Short-Term Relationship Between Air Pollution and Mortality from Respiratory and Cardiovascular Diseases in China, 2008–2020
Abstract
1. Introduction
2. Materials and Methods
2.1. Data Source and Quality Control
2.2. Environmental Assessment
2.3. Statistical Analysis
3. Results
3.1. General Characteristics of the Study Population
3.2. Air Pollution Exposure Levels
3.3. Percentage Increases in the Risk of Death from Respiratory Diseases and CVDs
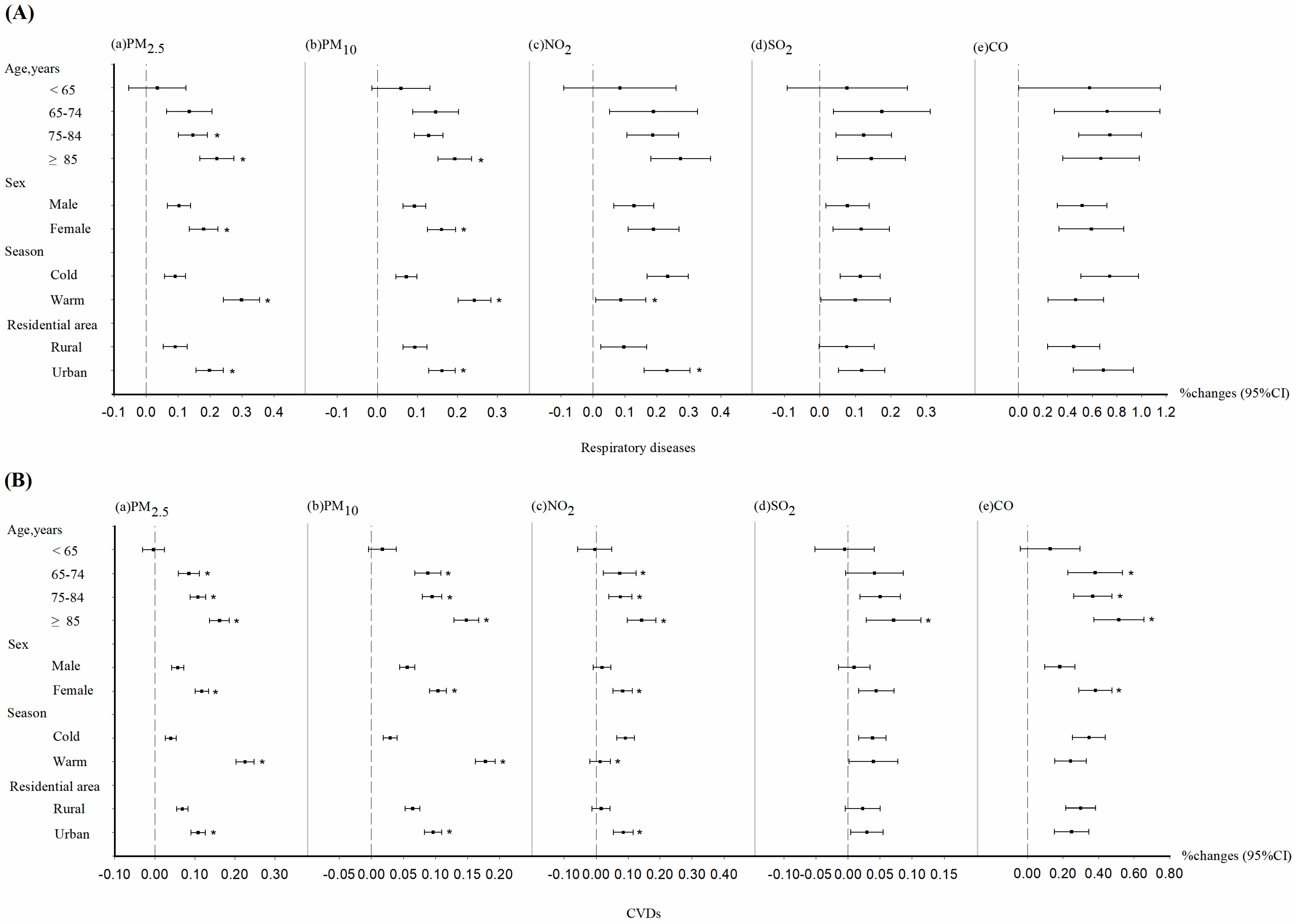
3.4. Stratified Analysis
3.5. Sensitivity Analysis
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- de Bont, J.; Jaganathan, S.; Dahlquist, M.; Persson, Å.; Stafoggia, M.; Ljungman, P. Ambient air pollution and cardiovascular diseases: An umbrella review of systematic reviews and meta-analyses. J. Intern. Med. 2022, 291, 779–800. [Google Scholar] [CrossRef] [PubMed]
- Institute for Health Metrics and Evaluation (IHME). Global Burden of Disease 2021: Findings from the GBD 2021 Study. [EB/OL]. Available online: https://www.healthdata.org/research-analysis/library/global-burden-disease-2021-findings-gbd-2021-study (accessed on 16 May 2024).
