Effects of Diazinon Exposure on Urinary Shedding of Leptospira interrogans Serogroup Hebdomadis in Mice
Abstract
1. Introduction
2. Materials and Methods
2.1. Culture Conditions of L. interrogans
2.2. In Vitro Viability Assay of L. interrogans
2.3. Leptospira Infection and Exposure to DZN
2.4. DNA Extraction from Kidney and Urine Samples
2.5. RNA Extraction and cDNA Synthesis from Kidney
2.6. Real-Time PCR
2.7. Quantification of Leptospiral DNA in Kidney and Urine
2.8. Quantification of Expression Levels of Cytokine Genes in Kidney Tissues
2.9. Histological Examination of Kidney Tissue
2.10. Extraction and Quantification of DZN and IMP in Kidney Tissues, Urine, and EMJH Medium
2.11. Statistical Analysis
3. Results
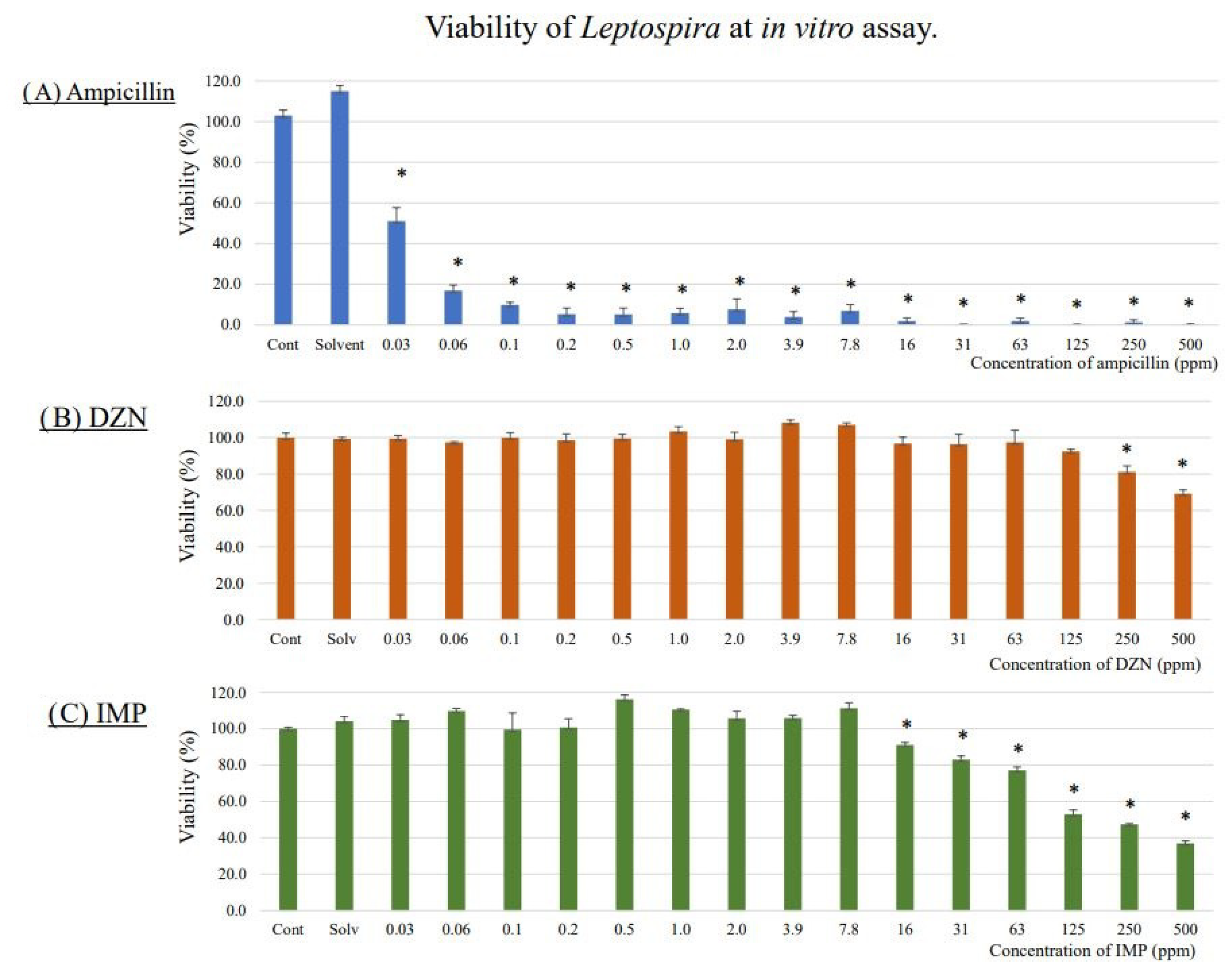
3.1. Lethal Concentrations of DZN and IMP for L. interrogans on In Vitro Assay
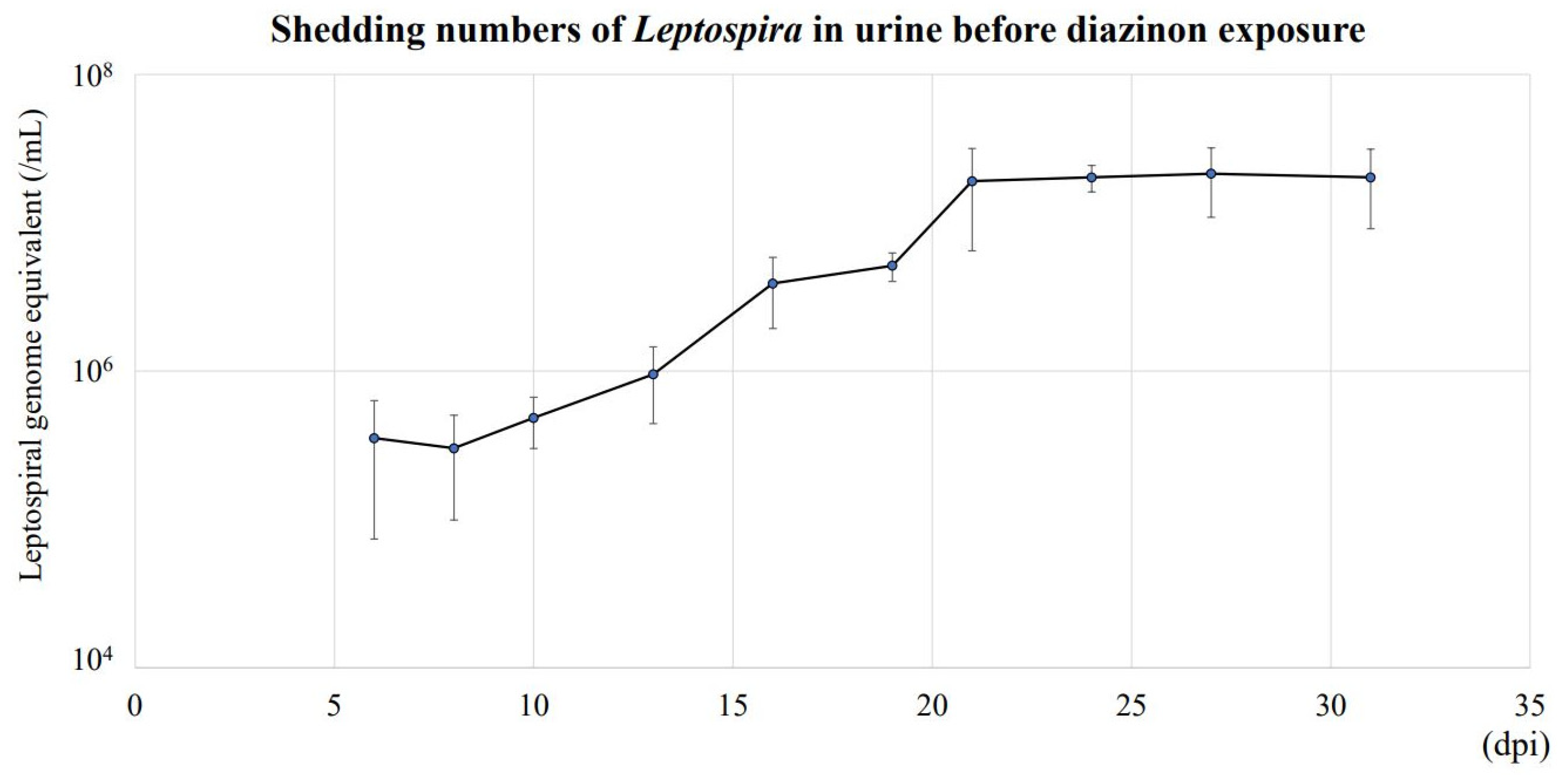
3.2. Urinary Shedding of L. interrogans in Mice Exposed to DZN
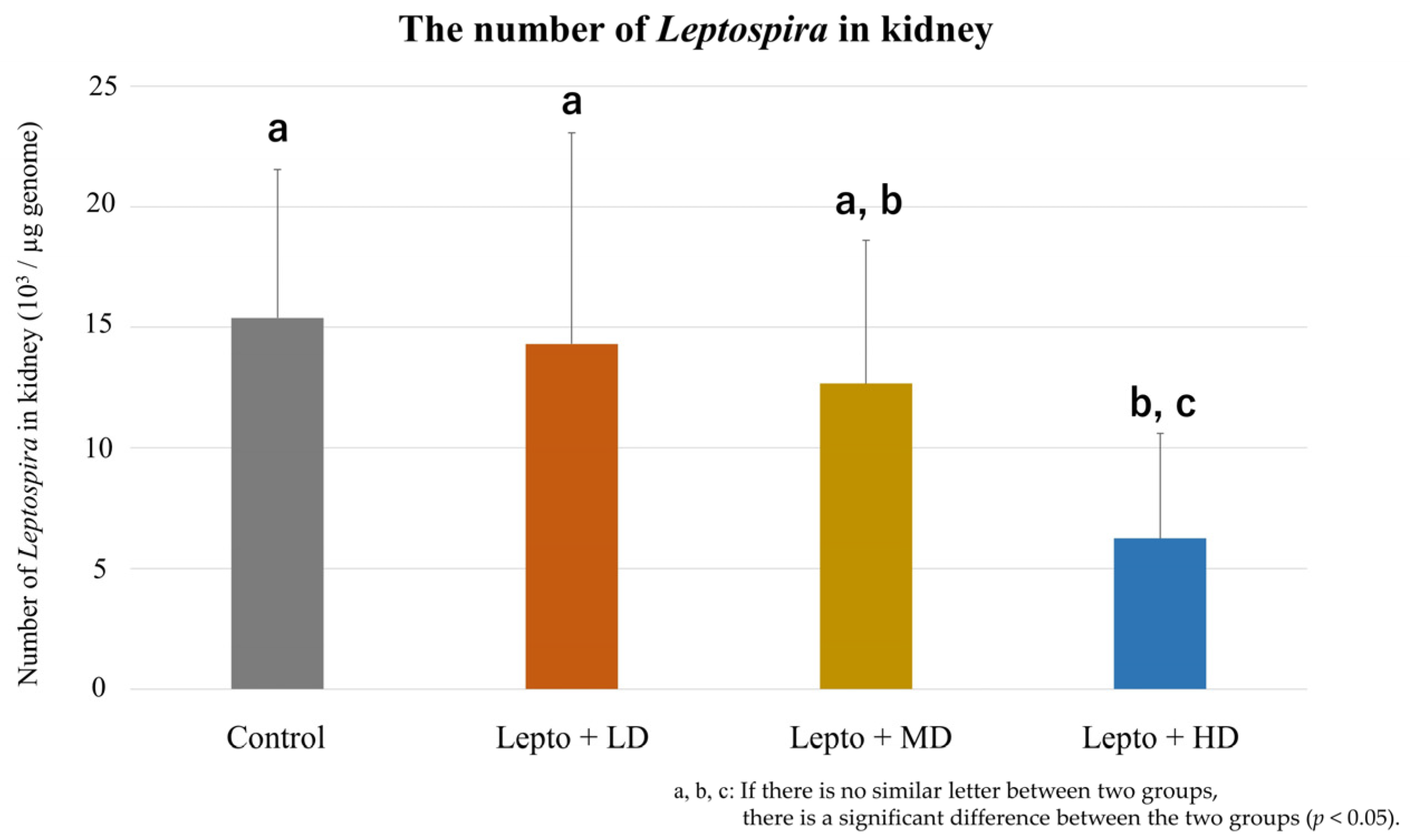
3.3. L. interrogans in Kidney Tissues of Mice Exposed to DZN
3.4. Concentrations of DZN and IMP in Kidney Tissue and Urine of Exposed Mice
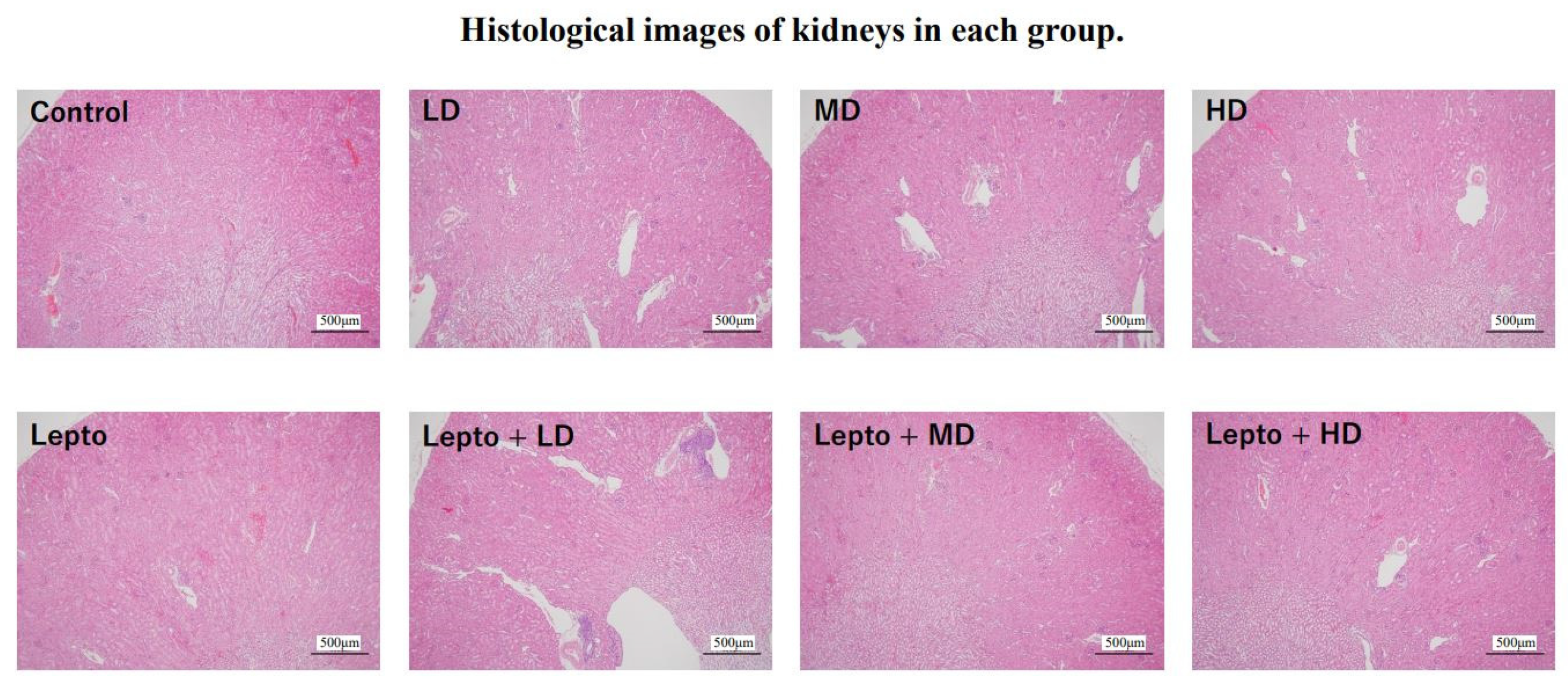
3.5. Pathological Characteristics of Kidney Tissues of Leptospira-Infected Mice Exposed to DZN
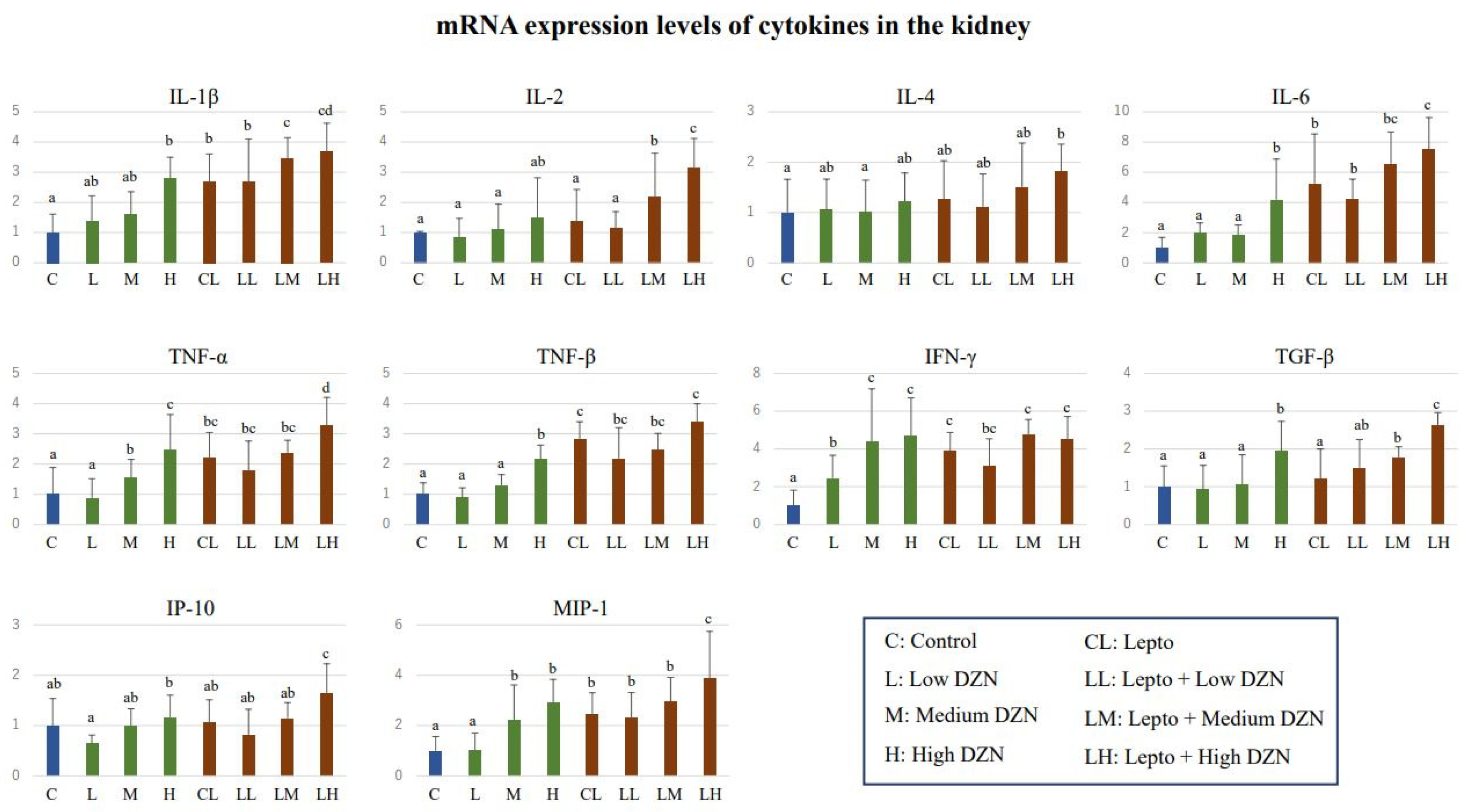
3.6. mRNA Expression Levels of Cytokine Genes in Kidney Tissue of DZN-Exposed Mice and Leptospira-Infected Mice Exposed to DZN
4. Discussion
4.1. Effect of DZN Exposure on Leptospira Proliferation in Kidney Tissue
