Leveraging Blockchain for Transparency: A Study on Organ Supply Chains and Transplant Processes
Abstract
:1. Introduction
2. Literature Review
2.1. Theoretical Underpinning
2.2. Development of Hypothesis and Research Model
2.2.1. Performance Expectancy (PE)
2.2.2. Effort Expectancy (EE)
2.2.3. Facilitating Conditions (FCs)
2.2.4. Trust (TRU)
2.2.5. Technology Readiness (TRE)
2.2.6. Government Support (RS)
2.2.7. Data Security and Privacy (DSP)
2.2.8. Technology Affinity (TA)
3. Research Methodology
3.1. Questionnaire Design
3.2. Data Collection Procedure
3.3. Common Method Bias
4. Data Analysis
4.1. Exploratory Factor Analysis (EFA)
| Indicators | References | Cronbach’s Alpha | Factor Loadings | CR | AVE |
|---|---|---|---|---|---|
| PE 1: I believe blockchain technologies would benefit the procurement of organs. | [52] | 0.787 | 0.770 | 0.796 | 0.513 |
| PE 2: I can complete tasks more rapidly by utilizing blockchain technologies. | 0.853 | ||||
| PE 3: My productivity is enhanced by the utilization of blockchain technologies. | 0.864 | ||||
| PE 4: The utilization of blockchain technologies will enhance my likelihood of achieving superior performance in the procurement of organs. | 0.565 | ||||
| EE 1: I find acquiring the knowledge necessary to operate blockchain technology effortless. | [53] | 0.829 | 0.806 | 0.833 | 0.625 |
| EE 2: My engagement with blockchain technology is transparent and comprehensible. | 0.864 | ||||
| EE 3: I find blockchain easy to use. | 0.850 | ||||
| FC 1: The appropriate resources for BC are available at my facility. | [52] | 0.846 | 0.797 | 0.837 | 0.633 |
| FC 2: If technical assistance is necessary, my hospitals possess the expertise. | 0.832 | ||||
| FC 3: My firm knows that it is necessary to operate BC | 0.832 | ||||
| FC 4: My hospital lacks sufficient expertise regarding the implementation of BC. | 0.757 | ||||
| TRU 1: I have faith in the efficacy of BC. | [84] | 0.855 | 0.865 | 0.856 | 0.598 |
| TRU 2: I am confident that BC can maintain the security of the data and reduce the likelihood of fraud. | 0.807 | ||||
| TRU 3: I am confident in operating BC consistently and without error. | 0.798 | ||||
| TRU 4: I think BC will consistently deliver satisfactory and effective outcomes in the workplace. | 0.770 | ||||
| TRE 1: The introduction and potential of BC are well-received by my hospitals. | [84] | 0.842 | 0.860 | 0.845 | 0.646 |
| TRE 2: The appropriate infrastructure for BC integration is in place at my organisation. | 0.897 | ||||
| TRE 3: My hospital has the necessary security measures for BC. | 0.802 | ||||
| GS 1: My firm’s decision to implement BCSCM would depend on industry standards in place | [84] | 0.88 | 0.851 | 0.882 | 0.714 |
| GS 2: Market volatility and policy normalisation | 0.904 | ||||
| GS 3: Effective government environment for data protection and consumer protection | 0.891 | ||||
| DSP 1: There are security concerns regarding the adoption of AI. | [45] | 0.906 | 0.920 | 0.91 | 0.771 |
| DSP 2: SE 2: Traditional technologies are more secure than the current technologies. | 0.904 | ||||
| DSP 3: There is a belief that AI will make the firm’s data safe and secure. | 0.856 | ||||
| TA 1: I possess a high level of proficiency in utilizing a diverse array of computer technologies. | [84] | 0.851 | 0.865 | 0.851 | 0.656 |
| TA 2: I enjoy evaluating the capabilities of emerging technological systems. | 0.831 | ||||
| TA 3: I enjoy dedicating time to acquiring a novel technological system. | 0.854 | ||||
| BAOSC 1: In the future, I plan to implement blockchain technology. | Added by the Authors | 0.898 | 0.854 | 0.898 | 0.688 |