- Santos, U.d.P.; Arbex, M.A.; Braga, A.L.F.; Mizutani, R.F.; Cancado, J.E.D.; Terra-Filho, M.; Chatkin, J.M. Environmental air pollution: Respiratory effects. J. Bras. Pneumol. 2021, 47, e20200267. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. WHO Global Air Quality Guidelines: Particulate Matter (PM2.5 and PM10), Ozone, Nitrogen Dioxide, Sulfur Dioxide and Carbon Monoxide; World Health Organization: Geneva, Switzerland, 2021.
- Wang, H.; Yang, T.; Wang, Z.; Li, J.; Chai, W.; Tang, G.; Kong, L.; Chen, X. An aerosol vertical data assimilation system (NAQPMS-PDAF v1.0): Development and application. Geosci. Model. Dev. 2022, 15, 3555–3585. [Google Scholar] [CrossRef]
- Xie, J.; Tang, X.; Zheng, F.; Wang, X.; Ding, N.; Song, Y.; Luo, H.; Wu, H.; Kong, L.; Zhu, J.; et al. Improvement of the ozone forecast over Beijing through combining the chemical transport model with multiple machine learning methods. Atmos. Pollut. Res. 2024, 15, 102184. [Google Scholar] [CrossRef]
- Wang, Z.; Xie, F.Y.; Wang, X.; An, J.; Zhu, J. Development and application of nested air quality prediction modeling system. Chin. J. Atmos. Sci. 2006, 30, 778–790. [Google Scholar]
- Wu, R.; Song, X.; Wu, J.; Chen, D.; Huang, X.; Xu, H. Applicability evaluation of air quality spatiotemporal simulation data in environmental epidemiology study. J. Environ. Health 2020, 37, 941–946. [Google Scholar]
- Xu, H.; Song, J.; He, X.; Guan, X.; Wang, T.; Zhu, Y.; Xu, X.; Li, M.; Liu, L.; Zhang, B.; et al. Ambient Anthropogenic Carbons and Pediatric Respiratory Infections: A Case-Crossover Analysis in the Megacity Beijing. Geohealth 2023, 7, e2023GH000820. [Google Scholar] [CrossRef] [PubMed]
- Chen, R.; Jiang, Y.; Hu, J.; Chen, H.; Li, H.; Meng, X.; Ji, J.S.; Gao, Y.; Wang, W.; Liu, C.; et al. Hourly Air Pollutants and Acute Coronary Syndrome Onset in 1.29 Million Patients. Circulation 2022, 145, 1749–1760. [Google Scholar] [CrossRef]
- Orellano, P.; Reynoso, J.; Quaranta, N.; Bardach, A.; Ciapponi, A. Short-term exposure to particulate matter (PM10 and PM2.5), nitrogen dioxide (NO2), and ozone (O3) and all-cause and cause-specific mortality: Systematic review and meta-analysis. Environ. Int. 2020, 142, 105876. [Google Scholar] [CrossRef]
- Jia, Y.; Lin, Z.; He, Z.; Li, C.; Zhang, Y.; Wang, J.; Liu, F.; Li, J.; Huang, K.; Cao, J.; et al. Effect of Air Pollution on Heart Failure: Systematic Review and Meta-Analysis. Environ. Health Perspect. 2023, 131, 76001. [Google Scholar] [CrossRef]
- Di, Q.; Dai, L.; Wang, Y.; Zanobetti, A.; Choirat, C.; Schwartz, J.D.; Dominici, F. Association of Short-term Exposure to Air Pollution with Mortality in Older Adults. JAMA 2017, 318, 2446–2456. [Google Scholar] [CrossRef] [PubMed]
- Lin, H.; Guo, Y.; Zheng, Y.; Di, Q.; Liu, T.; Xiao, J.; Li, X.; Zeng, W.; Cummings-Vaughn, L.A.; Howard, S.W.; et al. Long-Term Effects of Ambient PM2.5 on Hypertension and Blood Pressure and Attributable Risk Among Older Chinese Adults. Hypertension 2017, 69, 806–812. [Google Scholar] [CrossRef] [PubMed]
