A Systematic Review and Meta-Analysis of the Effects of Food Safety and Hygiene Training on Food Handlers
Abstract
:1. Introduction
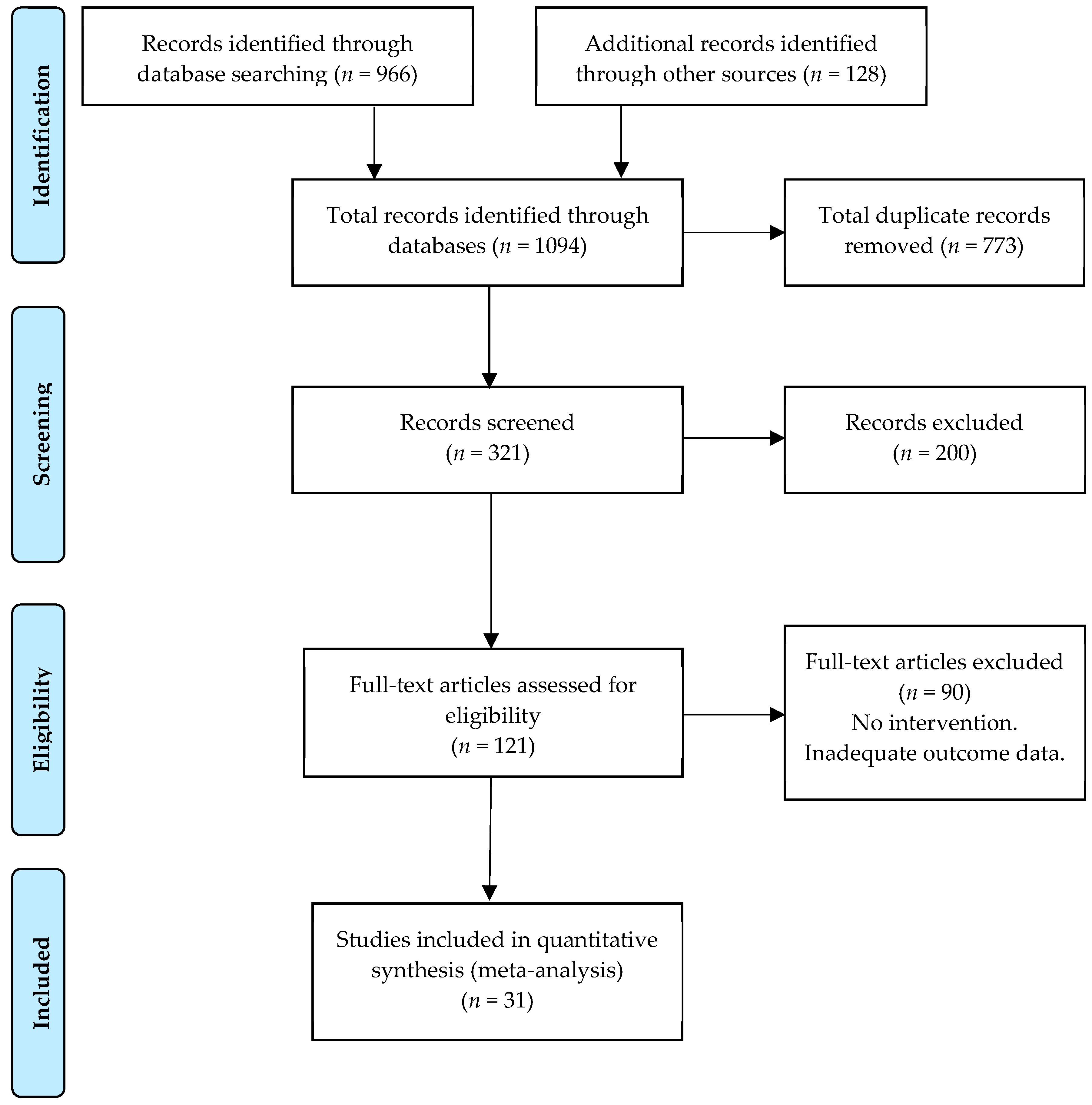
2. Materials and Methods
2.1. Search Strategy
2.2. Study Selection
2.3. Data Extraction and Quality Assessment
2.4. Data Synthesis and Analysis
3. Results
4. Discussion
4.1. Food Safety and Hygiene Training
4.2. Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Hanson, L.A.; Zahn, E.A.; Wild, S.R.; Döpfer, D.; Scott, J.; Stein, C. Estimating global mortality from potentially foodborne diseases: An analysis using vital registration data. Popul. Health Metr. 2012, 10, 5. [Google Scholar] [CrossRef] [Green Version]
- Callejón, R.M.; Rodríguez-Naranjo, M.I.; Ubeda, C.; Hornedo-Ortega, R.; Garcia-Parrilla, M.C.; Troncoso, A.M. Reported foodborne outbreaks due to fresh produce in the united states and European Union: Trends and causes. Foodborne Pathog. Dis. 2015, 12, 32–38. [Google Scholar] [CrossRef]
- Food-Borne Disease Burden Epidemiology Reference Group; World Health Organization. WHO Estimates of the Global Burden of Foodborne Diseases; World Health Organization: Geneva, Switzerland, 2015. [Google Scholar]
- Motarjemi, Y.; Käferstein, F. Food safety, Hazard Analysis and Critical Control Point and the increase in foodborne diseases: A paradox? Food Control 1999, 10, 325–333. [Google Scholar] [CrossRef]
- McIntyre, L.; Vallaster, L.; Wilcott, L.; Henderson, S.B.; Kosatsky, T. Evaluation of food safety knowledge, attitudes and self-reported hand washing practices in FOODSAFE trained and untrained food handlers in British Columbia, Canada. Food Control 2013, 30, 150–156. [Google Scholar] [CrossRef]
- Hardstaff, J.L.; Clough, H.E.; Lutje, V.; McIntyre, K.M.; Harris, J.P.; Garner, P.; O’Brien, S.J. Foodborne and Food-Handler Norovirus Outbreaks: A Systematic Review. Foodborne Pathog. Dis. 2018, 15, 589–597. [Google Scholar] [CrossRef] [Green Version]
- Lynch, M.F.; Tauxe, R.V.; Hedberg, C.W. The growing burden of foodborne outbreaks due to contaminated fresh produce: Risks and opportunities. Epidemiol. Infect. 2009, 137, 307–315. [Google Scholar] [CrossRef]
- Marcin, J.; Healthline Editorial Team; Higuera, V. Worst Foodborne Illness Outbreaks in Recent U.S. History. Available online: https://www.healthline.com/health/worst-foodborne-illness-outbreaks (accessed on 2 February 2020).