4.2. Influence of DZN Exposure on the Infectious Risk of Leptospirosis in Human
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Bharti, A.R.; Nally, J.E.; Ricaldi, J.N.; Matthias, M.A.; Diaz, M.M.; Lovett, M.A.; Levett, P.N.; Gilman, R.H.; Willig, M.R.; Gotuzzo, E.; et al. Leptospirosis: A zoonotic disease of global importance. Lancet Infect. Dis. 2003, 3, 757–771. [Google Scholar] [CrossRef] [PubMed]
- Faine, S.; Adler, B.; Bolin, C.; Perolat, P. Leptospira and Leptospirosis, 2nd ed.; Medisci Press: Melbourne, Australia, 1999. [Google Scholar]
- Costa, F.; Wunder, E.A.; De Oliveira, D.; Bisht, V.; Rodrigues, G.; Reis, M.G.; Ko, A.I.; Begon, M.; Childs, J.E. Patterns in Leptospira shedding in Norway rats (Rattus norvegicus) from Brazilian slum communities at high risk of disease transmission. PLoS Negl. Trop. Dis. 2015, 9, e0003819. [Google Scholar] [CrossRef]
- Barragan, V.; Nieto, N.; Keim, P.; Pearson, T. Meta-analysis to estimate the load of Leptospira excreted in urine: Beyond rats as important sources of transmission in low-income rural communities. BMC Res. Notes 2017, 10, 71. [Google Scholar] [CrossRef] [PubMed]
- Berny, P. Pesticides and the intoxication of wild animals. J. Vet. Pharmacol. Ther. 2007, 30, 93–100. [Google Scholar] [CrossRef]
- Chi-Coyoc, T.; Segura, E.G.; Moncada, V.A.; Contreras, A.V.J.; Vela, E.C.G.; Reyna, L.J. Organochlorine and anticholinergic pesticides in wild mice from wetland ecosystems of the Gulf of Mexico. Therya 2016, 7, 465–482. [Google Scholar] [CrossRef]