- Strak, M.; Janssen, N.A.; Godri, K.J.; Gosens, I.; Mudway, I.S.; Cassee, F.R.; Lebret, E.; Kelly, F.J.; Harrison, R.M.; Brunekreef, B.; et al. Respiratory health effects of airborne particulate matter: The role of particle size, composition, and oxidative potential-the RAPTES project. Environ. Health Perspect. 2012, 120, 1183–1189. [Google Scholar] [CrossRef]
- Schwarz, M.; Peters, A.; Stafoggia, M.; De’Donato, F.; Sera, F.; Bell, M.L.; Guo, Y.; Honda, Y.; Huber, V.; Jaakkola, J.J.K.; et al. Temporal variations in the short-term effects of ambient air pollution on cardiovascular and respiratory mortality: A pooled analysis of 380 urban areas over a 22-year period. Lancet Planet. Health 2024, 8, e657–e665. [Google Scholar] [CrossRef]
- Chen, Y.; Chen, S.; Zhang, L.; Kang, W.; Lin, G.; Yang, Q. Association between ambient air pollutants and short-term mortality risks during 2015–2019 in Guangzhou, China. Front. Public Health 2024, 12, 1359567. [Google Scholar] [CrossRef]
- Brook, R.D.; Rajagopalan, S.; Pope, C.A., 3rd; Brook, J.R.; Bhatnagar, A.; Diez-Roux, A.V.; Holguin, F.; Hong, Y.; Luepker, R.V.; Mittleman, M.A.; et al. Particulate matter air pollution and cardiovascular disease: An update to the scientific statement from the American Heart Association. Circulation 2010, 121, 2331–2378. [Google Scholar] [CrossRef]
- Katsouyanni, K.; Touloumi, G.; Samoli, E.; Gryparis, A.; Le Tertre, A.; Monopolis, Y.; Rossi, G.; Zmirou, D.; Ballester, F.; Boumghar, A.; et al. Confounding and effect modification in the short-term effects of ambient particles on total mortality: Results from 29 European cities within the APHEA2 project. Epidemiology 2001, 12, 521–531. [Google Scholar] [CrossRef]
- Chen, R.; Yin, P.; Meng, X.; Wang, L.; Liu, C.; Niu, Y.; Liu, Y.; Liu, J.; Qi, J.; You, J.; et al. Associations between Coarse Particulate Matter Air Pollution and Cause-Specific Mortality: A Nationwide Analysis in 272 Chinese Cities. Environ. Health Perspect. 2019, 127, 17008. [Google Scholar] [CrossRef]
- Wu, C.; He, G.; Wu, W.; Meng, R.; Zhou, C.; Bai, G.; Yu, M.; Gong, W.; Huang, B.; Xiao, Y.; et al. Ambient PM2.5 and cardiopulmonary mortality in the oldest-old people in China: A national time-stratified case-crossover study. Med 2024, 5, 62–72. [Google Scholar] [CrossRef]
- Zhu, F.; Yu, H.; Fan, X.; Ding, Z.; Wang, Q.; Zhou, J. Particulate air pollution and cardiovascular disease mortality in Jiangsu Province, China: A time-series analysis between 2015 and 2021. Front. Public Health 2023, 11, 1218479. [Google Scholar] [CrossRef]
- Chen, R.; Yin, P.; Meng, X.; Liu, C.; Wang, L.; Xu, X.; Ross, J.A.; Tse, L.A.; Zhao, Z.; Kan, H.; et al. Fine Particulate Air Pollution and Daily Mortality. A Nationwide Analysis in 272 Chinese Cities. Am. J. Respir. Crit. Care Med. 2017, 196, 73–81. [Google Scholar] [CrossRef] [PubMed]
