Current and Emerging Technologies for the Detection of Norovirus from Shellfish
Abstract
:1. Introduction
2. Current Norovirus Detection from Shellfish
3. Emerging Detection Technologies
3.1. Omics-Based Approaches
3.1.1. Metagenomics
3.1.2. Proteomics
3.1.3. Metabolomics
3.2. Emerging Technologies for Onsite Detection
3.2.1. Nanomaterials
3.2.2. Aptamer
3.2.3. Biosensor-Based Detection
3.2.4. Microfluidic Technology
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Hassard, F.; Sharp, J.H.; Taft, H.; LeVay, L.; Harris, J.P.; McDonald, J.E.; Tuson, K.; Wilson, J.; Jones, D.L.; Malham, S.K. Critical review on the public health impact of norovirus contamination in shellfish and the environment: A UK perspective. Food Environ. Virol. 2017, 9, 123–141. [Google Scholar] [CrossRef] [PubMed]
- Teunis, P.F.M.; Moe, C.L.; Liu, P.; Miller, S.E.; Lindesmith, L.; Baric, R.S.; Le Pendu, J.; Calderon, R.L. Norwalk virus: How infectious is it? J. Med. Virol. 2008, 80, 1468–1476. [Google Scholar] [CrossRef] [PubMed]
- Loisy, F.; Atmar, R.L.; Guillon, P.; Le Cann, P.; Pommepuy, M.; Le Guyader, F.S. Real-time RT-PCR for norovirus screening in shellfish. J. Virol. Methods 2005, 123, 1–7. [Google Scholar] [CrossRef]
- Le Guyader, F.S.; Atmar, R.L.; Le Pendu, J. Transmission of viruses through shellfish: When specific ligands come into play. Curr. Opin. Virol. 2012, 2, 103–110. [Google Scholar] [CrossRef]
- Provost, K.; Dancho, B.A.; Ozbay, G.; Anderson, R.S.; Richards, G.P.; Kingsley, D.H. Hemocytes are sites of enteric virus persistence within oysters. Appl. Environ. Microbiol. 2011, 77, 8360–8369. [Google Scholar] [CrossRef]
- Greening, G.E.; Hewitt, J.; Rivera-Aban, M.; Croucher, D. Molecular epidemiology of norovirus gastroenteritis outbreaks in New Zealand from 2002–2009. J. Med. Virol. 2012, 84, 1449–1458. [Google Scholar] [CrossRef] [PubMed]
- Alfano-Sobsey, E.; Sweat, D.; Hall, A.; Breedlove, F.; Rodriguez, R.; Greene, S.; Pierce, A.; Sobsey, M.; Davies, M.; Ledford, S.L. Norovirus outbreak associated with undercooked oysters and secondary household transmission. Epidemiol. Infect. 2012, 140, 276–282. [Google Scholar] [CrossRef]
- Bellou, M.; Kokkinos, P.; Vantarakis, A. Shellfish-borne viral outbreaks: A systematic review. Food Environ. Virol. 2013, 5, 13–23. [Google Scholar] [CrossRef]
- Lodo, K.L.; Veitch, M.G.K.; Green, M.L. An outbreak of norovirus linked to oysters in Tasmania. Commun. Dis. Intell. Q. Rep. 2014, 38, 16–19. [Google Scholar]
- Simmons, G.; Garbutt, C.; Hewitt, J.; Greening, G. A New Zealand outbreak of norovirus gastroenteritis linked to the consumption of imported raw Korean oysters. N. Z. Med. J. 2007, 120, U2773. [Google Scholar]
- Le Guyader, F.S.; Le Saux, J.C.; Ambert-Balay, K.; Krol, J.; Serais, O.; Parnaudeau, S.; Giraudon, H.; Delmas, G.; Pommepuy, M.; Pothier, P. Aichivirus, norovirus, astrovirus, enterovirus, and rotavirus involved in clinical cases from a French oyster-related gastroenteritis outbreak. J. Clin. Microbiol. 2008, 46, 4011–4017. [Google Scholar] [CrossRef] [PubMed]
- Hall, A.J.; Lopman, B.A.; Payne, D.C.; Patel, M.M.; Gastañaduy, P.A.; Vinje, J.; Parashar, U.D. Norovirus disease in the United States. Emerg. Infect. Dis. 2013, 19, 1198–1205. [Google Scholar] [CrossRef] [PubMed]
- Lim, K.L.; Hewitt, J.; Sitabkhan, A.; Eden, J.S.; Lun, J.; Levy, A.; Merif, J.; Smith, D.; Rawlinson, W.D.; White, P.A. A multi-site study of norovirus molecular epidemiology in Australia and New Zealand, 2013–2014. PLoS ONE 2016, 11, e0145254. [Google Scholar] [CrossRef] [PubMed]
- Ahmed, S.M.; Hall, A.J.; Robinson, A.E.; Verhoef, L.; Premkumar, P.; Parashar, U.D.; Koopmans, M.; Lopman, B.A. Global prevalence of norovirus in cases of gastroenteritis: A systematic review and meta-analysis. Lancet Infect. Dis. 2014, 14, 725–730. [Google Scholar] [CrossRef]
- Havelaar, A.H.; Kirk, M.D.; Torgerson, P.R.; Gibb, H.J.; Hald, T.; Lake, R.J.; Praet, N.; Bellinger, D.C.; De Silva, N.R.; Gargouri, N. World Health Organization global estimates and regional comparisons of the burden of foodborne disease in 2010. PLoS Med. 2015, 12, e1001923. [Google Scholar] [CrossRef] [PubMed]
- Torgerson, P.R.; Devleesschauwer, B.; Praet, N.; Speybroeck, N.; Willingham, A.L.; Kasuga, F.; Rokni, M.B.; Zhou, X.N.; Fèvre, E.M.; Sripa, B. World Health Organization estimates of the global and regional disease burden of 11 foodborne parasitic diseases, 2010: A data synthesis. PLoS Med. 2015, 12, e1001920. [Google Scholar] [CrossRef]