- Fenton, G.D.; Laborde, L.F.; Radhakrishna, R.B.; Brown, J.L.; Cutter, C.N. Comparison of Knowledge and Attitudes Using Computer-based and Face-to-Face Personal Hygiene Training Methods in Food Processing Facilities. J. Food Sci. Educ. 2006, 5, 45–50. [Google Scholar] [CrossRef]
- Todd, E.C.D.; Todda, E.C.D. Epidemiology of food borne diseases: A worldwide review. Rapp. Trimest. Stat. Sanit. Mond. 1997, 50, 30–50. [Google Scholar]
- Tirado, C.; Schmidt, K. WHO surveillance programme for control of foodborne infections and intoxications: Preliminary results and trends across greater Europe. J. Infect. 2001, 43, 80–84. [Google Scholar] [CrossRef]
- Cliver, D.O.; Riemann, H. Foodborne Diseases, 2nd ed.; Academic Press: San Diego, CA, USA, 2002; ISBN 0121765598. [Google Scholar]
- Shea, S.; Kubota, K.A.; Maguire, H.; Gladbach, S.; Woron, A.; Atkinson-Dunn, R.; Couturier, M.R.; Miller, M.B. Clinical microbiology laboratories’ adoption of culture-independent diagnostic tests is a threat to foodborne-disease surveillance in the United States. J. Clin. Microbiol. 2017, 55, 10–15. [Google Scholar] [CrossRef] [Green Version]
- Trienekens, J.; Zuurbier, P. Quality and safety standards in the food industry, developments and challenges. Int. J. Prod. Econ. 2008, 113, 107–122. [Google Scholar] [CrossRef]
- Varzakas, T.H.; Arvanitoyannis, I.S. Application of ISO22000 and comparison to HACCP for processing of ready to eat vegetables: Part I. Int. J. Food Sci. Technol. 2008, 43, 1729–1741. [Google Scholar] [CrossRef]
- Kotsanopoulos, K.V.; Arvanitoyannis, I.S. The Role of Auditing, Food Safety, and Food Quality Standards in the Food Industry: A Review. Compr. Rev. Food Sci. Food Saf. 2017, 16, 760–775. [Google Scholar] [CrossRef] [Green Version]
- Rossi, M.d.S.C.; Stedefeldt, E.; da Cunha, D.T.; de Rosso, V.V. Food safety knowledge, optimistic bias and risk perception among food handlers in institutional food services. Food Control 2017, 73, 681–688. [Google Scholar] [CrossRef]
- Janz, N.K.; Becker, M.H. The Health Belief Model: A Decade Later. Health Educ. Behav. 1984, 11, 1–47. [Google Scholar] [CrossRef] [Green Version]
- Becker, M.H. The Health Belief Model and Sick Role Behavior. Health Educ. Behav. 1974, 2, 409–419. [Google Scholar] [CrossRef]
- Worsfold, D.; Griffith, C.; Worsfold, P. A survey of environmental health officers’ views of food hygiene training. Br. Food J. 2004, 106, 51–64. [Google Scholar] [CrossRef]
- Mullan, B.A.; Wong, C.L. Hygienic food handling behaviours. An application of the Theory of Planned Behaviour. Appetite 2009, 52, 757–761. [Google Scholar] [CrossRef]
- Mullan, B.; Wong, C. Using the Theory of Planned Behaviour to design a food hygiene intervention. Food Control 2010, 21, 1524–1529. [Google Scholar] [CrossRef] [Green Version]
- Milton, A.C.; Mullan, B.A. An application of the theory of planned behavior—A randomized controlled food safety pilot intervention for young adults. Health Psychol. 2012, 31, 250–259. [Google Scholar] [CrossRef] [Green Version]
- Phillip, S.; Anita, E. Efficacy of the theory of planned behaviour model in predicting safe food handling practices. Food Control 2010, 21, 983–987. [Google Scholar] [CrossRef]
- Clayton, D.A.; Griffith, C.J.; Price, P.; Peters, A.C. Food handlers’ beliefs and self-reported practices. Int. J. Environ. Health Res. 2002, 12, 25–39. [Google Scholar] [CrossRef]
- Ajzen, I. From Intentions to Actions: A Theory of Planned Behavior. In Action Control; Kuhl, J., Ed.; Springer: Berlin/Heidelberg, Germany, 1985; pp. 11–39. [Google Scholar]
- Ajzen, I. The theory of planned behavior. Organ. Behav. Hum. Decis. Process. 1991, 50, 179–211. [Google Scholar] [CrossRef]
- Egan, M.B.; Raats, M.M.; Grubb, S.M.; Eves, A.; Lumbers, M.L.; Dean, M.S.; Adams, M.R. A review of food safety and food hygiene training studies in the commercial sector. Food Control 2007, 18, 1180–1190. [Google Scholar] [CrossRef]
- Ehiri, J.E.; Morris, G.P.; McEwen, J. Evaluation of a food hygiene training course in Scotland. Food Control 1997, 8, 137–147. [Google Scholar] [CrossRef]
- Seaman, P. Food hygiene training: Introducing the Food Hygiene Training Model. Food Control 2010, 21, 381–387. [Google Scholar] [CrossRef]
- Faour-Klingbeil, D.; Kuri, V.; Todd, E. Investigating a link of two different types of food business management to the food safety knowledge, attitudes and practices of food handlers in Beirut, Lebanon. Food Control 2015, 55, 166–175. [Google Scholar] [CrossRef]
- Stop TB Partnership (World Health Organization). Advocacy, Communication and Social Mobilization for TB Control A Guide to Developing Knowledge, Attitude and Practice Surveys; World Health Organization: Geneva, Switzerland, 2008. [Google Scholar]
- Hofstein, A.; Rosenfeld, S. Bridging the gap between formal and informal science learning. Stud. Sci. Educ. 1996, 28, 87–112. [Google Scholar] [CrossRef]
- Anderson, V.; Skinner, D. Organizational learning in practice: How do small businesses learn to operate internationally? Hum. Resour. Dev. Int. 1999, 2, 235–258. [Google Scholar] [CrossRef]
- Shin, C.Y.M. Speed of Internationalization, the Knowledge Link and Effects of Creativity. Ph.D. Thesis, Seoul National University, Seoul, Korea, 2020. [Google Scholar]
- Glanz, K.; Rimer, B.; Viswanath, K. Health Behaviour and Health Education: Theory Research and Practice, 4th ed.; John Wiley & Sons: San Francisco, CA, USA, 2008; Volume 4, ISBN 978-0-7879-9614-7. [Google Scholar]
- Baş, M.; Şafak Ersun, A.; Kivanç, G.; Bas, M.; Safak Ersun, A.; Kivanc, G. The evaluation of food hygiene knowledge, attitudes, and practices of food handlers’ in food businesses in Turkey. Food Control 2006, 17, 317–322. [Google Scholar] [CrossRef]
- Park, S.-H.H.; Kwak, T.-K.K.; Chang, H.-J.J. Evaluation of the food safety training for food handlers in restaurant operations. Nutr. Res. Pract. 2010, 4, 58–68. [Google Scholar] [CrossRef] [Green Version]
