarkably heavier in the Lepr−/− group than that in the WT group. The weights of liver and adipose tissues were lower in the KH group when compared with the KO group (p < 0.05) (Figure 1E–G and Figure S1). H & E staining results showed that the sizes of the inguinal and epididymal adipocytes were reduced in the KH group as compared to the KO group (p < 0.05) (Figure 1H–K). We measured food intake of each group of rats to determine if HTE affected energy intake in Lepr−/− rats. The results indicated that there were no significant differences in food intake between the Lepr−/− and KH groups (Figure S2). However, the food intake in Lepr−/− rats was elevated significantly by 55.29% in comparison with WT rats (p < 0.001).
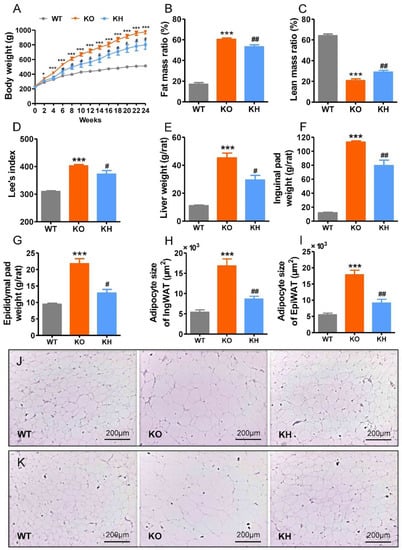
Figure 1.
HTE attenuated phenotypes of obesity in Lepr−/− rats. HTE, Huangshan Maofeng green tea extracts; WT, wild type littermates; KO, leptin receptor knockout rats; KH, leptin receptor knockout rats with HTE administration. (A) Body weight; (B) fat mass ratio; (C) lean mass ratio; (D) Lee’s index; (E) liver weight; (F) inguinal fat weight; (G) epididymal fat weight; (H) adipocyte size of inguinal fat; (I) adipocyte size of epididymal fat; (J,K) Hematoxylin–eosin staining of the inguinal fat and epididymal fat (100 × magnification). * p < 0.05, *** p < 0.001, compared to WT group; # p < 0.05, ## p < 0.01 versus KO group (n = 4–6, means ± SEM).
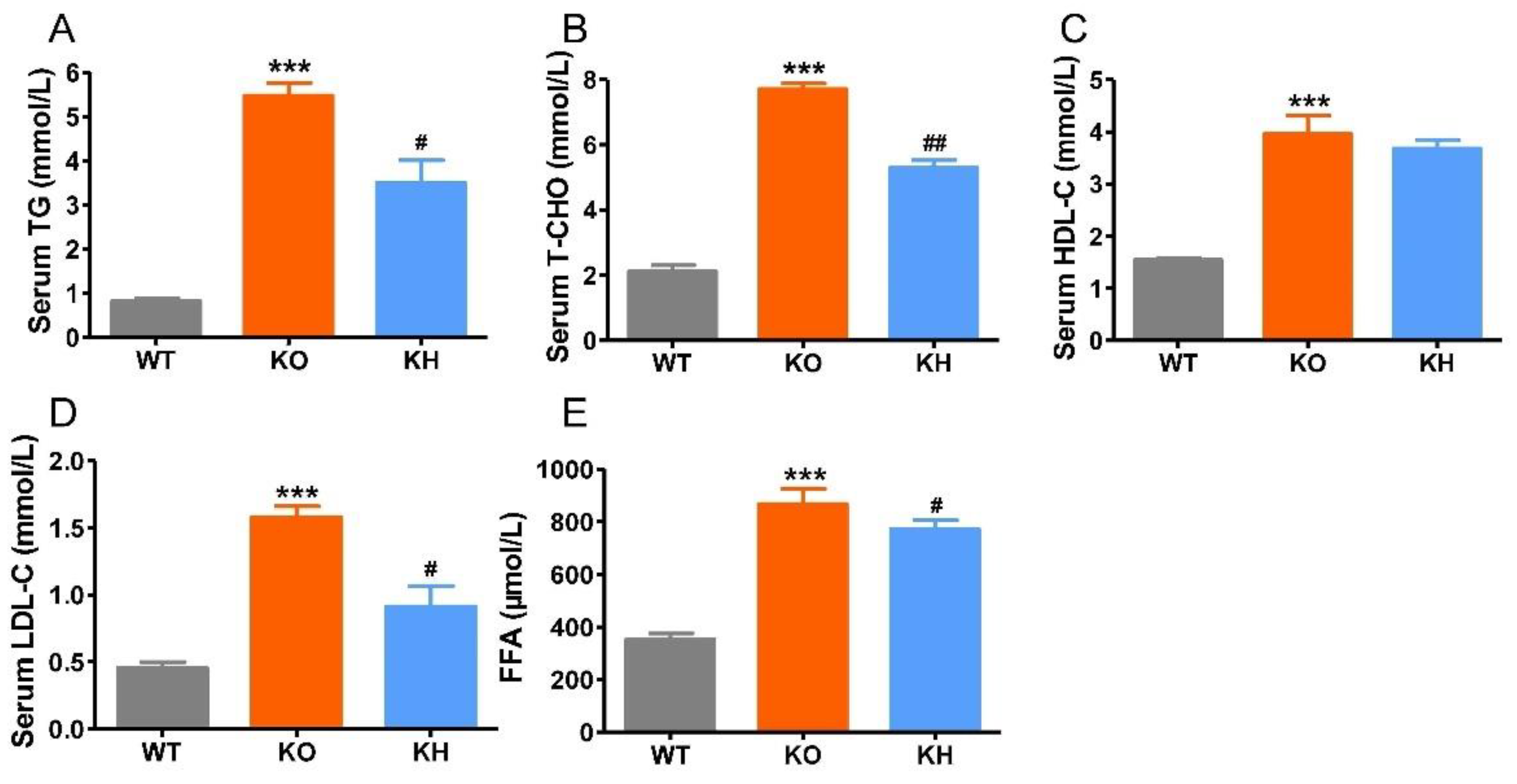
3.3. HTE Improved Dyslipidemia in Lepr−/− Rats
The measurement results for serum biochemical parameters including TG, T-CHO, LDL-C, HDL-C, and FFA levels are presented in Figure 2. The results showed that serum TG, TCHO, LDL-C, HDL-C, and FFA levels in the KO group showed all significant increase when compared with those in the WT group (p < 0.001). Supplementation with HTE significantly decreased serum TG, TC, LDL-C, and FFA levels (p < 0.05), although the levels of serum HDL-C did not appear to be altered by supplementation of HTE. The results suggested that HTE could improve dyslipidemia in Lepr−/− rats.
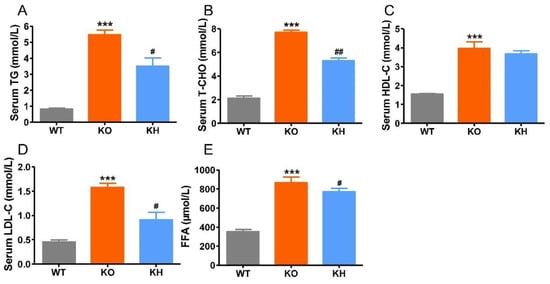
Figure 2.
The serum lipid panel of each group of rats. (A) Total cholesterol; (B) triglyceride; (C) high-density lipoprotein cholesterol; (D) low-density lipoprotein cholesterol; (E) free fatty acids. *** p < 0.001 versus WT group; # p < 0.05, ## p < 0.01 versus KO group (n = 5, means ± SEM).
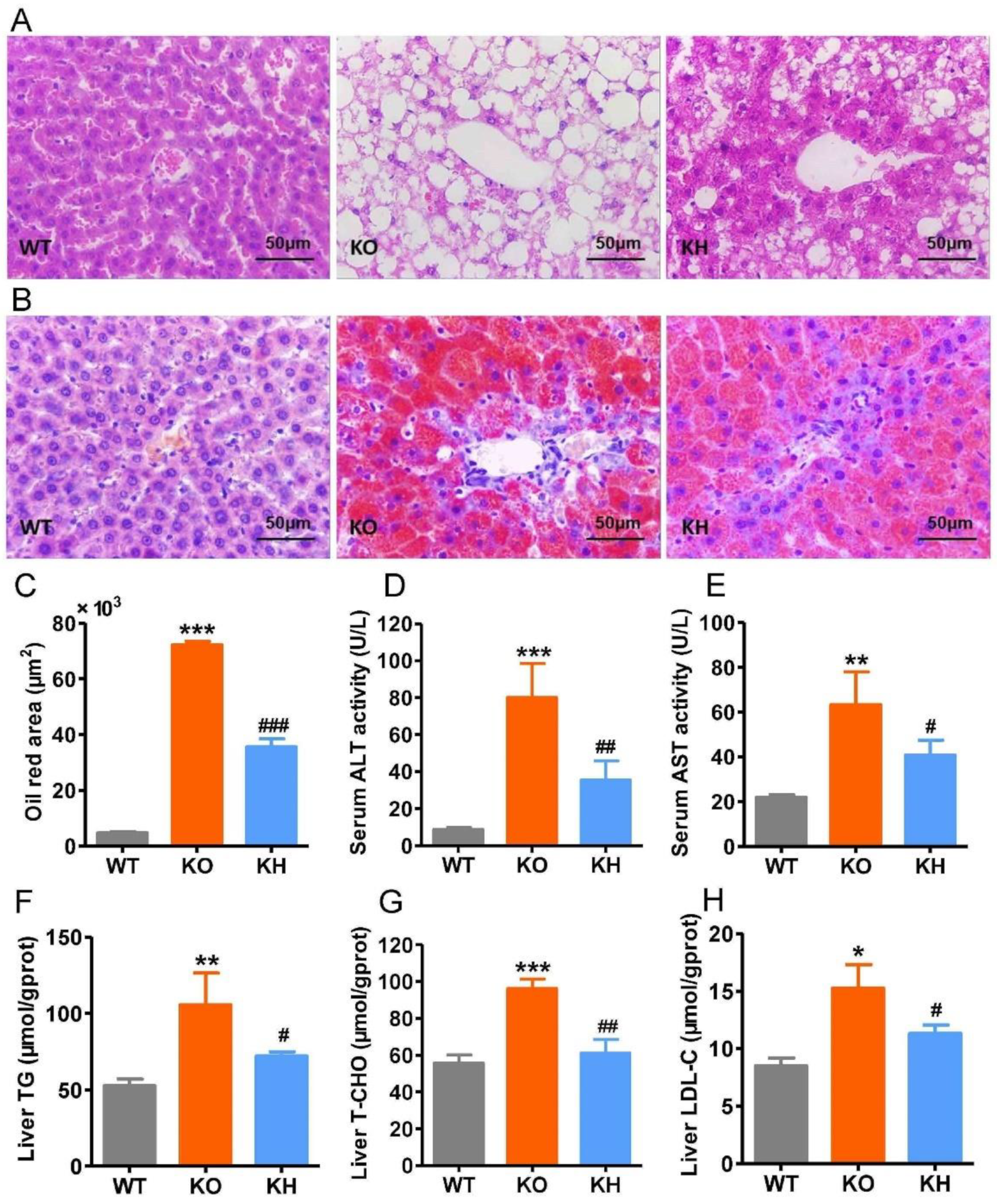
3.4. HTE Ameliorated Hepatic Steatosis in Lepr−/− Rats
Obesity is frequently associated with hepatic steatosis. As shown in Figure 3A, H & E staining showed that liver tissue from the WT group exhibited larger polygonal cells with clear round nuclei and less lipid accumulation, whereas liver tissue from the Lepr−/− group showed diffuse hepatic fatty infiltration. However, the hepatic steatosis in Lepr−/− rats was dramatically reduced after HTE intervention (the histopathology of the livers with lower magnification; see Figure S3). Oil red staining showed that the accumulation of higher levels of lipids in the liver of Lepr−/− rats was significantly reduced after administration of HTE (Figure 3B,C). The serum ALT and AST activities, used as the biochemical markers of hepatic injury, are shown in Figure 3D,E, respectively. The KO group showed remarkably elevated serum ALT and AST activities than the WT group (p < 0.001). However, HTE supplementation obviously reduced serum ALT and AST activities by 55.77% and 35.64% (p < 0.05), respectively. Moreover, the levels of liver TG, T-CHO, and LDL-C in the KH group were reduced when compared with those in the KO group (p < 0.05) (Figure 3F–H). Results all indicated that HTE alleviated hepatic steatosis in Lepr−/− rats.
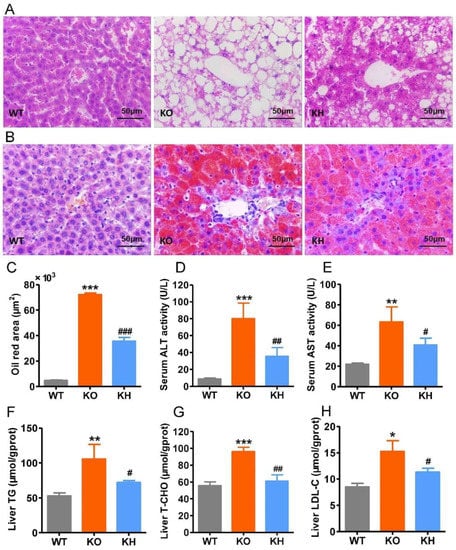
Figure 3.
HTE ameliorated hepatic steatosis in Lepr−/− rats. (A,B) Histological examination of liver structure with H & E staining and ORO staining; (C) oil red area of the liver tissue section; (D,E) the activity of serum ALT and AST, respectively; (F) triglyceride levels in liver; (G) total cholesterol levels in liver; (H) low-density lipoprotein cholesterol levels in liver. * p < 0.05, ** p < 0.01, *** p < 0.001, compared to WT group; # p < 0.05, ## p < 0.01, ### p < 0.001 versus KO group (n = 4–6, means ± SEM).
