Food Contaminants Effects on an In Vitro Model of Human Intestinal Epithelium
Abstract
:1. Introduction
2. Materials and Methods
2.1. Cell Culture Conditions
2.2. Pro-Inflammatory Cytokines Stimulation of the Caco2/TC7 and HT29/MTX Co-Culture
2.2.1. Comparison of the Mono-Culture and the Co-Culture Sensitivity to Pro-Inflammatory Cytokines
Modulation by the Cocktail of Cytokines of the Expression of Genes Coding for Proteins of the Pro-Inflammatory and Pro-Apoptotic Pathways
Chemokine Secretion Following a Cell Stimulation
2.3. Effects of Food Contaminants on the Co-Culture Model
2.3.1. Viability of Caco2/TC7 Mono-Culture after Exposure to Food Contaminants
2.3.2. Assessment of the Alteration of the Barrier Function by the Food Contaminants
Effects of the Food Contaminants on the Paracellular Permeability
Effects of the Food Contaminants on the Expression of Genes Coding for Tight Junctions and Mucins
2.3.3. Modulation of Pro-Inflammatory and Pro-Apoptotic Signaling Pathways by the Food Contaminants
2.4. Statistical Analyses
3. Results
3.1. Pro-Inflammatory Cytokines Stimulation of the Mono- and the Co-Culture
3.1.1. Comparison of the Mono and Co-Culture Sensitivity to Pro-Inflammatory Cytokines
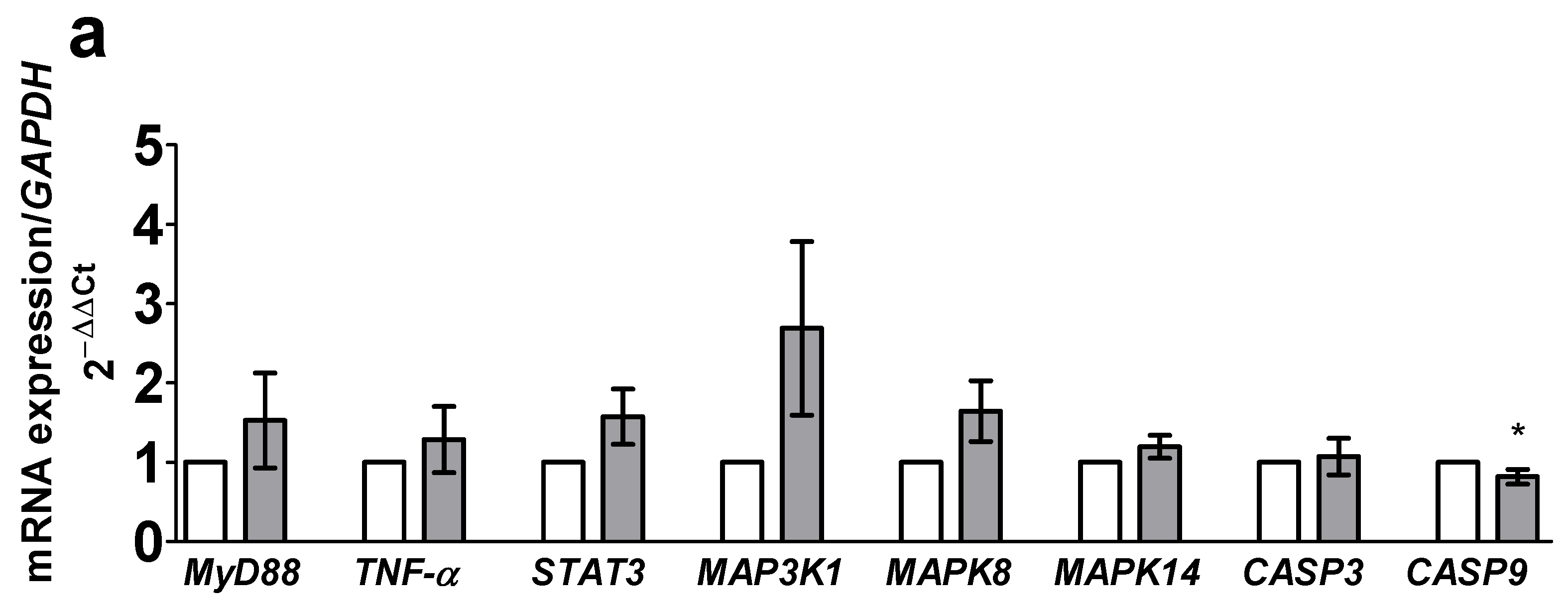
3.1.2. Modulation by the Cocktail of Cytokines of the Expression of Genes Coding for Proteins of the Pro-Inflammatory and Pro-Apoptotic Pathways
3.2. Effects of the Food Contaminants on the Mono- and Co-Culture
3.2.1. Viability of the Mono-Culture after Exposure to Food Contaminants
3.2.2. Assessment of the Alteration of the Barrier Function by the Food Contaminants
Effects of Food Contaminants on the Epithelial Permeability
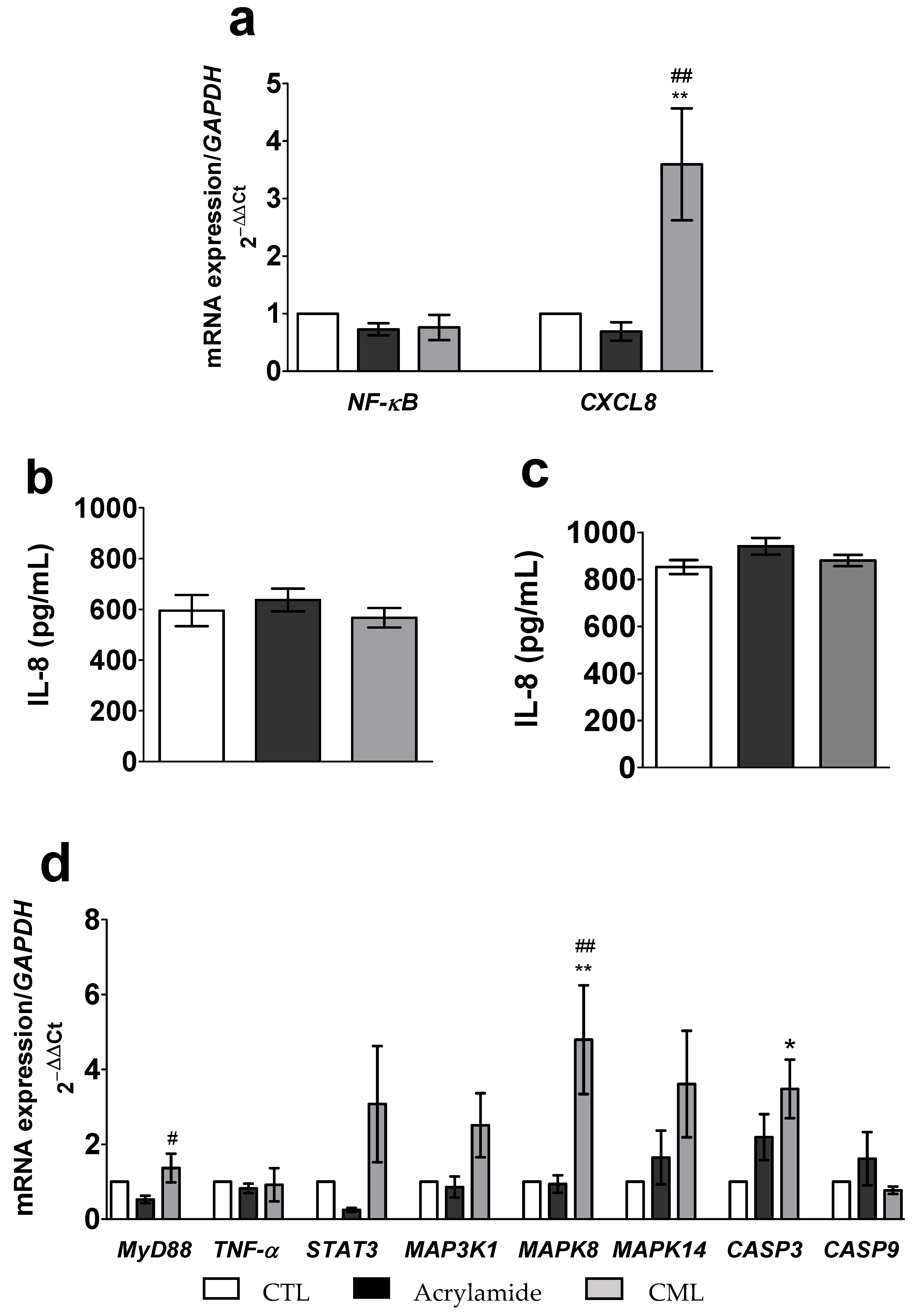
Modulation of Pro-Inflammatory and Pro-Apoptotic Signaling Pathways by the Food Contaminants
3.2.3. Effects of the Glycotoxins on the Caco2/TC7 and HT29/MTX Co-Culture