| BAOSC 2: In the future, I anticipate that I will implement blockchain technology. | 0.849 | ||||
| BAOSC 3: In the future, I intend to implement blockchain technology in my hospital. | 0.861 | ||||
| BAOSC 4: I intend to transform SC at my hospital digitally. | 0.871 |
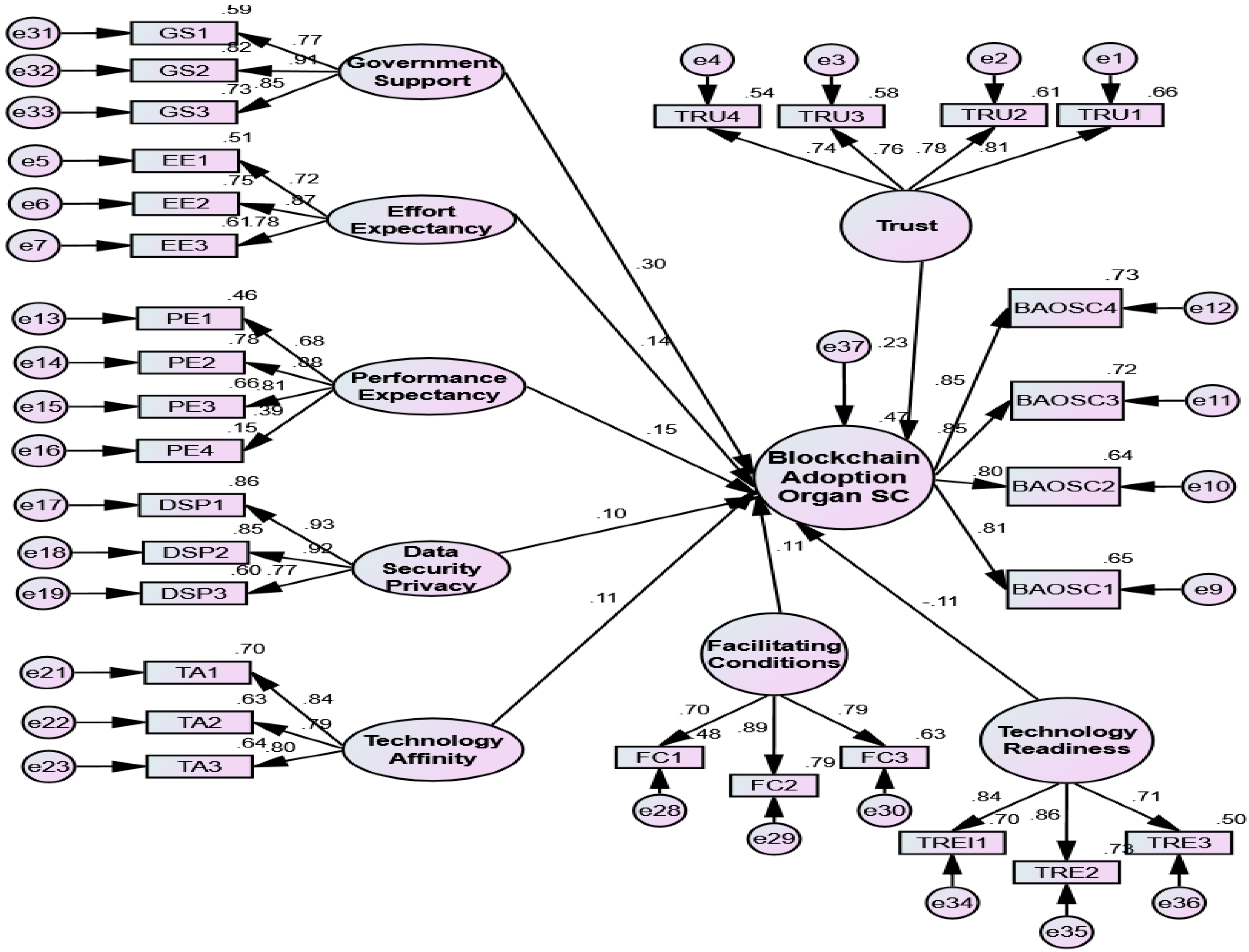
4.2. Confirmatory Factor Analysis (CFA)
4.3. Structural Model
4.4. Theoretical Implications
4.5. Practical Implications
5. Conclusions, Limitations and Future Developments
Author Contributions
Funding
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Bak, O.; Braganza, A.; Chen, W. Exploring blockchain implementation challenges in the context of healthcare supply chain (HCSC). Int. J. Prod. Res. 2023, 1–16. [Google Scholar] [CrossRef]
- Ghadge, A.; Bourlakis, M.; Kamble, S.; Seuring, S. Blockchain implementation in pharmaceutical supply chains: A review and conceptual framework. Int. J. Prod. Res. 2022, 61, 6633–6651. [Google Scholar] [CrossRef]
- Çaldağ, M.T.; Gökalp, E. Organizational Adoption of Blockchain Based Medical Supply Chain Management. Stud. Comput. Intell. 2023, 1128, 321–343. [Google Scholar] [CrossRef]
- Ahsan, M.; Siddique, Z. Industry 4.0 in Healthcare: A systematic review. Int. J. Inf. Manag. Data Insights 2022, 2, 100079. [Google Scholar] [CrossRef]
- Salimian, S.; Mousavi, S.M.; Antucheviciene, J. An Interval-Valued Intuitionistic Fuzzy Model Based on Extended VIKOR and MARCOS for Sustainable Supplier Selection in Organ Transplantation Networks for Healthcare Devices. Sustainability 2022, 14, 3795. [Google Scholar] [CrossRef]
- Mantecchini, L.; Paganelli, F.; Morabito, V.; Ricci, A.; Peritore, D.; Trapani, S.; Montemurro, A.; Rizzo, A.; Del Sordo, E.; Gaeta, A.; et al. Transportation of Organs by Air: Safety, Quality, and Sustainability Criteria. Transplant. Proc. 2016, 48, 304–308. [Google Scholar] [CrossRef]
- Mulu, A.; Ayenew, T. Characterization of Abattoir Wastewater and Evaluation of the Effectiveness of the Wastewater Treatment Systems in Luna and Kera Abattoirs in Central Ethiopia. Int. J. Sci. Eng. Res. 2015, 6, 1026–1040. [Google Scholar]
- Ahmadvand, S.; Pishvaee, M.S. Design and planning of organ transplantation networks. Int. Ser. Oper. Res. Manag. Sci. 2018, 262, 211–240. [Google Scholar] [CrossRef]
- Beliën, J.; De Boeck, L.; Colpaert, J.; Devesse, S.; Bossche, F.V.D. Optimizing the facility location design of organ transplant centers. Decis. Support Syst. 2013, 54, 1568–1579. [Google Scholar] [CrossRef]
- Arora, P.; Subramanian, R. Improving Societal Outcomes in the Organ Donation Value Chain. Prod. Oper. Manag. 2019, 28, 2110–2131. [Google Scholar] [CrossRef]
- Savaşer, S.; Kınay, B.; Kara, B.Y.; Cay, P. Organ transplantation logistics: A case for Turkey. OR Spectr. 2018, 41, 327–356. [Google Scholar] [CrossRef]
- Salimian, S.; Mousavi, S.M. A new scenario-based robust optimization approach for organ transplantation network design with queue condition and blood compatibility under climate change. J. Comput. Sci. 2022, 62, 101742. [Google Scholar] [CrossRef]
- Soltanisehat, L.; Alizadeh, R.; Hao, H.; Choo, K.-K.R. Technical, Temporal, and Spatial Research Challenges and Opportunities in Blockchain-Based Healthcare: A Systematic Literature Review. IEEE Trans. Eng. Manag. 2020, 70, 353–368. [Google Scholar] [CrossRef]
- Musamih, A.; Salah, K.; Jayaraman, R.; Arshad, J.; Debe, M.; Al-Hammadi, Y.; Ellahham, S. A blockchain-based approach for drug traceability in healthcare supply chain. IEEE Access 2021, 9, 9728–9743. [Google Scholar] [CrossRef]
- Omar, I.A.; Jayaraman, R.; Debe, M.S.; Salah, K.; Yaqoob, I.; Omar, M. Automating Procurement Contracts in the Healthcare Supply Chain Using Blockchain Smart Contracts. IEEE Access 2021, 9, 37397–37409. [Google Scholar] [CrossRef]