- Costafreda, M.I.; Bosch, A.; Pinto, R.M. Development, evaluation, and standardization of a real-time TaqMan reverse transcription-PCR assay for quantification of hepatitis A virus in clinical and shellfish samples. Appl. Environ. Microbiol. 2006, 72, 3846–3855. [Google Scholar] [CrossRef] [PubMed]
- Le Guyader, F.S.; Bon, F.; DeMedici, D.; Parnaudeau, S.; Bertone, A.; Crudeli, S.; Doyle, A.; Zidane, M.; Suffredini, E.; Kohli, E.; et al. Detection of multiple noroviruses associated with an international gastroenteritis outbreak linked to oyster consumption. J. Clin. Microbiol. 2006, 44, 3878–3882. [Google Scholar] [CrossRef]
- Nishida, T.; Nishio, O.; Kato, M.; Chuma, T.; Kato, H.; Iwata, H.; Kimura, H. Genotyping and quantitation of noroviruses in oysters from two distinct sea areas in Japan. Microbiol. Immunol. 2007, 51, 177–184. [Google Scholar] [CrossRef]
- Le Guyader, F.; Parnaudeau, S.; Schaeffer, J.; Bosch, A.; Loisy, F.; Pommepuy, M.; Atmar, R.L. Detection and quantification of noroviruses in shellfish. Appl. Environ. Microbiol. 2009, 75, 618–624. [Google Scholar] [CrossRef]
- Kingsley, D.H.; Richards, G.P. Rapid and efficient extraction method for reverse transcription-PCR detection of hepatitis A and Norwalk-like viruses in shellfish. Appl. Environ. Microbiol. 2001, 67, 4152–4157. [Google Scholar] [CrossRef] [PubMed]
- Jothikumar, N.; Lowther, J.A.; Henshilwood, K.; Lees, D.N.; Hill, V.R.; Vinje, J. Rapid and sensitive detection of noroviruses by using TaqMan-based one-step reverse transcription-PCR assays and application to naturally contaminated shellfish samples. Appl. Environ. Microbiol. 2005, 71, 1870–1875. [Google Scholar] [CrossRef] [PubMed]
- Casas, N.; Amarita, F.; de Maranon, I.M. Evaluation of an extracting method for the detection of Hepatitis A virus in shellfish by SYBR-Green real-time RT-PCR. Int. J. Food Microbiol. 2007, 120, 179–185. [Google Scholar] [CrossRef]
- Baert, L.; Uyttendaele, M.; Debevere, J. Evaluation of two viral extraction methods for the detection of human noroviruses in shellfish with conventional and real-time reverse transcriptase PCR. Lett. Appl. Microbiol. 2007, 44, 106–111. [Google Scholar] [CrossRef]
- Sincero, T.C.M.; Levin, D.B.; Simões, C.M.O.; Barardi, C.R.M. Detection of hepatitis A virus (HAV) in oysters (Crassostrea gigas). Water Res. 2006, 40, 895–902. [Google Scholar] [CrossRef]
- Papafragkou, E.; Plante, M.; Mattison, K.; Bidawid, S.; Karthikeyan, K.; Farber, J.M.; Jaykus, L.A. Rapid and sensitive detection of hepatitis A virus in representative food matrices. J. Virol. Methods 2008, 147, 177–187. [Google Scholar] [CrossRef] [PubMed]
- Kittigul, L.; Singhaboot, Y.; Chavalitshewinkoon-Petmitr, P.; Pombubpa, K.; Hirunpetcharat, C. A comparison of virus concentration methods for molecular detection and characterization of rotavirus in bivalve shellfish species. Food Microbiol. 2015, 46, 161–167. [Google Scholar] [CrossRef]
- Uhrbrand, K.; Myrmel, M.; Maunula, L.; Vainio, K.; Trebbien, R.; Nørrung, B.; Schultz, A.C. Evaluation of a rapid method for recovery of norovirus and hepatitis A virus from oysters and blue mussels. J. Virol. Methods 2010, 169, 70–78. [Google Scholar] [CrossRef]
- David, S.T.; McIntyre, L.; MacDougall, L.; Kelly, D.; Liem, S.; Schallie, K.; McNabb, A.; Houde, A.; Mueller, P.; Ward, P.; et al. An outbreak of norovirus caused by consumption of oysters from geographically dispersed harvest sites, British Columbia, Canada, 2004. Foodborne Pathog. Dis. 2007, 4, 349–358. [Google Scholar] [CrossRef]
- Comelli, H.L.; Rimstad, E.; Larsen, S.; Myrmel, M. Detection of norovirus genotype I.3b and II.4 in bioaccumulated blue mussels using different virus recovery methods. Int. J. Food Microbiol. 2008, 127, 53–59. [Google Scholar] [CrossRef]
- Lees, D. International standardisation of a method for detection of human pathogenic viruses in molluscan shellfish. Food Environ. Virol. 2010, 2, 146–155. [Google Scholar] [CrossRef]
- ISO. Microbiology of the Food Chain—Horizontal Method for Determination of Hepatitis A Virus and Norovirus in Food Using Real-Time RT-PCR—Part-1: Method for Quantification; ISO 15216-1:2017; International Organization for Standardization: Geneva, Switzerland, 2017. [Google Scholar]