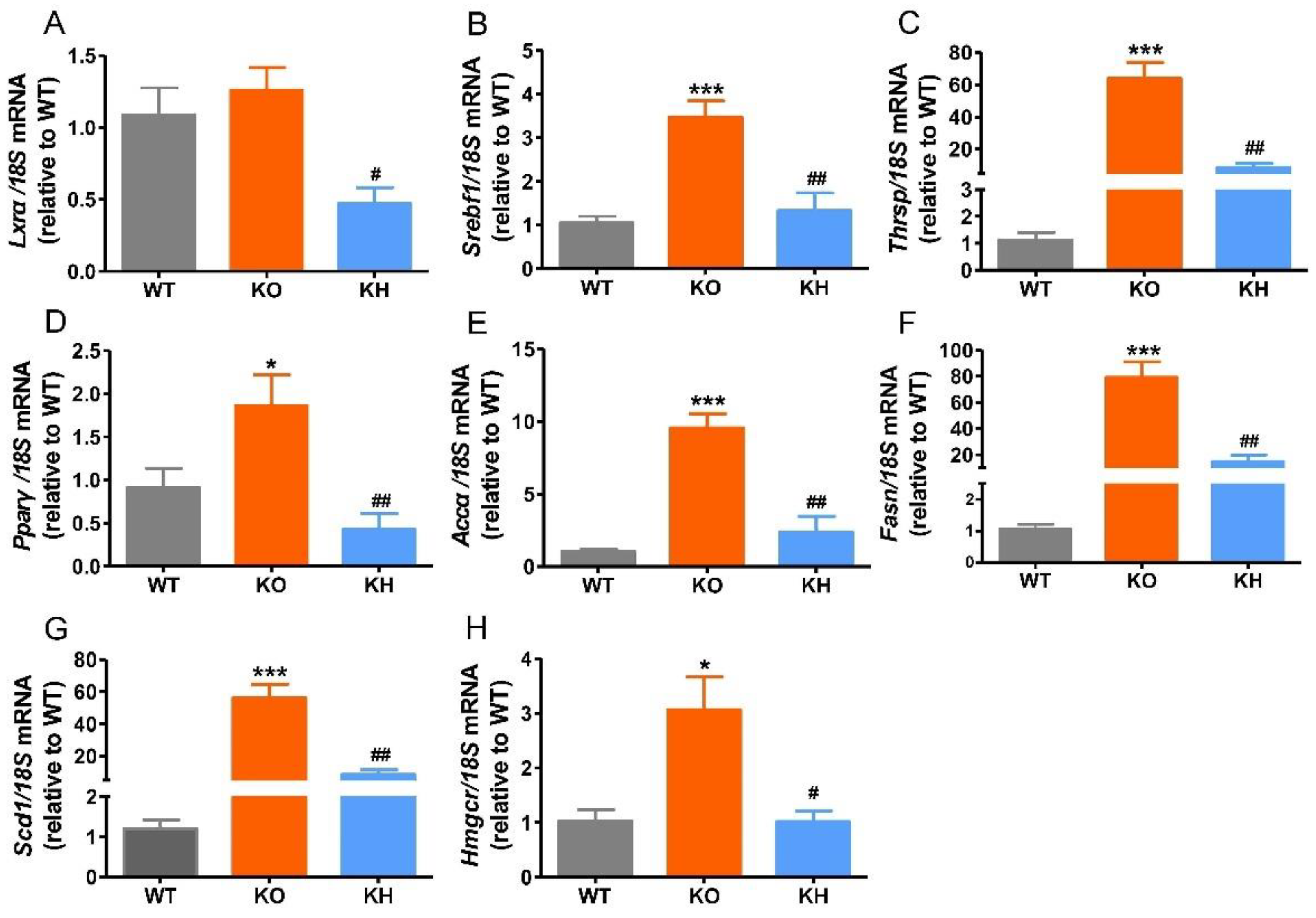
3.5. HTE Reduced the Expressions of Lipogenesis Related Genes in Liver of Lepr−/− Rats
Previous studies have shown that dysregulation of hepatic lipogenesis genes is associated with obesity [47]. Therefore, the expression levels of lipogenesis related genes were evaluated to investigate the regulating effect of HTE on lipid metabolism in Lepr−/− rats (Figure 4). Our results showed that the expression levels of Srebf1, Thrsp, Pparγ, Accα, Fasn, Scd1, and Hmgcr remarkably increased in the KO group compared to the WT group. However, HTE supplementation significantly reduced the expression levels of Lxrα, Srebf1, Thrsp, Pparγ, Accα, Fasn, Scd1, and Hmgcr (p < 0.05), which is consistent with lower levels of serum FFA, TG, and TC in the KH group.
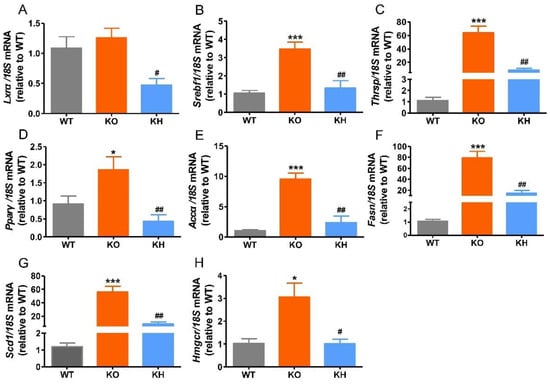
Figure 4.
HTE reduced the expressions of hepatic lipogenesis related genes in Lepr−/− rats. (A) Lxrα; (B) Srebf1; (C) Thrsp; (D) Pparγ; (E) Accα; (F) Fasn; (G) Scd1; (H) Hmgcr. * p < 0.05, *** p < 0.001, compared to WT group; # p < 0.05, ## p < 0.01 versus KO group (n = 5, means ± SEM).
3.6. HTE Improved Hepatic Lipid Profiles by Lipidomics Analysis
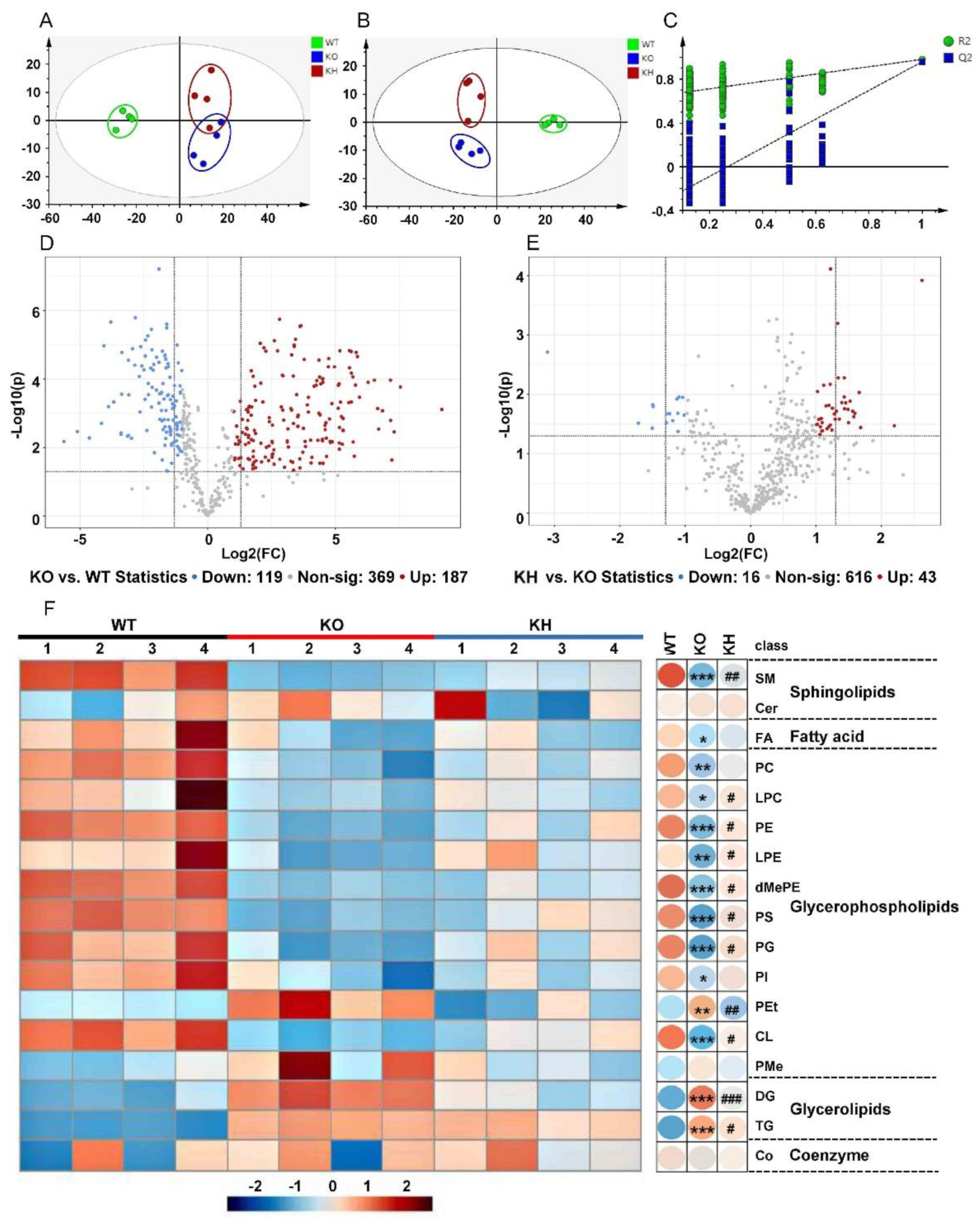
The liver is an important organ for nutrient metabolism and lipogenesis. To understand the preventing obesity effects of HTE in Lepr−/− rats, we further conducted hepatic lipidomics to analyze the liver lipid profiles. The typical total ion current chromatograms of liver samples were analyzed with the UHPLC-Orbitrap-MS/MS system, which yielded 675 metabolite ion features (Figure S4). Based on the lipid metabolites, a principal component analysis (PCA) was performed to visualize the data. Results showed that the lipid profiles from liver of the WT, KO, and KH group were clearly separated (Figure 5A), indicating a significant difference in lipid profiles between the three group samples. We then used partial least squares discrimination analysis (PLS-DA) to analyze potential discrimination among sample groups. The result also revealed that the three group samples were clearly separated from each other (Figure 5B). Furthermore, the permutation tests for PLS-DA model validation resulted in an R2 and Q2 of 0.645 and –0.35, which indicated that the models had been established successfully without being overfit (Figure 5C). The plot of volcanoes was used to identify lipid compounds responsible for discrepancies. Using the standard of FC ≥ 2 or ≤ 0.5 and p ≤ 0.05, a total of 306 significantly different lipid species were identified for the KO group versus the WT group (Figure 5D). Moreover, 59 significantly different lipid species were identified when the KH group and the KO group were compared (Figure 5E).
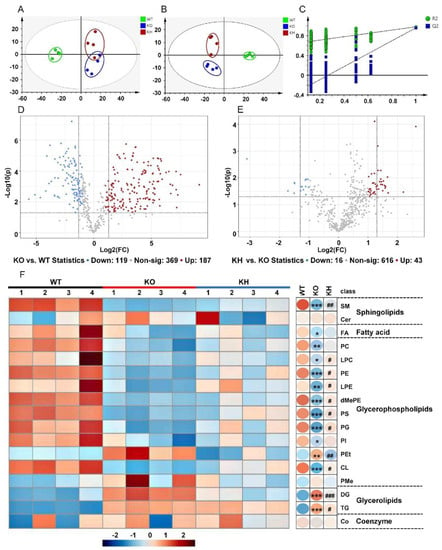
Figure 5.
HTE altered lipid classes in liver of Lepr−/− rats. (A) PCA score plots for the hepatic lipids (R2X = 0.907; Q2 = 0.518); (B) PLS–DA score for the hepatic lipids (R2X = 0.864; R2Y = 0.994; Q2 = 0.905); (C) PLS–DA model validation (R2 = 0.645; Q2 = −0.35); (D) Volcano plot displaying differential lipid classes between KO and WT; (E) Differential lipid classes between KH and KO. In the volcano plot, a number of significantly different lipid species were filtered out based on the criteria of FC ≥ 2 or ≤ 0.5 and p ≤ 0.05. Red (up) and blue (down) dots represent significant differentials of lipid species, whereas gray dots represent no significant differences of lipid species (n = 4). (F) Heat map representing lipid class levels. Values that were higher and lower than the mean will be shown in red and blue boxes, respectively. * p < 0.05, ** p < 0.01, *** p < 0.001, compared to WT group; # p < 0.05, ## p < 0.01, ### p < 0.001 versus KO group (n = 4, means ± SEM).