- Costa, A.F.; Hoek, G.; Brunekreef, B.; Ponce de Leon, A.C. Air Pollution and Deaths among Elderly Residents of São Paulo, Brazil: An Analysis of Mortality Displacement. Environ. Health Perspect. 2017, 125, 349–354. [Google Scholar] [CrossRef] [PubMed]
- Qiu, H.; Pun, V.C.; Tian, L. Short-term effects of fine and coarse particles on deaths in Hong Kong elderly population: An analysis of mortality displacement. Environ. Pollut. 2018, 241, 148–154. [Google Scholar] [CrossRef]
- Pan, W.; Wang, M.; Hu, Y.; Lian, Z.; Cheng, H.; Qin, J.-J.; Wan, J. The association between outdoor air pollution and body mass index, central obesity, and visceral adiposity index among middle-aged and elderly adults: A nationwide study in China. Front. Endocrinol. 2023, 14, 1221325. [Google Scholar] [CrossRef]
- Li, S.; Liu, Z.; Joseph, P.; Hu, B.; Yin, L.; Tse, L.A.; Rangarajan, S.; Wang, C.; Wang, Y.; Islam, S.; et al. Modifiable risk factors associated with cardiovascular disease and mortality in China: A PURE substudy. Eur. Heart J. 2022, 43, 2852–2863. [Google Scholar] [CrossRef]
- Yan, Y.; She, L.; Guo, Y.; Zhao, Y.; Zhang, P.; Xiang, B.; Zeng, J.; Yang, M.; Wang, L. Association between ambient air pollution and mortality from chronic obstructive pulmonary disease in Wuhan, China: A population-based time-series study. Environ. Sci. Pollut. Res. Int. 2021, 28, 33698–33706. [Google Scholar] [CrossRef]
- Zhang, P.; Dong, G.; Sun, B.; Zhang, L.; Chen, X.; Ma, N.; Yu, F.; Guo, H.; Huang, H.; Lee, Y.L.; et al. Long-term exposure to ambient air pollution and mortality due to cardiovascular disease and cerebrovascular disease in Shenyang, China. PLoS ONE 2011, 6, e20827. [Google Scholar] [CrossRef]
- McKenzie, R.; Burton, M.D.; Royce, S.G.; Tang, M.L.K.; Hons, M. Age and sex influences on airway hyperresponsiveness. J. Asthma 2010, 47, 651–654. [Google Scholar] [CrossRef]
- Kim, C.S.; Hu, S.C. Regional deposition of inhaled particles in human lungs: Comparison between men and women. J. Appl. Physiol. 1998, 84, 1834–1844. [Google Scholar] [CrossRef]
- Lee, H.; Myung, W.; Cheong, H.-K.; Yi, S.-M.; Hong, Y.-C.; Cho, S.-I.; Kim, H. Ambient air pollution exposure and risk of migraine: Synergistic effect with high temperature. Environ. Int. 2018, 121 Pt 1, 383–391. [Google Scholar] [CrossRef]
- Analitis, A.; Michelozzi, P.; D’ippoliti, D.; De’donato, F.; Menne, B.; Matthies, F.; Atkinson, R.W.; Iñiguez, C.; Basagaña, X.; Schneider, A.; et al. Effects of heat waves on mortality: Effect modification and confounding by air pollutants. Epidemiology 2014, 25, 15–22. [Google Scholar] [CrossRef] [PubMed]