- Keller, J. Attitude is Everything, 1st ed.; Attitude is Everything: East Norwich, NY, USA, 1999; ISBN 978-0-9790410-3-7. [Google Scholar]
- World Health Organization. Foodborne Disease: A Focus for Health Education, 1st ed.; World Health Organization: Geneva, Switzerland, 2000; ISBN 9241561963. [Google Scholar]
- Badran, I.G. Knowledge, attitude and practice the three pillars of excellence and wisdom: A place in the medical profession. EMHJ East. Mediterr. Health J. 1995, 1, 8–16. [Google Scholar]
- Askarian, M.; Kabir, G.; Aminbaig, M.; Memish, Z.A.; Jafari, P. Knowledge, Attitudes, and Practices of Food Service Staff Regarding Food Hygiene in Shiraz, Iran. Infect. Control Hosp. Epidemiol. 2004, 25, 16–20. [Google Scholar] [CrossRef] [PubMed]
- Sharif, L.; Obaidat, M.M.; Al-Dalalah, M.-R. Food Hygiene Knowledge, Attitudes and Practices of the Food Handlers in the Military Hospitals. Food Nutr. Sci. 2013, 4, 245–251. [Google Scholar] [CrossRef] [Green Version]
- Bou-Mitri, C.; Mahmoud, D.; El Gerges, N.; Jaoude, M.A. Food safety knowledge, attitudes and practices of food handlers in lebanese hospitals: A cross-sectional study. Food Control 2018, 94, 78–84. [Google Scholar] [CrossRef]
- Nee, S.O.; Sani, N.A. Assessment of Knowledge, Attitudes and Practices (KAP) Among food handlers at residential colleges and canteen regarding food safety. Sains Malays. 2011, 40, 403–410. [Google Scholar]
- Yarrow, L.K. Food Safety Attitudes, Beliefs, Knowledge and Self-Reported Practices of College Students Before and After Educational Intervention. Ph.D. Thesis, Kansas State University, Manhattan, KS, USA, 2006. [Google Scholar]
- Booth, R.; Hernandez, M.; Baker, E.L.; Grajales, T.; Pribis, P. Food safety attitudes in college students: A structural equation modeling analysis of a conceptual model. Nutrients 2013, 5, 328–339. [Google Scholar] [CrossRef] [Green Version]
- Liu, S.; Liu, Z.; Zhang, H.; Lu, L.; Liang, J.; Huang, Q. Knowledge, attitude and practices of food safety amongst food handlers in the coastal resort of Guangdong, China. Food Control 2015, 47, 457–461. [Google Scholar] [CrossRef]
- Firdaus Siau, A.; Son, R.; Mohhiddin, O.; Toh, P.S.; Chai, L.C. Food court hygiene assessment and food safety knowledge, attitudes and practices of food handlers in Putrajaya. Int. Food Res. J. 2015, 22, 1843–1854. [Google Scholar]
- Cuprasitrut, T.; Srisorrachatr, S.; Malai, D.; Srisorrachatr, S. Food Safety Knowledge, Attitude and Practice of Food Handlers and Microbiological and Chemical Food Quality Assessment of Food for Making Merit for Monks in Ratchathewi District, Bangkok. Asia J. Public Health 2011, 22, 27–34. [Google Scholar]
- Abdul-Mutalib, N.A.; Abdul-Rashid, M.F.; Mustafa, S.; Amin-Nordin, S.; Hamat, R.A.; Osman, M. Knowledge, attitude and practices regarding food hygiene and sanitation of food handlers in Kuala Pilah, Malaysia. Food Control 2012, 27, 289–293. [Google Scholar] [CrossRef] [Green Version]
- Rosnani, A.H.; Son, R.; Mohhidin, O.; Toh, P.S.; Chai, L.C. Assessment of knowledge, attitude and practices concerning food safety among restaurant workers in Putrajaya, Malaysia. Food Sci. Qual. Manag. 2014, 32, 20–28. [Google Scholar]
- Griffith, C.J.; Jackson, L.M.; Lues, R. The food safety culture in a large South African food service complex: Perspectives on a case study. Br. Food J. 2017, 119, 729–743. [Google Scholar] [CrossRef]
- Whiley, H.; Clarke, B.; Ross, K. Knowledge and Attitudes towards Handling Eggs in the Home: An Unexplored Food Safety Issue? Int. J. Environ. Res. Public Health 2017, 14, 48. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Unusan, N. Consumer food safety knowledge and practices in the home in Turkey. Food Control 2007, 18, 45–51. [Google Scholar] [CrossRef]
- Akonor, P.T.; Akonor, M.A. Food Safety Knowledge: The Case of Domestic Food Handlers in Accra. Eur. J. Nutr. Food Safety 2013, 3, 99–111. [Google Scholar] [CrossRef]
- Young, I.; Greig, J.; Wilhelm, B.J.; Waddell, L.A. Effectiveness of food handler training and education interventions: A systematic review and meta-analysis. J. Food Prot. 2019, 82, 1714–1728. [Google Scholar] [CrossRef]
- Soon, J.M.; Baines, R.; Seaman, P. Meta-analysis of food safety training on hand hygiene knowledge and attitudes among food handlers. J. Food Prot. 2012, 75, 793–804. [Google Scholar] [CrossRef] [Green Version]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G.; Altman, D.; Antes, G.; Atkins, D.; Barbour, V.; Barrowman, N.; Berlin, J.A.; et al. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Med. 2009, 6, 195–196. [Google Scholar] [CrossRef] [Green Version]
- Liberati, A.; Altman, D.G.; Tetzlaff, J.; Mulrow, C.; Gøtzsche, P.C.; Ioannidis, J.P.A.A.; Clarke, M.; Devereaux, P.J.J.; Kleijnen, J.; Moher, D.; et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: Explanation and elaboration. PLoS Med. 2009, 6, e1000100. [Google Scholar] [CrossRef]
- McGowan, J.; Sampson, M.; Salzwedel, D.M.; Cogo, E.; Foerster, V.; Lefebvre, C. PRESS Peer Review of Electronic Search Strategies: 2015 Guideline Statement. J. Clin. Epidemiol. 2016, 75, 40–46. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Higgins, J.; Green, S. (Eds.) Cochrane Handbook for Systematic Reviews of Interventions, 5th ed.; The Cochrane Collaboration: London, UK, 2011. [Google Scholar]
- Reeves, B.; Deeks, J.; Julian, H.; Shea, B.; Tugwell, P.; Wells, G. Chapter 24: Including non-randomized studies on intervention effects. In Cochrane Handbook for Systematic Reviews of Interventions; The Cochrane Collaboration: London, UK, 2019; pp. 1–40. [Google Scholar]
- Flay, B.R.; Biglan, A.; Boruch, R.F.; Castro, F.G.; Gottfredson, D.; Kellam, S.; Mościcki, E.K.; Schinke, S.; Valentine, J.C.; Ji, P. Standards of evidence: Criteria for efficacy, effectiveness and dissemination. Prev. Sci. 2005, 6, 151–175. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rychetnik, L.; Frommer, M.; Hawe, P.; Shiell, A. Criteria for evaluating evidence on public health interventions. J. Epidemiol. Community Health 2002, 56, 119–127. [Google Scholar] [CrossRef] [PubMed]