- Herrera, A.M.; Segura, E.G.; Jauregui, G.M.; Hurtado, R.R.; Coutreras, A.V.J.; Von Osten, R.J. Presence of organochlorine pesticides and characterization of biomarkers in wild mice living in crop fields. Therya 2018, 9, 209–218. [Google Scholar] [CrossRef]
- Abbasian, H.; Ashayeri, A.; Hosseinmarzeh, S.; Meigooni, G.H. Residues of diazinon in ab-bandans supplied by Babolroud, Talar and Siaroud Riveers, Iran. J. Ecol. Nat. Environ. 2014, 6, 153–158. [Google Scholar]
- Aggarwal, V.; Deng, X.; Tuli, A.; Goh, K.S. Diazinon-chemistry and environmental fate: A California perspective. Rev. Environ. Contam. Toxicol. 2013, 223, 107–140. [Google Scholar] [PubMed]
- Karyab, H.; Mahvi, A.H.; Nazmara, S.; Bahojb, A. Determination of water sources contamination to diazinon and malathion and spatial pollution patterns in Qazvin, Iran. Bull. Environ. Contam. Toxicol. 2013, 90, 126–131. [Google Scholar] [CrossRef] [PubMed]
- Alluwaimi, A.M.; Hussein, Y. Diazinon immunotoxicity in mice: Modulation of cytokines level and their gene expression. Toxicology 2007, 236, 123–131. [Google Scholar] [CrossRef]
- Neishabouri, E.Z.; Hassan, Z.M.; Azizi, E.; Ostad, S.N. Evaluation of immunotoxicity induced by diazinon in C57bl/6 mice. Toxicology 2004, 196, 173–179. [Google Scholar] [CrossRef]
- Ali, I.N.; Salem, M.L.; Elateek, Y.S.; Khalil, K.B.W. Modulation impact of diazinon forms on gene expression profile and DNA damage pathway in male mice. J. Appl. Pharm. Sci. 2020, 10, 67–74. [Google Scholar]