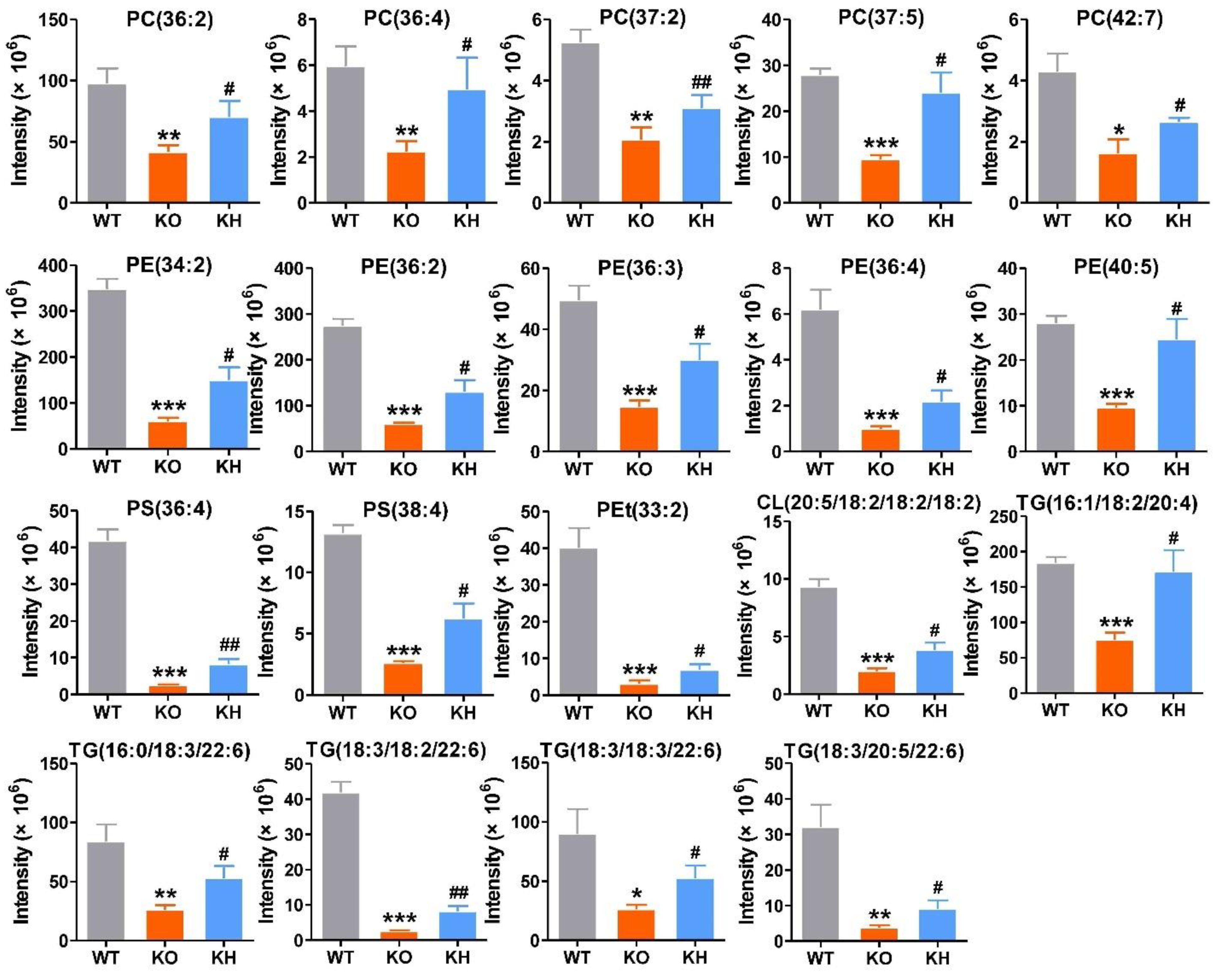
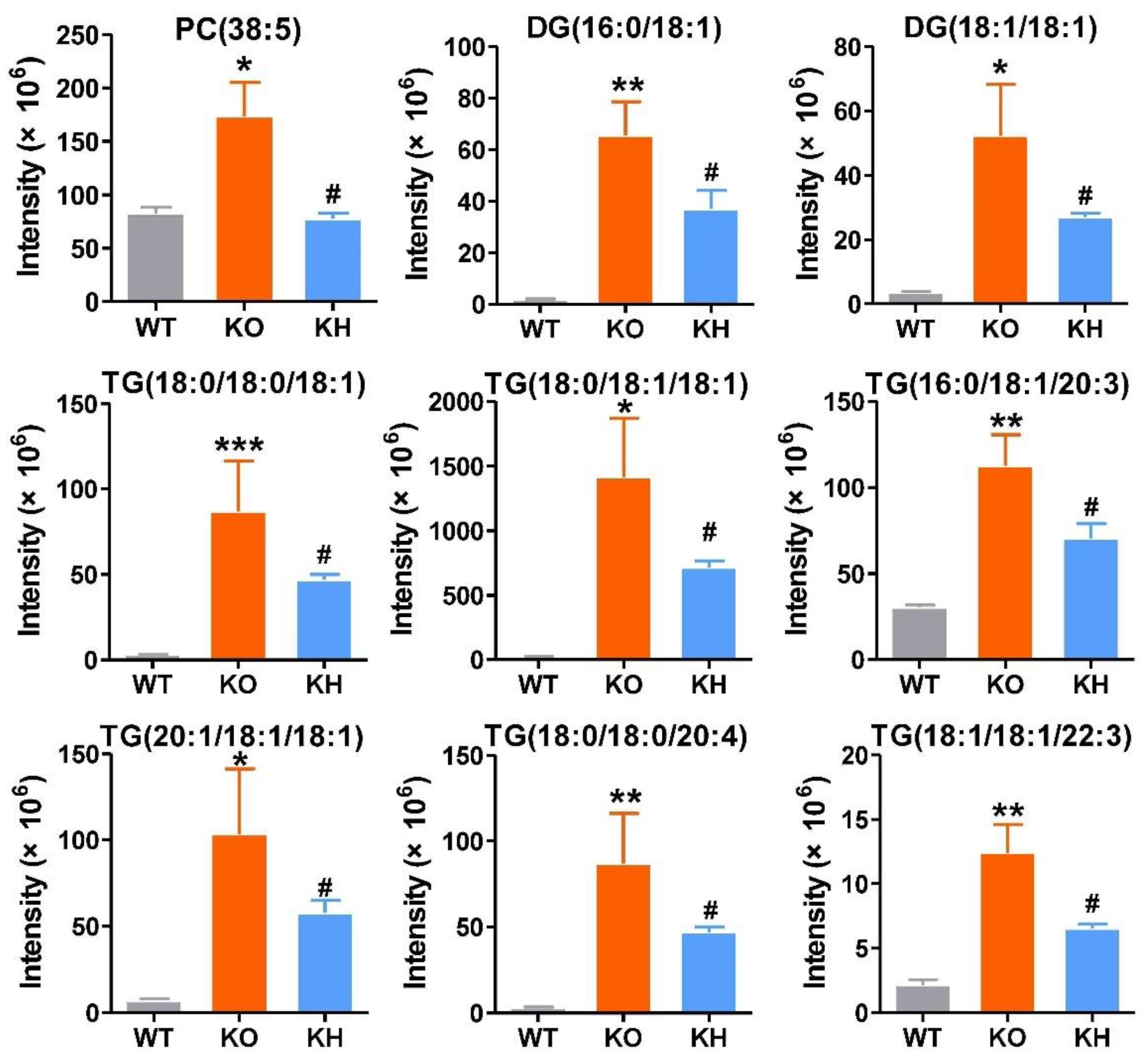
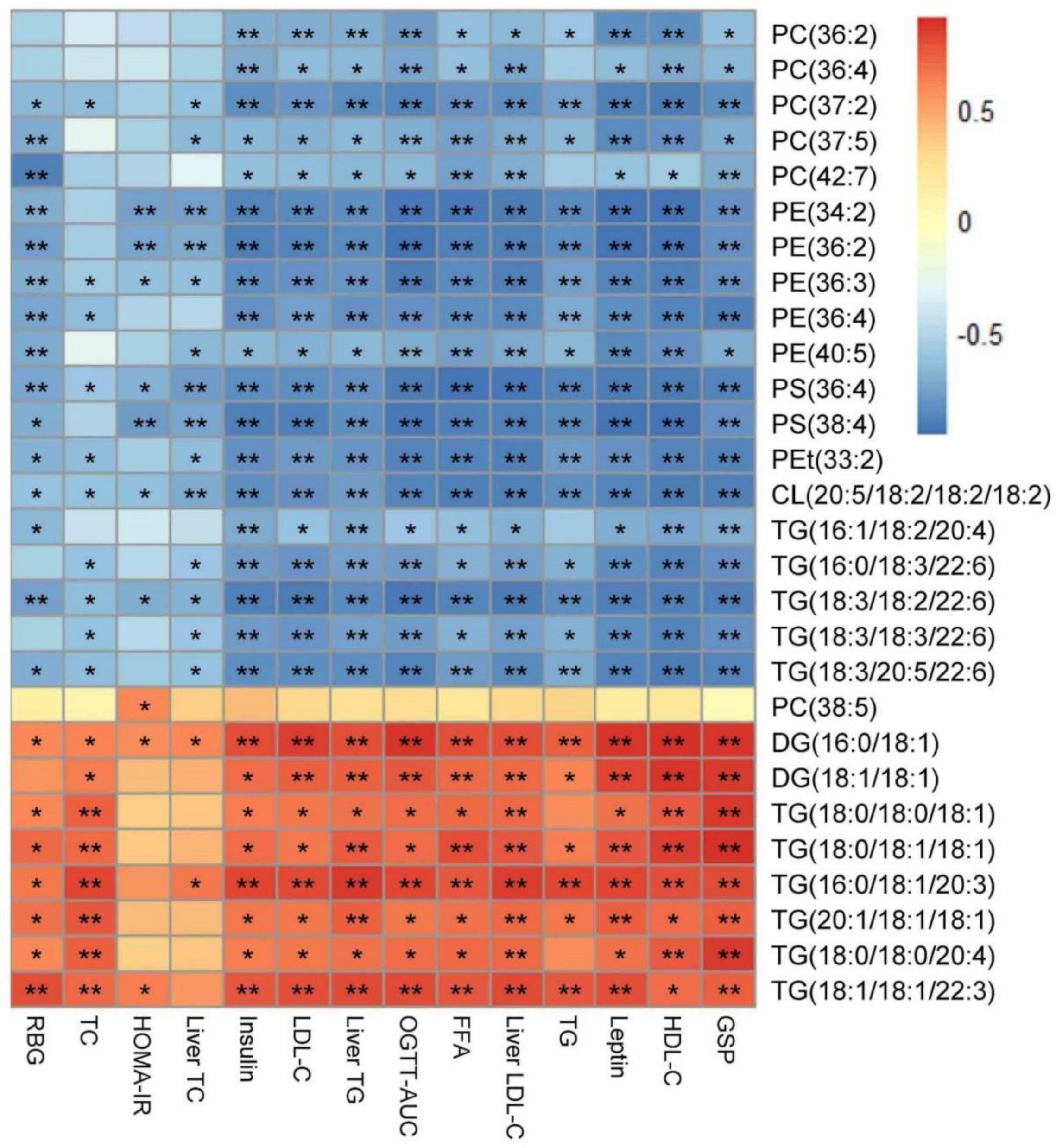
A heatmap was generated to show the changes of the lipid classes in the liver of rats. The results showed that the level of diglycerides (DGs), triglycerides (TGs), and phosphatidylethanol (PEts) remarkably increased in the KO group than the WT group. The following lipid classes, such as phosphatidylcholines (PCs), lyso-phosphatidylcholines (LPCs), phosphatidylethanolamines (PEs), lyso-phosphatidylethanolamines (LPEs), dimethyl-phosphatidylethanolamines (dMePEs), phosphatidylserines (PSs), phosphatidylglycerols (PGs), phosphatidylinositols (PIs), cardiolipins (CLs) in glycerophospholipids, and sphingomyelins (SMs) in sphingolipids were dramatically decreased in the KO group when compared to the WT group (Figure 5F). However, after HTE intervention, the lipid classes of Lepr−/− rats were reversed to the level of WT rats. The lipid metabolites significantly affected by HTE are shown in Figure 6 and Figure 7. The results showed that the 19 lipid classes, including 14 glycerophospholipid classes (PC (36: 2), PC (36: 4), PC (37: 2), PC (37: 5), PC (42: 7), PE (34: 2), PE (36: 2), PE (36: 3), PE (36: 4), PE (40: 5), PS (36: 4), PS (38: 4), Pet (33: 2), CL (20: 5/18: 2/18: 2/18: 2)) and 5 glycerolipids (TG (16: 1/18: 2/20: 4), TG (16: 0/18: 3/22: 6), TG (18: 3/18: 2/22: 6), TG (18: 3/18: 3/22: 6), TG (18: 3/20: 5/22: 6)), were significantly increased, while the 9 lipid classes, including 1 glycerophospholipid class (PC(38: 5)) and 8 glycerolipids (DG (16: 0/18: 1), DG (18: 1/18: 1), TG (18: 0/18: 0/18: 1), TG (18: 0/18: 1/18: 1), TG (16: 0/18: 1/20: 3), TG (21: 1/18: 1/18: 1), TG (18: 0/18: 0/20: 4), TG (18: 1/18: 1/22: 3)), were significantly decreased in Lepr−/− rats after HTE supplementation. Furthermore, according to the correlation analysis, the 28 lipid species were significantly correlated with the phenotypes of obesity, including serum TG, serum TC, serum LDL-C, liver TG, liver TC, liver LDL-C, etc. Additionally, 28 differential metabolites were identified among the three groups based on p values. Among these 28 lipid species, the level of PE (36:3), PS (36:4), CL (20:5/18:2/18:2/18:2), and TG (18:3/18:2/22:6) were strongly negatively correlated with obesity related disorder, whereas the level of DG (16:0/18:1) were strongly positively correlated with obesity related indexes (Figure 8).
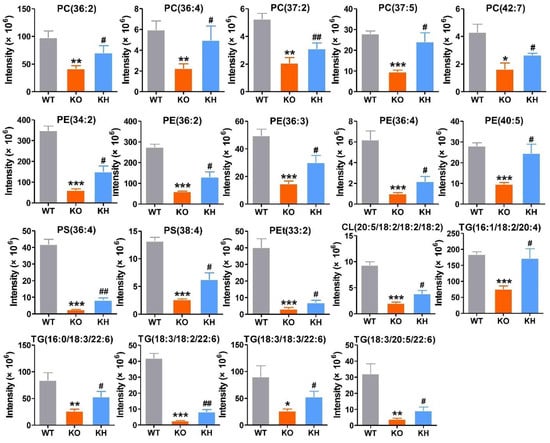
Figure 6.
Nineteen lipid species were significant reversibly increased by HTE in liver of Lepr−/− rats. Values are the mean ± SEM (n = 4). * p < 0.05, ** p < 0.01, *** p < 0.001, compared to WT group; # p < 0.05, ## p < 0.01 versus KO group.