Effects of the Glycotoxins on the Intestinal Barrier Function
Effects of the Glycotoxins on the Expression of Key Genes Involved in the Pro-Inflammatory and Pro-Apoptotic Signaling Pathways
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Costa, L.G. Organophosphorus Compounds at 80: Some Old and New Issues. Toxicol. Sci. 2018, 162, 24–35. [Google Scholar] [CrossRef] [Green Version]
- Murata, M. Browning and Pigmentation in Food through the Maillard Reaction. Glycoconj. J. 2021, 38, 283–292. [Google Scholar] [CrossRef]
- Darwiche, W.; Delanaud, S.; Dupont, S.; Ghamlouch, H.; Ramadan, W.; Joumaa, W.; Bach, V.; Gay-Quéheillard, J. Impact of Prenatal and Postnatal Exposure to the Pesticide Chlorpyrifos on the Contraction of Rat Ileal Muscle Strips: Involvement of an Inducible Nitric Oxide Synthase-Dependent Pathway. Neurogastroenterol. Motil. 2017, 29, e12918. [Google Scholar] [CrossRef]
- El Sabbouri, H.E.K.; Gay-Quéheillard, J.; Joumaa, W.H.; Delanaud, S.; Guibourdenche, M.; Darwiche, W.; Djekkoun, N.; Bach, V.; Ramadan, W. Does the Perigestational Exposure to Chlorpyrifos and/or High-Fat Diet Affect Respiratory Parameters and Diaphragmatic Muscle Contractility in Young Rats? Food Chem. Toxicol. 2020, 140, 111322. [Google Scholar] [CrossRef]
- Joly Condette, C.; Bach, V.; Mayeur, C.; Gay-Quéheillard, J.; Khorsi-Cauet, H. Chlorpyrifos Exposure During Perinatal Period Affects Intestinal Microbiota Associated With Delay of Maturation of Digestive Tract in Rats. J. Pediatr. Gastroenterol. Nutr. 2015, 61, 30–40. [Google Scholar] [CrossRef]
- Condette, C.J.; Khorsi-Cauet, H.; Morlière, P.; Zabijak, L.; Reygner, J.; Bach, V.; Gay-Quéheillard, J. Increased Gut Permeability and Bacterial Translocation after Chronic Chlorpyrifos Exposure in Rats. PLoS ONE 2014, 9, e102217. [Google Scholar] [CrossRef]