- Maliji, G.; Jorsaraei, S.; Zabihi, E.; Fattahi, E.; Rezaie, E.; Sohan, F.A. Diazinon alters sex hormones, interferon-gamma, interleukin-4 and 10 in male Wister rats. J. Gonabad Univ. Med. Sci. Health Serv. 2014, 16, 22–28. [Google Scholar]
- Bavia, L.; de Castro, Í.A.; Amano, M.T.; da Silva, A.M.G.; Vasconcellos, S.A.; Isaac, L. Cytokine profile in early infection by Leptospira interrogans in A/J mice. J. Immunol. Res. 2019, 2019, 1892508. [Google Scholar] [CrossRef] [PubMed]
- Marinho, M.; Langoni, H.; Oliveira, S.L.; Lima, V.M.F.; Peiro, J.R.; Perri, S.H.V.; Carreira, R. Role of cytokines, NO, and H2O2 on the immunopathology of leptospirosis un genetically selected mice. J. Venom. Anim. Toxins Incl. Trop. Dis. 2005, 11, 198–212. [Google Scholar] [CrossRef]
- Monahan, A.M.; Callanan, J.J.; Nally, J.E. Review paper: Host-pathogen interactions in the kidney during chronic leptospirosis. Vet. Pathol. 2009, 46, 792–799. [Google Scholar] [CrossRef]
- Cakici, O.; Akat, E. Effects of oral exposure to diazinon on mice liver and kidney tissues: Biometric analyses of histopathologic changes. Anal. Quant. Cytopathol. Histpathol. 2013, 35, 7–16. [Google Scholar]
- Fujita, R.; Koizumi, N.; Sugiyama, H.; Tomizawa, R.; Sato, R.; Ohnishi, M. Comparison of bacterial burden and cytokine gene expression in golden hamsters in early phase of infection with two different strains of Leptospira interrogans. PLoS ONE 2015, 10, e0132694. [Google Scholar] [CrossRef]