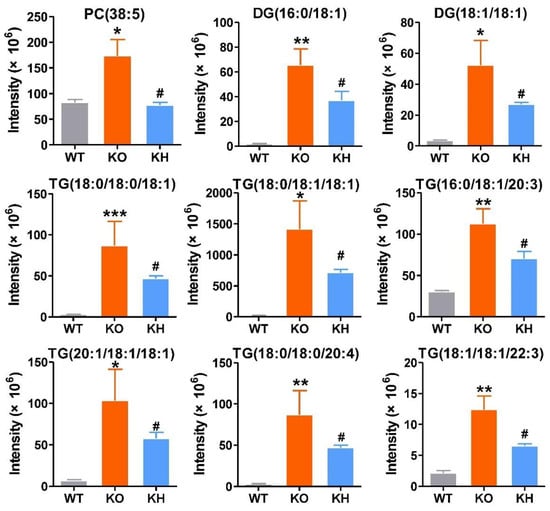
Figure 7.
Nine lipid species were remarkable reversibly decreased by HTE in liver of Lepr rats. Values are the mean ± SEM (n = 4). * p < 0.05, ** p < 0.01, *** p < 0.001, compared to WT group; # p < 0.05 versus KO group.
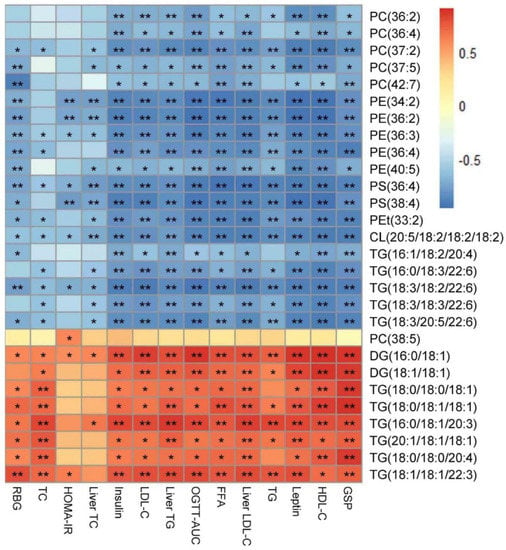
Figure 8.
Spearman’s correlation between lipid species and obesity related indexes. Significant correlations are indicated by * p < 0.05, ** p < 0.01. RBG, random blood glucose; HOMA−IR, homeostatic model assessment of insulin resistance; OGTT-AUC, area under curve of oral glucose tolerance test; GSP, glycated serum protein level. The RBG, HOMA−IR, OGTT−AUC, GSP, insulin, and leptin levels are showed in Figure S5 in the Supplementary Materials.
3.7. HTE Increased Gut Microbiota Diversity in Lepr−/− Rats
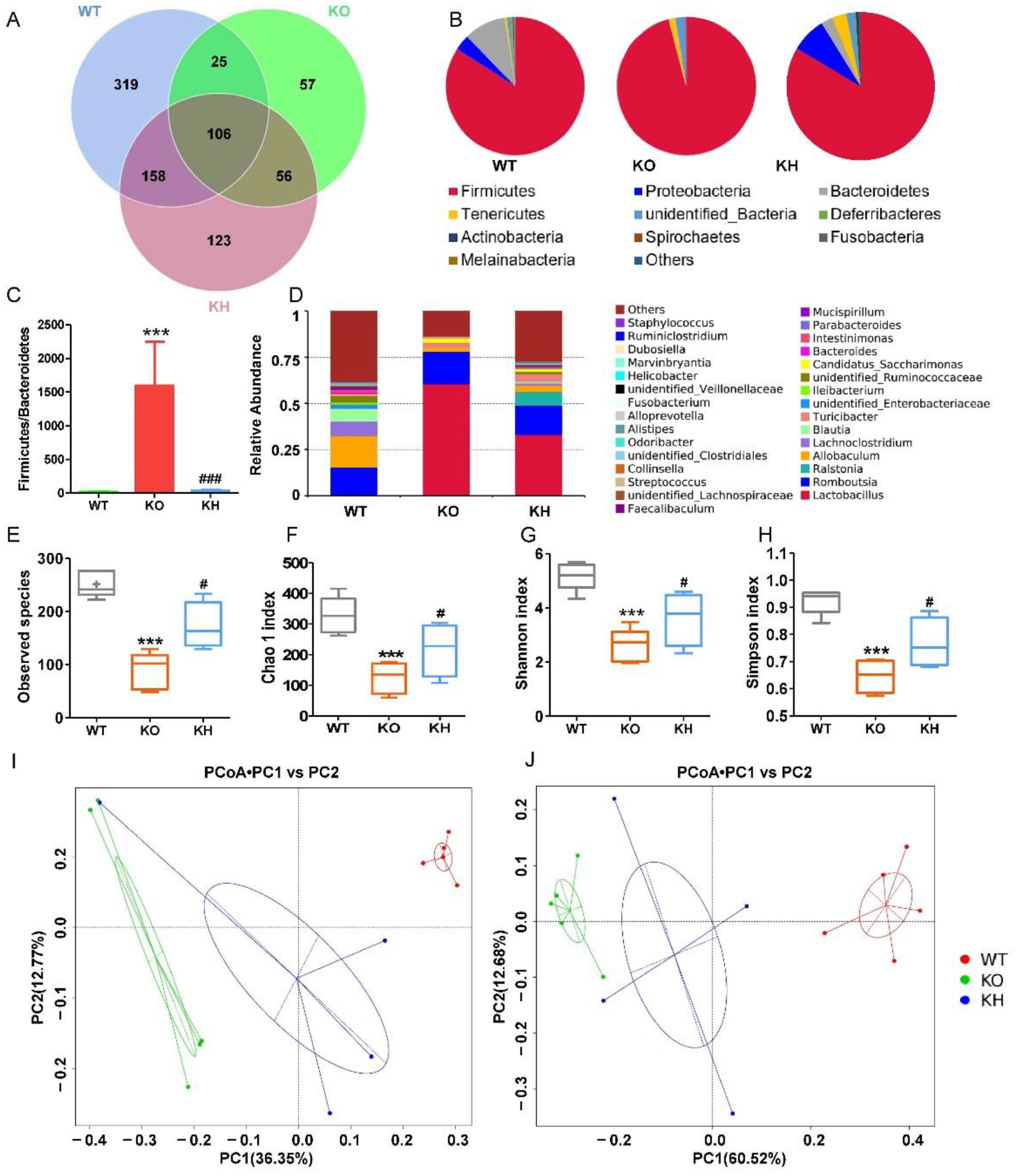
It has been shown that diet mediating biological function is closely related to gut microbiota modulation [48]. Therefore, we examined the effects of HTE on gut microbiota homeostasis using 16S rRNA sequencing. A total of 844 bacterial OTUs were obtained, and 608 OTUs were found in the WT group, whereas 244 OTUs were identified in the Lepr−/− group. After administration with HTE, the number of OTUs in the KH group increased to 443 (Figure 9A). At phylum level, the abundance of Firmicutes was significantly increased in the KO group, while the abundance of Proteobacteria, Bacteroidetes, Deferribacteres, Actinobacteria, Fusobacteria, and Melainabacteria were remarkably reduced in the KO group as compared to the WT group (Figure 9B). After administration with HTE, the microbiota composition at the phylum level in the KH group was revised to the WT group (Figure 9B). As shown in Figure 9C, by comparing the Lepr−/− group to the WT group, we found that the relative abundance of Bacteroidetes was decreased significantly, while Firmicutes were increased, which resulted in a higher F/B ratio in the KO group. After HTE intervention, the F/B ratio in the KO group was dramatically reduced. We further analyzed the microbiota composition at the genus level and found that the richness of gut microbiota in the KO group was reduced when compared to the WT group and KH group (Figure 9D). To investigate the effect of HTE on α–diversity of gut microbiota in Lepr−/− rats, including the observed species index, the Chao 1 index, and the Shannon and Simpson indexes, we found that the KH group showed significant increases in these indexes when compared with the KO group (Figure 9E–H). According to the principal coordinates analysis (PCoA) based on the unweighted and weighted UniFrac, three groups of rats had significantly different gut microbiota compositions and structures (Figure 9I,J).
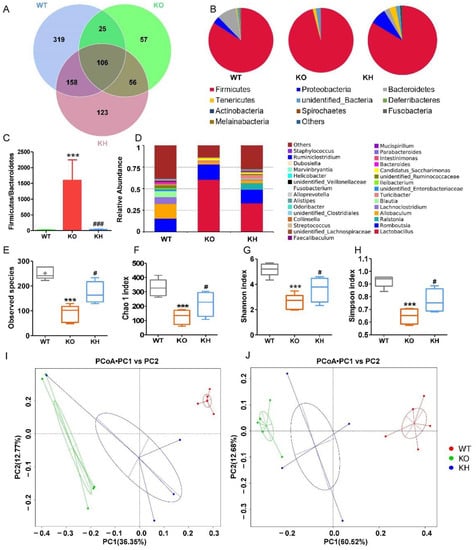
Figure 9.
HTE increased gut microbiota diversity in Lepr−/− rats. (A) Venn diagram of gut microbiota among the various groups; (B) the abundance of the top 10 phylum among the various groups; (C) the ratio of relative abundance of Firmicutes to Bacteroidetes; (D) the abundance of the top 30 genus among the various groups; (E–H) assessment of the alpha diversity of gut microbiota based on different indices; (I,J) principal coordinates analysis of gut microbiota based on unweighted UniFrac and weighted UniFrac. *** p < 0.001 versus WT group; # p < 0.05, ### p < 0.001, versus KO group (n = 4–5, means ± SEM).
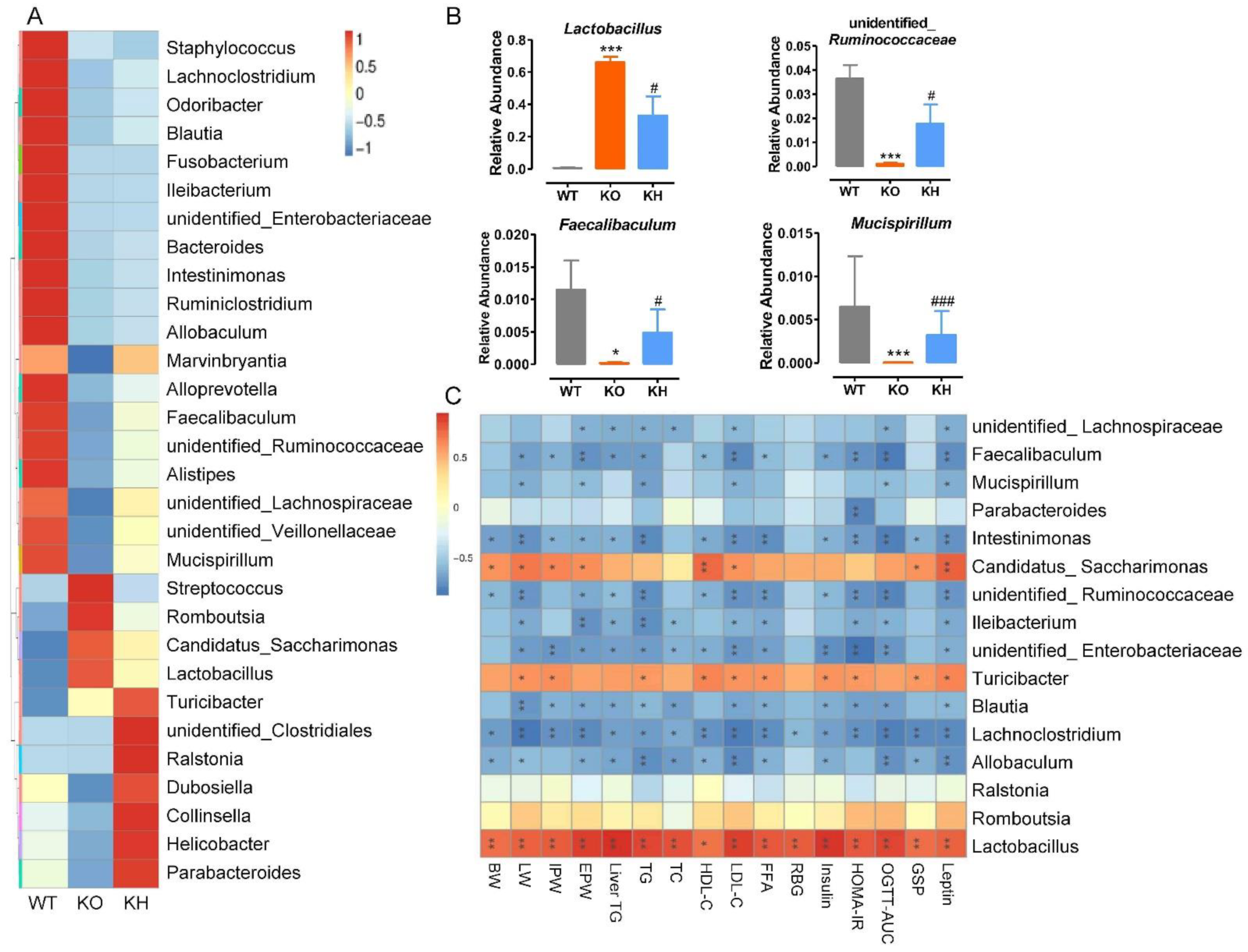
3.8. HTE Altered the Gut Microbiota Composition in Lepr−/− Rats
First, we analyzed the abundance of top 30 genera in gut microbiota among different groups of rats, and the results revealed that the microbiota composition of the Lepr−/− group was significantly different from that of the WT group (Figure 10A). The microbiota producing SCFAs, including Odoribacter, Blautia, Bacteroides, Intestinimonas, Faecalibaculum, unidentified_Ruminococcaceae, unidentified_Veillonellaceae, Turicibacter, and Parabacteroides, decreased and opportunistic pathogens (Streptococcus) increased in the Lepr−/− group compared to the WT group, which indicated that gut microbiota dysbiosis had occurred in the Lepr−/− group. Second, we ranked the microbiota according to the p values by comparing the Lepr−/− group with the KH group. At the genus level, compared with the WT group, the relative abundance of Lactobacillus was significantly higher, while the relative abundances of unidentified_Ruminococcaceae, Faecalibaculum, and Mucispirillum were dramatically reduced in the Lepr−/− group (p < 0.05) (Figure 10B). However, we found that HTE supplementation significantly reversed this balance to the WT group in the KH group (Figure 10B). In addition, a spearman correlation analysis was conducted to investigate the relationship between top 16 genera of gut microbiota and obesity complication-related parameters (Figure 10C). The correlation analysis showed that the abundance of Faecalibaculum, Intestinimonas, unidentified_Ruminococcaceae, Ileibacterium, unidentified_Enterobacteriaceae Blautia, Lachnoclostridium, and Allobaculum were significantly negatively correlated with obesity parameters, whereas the abundance of Lactobacillus, Turicibacter, and Candidatus_Saccharimonas were positively associated with obesity related indexes. Additionally, the abundance of unidentified_Lachnospiraceae and Mucispirillum was negatively associated with the serum TG, serum LDL-C, the AUC of OGTT, and leptin levels. The abundance of Parabacteroides was negatively associated with the HOMA-IR index. These results showed that HTE supplementation resulted in alterations in gut microbiota composition that were closely related to improving obesity complication in Lepr−/− rats. Furthermore, we determined the effects of HTE intervention on the SCFAs producing by gut microbiota in fecal of rats. The results showed that except for acetic acid, HTE supplementation significantly increased the levels of fecal propanoic acid, butyric acid, isobutyric acid, pentanoic acid, and isopentanoic acid in Lepr−/− rats (Figure S6).