- Vishwakarma, A.; Dangayach, G.S.; Meena, M.L.; Jindal, M.K.; Gupta, S.; Jagtap, S. Modelling challenges of blockchain technology enabled healthcare sustainable supply chain management: A modified-total interpretive structural modelling approach. Oper. Manag. Res. 2023, 16, 1781–1790. [Google Scholar] [CrossRef]
- Yadav, A.K.; Shweta; Kumar, D. Blockchain technology and vaccine supply chain: Exploration and analysis of the adoption barriers in the Indian context. Int. J. Prod. Econ. 2022, 255, 108716. [Google Scholar] [CrossRef]
- Chavez, N.; Kendzierskyj, S.; Jahankhani, H.; Hosseinian, A. Securing transparency and governance of organ supply chain through blockchain. Adv. Sci. Technol. Secur. Appl. 2020, 97–118. [Google Scholar] [CrossRef]
- Khatter, K.; Relan, D. Non-functional requirements for blockchain enabled medical supply chain. Int. J. Syst. Assur. Eng. Manag. 2021, 13, 1219–1231. [Google Scholar] [CrossRef]
- Alzahrani, S.; Daim, T.; Choo, K.-K.R. Assessment of the Blockchain Technology Adoption for the Management of the Electronic Health Record Systems. IEEE Trans. Eng. Manag. 2022, 70, 2846–2863. [Google Scholar] [CrossRef]
- Alam, M.T.; Raza, K. Blockchain technology in healthcare: Making digital healthcare reliable, more accurate, and revolutionary. Transl. Bioinform. Healthc. Med. 2021, 2021, 81–96. [Google Scholar] [CrossRef]
- Bamakan, S.M.H.; Moghaddam, S.G.; Manshadi, S.D. Blockchain-enabled pharmaceutical cold chain: Applications, key challenges, and future trends. J. Clean. Prod. 2021, 302, 127021. [Google Scholar] [CrossRef]
- Dajim, L.A.; Al-Farras, S.A.; Al-Shahrani, B.S.; Al-Zuraib, A.A.; Mathew, R.M. Organ Donation Decentralized Application Using Blockchain Technology. In Proceedings of the 2nd International Conference on Computer Applications and Information Security, ICCAIS 2019, Riyadh, Saudi Arabia, 1–3 May 2019. [Google Scholar] [CrossRef]
- Radanović, I.; Likić, R. Opportunities for Use of Blockchain Technology in Medicine. Appl. Health Econ. Health Policy 2018, 16, 583–590. [Google Scholar] [CrossRef]
- Venkatesh, V.; Zhang, X. Unified theory of acceptance and use of technology: U.S. Vs. China. J. Glob. Inf. Technol. Manag. 2010, 13, 5–27. [Google Scholar] [CrossRef]
- Venkatesh, V.; Thong, J.Y.L.; Xu, X. Consumer acceptance and use of information technology: Extending the unified theory of acceptance and use of technology. MIS Q. 2012, 36, 157–178. [Google Scholar] [CrossRef]
- Yusof, R.J.R.; Qazi, A.; Inayat, I. Student real-time visualization system in classroom using RFID based on UTAUT model. Int. J. Inf. Learn. Technol. 2017, 34, 274–288. [Google Scholar] [CrossRef]
- Mensah, I.K. Factors Influencing the Intention of University Students to Adopt and Use E-Government Services: An Empirical Evidence in China. SAGE Open 2019, 9. [Google Scholar] [CrossRef]
- Cabrera-Sánchez, J.-P.; Villarejo-Ramos, F. Acceptance and use of big data techniques in services companies. J. Retail. Consum. Serv. 2019, 52, 101888. [Google Scholar] [CrossRef]
- Cao, G.; Duan, Y.; Edwards, J.S.; Dwivedi, Y.K. Understanding managers’ attitudes and behavioral intentions towards using artificial intelligence for organizational decision-making. Technovation 2021, 106, 102312. [Google Scholar] [CrossRef]
- Chatterjee, S.; Bhattacharjee, K.K. Adoption of artificial intelligence in higher education: A quantitative analysis using structural equation modelling. Educ. Inf. Technol. 2020, 25, 3443–3463. [Google Scholar] [CrossRef]
- Widyanto, H.A.; Kusumawardani, K.A.; Yohanes, H. Safety first: Extending UTAUT to better predict mobile payment adoption by incorporating perceived security, perceived risk and trust. J. Sci. Technol. Policy Manag. 2021, 13, 952–973. [Google Scholar] [CrossRef]