- Boxman, I.L.A.; Tilburg, J.J.H.C.; Te Loeke, N.A.J.M.; Vennema, H.; Jonker, K.; de Boer, E.; Koopmans, M. Detection of noroviruses in shellfish in the Netherlands. Int. J. Food Microbiol. 2006, 108, 391–396. [Google Scholar] [CrossRef]
- De Roda Husman, A.M.; Lodder-Verschoor, F.; van den Berg, H.H.J.L.; Le Guyader, F.S.; Van Pelt, H.; van der Poel, W.H.M.; Rutjes, S.A. Rapid virus detection procedure for molecular tracing of shellfish associated with disease outbreaks. J. Food Prot. 2007, 70, 967–974. [Google Scholar] [CrossRef] [PubMed]
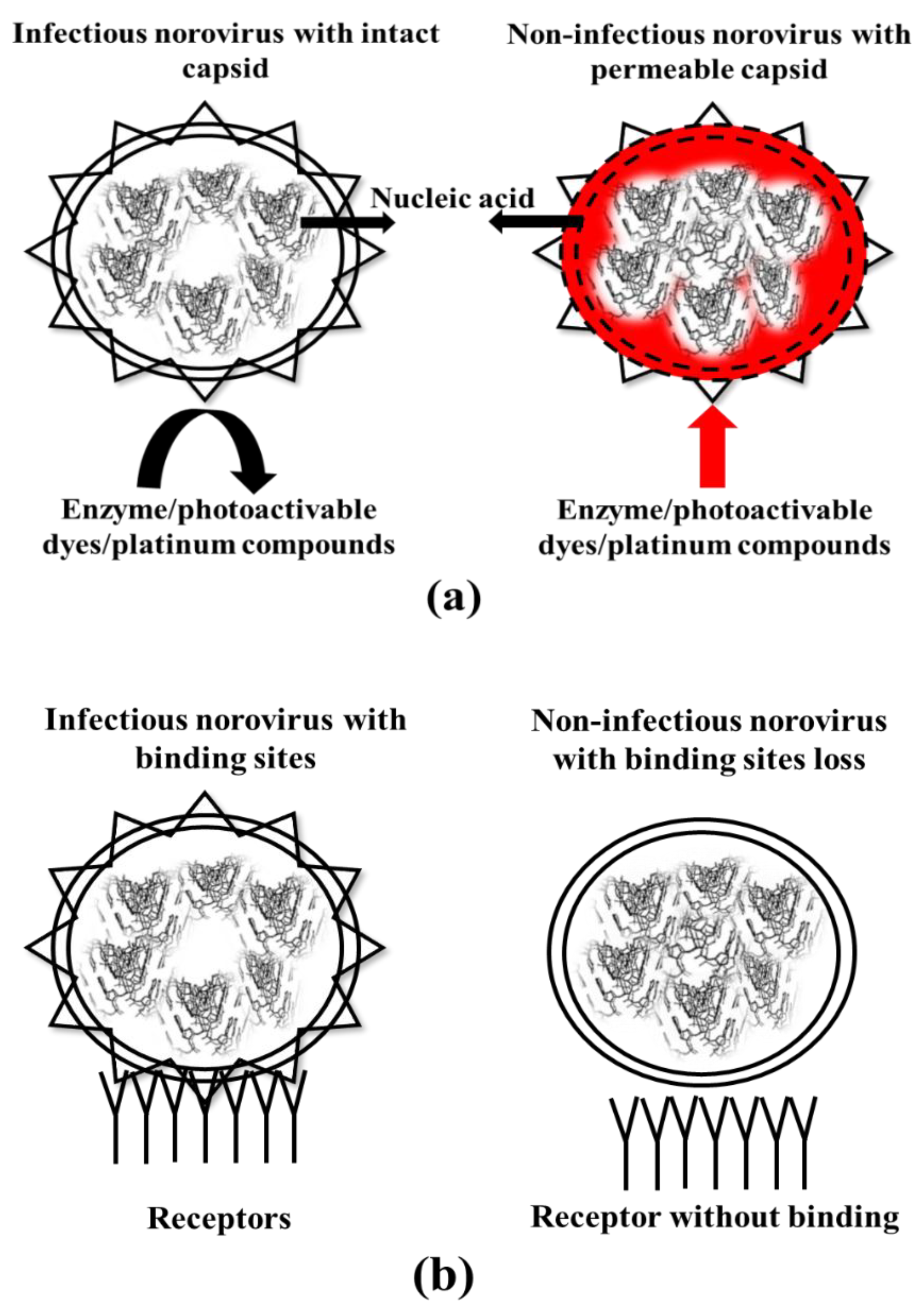
- Nuanualsuwan, S.; Cliver, D.O. Pre-treatment to avoid positive RT-PCR results with inactivated viruses. J. Virol. Methods 2002, 104, 217–225. [Google Scholar] [CrossRef]
- Lowther, J.A.; Bosch, A.; Butot, S.; Ollivier, J.; Made, D.; Rutjes, S.A.; Hardouin, G.; Lombard, B.; in’t Veld, P.; Leclercq, A. Validation of EN ISO method 15216-Part 1-quantification of hepatitis A virus and norovirus in food matrices. Int. J. Food Microbiol. 2019, 288, 82–90. [Google Scholar] [CrossRef] [PubMed]
- Langlet, J.; Kaas, L.; Croucher, D.; Hewitt, J. Effect of the shellfish proteinase K digestion method on norovirus capsid integrity. Food Environ. Virol. 2018, 10, 151–158. [Google Scholar] [CrossRef]
- Cromeans, T.L.; Nainan, O.V.; Margolis, H.S. Detection of hepatitis A virus RNA in oyster meat. Appl. Environ. Microbiol. 1997, 63, 2460–2463. [Google Scholar] [PubMed]
- Lowther, J.A.; Gustar, N.E.; Powell, A.L.; Hartnell, R.E.; Lees, D.N. Two-year systematic study to assess norovirus contamination in oysters from commercial harvesting areas in the United Kingdom. Appl. Environ. Microbiol. 2012, 78, 5812–5817. [Google Scholar] [CrossRef] [PubMed]
- Nishida, T.; Kimura, H.; Saitoh, M.; Kozawa, K.; Kato, M.; Shinohara, M.; Fukuda, S.; Munemura, T.; Mikami, T.; Kawamoto, A.; et al. Detection quantitation, and phylogenetic analysis of noroviruses in Japanese oysters. Appl. Environ. Microbiol. 2003, 69, 5782–5786. [Google Scholar] [CrossRef]
- Li, D.; Stals, A.; Tang, Q.J.; Uyttendaele, M. Detection of norovirus in shellfish and semi-processes fishery products from a Belgian seafood company. J. Food Prot. 2014, 77, 1342–1347. [Google Scholar] [CrossRef]
- Persson, S.; Eriksson, R.; Lowther, J.; Ellstrom, P.; Simonsson, M. Comparison between RT droplet digital PCR and RT real-time PCR for quantification of noroviruses in oysters. Int. J. Food Microbiol. 2018, 284, 73–83. [Google Scholar] [CrossRef] [PubMed]
- Polo, D.; Schaeffer, J.; Fournet, N.; Le Saux, J.C.; Parnaudeau, S.; McLeod, C.; Le Guyader, F.S. Digital PCR for quantifying norovirus in oysters implicated in outbreaks, France. Emerg. Infect. Dis. 2016, 22, 2189–2191. [Google Scholar] [CrossRef] [PubMed]
- Pinheiro, L.B.; Coleman, V.A.; Hindson, C.M.; Herrmann, J.; Hindson, B.J.; Bhat, S.; Emslie, K.R. Evaluation of a droplet digital polymerase chain reaction format for DNA copy number quantification. Anal. Chem. 2012, 84, 1003–1011. [Google Scholar] [CrossRef] [PubMed]
- Jeon, S.B.; Seo, D.J.; Oh, H.; Kingsley, D.H.; Choi, C. Development of one-step reverse transcription loop-mediated isothermal amplification for norovirus detection in oysters. Food Cont. 2017, 73, 1002–1009. [Google Scholar] [CrossRef]
- Fukuda, S.; Sasaki, Y.; Seno, M. Rapid and sensitive detection of norovirus genomes in oysters by a two-step isothermal amplification assay system combining nucleic acid sequences-based amplification and revers transcription-loop-mediated isothermal amplification assays. Appl. Environ. Microbiol. 2008, 74, 3912–3914. [Google Scholar] [CrossRef] [PubMed]
- Topping, J.R.; Schnerra, H.; Hainesa, J.; Scott, M.; Carter, M.J.; Willcocks, M.M.; Bellamy, K.; Brown, D.W.; Gray, J.J.; Gallimore, C.I.; et al. Temperature inactivation of feline calicivirus vaccine strain FCV F-9 in comparison with human noroviruses using an RNA exposure assay and reverse transcribed quantitative real-time polymerase chain reaction-A novel method for predicting virus infectivity. J. Virol. Methods 2009, 156, 89–95. [Google Scholar] [CrossRef]
- Mormann, S.; Dabisch, M.; Becker, B. Effects of technological processes on the tenacity and inactivation of norovirus genogroup II in experimentally contaminated foods. Appl. Environ. Microbiol. 2010, 76, 536–545. [Google Scholar] [CrossRef]