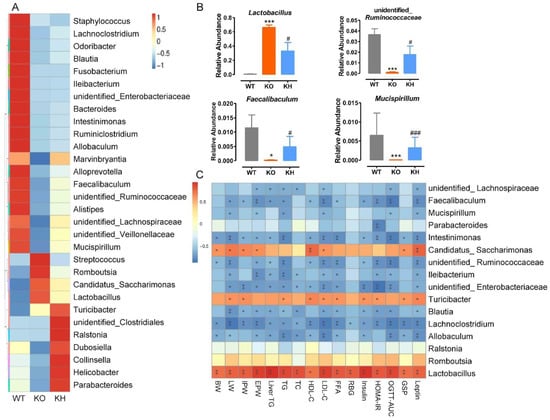
Figure 10.
HTE altered the gut microbiota composition in Lepr−/− rats. (A) The heatmap of the top 30 genera among the various groups; (B) relative abundance of the gut microbiota at the genus level (p < 0.05); (C) heatmap of spearman’s correlation between microbiota and obesity related parameters, significant correlations are marked as * p < 0.05, ** p < 0.01. BW, body weight of rats; LW, liver weight; IPW, inguinal fat weight; EPW, epididymal fat weight. * p < 0.05, *** p < 0.001 versus WT group; # p < 0.05, ### p < 0.001 versus KO group (n = 4–5, means ± SEM).
4. Discussion
Obesity complications are cluster disorders, including obese, dyslipidemia, diabetes, and fatty liver. There is an increasing body of evidence which suggests that dietary supplementation with tea and tea extracts may be a practical strategy for preventing or treating obesity complication in humans and animals [21]. The majority data from mice studies reported that green tea has health benefits on obesity prevention, and its polyphenols are the active ingredients believed to be responsible for these health benefits [49,50]. HMGT is one of the famous green teas produced and consumed for a long history in Anhui, China. However, the effect on obesity prevention of HMGT has not been investigated. The present study systematically investigated the obesity prevention effect of long-term supplement of water extracts of HMGT using Lepr−/− rats model. Our chemical analysis data showed that the water extracts of HMGT (HTE) was characterized as a polyphenol-enriched fraction containing high concentration of EGCG (178.14 ± 2.37% mg/g) as the major catechin, followed by polysaccharide (153.89 ± 1.36% mg/g), caffeine (106.92 ± 0.93% mg/g), and theanine (30.51 ± 1.43 mg/g). EGCG is one of the richest bioactive polyphenol components in tea and has been reported to have fat-reduction and weight-loss effects. Huang et al. reported that EGCG alleviated obesity and fatty liver development by reducing lipid and bile acid absorption in mice [51]. Choi et al. reported that EGCG reduces obesity by regulating Beclin1-dependent autophagy in white adipose tissues of mice [52]. Furthermore, studies have revealed that tea polysaccharides can reduce the risk of type 2 diabetes, obesity, as well as obesity-related diseases by modulating gut microbiota and metabolism [25,53]. Additionally, caffeine has been shown to be one of the most effective bioactive constituents in tea for reducing fat deposits and weight loss [54,55]. Here, we speculated that EGCG, polysaccharides, and caffeine from HTE all can contribute to prevention obesity complication in Lepr−/− rats. Studies have shown that the health benefits of whole tea extracts are usually superior to those of single component, which may be a result of the synergistic effects of the various functional components found in tea [12,56]. Therefore, the synergistic effects and mechanisms of combination of multiple functional components in tea against obesity complication need to be further investigated in the future. Many previous studies have demonstrated that green tea supplement did not significantly affect lipid metabolism in wild type rats [57,58,59]. Therefore, a WT rat with HTE intervention group was not included in present study. Our results demonstrated that dietary supplement of HTE (700 mg/kg BW) efficiently prevented obesity related disorders, including overweight, hyperlipidemia, hepatic steatosis, and excessive adipose tissue accumulation in Lepr−/− rats. The dose used in the present study (700 mg/kg BW) is equivalent to 15 g daily tea consumption for a 70 kg human, and this amount is reasonable for regular tea consumers on a daily basis [60].
Dyslipidemia is a characteristic of obesity complication, which can result in insulin resistance of the liver and nerve endings, and damage to the islets [61]. Previous studies have reported that the green tea extract can obviously decrease body weight and levels of TC, TG, and LDL-C [58,62]. Our data further showed that HTE reversibly decreased the levels of serum TC, TG, LDL-C, and FFA, but did not reduce the levels of serum HDL-C in Lepr−/− rats model. Our previous study reported that supplementation of large yellow tea did not alter the concentration of HDL-C in db/db mice [12]. A recent paper found that instant dark tea induced the level of serum HDL-C in high-fat diet-fed rat [63]. The possible reason for difference between this result and our present data might be due to the different chemical profiles between HTE and instant dark tea.
The liver is a vital organ for the regulation of lipid metabolism. An excessive accumulation of lipid in the liver is a characteristic of obesity, which can result in liver injury, fibrosis, and cirrhosis. In our study, as compared to the Lepr−/− rat group, supplementation of HTE reduced hepatic lipid accumulation, and suppressed ALT and AST activities, alleviating liver injury in Lepr−/− rats. It has been reported that tea and its functional ingredients can lower lipid accumulation by suppressing lipogenesis and promoting catabolism of lipids in the liver of rodent model [21]. Thus, we measured the expression levels of lipogenesis related genes by real-time PCR. The results indicated that the mRNA expression levels of Lxrα, Srebf1, Thrsp, Pparγ, Accα, Fasn, Scd1, and Hmgcr were remarkably suppressed in the KH group when compared to the Lepr−/− rat group. SREBP1 is a transcription factor that contributes to the differentiation of adipocytes and lipogenesis by regulating lipogenesis related genes, such as Thrsp, Accα, Fasn, and Scd1 [64,65]. LXRα is a transcription factor that is critical for regulating hepatic lipid metabolism, which could significantly increase SREBP-1c expression directly, thereby promoting de novo lipogenesis in the liver [66,67]. Thrsp was demonstrated to be a lipogenic gene whose expression is controlled by LXRα and SREBP-1c [68,69]. In addition, PPARγ is a nuclear receptor regulating fatty acid synthesis and oxidation. Studies suggested that lipid catabolism was stimulated, and fatty acid synthesis was suppressed by inhibiting PPARγ expression or activity in the liver [47,70,71]. Accα, Fasn, Scd1, and Hmgcr are de novo lipogenesis related genes [72,73,74]. These results suggested that HTE could ameliorate fatty liver and protect the liver injury by suppressing the expression of wide-ranging lipogenesis genes in the liver of Lepr−/− rats.
This study further examined the lipid classes in the liver of Lepr−/− rats after HTE supplementation using mass spectrometry-based lipidomic approaches [36]. We found that the relative abundance of glycerides in the liver of Lepr−/− rats dramatically increases, whereas glycerophospholipids and sphingolipids significantly decrease when compared to WT rats. In a previous study, high fat diets resulted in an increase in liver glycerolipids (DGs and TGs), while a decrease in glycerophospholipids (PCs and PEs) and sphingolipids (SMs) resulted in abnormal lipid metabolism in mice [75]. Our results on leptin receptor knockout rats indicated that HTE supplementation induced obvious recovery of lipid classes similar to WT rats in liver of Lepr−/− rats.
Next, we screened the group specific lipid species. The 28 lipid species, including 13 glycerolipids and 15 glycerophospholipid classes, were significantly altered by HTE supplementation. Glycerolipids are the main lipids in the body as well as the major source of energy, including MGs, DGs, and TGs. Studies have shown that high DGs and TG levels in glycerolipids are indicative of fatty liver disease [76]. A high level of monounsaturated DGs in the liver is associated with insulin resistance and fatty liver [76,77]. In a study by Feng et al., the abundance of DGs in the livers of rats fed a high-fat diet increased, and the reduction of DGs was associated with the weight loss and lipid lowering effects of Tangeretin [78]. Our data indicated that the decreased level of hepatic DG (16:0/18:1) and DG (18:1/18:1) in Lepr−/− rats might play an important role in the anti-obesity effect of HTE. Additionally, studies had shown that TG species with lower carbon numbers and double-bond content have been linked to increased cardiovascular disease and type II diabetes, while species with higher carbon numbers and higher double-bond content are linked to a decreased risk [79,80,81]. Recent population-based epidemiological studies also demonstrated that the elevation of low-carbon and low-double-bond content TG species significantly increased the risk of type 2 diabetes [82]. Our lipidemic data found that HTE supplementation exhibited anti-dyslipidemia effects by increasing the level of TG (16: 1/18: 2/20: 4), TG (16: 0/18: 3/22: 6), TG (18: 3/18: 2/22: 6), TG (18: 3/18: 3/22: 6), and TG (18: 3/20: 5/22: 6), and decreasing the level of TG (18: 0/18: 0/18: 1), TG (18: 0/18: 1/18: 1), TG (16: 0/18: 1/20: 3), TG (21: 1/18: 1/18: 1), TG (18: 0/18: 0/20: 4), and TG (18: 1/18: 1/22: 3) in the liver of Lepr−/− rats.
Glycerophospholipids are important cellular membrane components that regulate membrane function, including fluidity and homeostasis [83,84]. According to a previous study, defective PC biosynthesis leads to decreased VLDL synthesis and secretion, promoting NAFLD development [85]. Liu et al. reported that PCs were significantly reduced in nonalcoholic fatty livers induced by a western diet but increased significantly after highland barley β-glucan intervention [86]. Additionally, it was reported that an increase in hepatic steatosis was associated with an imbalance in the metabolism of PEs as well as the alteration in PEs content [87]. In the present study, HTE supplementation recovered the reduction of five PCs (PC (36: 2), PC (36: 4), PC (37: 2), PC (37: 5), PC (42: 7)) and 5 PEs (PE (34: 2), PE (36: 2), PE (36: 3), PE (36: 4), PE (40: 5)) in the liver of Lepr−/− rats. PSs are multifunctional bioactive lipids and are essential to maintaining healthy nerve cell membranes and myelin [88]. CLs form the inner mitochondrial membrane, and play an important role in maintaining the stability and activity of mitochondrial proteins [89]. HTE supplementation reversed the reduction of two PSs (PS (36: 4), PS (38: 4)) and one CL (CL (20: 5/18: 2/18: 2/18: 2)) in liver of Lepr−/− rats. In summary, our lipidemic data suggested that HTE supplement could restore lipid homeostasis by reducing glycerolipid levels and recovering glycerophospholipid levels in the liver of Lepr−/− rats. However, the mechanisms of HTE regulating fatty-acyl-chain lipids composition of TGs class and glycerophospholipids metabolic homeostasis are needed to be investigated in the future.