- Patil, P.; Tamilmani, K.; Rana, N.P.; Raghavan, V. Understanding consumer adoption of mobile payment in India: Extending Meta-UTAUT model with personal innovativeness, anxiety, trust, and grievance redressal. Int. J. Inf. Manag. 2020, 54, 102144. [Google Scholar] [CrossRef]
- DePietro, M.; Wiarda Fleischer, E. The context for change: Organization, technology and environment. In The Process of Technological Innovation; Lexington Books: Lexington, MA, USA, 1990. [Google Scholar]
- Ooi, K.-B.; Lee, V.-H.; Tan, G.W.-H.; Hew, T.-S.; Hew, J.-J. Cloud computing in manufacturing: The next industrial revolution in Malaysia? Expert Syst. Appl. 2018, 93, 376–394. [Google Scholar] [CrossRef]
- Tashkandi, A.N.; Al-Jabri, I.M. Cloud computing adoption by higher education institutions in Saudi Arabia: An exploratory study. Clust. Comput. 2015, 18, 1527–1537. [Google Scholar] [CrossRef]
- Senyo, P.K.; Effah, J.; Addae, E. Preliminary insight into cloud computing adoption in a developing country. J. Enterp. Inf. Manag. 2016, 29, 505–524. [Google Scholar] [CrossRef]
- Shee, H.; Miah, S.J.; Fairfield, L.; Pujawan, N. The impact of cloud-enabled process integration on supply chain performance and firm sustainability: The moderating role of top management. Supply Chain Manag. Int. J. 2018, 23, 500–517. [Google Scholar] [CrossRef]
- Rajan, C.A.; Baral, R. Adoption of ERP system: An empirical study of factors influencing the usage of ERP and its impact on end user. IIMB Manag. Rev. 2015, 27, 105–117. [Google Scholar] [CrossRef]
- Chang, M.-K.; Cheung, W.; Cheng, C.-H.; Yeung, J.H. Understanding ERP system adoption from the user’s perspective. Int. J. Prod. Econ. 2008, 113, 928–942. [Google Scholar] [CrossRef]
- AlBar, A.M.; Hoque, R. Determinants of Cloud ERP Adoption in Saudi Arabia: An Empirical Study. In Proceedings of the 2015 International Conference on Cloud Computing, ICCC 2015, Riyadh, Saudi Arabia, 26–29 April 2015. [Google Scholar] [CrossRef]
- Priyadarshinee, P.; Raut, R.D.; Jha, M.K.; Gardas, B.B. Understanding and predicting the determinants of cloud computing adoption: A two staged hybrid SEM—Neural networks approach. Comput. Hum. Behav. 2017, 76, 341–362. [Google Scholar] [CrossRef]
- Oliveira, T.; Thomas, M.; Espadanal, M. Assessing the determinants of cloud computing adoption: An analysis of the manufacturing and services sectors. Inf. Manag. 2014, 51, 497–510. [Google Scholar] [CrossRef]
- Maroufkhani, P.; Tseng, M.-L.; Iranmanesh, M.; Ismail, W.K.W.; Khalid, H. Big data analytics adoption: Determinants and performances among small to medium-sized enterprises. Int. J. Inf. Manag. 2020, 54, 102190. [Google Scholar] [CrossRef]
- Park, J.-H.; Kim, Y.B. Factors Activating Big Data Adoption by Korean Firms. J. Comput. Inf. Syst. 2019, 61, 285–293. [Google Scholar] [CrossRef]
- Pool, J.K.; Arabzad, S.M.; Asadi, A.; Ansari, M.R. RFID acceptance in SMEs using TOE framework: An empirical investigation on Iranian SMEs. Int. J. Logist. Syst. Manag. 2015, 21, 335. [Google Scholar] [CrossRef]
- Angeles, R. Purdue’s RFID supply chain for e-pedigree compliance: Applying the technology-organisation-environment (TOE) framework. Int. J. Bus. Inf. Syst. 2012, 10, 447. [Google Scholar] [CrossRef]
- Pillai, R.; Sivathanu, B.; Mariani, M.; Rana, N.P.; Yang, B.; Dwivedi, Y.K. Adoption of AI-empowered industrial robots in auto component manufacturing companies. Prod. Plan. Control. 2021, 33, 1517–1533. [Google Scholar] [CrossRef]
- Chatterjee, S.; Rana, N.P.; Dwivedi, Y.K.; Baabdullah, A.M. Understanding AI adoption in manufacturing and production firms using an integrated TAM-TOE model. Technol. Forecast. Soc. Chang. 2021, 170, 120880. [Google Scholar] [CrossRef]