- Young, I.; Waddell, L.; Harding, S.; Greig, J.; Mascarenhas, M.; Sivaramalingam, B.; Pham, M.T.; Papadopoulos, A. A systematic review and meta-analysis of the effectiveness of food safety education interventions for consumers in developed countries. BMC Public Health 2015, 15. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Borenstein, M.; Hedges, L.V.; Higgins, J.P.T.T.; Rothstein, H.R. Introductionto Meta-Analysis, 1st ed.; John Wiley & Sons: Chichester, UK, 2009; ISBN 0521834643. [Google Scholar]
- Cooper, H.; Hedges, L.V. Research synthesis as a scientific process. In The Handbook of Research Synthesis and Meta-Analysis; Russell Sage Foundation: New York, NY, USA, 2009; pp. 3–16. ISBN 9780871541635. [Google Scholar]
- Huedo-Medina, T.B.; Sánchez-Meca, J.; Marín-Martínez, F.; Botella, J. Assessing heterogeneity in meta-analysis: Q statistic or I 2 Index? Psychol. Methods 2006, 11, 193–206. [Google Scholar] [CrossRef] [Green Version]
- Higgins, J.P.T.; Thompson, S.G.; Deeks, J.J.; Altman, D.G. Measuring inconsistency in knowledgebases. BMJ 2003, 327, 557–560. [Google Scholar] [CrossRef] [Green Version]
- Egger, M.; Smith, G.D.; Schneider, M.; Minder, C. Bias in meta-analysis detected by a simple, graphical test. Br. Med. J. 1997, 315, 629–634. [Google Scholar] [CrossRef] [Green Version]
- Begg, C.B.; Mazumdar, M. Operating Characteristics of a Rank Correlation Test for Publication Bias. Biometrics 1994, 50, 1088–1101. [Google Scholar] [CrossRef]
- Viechtbauer, W. Conducting meta-analyses in R with the metafor. J. Stat. Softw. 2010, 36, 1–48. [Google Scholar] [CrossRef] [Green Version]
- Schwarzer, G.; Carpenter, J.R.; Rücker, G. Meta-Analysis with R; Springer: Freiburg, Germany, 2015; ISBN 9783319214153. [Google Scholar]
- Sterne, J.A.C.; Savović, J.; Page, M.J.; Elbers, R.G.; Blencowe, N.S.; Boutron, I.; Cates, C.J.; Cheng, H.Y.; Corbett, M.S.; Eldridge, S.M.; et al. RoB 2: A revised tool for assessing risk of bias in randomised trials. BMJ 2019, 366, l4898. [Google Scholar] [CrossRef] [Green Version]
- Julian, H.; Savović, J.; Page, M.J.; Sterne, J.A.C. RoB2 Development Group Revised Cochrane Risk-of-Bias Tool for Randomized Trials (RoB 2). Available online: https://drive.google.com/file/d/19R9savfPdCHC8XLz2iiMvL_71lPJERWK/view (accessed on 10 January 2020).
- Sterne, J.; Hernán, M.; Reeves, B.; Savović, J.; Berkman, N.D.; Viswanathan, M.; Henry, D.; Altman, D.; Ansari, M.; Boutron, I.; et al. ROBINS-I: A tool for assessing risk of bias in non-randomised studies of interventions. BMJ 2016, 355, i4919. [Google Scholar] [CrossRef] [Green Version]
- Sterne, J.; Higgins, J.; Elbers, R.; Reeves, B. The Development group for ROBINS-I. Risk of Bias. In Non-Randomized Studies of Interventions (ROBINS-I): Detailed Guidance; The Cochrane Collaboration: Bristol, UK, 2016. [Google Scholar]
- McGuinness, L.A.; Higgins, J.P.T. Risk-of-bias VISualization (robvis): An R package and Shiny web app for visualizing risk-of-bias assessments. In Proceedings of the Research Synthesis Methods; John Wiley and Sons Ltd.: Hoboken, NJ, USA, 2020. [Google Scholar]
- Craggs-Dino, L. The Effect of Food Safety Education on the Knowledge Attitude and Behavior of Foodservice Workers of Inner City Public Schools. Master’s Thesis, Florida International University, Miami, FL, USA, 28 June 2002. [Google Scholar]
- Mathiasen, L.A. Evaluating the Effectiveness of Food Safety Messages Along the Agri-Food Chain from Farm to Fork. Master’s Thesis, University of Guelph, Guelph, ON, Canada, 2004. [Google Scholar]
- Abernathy, T.; Hart, R. Evaluation of a HACCP pilot program for the food service industry. Can. J. Public Health 2004, 95, 470–472. [Google Scholar] [CrossRef] [PubMed]
- Lillquist, D.R.; McCabe, M.L.; Church, K.H. A Comparison of Traditional Handwashing Training with Active Handwashing Training in the Food Handler Industry. J. Environ. Health 2005, 67, 13–16. [Google Scholar] [PubMed]
- Walker, B.; Harrington, S.; Cole, C. The Usefulness of Computer-Based Instruction in Providing Educational Opportunities for Nursing Staff. J. Nurses Staff Dev. 2006, 22, 144–149. [Google Scholar] [CrossRef] [PubMed]
- Nieto-Montenegro, S.; Brown, J.L.; LaBorde, L.F. Development and assessment of pilot food safety educational materials and training strategies for Hispanic workers in the mushroom industry using the Health Action Model. Food Control 2008, 19, 616–633. [Google Scholar] [CrossRef]
- Acikel, C.H.; Ogur, R.; Yaren, H.; Gocgeldi, E.; Ucar, M.; Kir, T. The hygiene training of food handlers at a teaching hospital. Food Control 2008, 19, 186–190. [Google Scholar] [CrossRef]
- York, V.K.; Brannon, L.A.; Shanklin, C.W.; Roberts, K.R.; Barrett, B.B.; Howells, A.D. Intervention improves restaurant employees’ food safety compliance rates. Int. J. Contemp. Hosp. Manag. 2009, 21, 459–478. [Google Scholar] [CrossRef] [Green Version]
- Brannon, L.A.; York, V.K.; Roberts, K.R.; Shanklin, C.W.; Howells, A.D. Appreciation of food safety practices based on level of experience. J. Foodserv. Bus. Res. 2009, 12, 134–154. [Google Scholar] [CrossRef] [Green Version]
- Choudhury, M.; Mahanta, L.B.; Goswami, J.S.; Mazumder, M.D. Will capacity building training interventions given to street food vendors give us safer food? A cross-sectional study from India. Food Control 2011, 22, 1233–1239. [Google Scholar] [CrossRef]
- Fielding, L.; Ellis, L.; Clayton, D.; Peters, A. An evaluation of process specific information resources, aimed at hazard analysis, in Small and Medium Enterprises in food manufacturing. Food Control 2011, 22, 1171–1177. [Google Scholar] [CrossRef]