- Mouville, C.; Benaroudj, N. Survival Tests for Leptospira spp. Methods Mol. Biol. 2020, 2134, 215–228. [Google Scholar]
- Murai, I.; Sugimoto, M.; Ikeda, S.; Kume, S. Effects of high potassium chloride supplementation on water intake, urine volume and nitrogen balance in mice. Anim. Sci. J. 2010, 81, 80–84. [Google Scholar] [CrossRef]
- Torabi, E.; Talebi, K. Diazinon residues and degradation kinetics for grapes under field conditions. J. Environ. Sci. Health B 2013, 48, 260–265. [Google Scholar] [CrossRef]
- Vellers, H.L.; Letsinger, A.C.; Walker, N.R.; Granados, J.Z.; Lightfoot, J.T. High fat high sugar diet reduces voluntary wheel running in mice independent of sex hormone involvement. Front. Physiol. 2017, 8, 628. [Google Scholar] [CrossRef]
- National Institute of Environmental Studies. Public Database for Food Nutrition Facts Supplied by Ministry of Education, Culture, Sports, Science, and Technology. Available online: https://fooddb.mext.go.jp (accessed on 24 August 2022).
- Soupé-Gilbert, M.E.; Bierque, E.; Geroult, S.; Teurlai, M.; Goarant, C. Continuous excretion of Leptospira borgpetersenii Ballum in mice assessed by viability quantitative polymerase chain reaction. Am. J. Trop. Med. Hyg. 2017, 97, 1088–1093. [Google Scholar] [CrossRef] [PubMed]