Growing evidences suggest that gut microbiota dysbiosis contributes to obesity and multiple metabolic complications, and obese individuals often have a lower gut microbiota diversity than that of lean individuals [48,90,91]. In our study, along with the obesity prevention by HTE supplementation, we observed an obviously raised diversity of the gut microbiota in the KH group, which corresponds to previous research that tea could remarkably increase gut microbiota diversity [92]. It has been reported that the ratio of Firmicutes to Bacteroidetes (F/B) is positively correlated with obesity [93]. A greater abundance of Firmicutes facilitates energy harvesting and promotes obesity [48]. Chen et al. previously reported that Fuzhuan brick tea significantly decreased the ratio of Firmicutes to Bacteroidetes, which helped to reduce obesity in mice [94]. Our current results showed that the ratio of Firmicutes to Bacteroidetes (F/B) in Lepr−/− rats was dramatically increased when compared to WT rats, whereas it was significantly decreased by HTE supplementation, which may also explain the improvement of HTE on obesity. To analyze the specific cluster of microbiotas with significant alteration by HTE supplementation, we found that SCFA-producing microbiota, such as unidentified_Ruminococcaceae and Faecalibaculum, increased in the KH group. It has been reported that Ruminococcaceae is a major butyrate producer, and its levels are dramatically reduced in patients with inflammatory bowel disease [95]. Wang et al. found that colitis was ameliorated by increasing Ruminococcaceae growth, which increased butyrate production [96]. Several papers reported that butyrate could prevent and treat obesity and obesity-related diseases [97,98]. In addition, a study reported that the increased abundance of Ruminococcaceae reduced arterial stiffness [99]. There is an association between arterial stiffness and cardiovascular diseases, while obesity is a dangerous risk factor for arterial stiffness and cardiovascular disease [100,101]. Faecalibaculum has been reported to have a higher fermentation capability, especially for the production of butyrate [102]. Our results showed that HTE supplementation increases the level of SCFAs in Lepr−/− rats. SCFAs are organic fatty acids that have fewer than six carbon atoms and are considered a key mediator of the beneficial effects elicited by gut microbiota. Accumulating evidence suggests that SCFAs contribute to the improvement of physiological status of hosts by targeting multiple pathways [103,104]. Recent studies have shown that SCFAs can reduce inflammation and maintain blood glucose stability [104]. Additionally, the SCFAs also increase fatty acid oxidation inhibit fatty acid synthesis, and increase heat production to prevent obesity [105]. The results of our study indicated that the propanoic acid, butyric acid, isobutyric acid, pentanoic acid, as well as isopentanoic acid levels in the feces of the Lepr−/− rats increased significantly after supplementation with HTE. This may explain a further mechanism by which HTE improves obesity related disorder. Additionally, the present results showed that HTE supplementation significantly increased the abundance of Mucispirillum. Previous published papers reported that Mucispirillum can antagonize the toxicity of Salmonella and help mice resist colitis [106]. However, HTE supplementation significantly reduced Lactobacillus abundance in Lepr−/− rats. Studies reported that Lactobacillus may function as preventing HFD-induced obesity [107]. However, Lactobacillus functions are not consistent. According to Nie et al., Lactobacillus abundance is positively related to fasting blood glucose and HOMA-IR [108]. Sato et al. found a decline in butyrate-producing bacteria as well as an increase in Lactobacillus species and opportunistic pathogens in the development of type 2 diabetes [109]. Therefore, further research is required to understand the relationship between Lactobacillus and obesity. Altogether, the present study found that prevention of obesity complication by HTE may be possible through maintaining homeostasis of gut microbiota, increasing specific SCFA-producing bacteria, balancing hepatic lipid classes, and elevating certain hepatic lipid classes in Lepr−/− rats.
5. Conclusions
In conclusion, our results showed that long term HTE supplementation remarkably reduced excessive fat accumulation, as well as ameliorated hyperlipidemia and hepatic steatosis in Lepr−/− rats. In addition, HTE increased gut microbiota diversity and restored the relative abundance of the microbiota responsible for producing short chain fatty acids, including Ruminococcaceae, Faecalibaculum, and Veillonellaceae, etc. Hepatic lipidomics analysis found that HTE significantly recovered glycerolipid and glycerophospholipid classes in the liver of Lepr−/− rats. By combination of gut microbiota and hepatic lipidomics data, our results indicated that prevention of obesity related metabolic disorder by HTE may be possible through maintaining homeostasis of gut microbiota and certain hepatic glycerolipid and glycerophospholipid classes.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/foods11192939/s1, Figure S1: The weights of liver, inguinal fat, and epididymal fat relative to whole body weight in Lepr−/− rats; Figure S2: Effects of HTE on food intake in Lepr−/− rats; Figure S3: Histopathology image of the livers of Lepr−/− rats (H & E, 100×); Figure S4: The distribution of lipid classes determined by UHPLC-Orbitrap-MS/MS in liver samples; Figure S5: Effects of HTE on glucose tolerance in Lepr−/− rats; Figure S6: HTE enhanced SCFA production in Lepr−/− rats; Table S1. Experimental diet compositions; Table S2: Real-time PCR primers used to analyze gene expression.
Author Contributions
G.W. performed the experiments, analyzed data, and prepared the manuscript draft; W.G. analyzed the data and prepared the manuscript draft; H.C. and H.G. performed the experiments; D.L. conceived the research goals and experimental design and edited the manuscript; Z.X. conceived the research goals and experimental design, analyzed data, and prepared and edited the manuscript. All authors have read and agreed to the published version of the manuscript.
Funding
This study was supported by a key joint grant for regional innovation from the National Natural Science Foundation of China (U19A2034), a key grant for University Synergy Innovation Program of Anhui Province (GXXT-2019-49), a grant from China Agriculture Research System of MOF and MARA (CARS-19), and a grant for supporting animal core facility in Anhui Agricultural University from the Department of Sciences and Technology of Anhui Province.
Institutional Review Board Statement
All procedures involving animals studies were approved on 4 April 2019 by the Institutional Animal Care and Use Committee of the Anhui Agricultural University (ethical approval code: AHAU 2019-034).
Informed Consent Statement
Not applicable.
Data Availability Statement
The data are available from the corresponding author.
Conflicts of Interest
The authors declare no conflict of interest.
Abbreviations
ACC, acetyl–CoA carboxylase α; Cer, ceramides; CL, cardiolipins; Co, coenzyme; DG, diglyceride; dMePE, dimethyl–phosphatidylethanolamine(s); FAS, fatty acid synthase; GSP, glycated serum protein; HMGCR, 3-hydroxy-3-methylglutaryl-CoA reductase; LPC, lyso–phosphatidylcholine(s); LPE, lyso–phosphatidylethanolamine(s); LXRα, liver X receptor α; PC, phosphatidylcholine(s); PE, phosphatidylethanolamine(s); PEt, polyethylene terephthalate; PG, phosphatidylglycerols; PI, phosphatidylinositol(s); PPARγ, peroxisome proliferators–activated receptors; PS, phosphatidylserines; RBG, random blood glucose; SCD1, stearoyl–CoA desaturase 1; SM, sphingomyelin(s); SREBP1, sterol regulatory element–binding transcription factor 1; TC, total cholesterol; TG, triglyceride; THRSP, thyroid hormone responsive spot 14.
References
- Marie-Eve, P.; André, T.; Jean-Pierre, D. Obesity Phenotypes, Diabetes, and Cardiovascular Diseases. Circ. Res. 2020, 126, 1477–1500. [Google Scholar]
- Damsgaard, C.T.; Michaelsen, K.F.; Molbo, D.; Mortensen, E.L.; Sørensen, T. Trends in adult body-mass index in 200 countries from 1975 to 2014: A pooled analysis of 1698 population-based measurement studies with 19.2 million participants. Lancet 2016, 387, 1377. [Google Scholar]
- Afshin, A.; Reitsma, M.B.; Murray, C.J.L. Health Effects of Overweight and Obesity in 195 Countries. N. Engl. J. Med. 2017, 377, 1495–1497. [Google Scholar]
- Gammone, M.A.; D’Orazio, N. COVID-19 and Obesity: Overlapping of Two Pandemics. Obes. Facts. 2021, 14, 579–585. [Google Scholar] [CrossRef]
- Landecho, M.F.; Marin-Oto, M.; Recalde-Zamacona, B.; Bilbao, I.; Frühbeck, G. Obesity as an Adipose tissue dysfunction disease and A Risk Factor for Infections—COVID-19 as a case study. Eur. J. Intern. Med. 2021, 91, 3–9. [Google Scholar] [CrossRef]
- World Health Organization. World Health Statistics 2021: Monitoring Health for the SDGs, Sustainable Development Goals. 2021. Available online: www.who.int/data/gho/publications/world-health-statistics (accessed on 5 March 2022).
- Caballero, B. Humans against Obesity: Who Will Win. Adv. Nutr. 2019, 10, S4–S9. [Google Scholar] [CrossRef]
- Siavash, M.; Tabbakhian, M.; Sabzghabaee, A.M.; Razavi, N. Severity of gastrointestinal side effects of metformin tablet compared to metformin capsule in type 2 diabetes mellitus patients. J. Res. Pharm. Pract. 2017, 6, 73–76. [Google Scholar]
- Turner, R.M.; Pirmohamed, M. Statin-Related Myotoxicity: A Comprehensive Review of Pharmacokinetic, Pharmacogenomic and Muscle Components. J. Clin. Med. 2019, 9, 22. [Google Scholar] [CrossRef]
- Mammen, A.L.; Tiniakou, E. Intravenous Immune Globulin for Statin-Triggered Autoimmune Myopathy. N. Engl. J. Med. 2015, 373, 1680–1682. [Google Scholar] [CrossRef]
- Chen, H.; Nie, Q.; Hu, J.; Huang, X.; Zhang, K.; Pan, S.; Nie, S. Hypoglycemic and Hypolipidemic Effects of Glucomannan Extracted from Konjac on Type 2 Diabetic Rats. J. Agric. Food Chem. 2019, 67, 5278–5288. [Google Scholar] [CrossRef]
- Teng, Y.; Li, D.; Guruvaiah, P.; Xu, N.; Xie, Z. Dietary Supplement of Large Yellow Tea Ameliorates Metabolic Syndrome and Attenuates Hepatic Steatosis in db/db Mice. Nutrients 2018, 10, 75. [Google Scholar] [CrossRef]
- Wang, H.N.; Xiang, J.Z.; Qi, Z.; Du, M. Plant extracts in prevention of obesity. Crit. Rev. Food Sci. Nutr. 2022, 62, 2221–2234. [Google Scholar] [CrossRef]
- Busetto, L.; Sbraccia, P.; Vettor, R. Obesity management: At the forefront against disease stigma and therapeutic inertia. Eat. Weight Disord. 2022, 27, 761–768. [Google Scholar] [CrossRef]
- Aron-Wisnewsky, J.; Warmbrunn, M.V.; Nieuwdorp, M.; Clément, K. Metabolism and Metabolic Disorders and the Microbiome: The Intestinal Microbiota Associated with Obesity, Lipid Metabolism, and Metabolic Health-Pathophysiology and Therapeutic Strategies. Gastroenterology 2021, 160, 573–599. [Google Scholar] [CrossRef]
- Górowska-Kowolik, K.; Chobot, A. The role of gut micorbiome in obesity and diabetes. World J. Pediatr. 2019, 15, 332–340. [Google Scholar] [CrossRef]
- Chen, T.; Yang, C.S. Biological fates of tea polyphenols and their interactions with microbiota in the gastrointestinal tract: Implications on health effects. Crit. Rev. Food Sci. Nutr. 2020, 60, 2691–2709. [Google Scholar] [CrossRef]
- Nie, Q.; Chen, H.; Hu, J.; Fan, S.; Nie, S. Dietary compounds and traditional Chinese medicine ameliorate type 2 diabetes by modulating gut microbiota. Crit. Rev. Food Sci. Nutr. 2019, 59, 848–863. [Google Scholar] [CrossRef]