- Queiroz, M.M.; Wamba, S.F. Blockchain adoption challenges in supply chain: An empirical investigation of the main drivers in India and the USA. Int. J. Inf. Manag. 2018, 46, 70–82. [Google Scholar] [CrossRef]
- Queiroz, M.M.; Wamba, S.F.; De Bourmont, M.; Telles, R. Blockchain adoption in operations and supply chain management: Empirical evidence from an emerging economy. Int. J. Prod. Res. 2020, 59, 6087–6103. [Google Scholar] [CrossRef]
- Kaba, B.; Touré, B. Understanding information and communication technology behavioral intention to use: Applying the UTAUT model to social networking site adoption by young people in a least developed country. J. Assoc. Inf. Sci. Technol. 2014, 65, 1662–1674. [Google Scholar] [CrossRef]
- Khechine, H.; Lakhal, S.; Ndjambou, P. A meta-analysis of the UTAUT model: Eleven years later. Can. J. Adm. Sci./Rev. Can. Sci. l’Administration 2016, 33, 138–152. [Google Scholar] [CrossRef]
- Dulle, F.W.; Minishi-Majanja, M. The suitability of the Unified Theory of Acceptance and Use of Technology (UTAUT) model in open access adoption studies. Inf. Dev. 2011, 27, 32–45. [Google Scholar] [CrossRef]
- Alabdullah, J.H.; Van Lunen, B.L.; Claiborne, D.M.; Daniel, S.J.; Yen, C.; Gustin, T.S. Application of the unified theory of acceptance and use of technology model to predict dental students’ behavioral intention to use teledentistry. J. Dent. Educ. 2020, 84, 1262–1269. [Google Scholar] [CrossRef] [PubMed]
- Ben Arfi, W.; Ben Nasr, I.; Kondrateva, G.; Hikkerova, L. The role of trust in intention to use the IoT in eHealth: Application of the modified UTAUT in a consumer context. Technol. Forecast. Soc. Chang. 2021, 167, 120688. [Google Scholar] [CrossRef]
- Ndayizigamiye, P.; Maharaj, M. Mobile health adoption in Burundi: A UTAUT perspective. In Proceedings of the GHTC 2016—IEEE Global Humanitarian Technology Conference: Technology for the Benefit of Humanity, Conference Proceedings, Seattle, WA, USA, 13–16 October 2016; pp. 613–623. [Google Scholar] [CrossRef]
- Wang, H.; Tao, D.; Yu, N.; Qu, X. Understanding consumer acceptance of healthcare wearable devices: An integrated model of UTAUT and TTF. Int. J. Med. Inform. 2020, 139, 104156. [Google Scholar] [CrossRef] [PubMed]
- Mendoza-Tello, J.C.; Mora, H.; Pujol-Lopez, F.A.; Lytras, M.D. Social Commerce as a Driver to Enhance Trust and Intention to Use Cryptocurrencies for Electronic Payments. IEEE Access 2018, 6, 50737–50751. [Google Scholar] [CrossRef]
- Hegner, S.M.; Beldad, A.D.; Brunswick, G.J. In Automatic We Trust: Investigating the Impact of Trust, Control, Personality Characteristics, and Extrinsic and Intrinsic Motivations on the Acceptance of Autonomous Vehicles. Int. J. Human–Comput. Interact. 2019, 35, 1769–1780. [Google Scholar] [CrossRef]
- Warkentin, M.; Sharma, S.; Gefen, D.; Rose, G.M.; Pavlou, P. Social identity and trust in internet-based voting adoption. Gov. Inf. Q. 2018, 35, 195–209. [Google Scholar] [CrossRef]
- Alkhater, N.; Walters, R.; Wills, G. An empirical study of factors influencing cloud adoption among private sector organisations. Telemat. Inform. 2018, 35, 38–54. [Google Scholar] [CrossRef]
- Shin, D.; Bianco, W.T. In Blockchain We Trust: Does Blockchain Itself Generate Trust? Soc. Sci. Q. 2020, 101, 2522–2538. [Google Scholar] [CrossRef]
- Batwa, A.; Norrman, A. Blockchain Technology and Trust in Supply Chain Management: A Literature Review and Research Agenda. Oper. Supply Chain Manag. Int. J. 2021, 14, 203–220. [Google Scholar] [CrossRef]
- Shin, D.D. Blockchain: The emerging technology of digital trust. Telemat. Inform. 2019, 45, 101278. [Google Scholar] [CrossRef]