- Nowak, P.; Topping, J.R.; Fotheringham, V.; Gallimore, C.I.; Gray, J.J.; Iturriza-Gomara, M.; Knight, A.L. Measurement of the virolysis of Human GII.4 norovirus in response to disinfectants and sanitisers. J. Virol. Methods 2011, 174, 7–11. [Google Scholar] [CrossRef]
- Diez-Valcarce, M.; Kovac, K.; Raspor, P.; Rodriguez-Lazaro, D.; Hernandez, M. Virus genome quantification does not predict norovirus infectivity after application of food inactivation processing technologies. Food Environ. Virol. 2011, 3, 141–146. [Google Scholar] [CrossRef]
- Ronnqvist, M.; Mikkela, A.; Tuominen, P.; Salo, S.; Maunula, L. Ultraviolet light inactivation of murine norovirus and human norovirus GII: PCR may overestimate the persistence of noroviruses even when combined with pre-PCR treatment. Food Environ. Virol. 2014, 6, 48–57. [Google Scholar] [CrossRef]
- Gyawali, P.; Hewitt, J. Detection of infectious norovirus from wastewater and seawater using PEMAXTM treatment combined with RT-qPCR. Water 2018, 10, 841. [Google Scholar] [CrossRef]
- Randazzo, W.; Khezri, M.; Ollivier, J.; Le Guyader, F.C.; Rodríguez-Díaz, J.; Aznar, R.; Sánchez, G. Optimization of PMAxx pretreatment to distinguish between human norovirus with intact and altered capsids in shellfish and sewage samples. Int. J. Food Microbiol. 2018, 266, 1–7. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Karim, M.R.; Fout, G.S.; Johnson, C.H.; White, K.M.; Parshionikar, S.U. Propidium monoazide reverse transcriptase PCR and RT-qPCR for detecting infectious enterovirus and norovirus. J. Virol. Methods 2015, 219, 51–61. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Leifels, M.; Jurzik, L.; Wilhelm, M.; Hamza, I.A. Use of ethidium monoazide and propidium monoazide to determine viral infectivity upon inactivation by heat, UV-exposure and chlorine. Int. J. Hyg. Environ. Health 2015, 218, 686–693. [Google Scholar] [CrossRef]
- Li, X.; Huang, R.; Chen, H. Evaluation of assays to quantify infectious human norovirus for heat and high-pressure inactivation studies using Tulane virus. Food Environ. Virol. 2017, 9, 314–325. [Google Scholar] [CrossRef] [PubMed]
- Fraisse, A.; Niveau, F.; Hennechart-Collette, C.; Coudray-Meunier, C.; Martin-Latil, S.; Perelle, S. Discrimination of infectious and heat-treated norovirus by combining platinum compounds and real-time RT-PCR. Int. J. Food Microbiol. 2018, 269, 64–74. [Google Scholar] [CrossRef]
- Li, X.; Chen, H. Evaluation of the porcine gastric mucin binding assay for high pressure- inactivation studies using murine norovirus and Tulane virus. Appl. Environ. Microbiol. 2015, 81, 515–521. [Google Scholar] [CrossRef]
- Dancho, B.A.; Chen, H.; Kingsley, D.H. Discrimination between infectious and non-infectious human norovirus using porcine gastric mucin. Int. J. Food Microbiol. 2012, 155, 222–226. [Google Scholar] [CrossRef]
- Tian, P.; Engelbrektson, A.; Mandrell, R. Two-log increase in sensitivity for detection of norovirus in complex samples by concentration with porcine gastric mucin conjugated to magnetic beads. Appl. Environ. Microbiol. 2008, 74, 4271–4276. [Google Scholar] [CrossRef] [PubMed]
- Li, D.; Baert, L.; Van Coillie, E.; Uyttendaele, M. Critical studies on binding-based RT-PCR detection of infectious noroviruses. J. Virol. Methods 2011, 177, 153–159. [Google Scholar] [CrossRef] [PubMed]
- Tian, P.; Yang, D.; Shan, L.; Li, Q.; Liu, D.; Wang, D. Estimation of human norovirus infectivity from environmental water samples by in situ capture RT-qPCR method. Food Environ. Virol. 2018, 10, 29–38. [Google Scholar] [CrossRef]
- Wang, D.; Xu, S.; Yang, D.; Young, G.M.; Tian, P. New in situ capture quantitative (real-time) reverse transcription-PCR method as an alternative approach for determining inactivation of Tulane virus. Appl. Environ. Microbiol. 2014, 80, 2120–2124. [Google Scholar]
- Wang, D.; Tian, P. Inactivation conditions for human norovirus measured by an in situ capture-qRT-PCR method. Int. J. Food Microbiol. 2014, 172, 76–82. [Google Scholar] [CrossRef] [PubMed]
- Cannon, J.L.; Vinje, J. Histo-blood group antigen assay for detecting noroviruses in water. Appl. Environ. Microbiol. 2008, 78, 6818–6819. [Google Scholar] [CrossRef]