- Nascimento, A.L.; Verjovski-Almeida, S.; Van Sluys, M.A.; Monteiro-Vitorello, C.B.; Camargo, L.E.; Digiampietri, L.A.; Harstkeerl, R.A.; Ho, P.L.; Marques, M.V.; Oliveira, M.C.; et al. Genome features of Leptospira interrogans serovar Copenhageni. Braz. J. Med. Biol. Res. 2004, 37, 459–477. [Google Scholar] [CrossRef] [PubMed]
- Curthoys, N.P.; Moe, O.W. Proximal tubule function and response to acidosis. Clin. J. Am. Soc. Nephrol. 2014, 9, 1627–1638. [Google Scholar] [CrossRef]
- Van Vleet, T.R.; Schnellmann, R.G. Toxic nephropathy: Environmental chemicals. Semin. Nephrol. 2003, 23, 500–508. [Google Scholar] [CrossRef] [PubMed]
- Athanazio, D.A.; Silva, E.F.; Santos, C.S.; Rocha, G.M.; Vannier-Santos, M.A.; McBride, A.J.; Ko, A.I.; Reis, M.G. Rattus norvegicus as a model for persistent renal colonization by pathogenic Leptospira interrogans. Acta Trop. 2008, 105, 176–180. [Google Scholar] [CrossRef]
- Santos, A.A.; Figueira, C.P.; dos Reis, M.G.; Costa, F.; Ristow, P. Heterogenic colonization patterns by Leptospira interrogans in Rattus norvegicus from urban slums. Braz. J. Microbiol. 2015, 46, 1161–1164. [Google Scholar] [CrossRef]
- Oberholzer, A.; Oberholzer, C.; Moldawer, L.L. Cytokine signaling—regulation of the immune response in normal and critically ill states. Crit. Care Med. 2000, 28, N3–N12. [Google Scholar] [CrossRef]
- Schall, T.J.; Bacon, K.B. Chemokines, leukocyte trafficking, and inflammation. Curr. Opin. Immunol. 1994, 6, 865–873. [Google Scholar] [CrossRef]