- Leung, L.; Chen, C. E-health/m-health adoption and lifestyle improvements: Exploring the roles of technology readiness, the expectation-confirmation model, and health-related information activities. Telecommun. Policy 2019, 43, 563–575. [Google Scholar] [CrossRef]
- Mensah, I.K. Citizens’ Readiness to Adopt and Use E-government Services in the City of Harbin, China. Int. J. Public Adm. 2017, 41, 297–307. [Google Scholar] [CrossRef]
- Shirahada, K.; Ho, B.Q.; Wilson, A. Online public services usage and the elderly: Assessing determinants of technology readiness in Japan and the UK. Technol. Soc. 2019, 58, 101115. [Google Scholar] [CrossRef]
- Khayer, A.; Jahan, N.; Hossain, M.N.; Hossain, M.Y. The adoption of cloud computing in small and medium enterprises: A developing country perspective. VINE J. Inf. Knowl. Manag. Syst. 2021, 51, 64–91. [Google Scholar] [CrossRef]
- Munir, K. Cloud Computing and Big Data: Technologies, Applications and Security; Springer International Publishing: Berlin/Heidelberg, Germany, 2019; Volume 49. [Google Scholar]
- Takabi, H.; Joshi, J.B.; Ahn, G.-J. Security and privacy challenges in cloud computing environments. IEEE Secur. Priv. 2010, 8, 24–31. [Google Scholar] [CrossRef]
- Zhang, R.; Xue, R.; Liu, L. Security and Privacy for Healthcare Blockchains. IEEE Trans. Serv. Comput. 2021, 15, 3668–3686. [Google Scholar] [CrossRef]
- Kshetri, N. Blockchain’s roles in strengthening cybersecurity and protecting privacy. Telecommun. Policy 2017, 41, 1027–1038. [Google Scholar] [CrossRef]
- Esposito, C.; De Santis, A.; Tortora, G.; Chang, H.; Choo, K.-K.R. Blockchain: A Panacea for Healthcare Cloud-Based Data Security and Privacy? IEEE Cloud Comput. 2018, 5, 31–37. [Google Scholar] [CrossRef]
- Dwivedi, A.D.; Srivastava, G.; Dhar, S.; Singh, R. A Decentralized Privacy-Preserving Healthcare Blockchain for IoT. Sensors 2019, 19, 326. [Google Scholar] [CrossRef] [PubMed]
- Fleming, D.E.; Artis, A.B. Measuring Corporate Affinity for Technology: A Scale for Customers and Employees. J. Pers. Sell. Sales Manag. 2010, 30, 167–179. [Google Scholar] [CrossRef]
- Franke, T.; Attig, C.; Wessel, D. A Personal Resource for Technology Interaction: Development and Validation of the Affinity for Technology Interaction (ATI) Scale. Int. J. Human–Comput. Interact. 2018, 35, 456–467. [Google Scholar] [CrossRef]
- Malhotra, N.; Dash, S. Marketing Research: An Applied Orientation; Pearson Education: New Delhi, India, 2015. [Google Scholar]
- Podsakoff, P.M.; MacKenzie, S.B.; Lee, J.-Y.; Podsakoff, N.P. Common method biases in behavioral research: A critical review of the literature and recommended remedies. J. Appl. Psychol. 2003, 88, 879–903. [Google Scholar] [CrossRef]
- Hair, J.F.; Ringle, C.M.; Sarstedt, M. Partial Least Squares: The Better Approach to Structural Equation Modeling? Long Range Plan. 2012, 45, 312–319. [Google Scholar] [CrossRef]
- Olkin, I.; Sampson, A.R. Multivariate Analysis: Overview. In International Encyclopedia of the Social & Behavioral Sciences; Elsevier: Amsterdam, The Netherlands, 2001; pp. 10240–10247. [Google Scholar] [CrossRef]
- Hair, J.F.; Sarstedt, M.; Ringle, C.M.; Mena, J.A. An assessment of the use of partial least squares structural equation modeling in marketing research. J. Acad. Mark. Sci. 2012, 40, 414–433. [Google Scholar] [CrossRef]
- Wong, L.-W.; Tan, G.W.-H.; Lee, V.-H.; Ooi, K.-B.; Sohal, A. Unearthing the determinants of Blockchain adoption in supply chain management. Int. J. Prod. Res. 2020, 58, 2100–2123. [Google Scholar] [CrossRef]
- Fornell, C.; Larcker, D.F. Evaluating Structural Equation Models with Unobservable Variables and Measurement Error. J. Mark. Res. 1981, 18, 39–50. [Google Scholar] [CrossRef]