- Morton, V.; Jean, J.; Farber, J.; Mattison, K. Detection of norovirus in ready to eat foods using carbohydrate-coated magnetic beads. Appl. Environmen. Microbiol. 2009, 75, 4641–4643. [Google Scholar] [CrossRef] [PubMed]
- Zhou, Z.; Tian, Z.; Li, Q.; Tian, P.; Wu, Q.; Wang, D.; Shi, X. In situ capture RT-qPCR: A new simple and sensitive method to detect human norovirus in oysters. Front. Microbiol. 2017, 8, e554. [Google Scholar] [CrossRef]
- Manuel, C.S.; Moore, M.D.; Jaykus, L.A. Predicting human norovirus infectivity-Recent advancement and continued challenges. Food Microbiol. 2018, 76, 337–345. [Google Scholar] [CrossRef]
- Bergholz, T.M.; Moreno Switt, A.I.; Wiedmann, M. Omics approaches in food safety: Fulfilling the promise? Trends Microbiol. 2014, 22, 275–281. [Google Scholar] [CrossRef] [PubMed]
- Ellis, D.I.; Muhamadali, H.; Chisanga, M.; Goodacre, R. Omics methods for the detection of foodborne pathogens. In Encyclopedia of Food Chemistry; Melton, L., Shahidi, F., Varelis, P., Eds.; Academic Press: Oxford, UK, 2019; pp. 364–370. [Google Scholar]
- Liu, D.; Zhang, Z.; Yin, Y.; Jia, F.; Wu, Q.; Tian, P.; Wang, D. Development and evaluation of a novel in situ target-capture approach for aptamer selection of human noroviruses. Talanta 2019, 193, 199–205. [Google Scholar] [CrossRef]
- Zarei, M. Advance in point of care technologies for molecular diagnostics. Biosens. Bioelectron. 2017, 98, 494–506. [Google Scholar] [CrossRef]
- Ashiba, H.; Sugiyama, Y.; Wang, X.; Shirato, H.; Higo-Moriguchi, K.; Taniguchi, K.; Ohki, Y.; Fujimaki, M. Detection of norovirus virus-like particles using a surface plasmon resonance-assisted fluoroimmunosensor optimized for quantum dot fluorescent labels. Biosens. Bioelectron. 2017, 93, 260–266. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Neethirajan, S.; Ahmed, S.R.; Chand, R.; Buozis, J.; Nagy, E. Recent advances in biosensor development for foodborne viruse detection. Nanotheranostics 2017, 1, 272–295. [Google Scholar] [CrossRef] [PubMed]
- Weng, W.; Neethirajan, S. Aptamer-based fluorometric determination of norovirus using a paper-based microfluidic device. Microchim. Acta 2017, 184, 4545–4552. [Google Scholar] [CrossRef]
- Gong, H.; Woolley, A.T.; Nordin, G.P. 3D printed high density, reversible, chip to chip microfluidic interconnections. Lab Chip 2018, 18, 639–647. [Google Scholar] [CrossRef]
- Nooij, S.; Schmitz, D.; Vennema, H.; Kroneman, A.; Koopmans, M.P.G. Overview of virus metagenomics classification methods and their biological applications. Front. Microbiol. 2018, 9, e749. [Google Scholar] [CrossRef] [PubMed]
- Mokili, J.L.; Rohwer, F.; Dutilh, B.E. Metagenomics and future perspectives in virus discovery. Curr. Opin. Virol. 2012, 2, 63–77. [Google Scholar] [CrossRef]
- Miller, R.R.; Montoya, V.; Gardy, J.L.; Patrick, D.M.; Tang, P. Metagenomics for pathogen detection in public health. Genome Med. 2013, 5, e81. [Google Scholar] [CrossRef]
- Iritani, N.; Kaida, A.; Abe, N.; Kubo, H.; Sekiguchi, J.; Yamamoto, S.P.; Goto, K.; Tanaka, T.; Noda, M. Detection and genetic characterization of human enteric viruses in oyster-associated gastroenteritis outbreaks between 2001 and 2012 in Osaka City, Japan. J. Med. Virol. 2014, 86, 2019–2025. [Google Scholar] [CrossRef]
- Fratamico, P.; Gunther, N.W. 24 Advances in genomics and proteomics-based methods for the study of foodborne bacterial pathogens. In Advances in Microbial Food Safety; Sofos, J., Ed.; Woodhead Publishing: Cambridge, UK, 2013; pp. 462–497. [Google Scholar]
- Xu, Y.J. Foodomics: A novel approach for food microbiology. TrAC Trends Analyt. Chem. 2017, 96, 14–21. [Google Scholar] [CrossRef]
- Singhal, N.; Kumar, M.; Kanaujia, P.K.; Virdi, J.S. MALDI-TOF mass spectrometry: An emerging technology for microbial identification and diagnosis. Front. Microbiol. 2015, 6, e791. [Google Scholar] [CrossRef]
- Ortea, I.; O’Connor, G.; Maquet, A. Review on proteomics for food authentication. J. Proteomics 2016, 147, 212–225. [Google Scholar] [CrossRef] [PubMed]
- Vithanage, N.R.; Yeager, T.R.; Jadhav, S.R.; Palombo, E.A.; Datta, N. Comparison of identification systems for psychrotrophic bacteria isolated from raw bovine milk. Int. J. Food Microbiol. 2014, 189, 26–38. [Google Scholar] [CrossRef]