- Muraguchi, A.; Hirano, T.; Tang, B.; Matsuda, T.; Horii, Y.; Nakajima, K.; Kishimoto, T. The essential role of B cell stimulatory factor 2 (BSF-2/IL-6) for the terminal differentiation of B cells. J. Exp. Med. 1988, 167, 332–344. [Google Scholar] [CrossRef] [PubMed]
- Shah, M.D.; Iqbal, M. Diazinon-induced oxidative stress and renal dysfunction in rats. Food Chem. Toxicol. 2010, 48, 3345–3353. [Google Scholar] [CrossRef] [PubMed]
- Minter, A.; Diggle, P.J.; Costa, F.; Childs, J.; Ko, A.I.; Begon, M. Evidence of multiple intraspecific transmission routes for Leptospira acquisition in Norway rats (Rattus norvegicus). Epidemiol. Infect. 2017, 145, 3438–3448. [Google Scholar] [CrossRef] [PubMed]
- Karesh, W.B.; Dobson, A.; Lloyd-Smith, J.O.; Lubroth, J.; Dixon, M.A.; Bennett, M.; Aldrich, S.; Harrington, T.; Formenty, P.; Loh, E.H.; et al. Ecology of zoonoses: Natural and unnatural histories. Lancet 2012, 380, 1936–1945. [Google Scholar] [CrossRef] [PubMed]
- Boyd, R.S. Heavy metal pollutants and chemical ecology: Exploring new frontiers. J. Chem. Ecol. 2010, 36, 46–58. [Google Scholar] [CrossRef]
- Corsini, E.; Sokooti, M.; Galli, C.L.; Moretto, A.; Colosio, C. Pesticide induced immunotoxicity in humans: A comprehensive review of the existing evidence. Toxicology 2013, 307, 123–135. [Google Scholar] [CrossRef]
- Suzuki, T.; Hidaka, T.; Kumagai, Y.; Yamamoto, M. Environmental pollutants and the immune response. Nat. Immunol. 2020, 21, 1486–1495. [Google Scholar] [CrossRef]

| Measured Concentration (ppm) * | |||
|---|---|---|---|
| Compound | Exposure Dose | Kidney | Urine |