- Henseler, J.; Ringle, C.M.; Sarstedt, M. A new criterion for assessing discriminant validity in variance-based structural equation modeling. J. Acad. Mark. Sci. 2015, 43, 115–135. [Google Scholar] [CrossRef]
- Hair, J.F.; Page, M.; Brunsveld, N. Essentials of Business Research Methods, 4th ed.; Taylor & Franscis: Abingdon, UK, 2019; Volume 4. [Google Scholar]
- Sarstedt, M.; Ringle, C.M.; Hair, J.F. Partial Least Squares Structural Equation Modeling. In Handbook of Market Research; Springer International Publishing: Cham, Switzerland, 2022; pp. 587–632. [Google Scholar] [CrossRef]
- Byrne, B.M. Structural Equation Modeling with AMOS: Basic Concepts, Applications, and Programming; Multivariate Applications series; Taylor & Francis Group: Abingdon, UK, 2010; Volume 396, p. 7384. [Google Scholar]
- Dhingra, S.; Raut, R.; Gunasekaran, A.; Naik, B.K.R.; Masuna, V. Analysis of the challenges for blockchain technology adoption in the Indian health-care sector. J. Model. Manag. 2023, 19, 375–406. [Google Scholar] [CrossRef]
- Quayson, M.; Avornu, E.K.; Bediako, A.K. Modeling the enablers of blockchain technology implementation for information management in healthcare supply chains. Mod. Supply Chain Res. Appl. 2024, 6, 101–121. [Google Scholar] [CrossRef]
- Ahmed, W.A.; MacCarthy, B.L. Blockchain-enabled supply chain traceability—How wide? How deep? Int. J. Prod. Econ. 2023, 263, 108963. [Google Scholar] [CrossRef]
- Cole, H. The organ supply chain: Geography and the inequalities of transplant logistics. Trans. Inst. Br. Geogr. 2021, 46, 1008–1021. [Google Scholar] [CrossRef]
- Goli, A.; Ala, A.; Mirjalili, S. A robust possibilistic programming framework for designing an organ transplant supply chain under uncertainty. Ann. Oper. Res. 2022, 328, 493–530. [Google Scholar] [CrossRef]
- Zahiri, B.; Tavakkoli-Moghaddam, R.; Pishvaee, M.S. A robust possibilistic programming approach to multi-period location–allocation of organ transplant centers under uncertainty. Comput. Ind. Eng. 2014, 74, 139–148. [Google Scholar] [CrossRef]
- Francisco, K.; Swanson, D. The Supply Chain Has No Clothes: Technology Adoption of Blockchain for Supply Chain Transparency. Logistics 2018, 2, 2. [Google Scholar] [CrossRef]
- Ritchi, H.; Harnowo, A.; Sugianto, L.P.M.; Setiono, K.; Saputro, V. Reviving the information veracity in healthcare supply chain with blockchain: A systematic review. Supply Chain Forum Int. J. 2023, 25, 111–130. [Google Scholar] [CrossRef]
- Dwivedi, Y.K.; Rana, N.P.; Janssen, M.; Lal, B.; Williams, M.D.; Clement, M. An empirical validation of a unified model of electronic government adoption (UMEGA). Gov. Inf. Q. 2017, 34, 211–230. [Google Scholar] [CrossRef]
- Dwivedi, Y.K.; Rana, N.P.; Jeyaraj, A.; Clement, M.; Williams, M.D. Re-examining the Unified Theory of Acceptance and Use of Technology (UTAUT): Towards a Revised Theoretical Model. Inf. Syst. Front. 2019, 21, 719–734. [Google Scholar] [CrossRef]
- Chong, A.Y.-L.; Liu, M.J.; Luo, J.; Keng-Boon, O. Predicting RFID adoption in healthcare supply chain from the perspectives of users. Int. J. Prod. Econ. 2014, 159, 66–75. [Google Scholar] [CrossRef]
- Bandhu, K.C.; Litoriya, R.; Lowanshi, P.; Jindal, M.; Chouhan, L.; Jain, S. Making drug supply chain secure traceable and efficient: A Blockchain and smart contract based implementation. Multimed. Tools Appl. 2022, 82, 23541–23568. [Google Scholar] [CrossRef] [PubMed]
- Venkatesh, V.; Morris, M.G.; Davis, G.B.; Davis, F.D. User Acceptance of Information Technology: Toward a Unified View. MIS Q. 2003, 27, 425–478. [Google Scholar] [CrossRef]