- Vithanage, N.R.; Bhongir, J.; Jadhav, S.R.; Ranadheera, C.S.; Palombo, E.A.; Yeager, T.R.; Datta, N. Species-level discrimination of psychrotrophic pathogenic and spoilage gram-negative raw milk isolates using a combined MALDI-TOF MS proteomics-bioinformatics-based approach. J. Proteome Res. 2017, 16, 2188–2203. [Google Scholar] [CrossRef]
- Jadhav, S.; Gulati, V.; Fox, E.M.; Karpe, A.; Beale, D.J.; Sevior, D.; Bhave, M.; Palombo, E.A. Rapid identification and source-tracking of Listeria monocytogenes using MALDI-TOF mass spectrometry. Int. J. Food Microbiol. 2015, 202, 1–9. [Google Scholar] [CrossRef]
- Carrera, M.; Cañas, B.; Gallardo, J.M. Advanced proteomics and systems biology applied to study food allergy. Curr. Opin. Food Sci. 2018, 22, 9–16. [Google Scholar] [CrossRef] [Green Version]
- Nugraha, R.; Kamath, S.D.; Johnston, E.; Zenger, K.R.; Rolland, J.M.; O’Hehir, R.E.; Lopata, A.L. Rapid and comprehensive discovery of unreported shellfish allergens using large-scale transcriptomic and proteomic resources. J. Allergy Clin. Immunol. 2018, 141, 1501–1504. [Google Scholar] [CrossRef] [PubMed]
- Ruethers, T.; Taki, A.C.; Johnston, E.B.; Nugraha, R.; Le, T.T.K.; Kalic, T.; McLean, T.R.; Kamath, S.D.; Lopata, A.L. Seafood allergy: A comprehensive review of fish and shellfish allergens. Mol. Immunol. 2018, 100, 28–57. [Google Scholar] [CrossRef]
- Kouremenos, K.A.; Johansson, M.; Marriott, P.J. Advances in gas chromatographic methods for the identification of biomarkers in cancer. J. Cancer 2012, 3, 404–420. [Google Scholar] [CrossRef]
- Hall, R.D.; de Maagd, R.A. Plant metabolomics is not ripe for environmental risk assessment. Trends Biotechnol. 2014, 32, 391–392. [Google Scholar] [CrossRef]
- Lima, M.R.M.; Diaz, S.O.; Lamego, I.; Grusak, M.A.; Vasconcelos, M.W.; Gil, A.M. Nuclear magnetic resonance metabolomics of iron deficiency in soybean leaves. J. Proteome Res. 2014, 13, 3075–3087. [Google Scholar] [CrossRef]
- Hines, A.; Staff, F.J.; Widdows, J.; Compton, R.M.; Falciani, F.; Viant, M.R. Discovery of metabolic signatures for predicting whole organism toxicology. Toxicol. Sci. 2010, 115, 369–378. [Google Scholar] [CrossRef]
- Cevallos-Cevallos, J.M.; Danyluk, M.D.; Reyes-De-Corcuera, J.I. GC-MS based metabolomics for rapid simultaneous detection of Escherichia coli O157:H7, Salmonella Typhimurium, Salmonella Muenchen, and Salmonella Hartford in ground beef and chicken. J. Food Sci. 2011, 76, 238–246. [Google Scholar] [CrossRef]
- Singh, A.K.; Ulanov, A.V.; Li, Z.; Jayaswal, R.K.; Wilkinson, B.J. Metabolomes of the psychrotolerant bacterium Listeria monocytogenes 10403S grown at 37 °C and 8 °C. Int. J. Food Microbiol. 2011, 148, 107–114. [Google Scholar] [CrossRef]
- Beale, D.J.; Morrison, P.D.; Palombo, E.A. Detection of listeria in milk using non-targeted metabolic profiling of Listeria monocytogenes: A proof-of-concept application. Food Control. 2014, 42, 343–346. [Google Scholar] [CrossRef]
- Pinu, F.R. Metabolomics-The new frontier in food safety and quality research. Food Res. Int. 2015, 72, 80–81. [Google Scholar] [CrossRef]
- Pinu, F.R. Early detection of food pathogens and food spoilage microorganisms: Application of metabolomics. Trends Food Sci. Technol. 2016, 54, 213–215. [Google Scholar] [CrossRef]
- Castro-Puyana, M.; Pérez-Míguez, R.; Montero, L.; Herrero, M. Application of mass spectrometry-based metabolomics approaches for food safety, quality and traceability. TrAC Trends Anal. Chem. 2017, 93, 102–118. [Google Scholar] [CrossRef] [Green Version]
- Aru, V.; Pisano, M.B.; Savorani, F.; Engelsen, S.B.; Cosentino, S.; Cesare Marincola, F. Metabolomics analysis of shucked mussels’ freshness. Food Chem. 2016, 205, 58–65. [Google Scholar] [CrossRef]
- Alfaro, A.C.; Nguyen, T.V.; Mellow, D. A metabolomics approach to assess the effect of storage conditions on metabolic processes of New Zealand surf clam (Crassula aequilatera). Aquaculture 2019, 498, 315–321. [Google Scholar] [CrossRef]
- Nguyen, T.V.; Alfaro, A.C.; Young, T.; Merien, F. Tissue-specific immune responses to Vibrio sp. infection in mussels (Perna canaliculus): A metabolomics approach. Aquaculture 2019, 500, 118–125. [Google Scholar] [CrossRef]
- Eguchi, A.; Nomiyama, K.; Sakurai, K.; Kim Trang, P.T.; Viet, P.H.; Takahashi, S.; Iwata, H.; Tanabe, S.; Todaka, E.; Mori, C. Alterations in urinary metabolomic profiles due to lead exposure from a lead–acid battery recycling site. Environ. Pollut. 2018, 242, 98–105. [Google Scholar] [CrossRef]