- Soon, J.M.; Baines, R.N. Food safety training and evaluation of handwashing intention among fresh produce farm workers. Food Control 2012, 23, 437–448. [Google Scholar] [CrossRef]
- Farzianpour, F.; Khaniki, G.J.; Batebi, F.; Yunesian, M. Compare the effects of two educational methods on the health principles knowledge of employees in food preparation. Am. J. Appl. Sci. 2012, 9, 1678–1683. [Google Scholar] [CrossRef] [Green Version]
- Nyamari, J. Evaluation of compliance to food saftey standards amongst food handlers in selected Hospitals in Kenya. Ph.D. Thesis, Kenyatta University, Nairobi, Kenya, 15 August 2013. [Google Scholar]
- Richard, A.E.; Brown, J.L.; Radhakrishna, R.B.; Yoder, E.P.; Nieto-Montenegro, S.; Cutter, C.N. Development and Implementation of a “Counter-Top” Training Program to Increase Retention of Food Safety Knowledge, Alter Behavior, Improve Attitude and Increase Skills of Spanish-speaking Retail Employees. Food Prot. Trends 2013, 33, 10–19. [Google Scholar]
- Strohbehn, C.; Arendt, S.W.; Ungku, U.F.; Meyer, J.R. Effectiveness of Food Safety Managerial Training: Face-to-Face or Computer-Based Delivery. J. Foodserv. Manag. Educ. 2013, 7, 7–19. [Google Scholar]
- Afolaranmi, T.O.; Hassan, Z.I.; Bello, D.A.; Tagurum, Y.O.; Miner, C.A.; Zoakah, A.; Ogbonna, C. Training: A vital tool for improving the knowledge and practice of food safety and hygiene among food handlers in boarding secondary schools in Plateau State. J. Med. Trop. 2014, 16, 87. [Google Scholar] [CrossRef]
- Da Cunha, D.T.; Stedefeldt, E.; de Rosso, V.V. The role of theoretical food safety training on Brazilian food handlers’ knowledge, attitude and practice. Food Control 2014, 43, 167–174. [Google Scholar] [CrossRef]
- Abushelaibi, A.M.; Jobe, B.; Afifi, H.S.; Mostafa, B.E.; Murad, A.A.; Mohammed, A.K. Evaluation of the effect of person-in-charge (PIC) program on knowledge and practice change of food handlers in Dubai. Food Control 2015, 50, 382–392. [Google Scholar] [CrossRef]
- Nik Husain, N.R.; Wan Muda, W.M.; Noor Jamil, N.I.; Nik Hanafi, N.N.; Abdul Rahman, R. Effect of food safety training on food handlers’ knowledge and practices: A randomized controlled trial. Br. Food J. 2016, 118, 795–808. [Google Scholar] [CrossRef]
- Norhaslinda, R.; Norhayati, A.; Mohd, A. Knowledge, attitudes and practices (KAP) on good manufacturing practices (GMP) among food handlers in Terengganu hospitals. Int. J. Pharm. Pharm. Sci. 2016, 8, 53–59. [Google Scholar] [CrossRef]
- Riaz, B.K.; Alim, M.A.; Islam, A.N.M.S.; Amin, K.M.B.; Sarker, M.A.B.; Hasan, K.; Ashad-Uz-Zaman, M.N.; Selim, S.; Quaiyum, S.; Haque, E.; et al. Role of courtyard counselling meeting in improving household food safety knowledge and practices in Munshiganj district of Bangladesh. Nagoya J. Med. Sci. 2016, 78, 387–398. [Google Scholar] [CrossRef]
- Nik Rosmawati, N.H.; Wan Manan, W.M.; Noor Izani, N.J.; Nik Nurain, N.H.; Razlina, A.R. The effect of Food Safety Education on handwashing practices in school canteens’ food handlers. Sains Malays. 2018, 47, 2119–2128. [Google Scholar] [CrossRef]
- Che-Has, S.; Afifah-Jaafar, S.; Tuan-Chilek, T. An assessment on pre-and post-food hygiene training on food safety’s Kap level among food handlers in Kuala Terengganu and Kuala Nerus. Malays. Appl. Biol. 2018, 47, 61–69. [Google Scholar]
- Grappasonni, I.; Petrelli, F.; Scuri, S.; Mahdi, S.S.; Sibilio, F.; Amenta, F. Knowledge and attitudes on food hygiene among food services staff on board ships. Ann. Ig. 2018, 30, 162–172. [Google Scholar] [CrossRef] [PubMed]
- Ma, L.; Chen, H.; Yan, H.; Wu, L.; Zhang, W. Food safety knowledge, attitudes, and behavior of street food vendors and consumers in Handan, a third tier city in China. BMC Public Health 2019, 19, 1128. [Google Scholar] [CrossRef]
- Auad, L.I.; Ginani, V.C.; Stedefeldt, E.; Nakano, E.Y.; Nunes, A.C.S.; Zandonadi, R.P. Food safety knowledge, attitudes, and practices of brazilian food truck food handlers. Nutrients 2019, 11, 1784. [Google Scholar] [CrossRef] [Green Version]
- Viator, C.; Blitstein, J.; Brophy, J.E.; Fraser, A. Preventing and controlling foodborne disease in commercial and institutional food service settings: A systematic review of published intervention studies. J. Food Prot. 2015, 78, 446–456. [Google Scholar] [CrossRef]
- Lynch, R.A.; Elledge, B.L.; Griffith, C.C.; Boatright, D.T. A Comparison of Food Safety Knowledge among Restaurant Managers, by Source of Training and Experience, in Oklahoma County, Oklahoma. J. Environ. Health 2003, 66, 9–14. [Google Scholar]
- Mortlock, M.P.; Peters, A.C.; Griffith, C.J. Food hygiene and hazard analysis critical control point in United Kingdom food industry: Practices, perceptions, and attitudes. J. Food Prot. 1999, 62, 786–792. [Google Scholar] [CrossRef]
- Clayton, D. Understanding and Predicting Food Handlers’ Implementation of Specific Food Safety Practices using Social Cognition Models. Ph.D. Thesis, University of Wales, Cardiff, UK, 2004. [Google Scholar]
- Pilling, V.K.; Brannon, L.A.; Shanklin, C.W.; Howells, A.D.; Roberts, K.R. Identifying Specific Beliefs to Target to Improve Restaurant Employees’ Intentions for Performing Three Important Food Safety Behaviors. J. Am. Diet. Assoc. 2008, 108, 991–997. [Google Scholar] [CrossRef] [Green Version]
- Joshi, Y.; Rahman, Z. Predictors of young consumer’s green purchase behaviour. Manag. Environ. Qual. 2016, 27, 452–472. [Google Scholar] [CrossRef]
- Jespersen, L.; MacLaurin, T.; Vlerick, P. Development and validation of a scale to capture social desirability in food safety culture. Food Control 2017, 82, 42–47. [Google Scholar] [CrossRef]
- DeDonder, S.; Jacob, C.J.; Surgeoner, B.V.; Chapman, B.; Phebus, R.; Powell, D.A. Self-reported and observed behavior of primary meal preparers and adolescents during preparation of frozen, uncooked, breaded chicken products. Br. Food J. 2009, 111, 915–929. [Google Scholar] [CrossRef]