- Gordon, C.J. Role of environmental stress in the physiological response to chemical toxicants. Environ. Res. 2003, 92, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Duan, Y.; Liao, Y.; Li, H.; Yan, S.; Zhao, Z.; Yu, S.; Fu, Y.; Wang, Z.; Yin, P.; Cheng, J.; et al. Effect of changes in season and temperature on cardiovascular mortality associated with nitrogen dioxide air pollution in Shenzhen, China. Sci. Total Environ. 2019, 697, 134051. [Google Scholar] [CrossRef] [PubMed]
- Zeng, J.; Lin, G.; Dong, H.; Li, M.; Ruan, H.; Yang, J. Association Between Nitrogen Dioxide Pollution and Cause-Specific Mortality in China: Cross-Sectional Time Series Study. JMIR Public Health Surveill. 2024, 10, e44648. [Google Scholar] [CrossRef]
- Ni, W.; Breitner, S.; Nikolaou, N.; Wolf, K.; Zhang, S.; Peters, A.; Herder, C.; Schneider, A. Effects of Short- and Medium-Term Exposures to Lower Air Temperature on 71 Novel Biomarkers of Subclinical Inflammation: Results from the KORA F4 Study. Environ. Sci. Technol. 2023, 57, 12210–12221. [Google Scholar] [CrossRef]
- Sicard, P.; Agathokleous, E.; De Marco, A.; Paoletti, E.; Calatayud, V. Calatayud V. Urban population exposure to air pollution in Europe over the last decades. Environ. Sci. Eur. 2021, 33, 28. [Google Scholar] [CrossRef]
- Pugh, T.A.M.; MacKenzie, A.R.; Whyatt, J.D.; Hewitt, C.N. Effectiveness of green infrastructure for improvement of air quality in urban street canyons. Environ. Sci. Technol. 2012, 46, 7692–7699. [Google Scholar] [CrossRef]
- Liu, M.; Huang, Y.; Ma, Z.; Jin, Z.; Liu, X.; Wang, H.; Liu, Y.; Wang, J.; Jantunen, M.; Bi, J.; et al. Spatial and temporal trends in the mortality burden of air pollution in China: 2004–2012. Environ. Int. 2017, 98, 75–81. [Google Scholar] [CrossRef]
- Hankey, S.; Marshall, J.D. Urban Form, Air Pollution, and Health. Curr. Environ. Health Rep. 2017, 4, 491–503. [Google Scholar] [CrossRef]
- Liu, T.; Meng, H.; Yu, M.; Xiao, Y.; Huang, B.; Lin, L.; Zhang, H.; Hu, R.; Hou, Z.; Xu, Y.; et al. Urban-rural disparity of the short-term association of PM2.5 with mortality and its attributable burden. Innovation 2021, 2, 100171. [Google Scholar] [CrossRef]
- Brugha, R.; Grigg, J. Urban air pollution and respiratory infections. Paediatr. Respir. Rev. 2014, 15, 194–199. [Google Scholar] [CrossRef]
- Zhao, S.; Liu, S.; Hou, X.; Sun, Y.; Beazley, R. Air pollution and cause-specific mortality: A comparative study of urban and rural areas in China. Chemosphere 2021, 262, 127884. [Google Scholar] [CrossRef]

| Variables | Respiratory Diseases | CVDs |
|---|---|---|
| Total | 7,171,833 | 30,339,986 |
| Sex | ||
| Male | 4,201,902 | 16,613,491 |
| Female | 2,969,931 | 13,726,495 |
| Age (years) | ||
| <65 | 892,402 | 5,963,697 |
| 65–74 | 1,331,472 | 6,447,635 |
| 75–84 | 2,837,174 | 10,734,098 |
| ≥85 | 2,110,785 | 7,194,556 |
| Residential area | ||
| Urban | 2,796,900 | 11,780,344 |
| Rural | 4,374,933 | 18,559,642 |
| Cause of death | ||
| Pneumonia | 1,125,243 | |
| Chronic obstructive pulmonary disease (COPD) | 5,052,902 | |
| Chronic bronchitis (CB) | 1,090,813 | |