- Jiang, Z.; Wang, X.; Rastrick, S.P.S.; Fang, J.; Du, M.; Gao, Y.; Li, F.; Strand, Ø.; Fang, J. Metabolic responses to elevated pCO2 in the gills of the Pacific oyster (Crassostrea gigas) using a GC-TOF-MS-based metabolomics approach. Comp. Biochem. Physiol. 2019, 29, 330–338. [Google Scholar] [CrossRef] [PubMed]
- Rosilo, H.; McKee, J.R.; Kontturi, E.; Koho, T.; Hytönen, V.P.; Ikkala, O.; Kostiainen, M.A. Cationic polymer brush-modified cellulose nanocrystals for high-affinity virus binding. Nanoscale 2014, 6, 11871–11881. [Google Scholar] [CrossRef] [PubMed]
- Junesch, J.; Emilsson, G.; Xiong, K.; Kumar, S.; Sannomiya, T.; Pace, H.; Vörös, J.; Oh, S.H.; Bally, M.; Dahlin, A.B. Location-specific nanoplasmonic sensing of biomolecular binding to lipid membranes with negative curvature. Nanoscale 2015, 7, 15080–15085. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ahmed, S.R.; Takemeura, K.; Li, T.C.; Kitamoto, N.; Tanaka, T.; Suzuki, T.; Park, E.Y. Size-controlled preparation of peroxidase-like graphene-gold nanoparticle hybrids for the visible detection of norovirus-like particles. Biosens. Bioelectron. 2017, 87, 558–565. [Google Scholar] [CrossRef]
- Moore, M.D.; Escudero-Abarca, B.I.; Suh, S.H.; Jaykus, L.A. Generation and characterization of nucleic acid aptamers targeting the capsid P domain of a human norovirus GII.4 strain. J. Biotechnol. 2015, 209, 41–49. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Moore, M.D.; Bobay, B.G.; Mertens, B.; Jaykus, L.A. Human norovirus aptamer exhibits high degree of target conformation-dependent binding similar to that of receptors and discriminates particle functionality. mSphere 2016, 1, e00298. [Google Scholar] [CrossRef] [PubMed]
- Giamberardino, A.; Labib, M.; Hassan, E.M.; Tetro, J.A.; Springthorpe, S.; Sattar, S.A.; Berezovski, M.V.; DeRosa, M.C. Ultrasensitive norovirus detection using DNA aptasensor technology. PLoS ONE 2013, 8, e79087. [Google Scholar] [CrossRef]
- Escudero-Abarca, B.I.; Suh, S.H.; Moore, M.D.; Dwivedi, H.P.; Jaykus, L.A. Selection, characterization and application of nucleic acid aptamers for the capture and detection of human norovirus strains. PLoS ONE 2014, 9, e106805. [Google Scholar] [CrossRef]
- Wang, N.; Kitajima, M.; Mani, K.; Kanhere, E.; Whittle, A.J.; Triantafyllou, M.S.; Miao, J. Miniaturized electrochemical sensor modified with aptamers for rapid norovirus detection. In Proceedings of the 11th Annual IEEE International Conference on Nano/Micro Engineered and Molecular Systems (IEEE-NEMS 2016), Matsushima Bay and Sendai MEMS City, Japan, 17–20 April 2016; pp. 587–590. [Google Scholar]
- Marín, M.J.; Rashid, A.; Rejzek, M.; Fairhurst, S.A.; Wharton, S.A.; Martin, S.R.; McCauley, J.W.; Wileman, T.; Field, R.A.; Russell, D.A. Glyconanoparticles for the plasmonic detection and discrimination between human and avian influenza virus. Org. Biomol. Chem. 2013, 11, 7101–7107. [Google Scholar] [CrossRef]
- Velusamy, V.; Arshak, K.; Korostynska, O.; Oliwa, K.; Adley, C. An overview of foodborne pathogen detection: In the perspective of biosensors. Biotechnol. Adv. 2010, 28, 232–254. [Google Scholar] [CrossRef] [PubMed]
- Hong, S.A.; Kwon, J.; Kim, D.; Yang, S. A rapid, sensitive and selective electrochemical biosensor with concanavalin A for the preemptive detection of norovirus. Biosens. Bioelectron. 2015, 64, 338–344. [Google Scholar] [CrossRef]
- Nakatsuka, K.; Shigeto, H.; Kuroda, A.; Funabashi, H. A split G-quadruplex-based DNA nano-tweezers structure as a signal-transducing molecule for the homogeneous detection of specific nucleic acids. Biosens. Bioelectron. 2015, 74, 222–226. [Google Scholar] [CrossRef] [PubMed]
- Adegoke, O.; Seo, M.W.; Kato, T.; Kawahito, S.; Park, E.Y. An ultrasensitive SiO2-encapsulated alloyed CdZnSeS quantum dot-molecular beacon nanobiosensor for norovirus. Biosens. Bioelectron. 2016, 86, 135–142. [Google Scholar] [CrossRef] [Green Version]
- Hwang, H.J.; Ryu, M.Y.; Park, C.Y.; Ahn, J.; Park, H.G.; Choi, C.; Ha, S.D.; Park, T.J.; Park, J.P. High sensitivity and selective electrochemical biosensor: Label-free detection of human norovirus using affinity peptide as molecular binder. Biosens. Bioelectron. 2017, 87, 164–170. [Google Scholar] [CrossRef] [PubMed]