- Dharod, J.M.; Pérez-Escamilla, R.; Paciello, S.; Bermúdez-Millán, A.; Venkitanarayanan, K.; Damio, G. Comparison between self-reported and observed food handling behaviors among latinas. J. Food Prot. 2007, 70, 1927–1932. [Google Scholar] [CrossRef] [PubMed]
- Choudhury, M.; Mahanta, L.; Goswami, J.; Mazumder, M.; Pegoo, B. Socio-economic profile and food safety knowledge and practice of street food vendors in the city of Guwahati, Assam, India. Food Control 2011, 22, 196–203. [Google Scholar] [CrossRef]
- Medeiros, L.; Hillers, V.; Kendall, P.; Mason, A. Evaluation of food safety education for consumers. J. Nutr. Educ. Behav. 2001, 33, S27–S34. [Google Scholar] [CrossRef]
- Zanin, L.M.; da Cunha, D.T.; de Rosso, V.V.; Capriles, V.D.; Stedefeldt, E. Knowledge, attitudes and practices of food handlers in food safety: An integrative review. Food Res. Int. 2017, 100, 53–62. [Google Scholar] [CrossRef] [PubMed]
- Mullan, B.; Allom, V.; Sainsbury, K.; Monds, L.A. Examining the predictive utility of an extended theory of planned behaviour model in the context of specific individual safe food-handling. Appetite 2015, 90, 91–98. [Google Scholar] [CrossRef] [Green Version]
- Miralles, M.M.; Maestre-Carballa, L.; Lluesma-Gomez, M.; Martinez-Garcia, M. High-throughput 16S rRNA sequencing to assess potentially active bacteria and foodborne pathogens: A case example in ready-to-eat food. Foods 2019, 8, 480. [Google Scholar] [CrossRef] [Green Version]
- Lee, H.; Abdul Halim, H.; Thong, K.; Chai, L. Assessment of Food Safety Knowledge, Attitude, Self-Reported Practices, and Microbiological Hand Hygiene of Food Handlers. Int. J. Environ. Res. Public Health 2017, 14, 55. [Google Scholar] [CrossRef] [Green Version]
- Donkor, E.S.; Kayang, B.B.; Quaye, J.; Akyeh, M.L. Application of the WHO keys of safer food to improve food handling practices of food vendors in a poor resource community in Ghana. Int. J. Environ. Res. Public Health 2009, 6, 2833–2842. [Google Scholar] [CrossRef]
- Frewer, L.; Shepherd, R.; Sparks, P. The interrelationship between perceived knowledge, control and risk associated with a range of food-related hazards targeted at the individual, other people and society. J. Food Saf. 1994, 14, 19–40. [Google Scholar] [CrossRef]
- Rhodes, L. Competency-based adult learning in food safety programs. In Food Protection Technology; Felix, C., Ed.; CRC Press: Boca Raton, FL, USA, 1987; pp. 299–306. ISBN 13:978-1-351-07207-6. [Google Scholar]
- Báez, Y.A.; Rodríguez, M.A.; De La Vega, E.J.; Tlapa, D.A. Factors Influencing the Human Error of Workers in Manual Assembly Lines. Inf. Tecnol. 2013, 24, 67–78. [Google Scholar] [CrossRef]
- Rennie, D.M. Evaluation of Food Hygiene Education. Br. Food J. 1994, 96, 20–25. [Google Scholar] [CrossRef]
- Flores, A.-L.; Gonzalez, A.; Neumann, T.C. Estimating the Effects of Length of Exposure to a Training Program: The Case of Job Corps; IZA Discussion Paper; Institute for the Study of Labor: Bonn, Germany, 2007; pp. 1–37. [Google Scholar]
- Jevšnik, M.; Hlebec, V.; Raspor, P. Food safety knowledge and practices among food handlers in Slovenia. Food Control 2008, 19, 1107–1118. [Google Scholar] [CrossRef]
- Kassa, H.; Silverman, G.S.; Baroudi, K. Effect of a Manager Training and Certification Program on Food safety and Hygiene in Food service Operations. Environ. Health Insights 2010, 4, 13–20. [Google Scholar] [CrossRef]
- Jones, T.F.; Pavlin, B.I.; LaFleur, B.J.; Ingram, L.A.; Schaffner, W. Restaurant Inspection Scores and Foodborne Disease. Emerg. Infect. Dis. 2004, 10, 688–692. [Google Scholar] [CrossRef]
- Hedberg, C.W.; Smith, S.J.; Kirklanb, E.; Radke, V.; Jones, T.F.; Selman, C.A. Systematic environmental evaluations to identify food safety differences between outbreak and nonoutbreak restaurants. J. Food Prot. 2006, 69, 2697–2702. [Google Scholar] [CrossRef]
- Murphy, K.S.; DiPietro, R.B.; Kock, G.; Lee, J.S. Does mandatory food safety training and certification for restaurant employees improve inspection outcomes? Int. J. Hosp. Manag. 2011, 30, 150–156. [Google Scholar] [CrossRef]
- Insfran, A.M.; Redondo, E.D. Factores de Éxito de Lean Seis Sigma en la Industria Alimentaria. Lat. Am. J. Appl. Eng. 2018, 3, 1–6. [Google Scholar]
- Green, L.R.; Selman, C. Factors Impacting Food Workers’ and Managers’ Safe Food Preparation Practices: A Qualitative Study. Food Prot. Trends 2005, 25, 981–990. [Google Scholar]
- Howells, A.D.; Roberts, K.R.; Shanklin, C.W.; Pilling, V.K.; Brannon, L.A.; Barrett, B.B. Restaurant Employees’ Perceptions of Barriers to Three Food Safety Practices. J. Am. Diet. Assoc. 2008, 108, 1345–1349. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mohammad, Z.H.; Yu, H.; Neal, J.A.; Gibson, K.E.; Sirsat, S.A. Food safety challenges and barriers in southern United States farmers markets. Foods 2020, 9, 12. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Guo, Z.; Bai, L.; Gong, S. Government regulations and voluntary certifications in food safety in China: A review. Trends Food Sci. Technol. 2019, 90, 160–165. [Google Scholar] [CrossRef]
- O’Brien, S.J. Foodborne Diseases: Prevalence of Foodborne Diseases in Europe. In Encyclopedia of Food Safety; Elsevier: Amsterdam, The Netherlands, 2014; Volume 1, pp. 302–311. ISBN 9780123786128. [Google Scholar]
- Dudeja, P.; Singh, A.; Sahni, N.; Kaur, S.; Goel, S. Effectiveness of an intervention package on knowledge, attitude, and practices of food handlers in a tertiary care hospital of north India: A before and after comparison study. Med. J. Armed Forces India 2017, 73, 49–53. [Google Scholar] [CrossRef] [PubMed] [Green Version]





| Author, Year | Setting, Location | Main Intervention | Study Overview | Outcome | Summary of Findings Mean (SD) |
|---|---|---|---|---|---|
| Ehiri (1997) [29] | Centres and City Council, Scotland | Elementary food hygiene training | RCT; nc1 = 75, nc2 = 204; ni1 = 94, ni2 = 94; participants = 63% female | Knowledge score | Control = 61.66; Intervention = 66; (p < 0.05) |