| DZN | 0.2 mg/kg/day | 0.25 ± 0.10 | 0.07 ± 0.03 |
| 1.0 mg/kg/day | 1.03 ± 0.34 | 0.14 ± 0.07 | |
| 5.0 mg/kg/day | 2.21 ± 0.56 | 0.56 ± 0.27 | |
| IMP | 0.2 mg/kg/day | 0.23 ± 0.05 | 0.81 ± 0.19 |
| 1.0 mg/kg/day | 0.32 ± 0.09 | 2.57 ± 0.80 | |
| 5.0 mg/kg/day | 0.66 ± 0.12 | 12.51 ± 2.1 | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Shinya, S.; Muthusinghe, D.S.; Koizumi, N.; Yoshimatsu, K.; Nakayama, S.M.M.; Ishizuka, M.; Ikenaka, Y. Effects of Diazinon Exposure on Urinary Shedding of Leptospira interrogans Serogroup Hebdomadis in Mice. Toxics 2023, 11, 361. https://doi.org/10.3390/toxics11040361
Shinya S, Muthusinghe DS, Koizumi N, Yoshimatsu K, Nakayama SMM, Ishizuka M, Ikenaka Y. Effects of Diazinon Exposure on Urinary Shedding of Leptospira interrogans Serogroup Hebdomadis in Mice. Toxics. 2023; 11(4):361. https://doi.org/10.3390/toxics11040361
Chicago/Turabian StyleShinya, So, Devinda S. Muthusinghe, Nobuo Koizumi, Kumiko Yoshimatsu, Shouta M. M. Nakayama, Mayumi Ishizuka, and Yoshinori Ikenaka. 2023. "Effects of Diazinon Exposure on Urinary Shedding of Leptospira interrogans Serogroup Hebdomadis in Mice" Toxics 11, no. 4: 361. https://doi.org/10.3390/toxics11040361
APA StyleShinya, S., Muthusinghe, D. S., Koizumi, N., Yoshimatsu, K., Nakayama, S. M. M., Ishizuka, M., & Ikenaka, Y. (2023). Effects of Diazinon Exposure on Urinary Shedding of Leptospira interrogans Serogroup Hebdomadis in Mice. Toxics, 11(4), 361. https://doi.org/10.3390/toxics11040361