- Gervais, L.; de Rooij, N.; Delamarche, E. Microfluidic chips for point-of-care immunodiagnostics. Adv. Mater. 2011, 23, H151–H176. [Google Scholar] [CrossRef] [PubMed]
- Connelly, J.T.; Kondapalli, S.; Skoupi, M.; Parker, J.S.; Kirby, B.J.; Baeumner, A.J. Micro-total analysis system for virus detection: Microfluidic pre-concentration coupled to liposome-based detection. Anal. Bioanal. Chem. 2012, 402, 315–323. [Google Scholar] [CrossRef]
- Tao, Y.; Rotem, A.; Zhang, H.; Chang, C.B.; Basu, A.; Kolawole, A.O.; Koehler, S.A.; Ren, Y.; Lin, J.S.; Pipas, J.M.; et al. Rapid, targeted and culture-free viral infectivity assay in drop-based microfluidics. Lab Chip 2015, 15, 3934–3940. [Google Scholar] [CrossRef] [PubMed]
- Chung, S.H.; Baek, C.; Cong, V.T.; Min, J. The microfluidic chip module for the detection of murine norovirus in oysters using charge switchable micro-bead beating. Biosens. Bioelectron. 2015, 67, 625–633. [Google Scholar] [CrossRef] [PubMed]
- Li, X.; Ballerini, D.R.; Shen, W. A perspective on paper-based microfluidics: Current status and future trends. Biomicrofluidics 2012, 6, 11301. [Google Scholar] [CrossRef]
- Zhang, H.; Cockrell, S.K.; Kolawole, A.O.; Rotem, A.; Serohijos, A.W.; Chang, C.B.; Tao, Y.; Mehoke, T.S.; Han, Y.; Lin, J.S.; et al. Isolation and analysis of rare norovirus recombinants from coinfected mice using drop-based microfluidics. J. Virol. 2015, 89, 7722–7734. [Google Scholar] [CrossRef]
- Ishii, S.; Kitamura, G.; Segawa, T.; Kobayashi, A.; Miura, T.; Sano, D.; Okabe, S. Microfluidic quantitative PCR for simultaneous quantification of multiple viruses in environmental water samples. Appl. Environ. Microbiol. 2014, 80, 7505–7511. [Google Scholar] [CrossRef] [PubMed]
- Ettayebi, K.; Crawford, S.E.; Murakami, K.; Broughman, J.R.; Karandikar, U.; Tenge, V.R.; Neill, F.H.; Blutt, S.E.; Zeng, X.L.; Qu, L.; et al. Replication of human noroviruses in stem cell-derived human enteroids. Science 2016, 353, 1387–1393. [Google Scholar] [CrossRef] [PubMed]
- Costantini, V.; Morantz, E.K.; Browne, H.; Ettayebi, K.; Zeng, X.L.; Atmar, R.L.; Estes, M.K.; Vinje, J. Human norovirus replication in human intestinal enteroids as model to evaluate virus inactivation. Emerg. Infect. Dis. 2018, 24, 1453–1464. [Google Scholar] [CrossRef] [PubMed]





| Methods | Concentration Method (Where Applicable) | Shellfish (Weight) | Viruses | Limit of Detection/Recovery Rate | References |
|---|---|---|---|---|---|
| Elution and concentration | PEG | Oysters (25 g) | Norovirus | 22 RT-PCR U | [21] |
| Mussels (2 g) | Norovirus GII | 20 RT-PCR U | [24] | ||
| Mussels (2 g) | Rotavirus | 10 RT-PCR U | [25] | ||
| Oysters (4 g) | Rotavirus | 1.39 GC/4 g | [27] | ||
| Mussels (4 g) | Rotavirus | 1.39 GC/4 g | [27] | ||
| Cockles (4 g) | Rotavirus | 1.39 GC/4 g | [27] | ||
| Mussels (1.5 g) | Mengovirus | 1.8% | [28] | ||
| Oysters (1.5 g) | Mengovirus | 1.2% | [28] | ||
| Oysters (1.5 g) | Norovirus GI | 70 RT PCR U/g | [3] | ||
| Oysters (1.5 g) | Norovirus GII | 70 RT PCR U/g | [3] | ||
| Ultracentrifuge | Oysters (25 g) | Hepatitis A virus | 9.9% | [23] | |
| Cationic separation | Oysters (5 g) | Hepatitis A virus | 20 RT-PCR U | [26] | |
| Proteinases K digestion | Not applicable | Oysters (1.5 g) | Norovirus GI | 20.5 ± 14.7% | [20] |
| Oysters (1.5 g) | Norovirus GII | 33.6 ± 5.3% | [20] | ||
| Mussels (25 g) | Norovirus GI | 3% | [30] | ||
| Mussels (25 g) | Norovirus GII | 3.5% | [30] | ||
| Oysters (3 g) | Norovirus GI | 34 GC/g | [36] | ||
| Oysters (3 g) | Norovirus GII | 53 GC/g | [36] | ||
| Oysters (3 g) | Hepatitis A virus | 198 GC/g | [36] | ||
| Direct RNA extraction | Not applicable | Oysters (0.15 g) | Norovirus | 10 RT-PCR U | [34] |
| Oysters (5–50 g) | Hepatitis A virus | 8 PFU | [38] |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gyawali, P.; KC, S.; Beale, D.J.; Hewitt, J. Current and Emerging Technologies for the Detection of Norovirus from Shellfish. Foods 2019, 8, 187. https://doi.org/10.3390/foods8060187
Gyawali P, KC S, Beale DJ, Hewitt J. Current and Emerging Technologies for the Detection of Norovirus from Shellfish. Foods. 2019; 8(6):187. https://doi.org/10.3390/foods8060187
Chicago/Turabian StyleGyawali, Pradip, Sanjaya KC, David J. Beale, and Joanne Hewitt. 2019. "Current and Emerging Technologies for the Detection of Norovirus from Shellfish" Foods 8, no. 6: 187. https://doi.org/10.3390/foods8060187