| Craggs-Dino (2002) [80] | Foodservice at schools, USA | Food safety videotapes | RCT; nc = 10, ni = 22; TL = 3 h; FU = 2 weeks; participants = 94% female | Knowledge score | Control Pre 57.7 (14.7), Post 60.0 (12.3); Intervention Pre 53 (14.8), Post 65.3 (14.0) |
| Attitude score | Control Pre 4.0 (0.5), Post 4.38 (0.3); Intervention Pre 4.12 (0.5), Post 4.04 (0.5) | ||||
| Observed behavior (practice) | Control Pre 4.39 (0.4), Post 4.30 (0.3); Intervention Pre 4.44 (0.4), Post 4.38 (0.4) | ||||
| Mathiasen (2004) [81] | Greenhouses, Canada | Agricultural training video | Pre-post study; n = 50; TL = 1 day; participants = 78.3% female | Knowledge score | Pre 4.56 (0.312), Post 4.68 (0.165); (p = 0.07) |
| Abernathy and Hart (2004) [82] | Restaurants, Canada | Critical Approach© program. | RCT; nc = 42, ni = 16; FU = 1 year | Knowledge quantity | Control Pre 36.5 (28.6), Post 49.2 (36.4); Intervention Pre 50 (41), Post 81.3 (32.5) |
| Self-reported practice score | Control Pre 46.8 (38.8), Post 57.1 (47.8); Intervention Pre 56.3 (48.8), Post 75(43.3) | ||||
| Lillquist et al. (2005) [83] | Food handlers, USA | Lecture and video | RCT; n = 22; TL = 1.5 h; FU= 2 weeks; participants = 82% female | Knowledge score | Control 8.00 (3.2); Intervention 12.4 (2.3); (p <0.050) |
| Lecture, video, and hand washing training | RCT; n = 22; TL = 1.5 h; FU= 2 weeks | Knowledge score | Control 8.00 (3.2); Intervention 15.80 (1.3); (p < 0.05) | ||
| Fenton et al. (2006) [9] | Food processing facilities, USA | Face to face training | RCT; nc = 28, ni = 31; TL= 1 day | Knowledge score | Control Pre 15.1 (1.9), Post 15.8 (2.1); Intervention Pre 12.60 (3.8), Post 15.70 (3.0); (p < 0.05) |
| Attitude score | Control 40.3 (2.5); Intervention Pre 36.40 (5.6), Post 40.30 (3.4); (p < 0.05) | ||||
| Computer based training | RCT; nc = 28, ni = 35 | Knowledge score | Control Pre 15.1 (1.9), Post 15.8 (2.1); Intervention Pre 12.80 (4.4), Post 14.5 (4.5); (p < 0.05) | ||
| Attitude score | Control 40.3 (2.5) Intervention Pre 36.50 (5.3), Post 40.60 (3.5); (p < 0.05) | ||||
| Walker et al. (2006) [84] | Care settings for elderly residents, USA | Computer based training | Pre-post study, n = 10; TL = 40 min | Knowledge score | Pre 25.9 (2.85), Post 28.6 (1.89) |
| Instructor-led workshops | Pre-post study, n = 8 TL = 62 min | Knowledge score | Pre 23.88 (3.18), Post 28.25 (1.39) | ||
| Nieto-Montenegro et Al. (2007) [85] | Mushrooms companies, USA | Visual aids, discussion topics, demonstrations, and hands-on activities | RCT; (Track C packing house); nc = 52, ni = 61; TL = 225 min; participants = 49.1% female | Knowledge score | Control Pre 6.79 (1.55), Post 6.16 (0.166); Intervention Pre 5.84 (1.43), Post 9.29 (0.163) |
| Attitude score | Control Pre 87.1 (6.3), Post 97.4 (2.2); Intervention Pre 41.30 (19.7), Post 94.5 (6.3) | ||||
| Acikel et Al. (2008) [86] | Kitchen of a military medical academic, Turkey | Lecture and practice | Pre-post study; n = 78; TL = 1 day; FU = 1 mo.; participants = 14% female | Knowledge score | Pre 45.60 (11.2), Post 56.50 (11.5); (p = 0.001) |
| Attitude score | Pre 2.70 (1.73), Post 2.59 (1.8); (p > 0.05) | ||||
| York et al. (2009) [87] | Restaurants, USA | Servsafe® Training | RCT; nc = 140, ni = 94; TL = 4 h | Attitude score | Control 37.05 (23.86); Training group 47.77 (24.13) |
| A theory-based intervention | RCT; nc = 140, ni = 83; TL = 4 h | Attitude score | Control 37.05 (23.86); Training group 46.38(23.04) | ||
| Servsafe® and a theory-based intervention | RCT; nc = 140, ni= 51; TL = 4 h | Attitude score | Control 37.05 (23.86); Training group 56.19 (21.45) | ||
| Brannon et al. (2009) [88] | University, USA | Formal food certification class | CS; nc= 68; ni = 120; participants = 68.5% female | Attitude score | No experience 8.78 (3.21); Well-informed 10.54 (3.3) |
| Park et Al. (2010) [38] | Restaurants, Korea | Lecture and demonstration techniques | Control-intervention (non randomized) and pre-post study; ni = 41, nc = 49; TL = 1 h; participants = 65.5% female | Knowledge score | Intervention Pre 49.30 (19.5), Post 66.60 (16.5); Control Pre 51.7 (17.4), Post 45.8 (18.8) |
| Self-reported practice score | Intervention Pre 103.2 (14.7), Post 102.40 (16.4); Control Pre 107.5 (20.4), Post 105.4 (32.2) | ||||
| Observed practice score | Pre 57.2 (7.8), Post 63.7 (7.6) | ||||
| Choudhury (2011) [89] | Street food vendors, India | Charts, posters, videos, role plays, demonstration, puppet shows, and handouts | Pre-post study; n1 = 43, n2 = 26; TL = 60 h | Knowledge score | Pre 22.30 (16.46), Post 63.50 (15.83); (p = 0.00) |
| Observed practice score | Pre 4.57 (12.18), Post 44.67 (42.14); (p = 0.00) | ||||
| Fielding (2011) [90] | Micro and SME Manufacturers of soups and sauces, UK | Landscape booklet | Control-intervention study (non randomized); ni = 26, nc = 16; TL = 6 weeks | Knowledge score | Control 91.23 (4.89); Intervention 85.22 (4.27) |
| Self-reported practice score | Control 71.98 (9.62); Intervention 63.99 (7.12) | ||||
| Soon and Baines (2012) [91] | Fresh produce farms, UK | Booklet, slides, youtube®, and demonstrations | Pre-post study; n1 = 62, n2 = 42; FU = 1 day; participants = 45% female | Knowledge score | Pre 5.74 (1.77), Post 7.76 (0.43); (p < 0.001) |
| Farzianpour (2012) [92] | Food preparation and supply centers, Iran | Face-to-face training | RCT; nc = 140, ni = 135 | Knowledge score | Control Pre 39.81 (13.06), Post 42.62 (13.16); Intervention Pre 41.98 (15.51), Post 51.04 (11.51) |
| Distant learning using educational booklet | RCT; nc = 140, ni = 145 | Knowledge score | Control Pre 39.81 (13.06), Post 42.62 (13.16); Intervention Pre 40.89 (12.54), Post 51.88 (14.67) | ||