- Kamble, S.; Gunasekaran, A.; Arha, H. Understanding the Blockchain technology adoption in supply chains-Indian context. Int. J. Prod. Res. 2018, 57, 2009–2033. [Google Scholar] [CrossRef]
- Santhi, A.R.; Muthuswamy, P. Influence of Blockchain Technology in Manufacturing Supply Chain and Logistics. Logistics 2022, 6, 15. [Google Scholar] [CrossRef]
- Moretto, A.; Macchion, L. Drivers, barriers and supply chain variables influencing the adoption of the blockchain to support traceability along fashion supply chains. Oper. Manag. Res. 2022, 15, 1470–1489. [Google Scholar] [CrossRef]
- Alazab, M.; Alhyari, S.; Awajan, A.; Abdallah, A.B. Blockchain technology in supply chain management: An empirical study of the factors affecting user adoption/acceptance. Clust. Comput. 2020, 24, 83–101. [Google Scholar] [CrossRef]
| (A) Discriminant Validity (Fornell and Larcker Approach) | |||||||||
| TRU | EE | BAOSC | PE | DSP | TA | FC | GS | TRE | |
| TRU | 0.773 | ||||||||
| EE | 0.213 ** | 0.791 | |||||||
| BAOSC | −0.046 | −0.076 | 0.83 | ||||||
| PE | 0.197 ** | 0.076 | 0.074 | 0.716 | |||||
| DSP | −0.019 | −0.104 | 0.215 ** | −0.258 *** | 0.878 | ||||
| TA | 0.134 † | −0.067 | 0.334 *** | −0.091 | 0.303 *** | 0.81 | |||
| FC | 0.399 *** | 0.290 *** | 0.096 | 0.106 | −0.047 | 0.099 | 0.796 | ||
| GS | −0.052 | −0.150 * | 0.250 *** | −0.011 | 0.199 ** | 0.203 ** | 0.041 | 0.845 | |
| TRE | 0.002 | 0.351 *** | −0.122 † | 0.109 | −0.083 | −0.109 | 0.170 * | −0.039 | 0.804 |
| (B) Discriminant Validity (HTMT) Analysis | |||||||||
| TRU | EE | BAOSC | PE | DSP | TA | FC | GS | TRE | |
| TRU | |||||||||
| EE | 0.205 | ||||||||
| BAOSC | 0.039 | 0.079 | |||||||
| PE | 0.223 | 0.059 | 0.068 | ||||||
| DSP | 0.007 | 0.116 | 0.211 | 0.254 | |||||
| TA | 0.136 | 0.084 | 0.339 | 0.087 | 0.311 | ||||
| FC | 0.423 | 0.288 | 0.093 | 0.092 | 0.059 | 0.11 | |||
| GS | 0.045 | 0.158 | 0.248 | 0.015 | 0.215 | 0.216 | 0.047 | ||
| TRE | 0.003 | 0.364 | 0.14 | 0.098 | 0.091 | 0.108 | 0.17 | 0.057 | |
| Parameters | Estimate | SE | CR | p | Hypotheses |
|---|---|---|---|---|---|
| BAOSC <--- PE | 0.152 | 0.048 | 2.410 | 0.016 | Supported at less than LOS 5% |
| BAOSC <--- EE | −0.010 | 0.043 | −0.157 | 0.876 | Not supported |
| BAOSC <--- FC | 0.126 | 0.050 | 2.003 | 0.045 | Supported at less than LOS 5% |
| BAOSC <--- TRU | −0.135 | 0.054 | −2.154 | 0.031 | Supported at less than LOS 5% |
| BAOSC <--- TRE | −0.109 | 0.038 | −1.750 | 0.080 | Not supported |
| BAOSC <--- GS | 0.166 | 0.057 | 2.686 | 0.007 | Supported at less than LOS 5% |
| BAOSC <--- DSP | 0.142 | 0.041 | 2.367 | 0.018 | Supported at less than LOS 5% |
| BAOSC <--- TA | 0.274 | 0.060 | 4.251 | *** | Supported at less than LOS 1% |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Panigrahi, R.R.; Mukherjee, S.; Shaikh, Z.H.; Nomran, N.M. Leveraging Blockchain for Transparency: A Study on Organ Supply Chains and Transplant Processes. Logistics 2025, 9, 9. https://doi.org/10.3390/logistics9010009
Panigrahi RR, Mukherjee S, Shaikh ZH, Nomran NM. Leveraging Blockchain for Transparency: A Study on Organ Supply Chains and Transplant Processes. Logistics. 2025; 9(1):9. https://doi.org/10.3390/logistics9010009
Chicago/Turabian StylePanigrahi, Rashmi Ranjan, Subhodeep Mukherjee, Zakir Hossen Shaikh, and Naji Mansour Nomran. 2025. "Leveraging Blockchain for Transparency: A Study on Organ Supply Chains and Transplant Processes" Logistics 9, no. 1: 9. https://doi.org/10.3390/logistics9010009
APA StylePanigrahi, R. R., Mukherjee, S., Shaikh, Z. H., & Nomran, N. M. (2025). Leveraging Blockchain for Transparency: A Study on Organ Supply Chains and Transplant Processes. Logistics, 9(1), 9. https://doi.org/10.3390/logistics9010009