- Fang, Q.; Hu, J.; Nie, Q.; Nie, S. Effects of polysaccharides on glycometabolism based on gut microbiota alteration. Trends Food Sci. Technol. 2019, 92, 65–70. [Google Scholar] [CrossRef]
- Sang, S.; Lambert, J.D.; Ho, C.T.; Yang, C.S. The chemistry and biotransformation of tea constituents. Pharmacol. Res. 2011, 64, 87–99. [Google Scholar] [CrossRef] [PubMed]
- Yang, C.S.; Zhang, J.; Zhang, L.; Huang, J.; Wang, Y. Mechanisms of body weight reduction and metabolic syndrome alleviation by tea. Mol. Nutr. Food Res. 2016, 60, 160–174. [Google Scholar] [CrossRef] [PubMed]
- Khan, N.; Mukhtar, H. Tea Polyphenols in Promotion of Human Health. Nutrients 2018, 11, 39. [Google Scholar] [CrossRef]
- Li, D.; Wang, R.; Huang, J.; Cai, Q.; Yang, C.S.; Wan, X.; Xie, Z. Effects and Mechanisms of Tea Regulating Blood Pressure: Evidences and Promises. Nutrients 2019, 11, 1115. [Google Scholar] [CrossRef]
- Liu, Z.; Chen, Z.; Guo, H.; He, D.; Zhao, H.; Wang, Z.; Zhang, W.; Liao, L.; Zhang, C.; Ni, L. The modulatory effect of infusions of green tea, oolong tea, and black tea on gut microbiota in high-fat-induced obese mice. Food Funct. 2016, 7, 4869–4879. [Google Scholar] [CrossRef]
- Li, H.; Fang, Q.; Nie, Q.; Hu, J.; Yang, C.; Huang, T.; Li, H.; Nie, S. Hypoglycemic and Hypolipidemic Mechanism of Tea Polysaccharides on Type 2 Diabetic Rats via Gut Microbiota and Metabolism Alteration. J. Agric. Food Chem. 2020, 68, 10015–10028. [Google Scholar] [CrossRef]
- Liu, D.; Huang, J.; Luo, Y.; Wen, B.; Wu, W.; Zeng, H.; Zhonghua, L. Fuzhuan Brick Tea Attenuates High-Fat Diet-Induced Obesity and Associated Metabolic Disorders by Shaping Gut Microbiota. J. Agric. Food Chem. 2019, 67, 13589–13604. [Google Scholar] [CrossRef]
- Chen, T.; Liu, A.B.; Sun, S.; Ajami, N.J.; Ross, M.C.; Wang, H.; Zhang, L.; Reuhl, K.; Kobayashi, K.; Onishi, J.C. Green Tea Polyphenols Modify the Gut Microbiome in db/db Mice as Co-Abundance Groups Correlating with the Blood Glucose Lowering Effect. Mol. Nutr. Food Res. 2019, 63, e1801064. [Google Scholar] [CrossRef]
- Wu, G.; Sun, X.; Cheng, H.; Xu, S.; Li, D.; Xie, Z. Large Yellow Tea Extract Ameliorates Metabolic Syndrome by Suppressing Lipogenesis through SIRT6/SREBP1 Pathway and Modulating Microbiota in Leptin Receptor Knockout Rats. Foods 2022, 11, 1638. [Google Scholar] [CrossRef]
- Han, Z.; Wen, M.; Zhang, H.; Zhang, L.; Wan, X.; Ho, C.T. LC-MS based metabolomics and sensory evaluation reveal the critical compounds of different grades of Huangshan Maofeng green tea. Food Chem. 2022, 374, 131796. [Google Scholar] [CrossRef]
- Zeng, X.; Tian, J.; Cai, K.; Wu, X.; Wang, Y.; Zheng, Y.; Su, Y.; Cui, L. Promoting osteoblast differentiation by the flavanes from Huangshan Maofeng tea is linked to a reduction of oxidative stress. Phytomedicine 2014, 21, 217–224. [Google Scholar] [CrossRef]
- Cui, Y.; Yang, X.; Lu, X.; Chen, J.; Zhao, Y. Protective effects of polyphenols-enriched extract from Huangshan Maofeng green tea against CCl4-induced liver injury in mice. Chem. Biol. Interact. 2014, 220, 75–83. [Google Scholar] [CrossRef]
- Liu, Z.; Xiao, M.; Du, Z.; Li, M.; Guo, H.; Yao, M.; Wan, X.; Xie, Z. Dietary supplementation of Huangshan Maofeng green tea preventing hypertension of older C57BL/6 mice induced by desoxycorticosterone acetate and salt. J. Nutr. Biochem. 2021, 88, 108530. [Google Scholar] [CrossRef]
- Bechmann, L.P.; Hannivoort, R.A.; Gerken, G.; Hotamisligil, G.S.; Trauner, M.; Canbay, A. The interaction of hepatic lipid and glucose metabolism in liver diseases. J. Hepatol. 2012, 56, 952–964. [Google Scholar] [CrossRef]
- Preuss, C.; Jelenik, T.; Bódis, K.; Müssig, K.; Burkart, V.; Szendroedi, J.; Roden, M.; Markgraf, D.F. A New Targeted Lipidomics Approach Reveals Lipid Droplets in Liver, Muscle and Heart as a Repository for Diacylglycerol and Ceramide Species in Non-Alcoholic Fatty Liver. Cells 2019, 8, 277. [Google Scholar] [CrossRef]
- Marchesini, G.; Petta, S.; Dalle Grave, R. Diet, Weight Loss, and Liver Health in NAFLD: Pathophysiology, Evidence and Practice. Hepatology 2016, 63, 2032–2043. [Google Scholar] [CrossRef]
- Yang, K.; Han, X. Lipidomics: Techniques, Applications, and Outcomes Related to Biomedical Sciences. Trends Biochem. Sci. 2016, 41, 954–969. [Google Scholar] [CrossRef]
- Shon, J.C.; Kim, W.C.; Ryu, R.; Wu, Z.; Seo, J.S.; Choi, M.S.; Liu, K.H. Plasma Lipidomics Reveals Insights into Anti-Obesity Effect of Chrysanthemum morifolium Ramat Leaves and Its Constituent Luteolin in High-Fat Diet-Induced Dyslipidemic Mice. Nutrients 2020, 12, 2973. [Google Scholar] [CrossRef]
- Nam, M.; Choi, M.S.; Choi, J.Y.; Kim, N.; Kim, M.S.; Jung, S.; Kim, J.; Ryu, D.H.; Hwang, G.S. Effect of green tea on hepatic lipid metabolism in mice fed a high-fat diet. J. Nutr. Biochem. 2018, 51, 1–7. [Google Scholar] [CrossRef]
- Bao, D.; Ma, Y.; Zhang, X.; Guan, F.; Chen, W.; Gao, K.; Qin, C.; Zhang, L. Preliminary Characterization of a Leptin Receptor Knockout Rat Created by CRISPR/Cas9 System. Sci. Rep. 2015, 5, 15942. [Google Scholar] [CrossRef]
- Yao, F.; Jiang, D.D.; Guo, W.H.; Guo, L.S.; Gao, M.M.; Bai, Y.; Wang, X.; Zhang, L.S. FABP4 inhibitor attenuates inflammation and endoplasmic reticulum stress of islet in leptin receptor knockout rats. Eur. Rev. Med. Pharmacol. Sci. 2020, 24, 12808–12820. [Google Scholar]
- Li, R.; Peng, S.; Ye, H.; Li, D.; Granato, D.; Guo, H.; Xie, Z. Metabolite differentiation and antiobesity effects between different grades of Yuexi Cuilan green tea. J. Funct. Foods 2021, 87, 104794. [Google Scholar] [CrossRef]
- Wen, J.J.; Li, M.Z.; Gao, H.; Hu, J.L.; Nie, Q.X.; Chen, H.H.; Zhang, Y.L.; Xie, M.Y.; Nie, S.P. Polysaccharides from fermented Momordica charantia L. with Lactobacillus plantarum NCU116 ameliorate metabolic disorders and gut microbiota change in obese rats. Food Funct. 2021, 12, 2617–2630. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.; Gu, M.; Wang, R.; Li, M.; Li, D.; Xie, Z. Dietary supplement of Yunkang 10 green tea and treadmill exercise ameliorate high fat diet induced metabolic syndrome of C57BL/6J mice. Nutr. Metab. 2020, 17, 14. [Google Scholar] [CrossRef] [PubMed]
- Xie, Z.; Su, W.; Liu, S.; Zhao, G.; Esser, K.; Schroder, E.A.; Lefta, M.; Stauss, H.M.; Guo, Z.; Gong, M.C. Smooth-muscle BMAL1 participates in blood pressure circadian rhythm regulation. J. Clin. Investig. 2015, 125, 324–336. [Google Scholar] [CrossRef] [PubMed]
- Li, M.; Shen, Y.; Ling, T.; Ho, C.T.; Li, D.; Guo, H.; Xie, Z. Analysis of Differentiated Chemical Components between Zijuan Purple Tea and Yunkang Green Tea by UHPLC-Orbitrap-MS/MS Combined with Chemometrics. Foods 2021, 10, 1070. [Google Scholar] [CrossRef]
- Pourabedin, M.; Guan, L.; Zhao, X. Xylo-oligosaccharides and virginiamycin differentially modulate gut microbial composition in chickens. Microbiome 2015, 3, 15. [Google Scholar] [CrossRef]
- Besten, G.D.; Bleeker, A.; Gerding, A.; Eunen, K.V.; Havinga, R.; Dijk, T.V.; Oosterveer, M.H.; Jonker, J.W.; Groen, A.K.; Reijngoud, D.J. Short-Chain Fatty Acids Protect Against High-Fat Diet-Induced Obesity via a PPARγ-Dependent Switch from Lipogenesis to Fat Oxidation. Diabetes 2015, 64, 2398–2408. [Google Scholar] [CrossRef]
- Turnbaugh, P.J.; Hamady, M.; Yatsunenko, T.; Cantarel, B.L.; Duncan, A.; Ley, R.E.; Sogin, M.L.; Jones, W.J.; Roe, B.A.; Affourtit, J.P.; et al. A core gut microbiome in obese and lean twins. Nature 2009, 457, 480–484. [Google Scholar] [CrossRef]
- Huang, J.; Wang, Y.; Xie, Z.; Zhou, Y.; Zhang, Y.; Wan, X. The anti-obesity effects of green tea in human intervention and basic molecular studies. Eur. J. Clin. Nutr. 2014, 68, 1075–1087. [Google Scholar] [CrossRef]
- Dinh, T.C.; Thi Phuong, T.N.; Minh, L.B.; Minh Thuc, V.T.; Bac, N.D.; Van Tien, N.; Pham, V.H.; Show, P.L.; Tao, Y.; Nhu Ngoc, V.T.; et al. The effects of green tea on lipid metabolism and its potential applications for obesity and related metabolic disorders—An existing update. Diabetes Metab. Syndr. 2019, 13, 1667–1673. [Google Scholar] [CrossRef]
- Huang, J.; Feng, S.; Liu, A.; Dai, Z.; Wang, H.; Reuhl, K.; Lu, W.; Yang, C.S. Green Tea Polyphenol EGCG Alleviates Metabolic Abnormality and Fatty Liver by Decreasing Bile Acid and Lipid Absorption in Mice. Mol. Nutr. Food Res. 2018, 62, 101002. [Google Scholar] [CrossRef]
- Choi, C.; Song, H.D.; Son, Y.; Cho, Y.K.; Ahn, S.Y.; Jung, Y.S.; Yoon, Y.C.; Kwon, S.W.; Lee, Y.H. Epigallocatechin-3-Gallate Reduces Visceral Adiposity Partly through the Regulation of Beclin1-Dependent Autophagy in White Adipose Tissues. Nutrients 2020, 12, 3072. [Google Scholar] [CrossRef]
- Chen, G.; Chen, R.; Chen, D.; Ye, H.; Hu, B.; Zeng, X.; Liu, Z. Tea Polysaccharides as Potential Therapeutic Options for Metabolic Diseases. J. Agric. Food Chem. 2019, 67, 5350–5360. [Google Scholar] [CrossRef]
- Wu, L.; Meng, J.; Shen, Q.; Zhang, Y.; Pan, S.; Chen, Z.; Zhu, L.Q.; Lu, Y.; Huang, Y.; Zhang, G. Caffeine inhibits hypothalamic A1R to excite oxytocin neuron and ameliorate dietary obesity in mice. Nat. Commun. 2017, 8, 15904. [Google Scholar] [CrossRef]
- Zhu, M.Z.; Zhou, F.; Ouyang, J.; Wang, Q.Y.; Li, Y.L.; Wu, J.L.; Huang, J.A.; Liu, Z.H. Combined use of epigallocatechin-3-gallate (EGCG) and caffeine in low doses exhibits marked anti-obesity synergy through regulation of gut microbiota and bile acid metabolism. Food Funct. 2021, 12, 4105–4116. [Google Scholar] [CrossRef]
- Wu, G.; Liu, A.B.; Xu, Y.; Wang, Y.; Zhao, L.; Hara, Y.; Lam, Y.Y.; Yang, C.S. The Effects of Green Tea on Diabetes and Gut Microbiome in db/db Mice: Studies with Tea Extracts vs. Tea Powder. Nutrients 2021, 13, 3135. [Google Scholar] [CrossRef]
- Yousaf, S.; Butt, M.S.; Suleria, H.A.R.; Iqbal, M.J. The role of green tea extract and powder in mitigating metabolic syndromes with special reference to hyperglycemia and hypercholesterolemia. Food Funct. 2014, 5, 545–556. [Google Scholar] [CrossRef]
- Rocha, A.; Bolin, A.P.; Cardoso, C.A.; Otton, R. Green tea extract activates AMPK and ameliorates white adipose tissue metabolic dysfunction induced by obesity. Eur. J. Nutr. 2016, 55, 2231–2244. [Google Scholar] [CrossRef]
- Xia, H.M.; Wang, J.; Xie, X.J.; Xu, L.J.; Tang, S.Q. Green tea polyphenols attenuate hepatic steatosis, and reduce insulin resistance and inflammation in high-fat diet-induced rats. Int. J. Mol. Med. 2019, 44, 1523–1530. [Google Scholar] [CrossRef]
- Han, M.; Zhao, G.; Wang, Y.; Wang, D.; Sun, F.; Ning, J.; Wan, X.; Zhang, J. Safety and anti-hyperglycemic efficacy of various tea types in mice. Sci. Rep. 2016, 6, 31703. [Google Scholar] [CrossRef]
- Hawkins, M.; Tonelli, J.; Kishore, P.; Stein, D.; Ragucci, E.; Gitig, A.; Reddy, K. Contribution of Elevated Free Fatty Acid Levels to the Lack of Glucose Effectiveness in Type 2 Diabetes. Diabetes 2003, 52, 2748–2758. [Google Scholar] [CrossRef]
- Bogdanski, P.; Suliburska, J.; Szulinska, M.; Stepien, M.; Pupek-Musialik, D.; Jablecka, A. Green tea extract reduces blood pressure, inflammatory biomarkers, and oxidative stress and improves parameters associated with insulin resistance in obese, hypertensive patients. Nutr. Res. 2012, 32, 421–427. [Google Scholar] [CrossRef] [PubMed]
- Qin, S.; He, Z.; Wu, Y.; Zeng, C.; Zheng, Z.; Zhang, H.; Lv, C.; Yuan, Y.; Wu, H.; Ye, J.; et al. Instant Dark Tea Alleviates Hyperlipidaemia in High-Fat Diet-Fed Rat: From Molecular Evidence to Redox Balance and Beyond. Front. Nutr. 2022, 9, 819980. [Google Scholar] [CrossRef] [PubMed]
- Sanders, F.W.; Griffin, J.L. De novo lipogenesis in the liver in health and disease: More than just a shunting yard for glucose. Biol. Rev. Camb. Philos. Soc. 2016, 91, 452–468. [Google Scholar] [CrossRef] [PubMed]