| Emphysema | 436,005 | |
| Asthma | 149,063 | |
| Other Respiratory diseases | 844,625 | |
| Rheumatic heart disease (RHD) | 448,467 | |
| Hypertensive heart disease (HHB) | 2,982,601 | |
| Ischemic heart disease (IHD) | 10,761,227 | |
| Cerebrovascular disease | 13,741,489 | |
| Inflammatory heart diseases | 150,351 | |
| Other CVDs | 2,255,851 |
| Exposure | Respiratory Diseases | CVDs | ||
|---|---|---|---|---|
| Mean (SD), μg/m3 | Median (IQR) [Difference], μg/m3 | Mean (SD), μg/m3 | Median (IQR) [Difference], μg/m3 | |
| Case days | ||||
| PM2.5 | 49.67 (35.84) | 40.45 (41.44) | 50.97 (37.21) | 41.32 (43.25) |
| PM10 | 65.43 (44.72) | 54.41 (52.86) | 68.72 (46.65) | 57.62 (56.42) |
| NO2 | 30.47 (22.59) | 25.06 (30.87) | 31.71 (22.49) | 26.95 (31.31) |
| SO2 | 21.43 (21.12) | 21.43 (20.47) | 22.52 (22.21) | 22.52 (21.99) |
| CO | 0.78 (0.46) | 0.78 (0.53) | 0.79 (0.47) | 0.79 (0.54) |
| Control days | ||||
| PM2.5 | 49.35 (35.75) | 40.10 (41.20) | 50.69 (37.14) | 41.01 (43.06) |
| PM10 | 65.04 (44.59) | 53.97 (52.50) | 68.37 (46.56) | 57.21 (56.15) |
| NO2 | 30.37 (22.53) | 24.96 (30.76) | 31.62 (22.44) | 26.86 (31.22) |
| SO2 | 21.34 (21.05) | 21.34 (20.40) | 22.43 (22.15) | 22.43 (21.91) |
| CO | 0.78 (0.46) | 0.78 (0.53) | 0.79 (0.47) | 0.79 (0.54) |
| Respiratory Diseases | CVDs | ||||||
|---|---|---|---|---|---|---|---|
| All Participants | Subgroup | All Participants | Subgroup | ||||
| Urban | Rural | Urban | Rural | ||||
| PM2.5 | 0.12 (0.09, 0.14) | 0.20 (0.16, 0.24) | 0.09 (0.05, 0.13) | PM2.5 | 0.08 (0.07, 0.09) | 0.11 (0.09, 0.13) | 0.07 (0.05, 0.08) |
| +NO2 | 0.12 (0.09, 0.15) | 0.18 (0.12, 0.23) | 0.09 (0.05, 0.14) | +NO2 | 0.10 (0.09, 0.12) | 0.12 (0.10, 0.14) | 0.10 (0.08, 0.12) |
| +SO2 | 0.14 (0.11, 0.17) | 0.22 (0.17, 0.27) | 0.10 (0.06, 0.15) | +SO2 | 0.10 (0.09, 0.12) | 0.14 (0.12, 0.16) | 0.09 (0.08, 0.11) |
| +CO | 0.10 (0.07, 0.13) | 0.18 (0.13, 0.23) | 0.07 (0.03, 0.11) | +CO | 0.07 (0.06, 0.09) | 0.11 (0.09, 0.14) | 0.06 (0.04, 0.07) |
| PM10 | 0.10 (0.08, 0.12) | 0.16 (0.13, 0.19) | 0.09 (0.06, 0.12) | PM10 | 0.07 (0.06, 0.08) | 0.10 (0.08, 0.11) | 0.06 (0.05, 0.08) |
| +NO2 | 0.11 (0.08, 0.13) | 0.15 (0.11, 0.19) | 0.10 (0.07, 0.14) | +NO2 | 0.09 (0.08, 0.10) | 0.11 (0.09, 0.13) | 0.10 (0.08, 0.11) |
| +SO2 | 0.11 (0.09, 0.14) | 0.17 (0.14, 0.21) | 0.11 (0.07, 0.15) | +SO2 | 0.09 (0.08, 0.10) | 0.12 (0.10, 0.13) | 0.09 (0.07, 0.10) |
| +CO | 0.09 (0.07, 0.11) | 0.15 (0.11, 0.19) | 0.08 (0.05, 0.11) | NO2 | 0.03 (0.05, 0.14) | 0.08 (0.05, 0.12) | 0.02 (−0.01, 0.04) |
| NO2 | 0.10 (0.05, 0.14) | 0.23 (0.16, 0.30) | 0.10 (0.02, 0.17) | +PM2.5 | −0.08 (−0.11, −0.06) | −0.04 (−0.08, 0.00) | −0.11 (−0.15, −0.07) |
| +PM2.5 | −0.02 (−0.08, 0.03) | 0.06 (−0.03, 0.15) | −0.01 (−0.09, 0.08) | +PM10 | −0.10 (−0.12, −0.07) | −0.06 (−0.10, −0.02) | −0.13 (−0.17, −0.10) |