| Nyamari (2013) [93] | Hospitals, Kenya | Lectures, demonstration, group discussions, and practical experiences | RCT; nc = 140, ni = 129; TL = 1 week; FU= 3 mo.; participants = 54.8% female | Knowledge score | Control Pre 51.8 (15.1), Post 53.4 (17.8); Intervention 50.6 (16.5), 76.4 (15.5) |
| Self-reported practice score | Control Pre 110.7, Post 102.7; Intervention Pre 101.3 (11.6), Post 105.3 (12.2) | ||||
| Richard (2013) [94] | Delicatessens meat shops, USA | Face to face training | RCT; nc = 10, ni=10; FU= 6 months; participants = 20.7% female | Knowledge score | Control 0.6(0.7) Intervention 4.3(0.8) |
| Strohbehn (2013) [95] | Retail foodservices (restaurants, hospitals, schools, others), USA | Face to face Training | Pre-post study; n1= 39, n2 = 21; participants = 80.9% female | Score in communicating safety culture attitude | Pre 3.99 (0.32), Post 4.13 (0.41) |
| Computer based instruction | Pre-post study; n1 = 39, n2 = 15; participants = 50% female | Score in communicating safety culture attitude | Pre 3.99 (0.32), Post 4.0 (0.29) | ||
| Afolaranmi (2014) [96] | Kitchens of Secondary schools, Nigeria | Lectures, practical demonstrations, charts, manuals, and posters | Pre-post study; n1 = 132, n2 = 130; TL = 1 day; FU = 3 mo.; participants = 93.2% female | Knowledge score | Pre 8.91 (2.18), Post 22.20 (3.62); (p <0.001) |
| Self-reported practice score | Pre 32.66 (3.24), Post 44.46 (3.80); (p < 0.001) | ||||
| da Cunha (2014) [97] | Street food kiosks, beach kiosks, restaurants, hospitals and school, Brazil | Lecture based training | CS; nc = 58, ni = 125; FU = 10 h; participants = 65.5% female | Knowledge score | Untrained 5.40 (1.8); Trained 6.60(2.0); (p <0.001) |
| Attitude score | Untrained 9.00(1.1); Trained 9.20 (1.8); (p = 0.40) | ||||
| Self-reported practice score | Untrained 36.00 (3.6); Trained 35.70 (4.0); (p = 0.59) | ||||
| Observed practice score | Untrained 23.00 (6.25) Trained 24.20 (7.8); (p = 0.67) | ||||
| Faour-Klingbeil (2015) [31] | Food businesses, Lebanon | Face to face/lectures | CS; nc = 46, ni = 34; participants = 93% female | Knowledge score | Control 52.20 (19.6); Intervention 62.50 (21.7) |
| Self-reported practice score | Control 57.60 (14.3); Intervention 66.40 (10.7); (p < 0.01) | ||||
| Abushelaibi (2015) [98] | Food stablishments, UAE | Face to face training | Pre-post study; n = 48; FU = 3 months | Observed practice score | Pre 2.80 (0.27), Post 2.79 (0.23); (p < 0.05) |
| Nik Husain (2016) [99] | School canteens, Malaysia | Health talks, demonstrations, self-practice, posters | RCT; nc = 46, ni = 33; TL = 235 min; FU = 3 weeks; participants = majority female | Knowledge score | Control 19.49 (0.57) Intervention 21.03 (0.76); (p = 0.59) |
| Self-reported practice score | Control 28.59 (5.45); Intervention 28.79 (4.51) | ||||
| Norhaslinda (2016) [100] | Hospitals, Malaysia | Training course attendance | CS; ni = 47, nc = 3; participants = 72% female | GMP knowledge score | Untrained 79.00 (2.51); Trained 83.30 (1.46) |
| GMP attitude score | Untrained 88.00 (3.0); Trained 87.00 (3.49); (p = 0.65) | ||||
| Self-reported practice score | Untrained 83.40 (2.08); Trained 91.20 (1.72); (p = 0.74) | ||||
| Riaz (2016) [101] | Household, Bangladesh | Face to face workshops (courtyard counselling meetings) | Pre-post study; n = 194; TL = 4 days; participants = 100% female | Knowledge score | Pre 23.70 (5.7), Post 25.60 (5.3); (p < 0.001) |
| Observed practice score | Pre 20.50 (5.34), Post 22.10 (3.9); (p < 0.001) | ||||
| Nik Husain (2018) [102] | School canteens, Malaysia | Demonstrations, self-practice, and posters | RCT; ni = 33, nc = 46; TL = 195 min; participants = 89.9% female | Observed handwashing practice score | Control Pre 35.06 (29.23), Post 7.59 (29.84); Intervention Pre 29.0 (24.17), Post 44.52 (31.97) |
| Che-Has (2018) [103] | Food stablishment, Malaysia | Face to face training | Pre-post study; n = 100; Participants = 48% female | Knowledge score | Pre 11.12 (2.69), Post 12.83 (2.36); (p = 0.00) |
| Attitude score | Pre 4.21 (0.54), Post 4.21 (0.54); (p = 1.00) | ||||
| Self-reported practice score | Pre 9.01 (1.09), Post 10.22 (0.99); (p = 0.00) | ||||
| Grappasonni (2018) [104] | board merchant ships, Italy | Food safety training | CS; nc = 28, ni = 130; participants = male 100% | Knowledge score | Untrained 46.1 (3.4); Trained 52.9 (3.9) |
| MA (2019) [105] | Street vendors, China | Food safety training | CS; nc = 67, ni = 30; participants = 47.1% female | Knowledge score | Untrained 56 (16); Trained 60 (16); (p = 0.287) |
| Attitude score | Untrained 59 (16); Trained 63 (15) | ||||
| Auad (2019) [106] | Food trucks, Brazil | Food safety training | CS; nc = 18, ni = 22; participants = 20% female | Knowledge score | Untrained 7.00 (2.14); Trained 7.41 (1.44); (p = 0.638) |
| Attitude score | Untrained 6.39 (1.29); Trained 7.23 (1.02); (p = 0.033) | ||||
| Mean score in self-reported practice | Untrained 7.28 (1.41); Trained 8.09 (1.27); (p = 0.085) |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Insfran-Rivarola, A.; Tlapa, D.; Limon-Romero, J.; Baez-Lopez, Y.; Miranda-Ackerman, M.; Arredondo-Soto, K.; Ontiveros, S. A Systematic Review and Meta-Analysis of the Effects of Food Safety and Hygiene Training on Food Handlers. Foods 2020, 9, 1169. https://doi.org/10.3390/foods9091169
Insfran-Rivarola A, Tlapa D, Limon-Romero J, Baez-Lopez Y, Miranda-Ackerman M, Arredondo-Soto K, Ontiveros S. A Systematic Review and Meta-Analysis of the Effects of Food Safety and Hygiene Training on Food Handlers. Foods. 2020; 9(9):1169. https://doi.org/10.3390/foods9091169
Chicago/Turabian StyleInsfran-Rivarola, Andrea, Diego Tlapa, Jorge Limon-Romero, Yolanda Baez-Lopez, Marco Miranda-Ackerman, Karina Arredondo-Soto, and Sinue Ontiveros. 2020. "A Systematic Review and Meta-Analysis of the Effects of Food Safety and Hygiene Training on Food Handlers" Foods 9, no. 9: 1169. https://doi.org/10.3390/foods9091169