- Shrestha, S.; Ehlers, S.J.; Lee, J.Y.; Fernandez, M.L.; Koo, S.I. Dietary green tea extract lowers plasma and hepatic triglycerides and decreases the expression of sterol regulatory element-binding protein-1c mRNA and its responsive genes in fructose-fed, ovariectomized rats. J. Nutr. 2009, 139, 640–645. [Google Scholar] [CrossRef]
- Oppi-Williams, C.; Suagee, J.K.; Corl, B.A. Regulation of lipid synthesis by liver X receptor α and sterol regulatory element-binding protein 1 in mammary epithelial cells. J. Dairy. Sci. 2013, 96, 112–121. [Google Scholar] [CrossRef]
- Joseph, S.B.; Laffitte, B.A.; Patel, P.H.; Watson, M.A.; Matsukuma, K.E.; Walczak, R.; Collins, J.L.; Osborne, T.F.; Tontonoz, P. Direct and indirect mechanisms for regulation of fatty acid synthase gene expression by liver X receptors. J. Biol. Chem. 2002, 277, 11019–11025. [Google Scholar] [CrossRef]
- Jing, W.; Wang, C.; Li, S.; Sha, L.; Wang, W.; Jing, L.; Chi, Y.; Hang, Y.; Kong, X. Thrsp promotes hepatic lipogenesis, and its expression is regulated by LXRα through an SREBP1c-dependent mechanism. Hepatology 2013, 58, 617–628. [Google Scholar]
- Zhu, Q.; Anderson, G.W.; Mucha, G.T.; Parks, E.J.; Metkowski, J.K.; Mariash, C.N. The Spot 14 protein is required for de novo lipid synthesis in the lactating mammary gland. Endocrinology 2005, 146, 3343. [Google Scholar] [CrossRef]
- Evans, R.M.; Barish, G.D.; Wang, Y.X. PPARs and the complex journey to obesity. Nat. Med. 2004, 10, 355–361. [Google Scholar] [CrossRef]
- Matsusue, K.; Haluzik, M.; Lambert, G.; Yim, S.H.; Gavrilova, O.; Ward, J.M.; Brewer, B., Jr.; Reitman, M.L.; Gonzalez, F.J. Liver-specific disruption of PPARγ in leptin-deficient mice improves fatty liver but aggravates diabetic phenotypes. J. Clin. Investig. 2003, 111, 737. [Google Scholar] [CrossRef]
- Li, Z.Z.; Berk, M.; McIntyre, T.M.; Feldstein, A.E. Hepatic lipid partitioning and liver damage in nonalcoholic fatty liver disease: Role of stearoyl-CoA desaturase. J. Biol. Chem. 2009, 284, 5637–5644. [Google Scholar] [CrossRef]
- Chirala, S.S.; Chang, H.; Matzuk, M.; Abu-Elheiga, L.; Mao, J.; Mahon, K.; Finegold, M.; Wakil, S.J. Fatty acid synthesis is essential in embryonic development: Fatty acid synthase null mutants and most of the heterozygotes die in utero. Proc. Natl. Acad. Sci. USA 2003, 100, 6358–6363. [Google Scholar] [CrossRef]
- Zhong, S.; Li, L.; Liang, N.; Zhang, L.; Xu, X.; Chen, S.; Yin, H. Acetaldehyde Dehydrogenase 2 regulates HMG-CoA reductase stability and cholesterol synthesis in the liver. Redox Biol. 2021, 41, 101919. [Google Scholar] [CrossRef]
- Feng, S.; Dai, Z.; Liu, A.B.; Huang, J.; Narsipur, N.; Guo, G.; Kong, B.; Reuhl, K.; Lu, W.; Luo, Z.; et al. Intake of stigmasterol and β-sitosterol alters lipid metabolism and alleviates NAFLD in mice fed a high-fat western-style diet. Biochim. Biophys. Acta Mol. Cell Biol. Lipids 2018, 1863, 1274–1284. [Google Scholar] [CrossRef]
- Gorden, D.L.; Ivanova, P.T.; Myers, D.S.; McIntyre, J.O.; VanSaun, M.N.; Wright, J.K.; Matrisian, L.M.; Brown, H.A. Increased diacylglycerols characterize hepatic lipid changes in progression of human nonalcoholic fatty liver disease; comparison to a murine model. PLoS ONE 2011, 6, e22775. [Google Scholar] [CrossRef]
- Ruby, M.A.; Massart, J.; Hunerdosse, D.M.; Schönke, M.; Correia, J.C.; Louie, S.M.; Ruas, J.L.; Näslund, E.; Nomura, D.K.; Zierath, J.R. Human Carboxylesterase 2 Reverses Obesity-Induced Diacylglycerol Accumulation and Glucose Intolerance. Cell Rep. 2017, 18, 636–646. [Google Scholar] [CrossRef]
- Feng, K.; Lan, Y.; Zhu, X.; Li, J.; Chen, T.; Huang, Q.; Ho, C.T.; Chen, Y.; Cao, Y. Hepatic Lipidomics Analysis Reveals the Antiobesity and Cholesterol-Lowering Effects of Tangeretin in High-Fat Diet-Fed Rats. J. Agric. Food Chem. 2020, 68, 6142–6153. [Google Scholar] [CrossRef]
- Rhee, E.P.; Cheng, S.; Larson, M.G.; Walford, G.A.; Lewis, G.D.; McCabe, E.; Yang, E.; Farrell, L.; Fox, C.S.; O’Donnell, C.J.; et al. Lipid profiling identifies a triacylglycerol signature of insulin resistance and improves diabetes prediction in humans. J. Clin. Investig. 2011, 121, 1402–1411. [Google Scholar] [CrossRef]
- Stegemann, C.; Pechlaner, R.; Willeit, P.; Langley, S.R.; Mangino, M.; Mayr, U.; Menni, C.; Moayyeri, A.; Santer, P.; Rungger, G.; et al. Lipidomics profiling and risk of cardiovascular disease in the prospective population-based Bruneck study. Circulation 2014, 129, 1821–1831. [Google Scholar] [CrossRef]
- Kihara, A. Very long-chain fatty acids: Elongation, physiology and related disorders. J. Biochem. 2012, 152, 387–395. [Google Scholar] [CrossRef]
- Niu, Z.; Wu, Q.; Sun, L.; Qi, Q.; Zheng, H.; Li, H.; Zeng, R.; Lin, X.; Zong, G. Circulating Glycerolipids, Fatty Liver Index, and Incidence of Type 2 Diabetes: A Prospective Study Among Chinese. J. Clin. Endocrinol. Metab. 2021, 106, 2010–2020. [Google Scholar] [CrossRef] [PubMed]
- Tabe, S.; Hikiji, H.; Ariyoshi, W.; Hashidate-Yoshida, T.; Shindou, H.; Shimizu, T.; Okinaga, T.; Seta, Y.; Tominaga, K.; Nishihara, T. Lysophosphatidylcholine acyltransferase 4 is involved in chondrogenic differentiation of ATDC5 cells. Sci. Rep. 2017, 7, 16701. [Google Scholar] [CrossRef] [PubMed]
- Hishikawa, D.; Hashidate, T.; Shimizu, T.; Shindou, H. Diversity and function of membrane glycerophospholipids generated by the remodeling pathway in mammalian cells. J. Lipid Res. 2014, 55, 799–807. [Google Scholar] [CrossRef] [PubMed]
- Feng, S.; Gan, L.; Yang, C.S.; Liu, A.B.; Lu, W.; Shao, P.; Dai, Z.; Sun, P.; Luo, Z. Effects of Stigmasterol and beta-Sitosterol on Nonalcoholic Fatty Liver Disease in a Mouse Model: A Lipidomic Analysis. J. Agric. Food Chem. 2018, 66, 3417–3425. [Google Scholar] [CrossRef] [PubMed]
- Liu, H.; Chen, T.; Xie, X.; Wang, X.; Luo, Y.; Xu, N.; Sa, Z.; Zhang, M.; Chen, Z.; Hu, X.; et al. Hepatic Lipidomics Analysis Reveals the Ameliorative Effects of Highland Barley β-Glucan on Western Diet-Induced Nonalcoholic Fatty Liver Disease Mice. J. Agric. Food Chem. 2021, 69, 9287–9298. [Google Scholar] [CrossRef] [PubMed]
- Calzada, E.; Onguka, O.; Claypool, S.M. Phosphatidylethanolamine Metabolism in Health and Disease. Int. Rev. Cell Mol. Bio. 2016, 321, 29–88. [Google Scholar]
- Glade, M.J.; Smith, K. Phosphatidylserine and the human brain. Nutrition 2015, 31, 781–786. [Google Scholar] [CrossRef] [PubMed]
- Osman, C.; Voelker, D.R.; Langer, T. Making heads or tails of phospholipids in mitochondria. J. Cell Biol. 2011, 192, 7–16. [Google Scholar] [CrossRef]
- Bouter, K.E.; Raalte, D.V.; Groen, A.K.; Nieuwdorp, M. Role of the Gut Microbiome in the Pathogenesis of Obesity and Obesity-Related Metabolic Dysfunction. Gastroenterology 2017, 152, 1671. [Google Scholar] [CrossRef]
- Goodrich, J.; Waters, J.; Poole, A.; Sutter, J.; Koren, O.; Blekhman, R.; Beaumont, M.; Van Treuren, W.; Knight, R.; Bell, J. Human genetics shape the gut microbiome. Cell 2014, 159, 789–799. [Google Scholar] [CrossRef]
- Wang, L.; Zeng, B.; Liu, Z.; Liao, Z.; Zhong, Q.; Gu, L.; Wei, H.; Fang, X. Green Tea Polyphenols Modulate Colonic Microbiota Diversity and Lipid Metabolism in High-Fat Diet Treated HFA Mice. J. Food Sci. 2018, 83, 864–873. [Google Scholar] [CrossRef]
- Santacruz, A.; Collado, M.C.; García-Valdés, L.; Segura, M.T.; Martín-Lagos, J.A.; Anjos, T.; Martí-Romero, M.; Lopez, R.M.; Florido, J.; Campoy, C.; et al. Gut microbiota composition is associated with body weight, weight gain and biochemical parameters in pregnant women. Br. J. Nutr. 2010, 104, 83–92. [Google Scholar] [CrossRef]
- Chen, G.; Xie, M.; Dai, Z.; Wan, P.; Ye, H.; Zeng, X.; Sun, Y. Kudingcha and Fuzhuan Brick Tea Prevent Obesity and Modulate Gut Microbiota in High-Fat Diet Fed Mice. Mol. Nutr. Food Res. 2018, 62, e1700485. [Google Scholar] [CrossRef]
- Darnaud, M.; Dos Santos, A.; Gonzalez, P.; Augui, S.; Lacoste, C.; Desterke, C.; De Hertogh, G.; Valentino, E.; Braun, E.; Zheng, J.; et al. Enteric Delivery of Regenerating Family Member 3 alpha Alters the Intestinal Microbiota and Controls Inflammation in Mice with Colitis. Gastroenterology 2018, 154, 1009–1023.e14. [Google Scholar] [CrossRef]
- Wang, L.; Liao, Y.; Yang, R.; Zhu, Z.; Zhang, L.; Wu, Z.; Sun, X. An engineered probiotic secreting Sj16 ameliorates colitis via Ruminococcaceae/butyrate/retinoic acid axis. Bioeng. Transl. Med. 2021, 6, e10219. [Google Scholar] [CrossRef]
- Coppola, S.; Avagliano, C.; Calignano, A.; Berni Canani, R. The Protective Role of Butyrate against Obesity and Obesity-Related Diseases. Molecules 2021, 26, 682. [Google Scholar] [CrossRef]
- Alsharairi, N.A. The Role of Short-Chain Fatty Acids in Mediating Very Low-Calorie Ketogenic Diet-Infant Gut Microbiota Relationships and Its Therapeutic Potential in Obesity. Nutrients 2021, 13, 3702. [Google Scholar] [CrossRef]
- Menni, C.; Lin, C.; Cecelja, M.; Mangino, M.; Matey-Hernandez, M.L.; Keehn, L.; Mohney, R.P.; Steves, C.J.; Spector, T.D.; Kuo, C.F.; et al. Gut microbial diversity is associated with lower arterial stiffness in women. Eur. Heart J. 2018, 39, 2390–2397. [Google Scholar] [CrossRef]
- Aroor, A.R.; Jia, G.; Sowers, J.R. Cellular mechanisms underlying obesity-induced arterial stiffness. Am. J. Physiol. Regul. Integr. Comp. Physiol. 2018, 314, R387–R398. [Google Scholar] [CrossRef]
- Koenen, M.; Hill, M.A.; Cohen, P.; Sowers, J.R. Obesity, Adipose Tissue and Vascular Dysfunction. Circ. Res. 2021, 128, 951–968. [Google Scholar] [CrossRef]
- Mao, G.; Li, S.; Orfila, C.; Shen, X.; Zhou, S.; Linhardt, R.J.; Ye, X.; Chen, S. Depolymerized RG-I-enriched pectin from citrus segment membranes modulates gut microbiota, increases SCFA production, and promotes the growth of Bifidobacterium spp., Lactobacillus spp. and Faecalibaculum spp. Food Funct. 2019, 10, 7828–7843. [Google Scholar] [CrossRef]
- González-Bosch, C.; Boorman, E.; Zunszain, P.A.; Mann, G.E. Short-chain fatty acids as modulators of redox signaling in health and disease. Redox Biol. 2021, 47, 102165. [Google Scholar] [CrossRef]
- He, J.; Zhang, P.; Shen, L.; Niu, L.; Tan, Y.; Chen, L.; Zhao, Y.; Bai, L.; Hao, X.; Li, X.; et al. Short-Chain Fatty Acids and Their Association with Signalling Pathways in Inflammation, Glucose and Lipid Metabolism. Int. J. Mol. Sci. 2020, 21, 6356. [Google Scholar] [CrossRef]
- Hu, J.; Lin, S.; Zheng, B.; Cheung, P.C.K. Short-chain fatty acids in control of energy metabolism. Crit. Rev. Food Sci. Nutr. 2018, 58, 1243–1249. [Google Scholar] [CrossRef]
- Herp, S.; Brugiroux, S.; Garzetti, D.; Ring, D.; Jochum, L.M.; Beutler, M.; Eberl, C.; Hussain, S.; Walter, S.; Gerlach, R.G.; et al. Mucispirillum schaedleri Antagonizes Salmonella Virulence to Protect Mice against Colitis. Cell Host Microbe 2019, 25, 681–694.e8. [Google Scholar] [CrossRef]
- Wang, J.; Tang, H.; Zhang, C.; Zhao, Y.; Derrien, M.; Rocher, E.; van-Hylckama Vlieg, J.E.; Strissel, K.; Zhao, L.; Obin, M.; et al. Modulation of gut microbiota during probiotic-mediated attenuation of metabolic syndrome in high fat diet-fed mice. ISME J. 2015, 9, 1–15. [Google Scholar] [CrossRef]
- Nie, Q.; Hu, J.; Chen, H.; Geng, F.; Nie, S. Arabinoxylan ameliorates type 2 diabetes by regulating the gut microbiota and metabolites. Food Chem. 2022, 371, 131106. [Google Scholar] [CrossRef]
- Sato, J.; Kanazawa, A.; Ikeda, F.; Yoshihara, T.; Goto, H.; Abe, H.; Komiya, K.; Kawaguchi, M.; Shimizu, T.; Ogihara, T.; et al. Gut dysbiosis and detection of “live gut bacteria” in blood of Japanese patients with type 2 diabetes. Diabetes Care 2014, 37, 2343–2350. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).