| +PM10 | −0.03 (−0.09, 0.03) | 0.05 (−0.04, 0.13) | −0.05 (−0.13, 0.04) | +CO | 0.00 (−0.02, 0.02) | 0.06 (0.03, 0.10) | −0.03 (−0.06, 0.04) |
| +SO2 | 0.10 (0.04, 0.16) | 0.25 (0.16, 0.34) | 0.09 (0.00, 0.18) | SO2 | 0.02 (0.00, 0.03) | 0.03 (0.00, 0.05) | 0.02 (0.00, 0.05) |
| +CO | 0.06 (0.01, 0.11) | 0.18 (0.01, 0.26) | 0.05 (−0.03, 0.12) | +PM2.5 | −0.08 (−0.10, −0.06) | −0.08 (−0.11, −0.05) | −0.08 (−0.12, −0.05) |
| SO2 | 0.05 (0.01, 0.10) | 0.12 (0.05, 0.18) | 0.08 (0.00, 0.15) | +PM10 | −0.08 (−0.10, −0.06) | −0.08 (−0.11, −0.05) | −0.09 (−0.12, −0.06) |
| +PM2.5 | −0.07 (−0.12, −0.02) | −0.06 (−0.14, 0.02) | −0.05 (−0.14, 0.05) | +CO | −0.01 (−0.03, 0.01) | 0.01 (−0.02, 0.03) | −0.02 (−0.05, 0.01) |
| +PM10 | −0.06 (−0.11, 0.06) | −0.05 (−0.12, 0.03) | −0.08 (−0.17, 0.01) | CO | 0.22 (0.16, 0.28) | 0.25 (0.15, 0.34) | 0.30 (0.22, 0.38) |
| +NO2 | −0.01 (−0.06, 0.05) | −0.02 (−0.11, 0.06) | 0.02 (−0.08, 0.12) | +PM2.5 | 0.03 (−0.04, 0.10) | −0.04 (−0.15, 0.08) | 0.14 (0.04, 0.24) |
| +CO | 0.02 (−0.03, 0.06) | 0.06 (−0.01, 0.13) | 0.02 (−0.06, 0.10) | +NO2 | 0.22 (0.15, 0.28) | 0.17 (0.06, 0.28) | 0.34 (0.24, 0.43) |
| CO | 0.40 (0.25, 0.54) | 0.69 (0.45, 0.93) | 0.45 (0.24, 0.66) | +SO2 | 0.23 (0.17, 0.30) | 0.24 (0.13, 0.34) | 0.32 (0.23, 0.42) |
| +PM2.5 | 0.14 (−0.02, 0.31) | 0.22 (−0.06, 0.50) | 0.28 (0.04, 0.51) | ||||
| +PM10 | 0.11 (−0.05, 0.28) | 0.19 (−0.08, 0.47) | 0.20 (−0.03, 0.44) | ||||
| +NO2 | 0.32 (0.17, 0.48) | 0.45 (0.18, 0.72) | 0.40 (0.17, 0.63) | ||||
| +SO2 | 0.38 (0.22, 0.53) | 0.61 (0.35, 0.87) | 0.43 (0.20, 0.66) | ||||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Liu, Y.; Shan, X.; Sun, Y.; Guan, X.; Wang, L.; He, X.; Liu, J.; You, J.; Wu, R.; Wu, J.; et al. Short-Term Relationship Between Air Pollution and Mortality from Respiratory and Cardiovascular Diseases in China, 2008–2020. Toxics 2025, 13, 156. https://doi.org/10.3390/toxics13030156
Liu Y, Shan X, Sun Y, Guan X, Wang L, He X, Liu J, You J, Wu R, Wu J, et al. Short-Term Relationship Between Air Pollution and Mortality from Respiratory and Cardiovascular Diseases in China, 2008–2020. Toxics. 2025; 13(3):156. https://doi.org/10.3390/toxics13030156
Chicago/Turabian StyleLiu, Yunning, Xuyang Shan, Yitong Sun, Xinpeng Guan, Lijun Wang, Xinghou He, Jiangmei Liu, Jinling You, Rongshan Wu, Jianbin Wu, and et al. 2025. "Short-Term Relationship Between Air Pollution and Mortality from Respiratory and Cardiovascular Diseases in China, 2008–2020" Toxics 13, no. 3: 156. https://doi.org/10.3390/toxics13030156
APA StyleLiu, Y., Shan, X., Sun, Y., Guan, X., Wang, L., He, X., Liu, J., You, J., Wu, R., Wu, J., Zhang, B., Qi, J., Yin, P., Li, M., He, X., Wang, Z., Xu, H., Wu, J., & Huang, W. (2025). Short-Term Relationship Between Air Pollution and Mortality from Respiratory and Cardiovascular Diseases in China, 2008–2020. Toxics, 13(3), 156. https://doi.org/10.3390/toxics13030156