- Tirelli, V.; Catone, T.; Turco, L.; Di Consiglio, E.; Testai, E.; De Angelis, I. Effects of the Pesticide Clorpyrifos on an in Vitro Model of Intestinal Barrier. Toxicol. In Vitro 2007, 21, 308–313. [Google Scholar] [CrossRef]
- Nowotny, K.; Schröter, D.; Schreiner, M.; Grune, T. Dietary Advanced Glycation End Products and Their Relevance for Human Health. Ageing Res. Rev. 2018, 47, 55–66. [Google Scholar] [CrossRef]
- Takeuchi, M. Toxic AGEs (TAGE) Theory: A New Concept for Preventing the Development of Diseases Related to Lifestyle. Diabetol. Metab. Syndr. 2020, 12, 105. [Google Scholar] [CrossRef] [PubMed]
- Clarke, R.E.; Dordevic, A.L.; Tan, S.M.; Ryan, L.; Coughlan, M.T. Dietary Advanced Glycation End Products and Risk Factors for Chronic Disease: A Systematic Review of Randomised Controlled Trials. Nutrients 2016, 8, 125. [Google Scholar] [CrossRef] [Green Version]
- Nowotny, K.; Jung, T.; Höhn, A.; Weber, D.; Grune, T. Advanced Glycation End Products and Oxidative Stress in Type 2 Diabetes Mellitus. Biomolecules 2015, 5, 194–222. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cencič, A.; Langerholc, T. Functional Cell Models of the Gut and Their Applications in Food Microbiology—A Review. Int. J. Food Microbiol. 2010, 141, S4–S14. [Google Scholar] [CrossRef] [PubMed]
- Ponce de León-Rodríguez, M.d.C.; Guyot, J.-P.; Laurent-Babot, C. Intestinal in Vitro Cell Culture Models and Their Potential to Study the Effect of Food Components on Intestinal Inflammation. Crit. Rev. Food Sci. Nutr. 2019, 59, 3648–3666. [Google Scholar] [CrossRef] [PubMed]
- Engle, M.J.; Goetz, G.S.; Alpers, D.H. Caco-2 Cells Express a Combination of Colonocyte and Enterocyte Phenotypes. J. Cell. Physiol. 1998, 174, 362–369. [Google Scholar] [CrossRef]
- Li, N.; Lewis, P.; Samuelson, D.; Liboni, K.; Neu, J. Glutamine Regulates Caco-2 Cell Tight Junction Proteins. Am. J. Physiol. Liver Physiol. 2004, 287, G726–G733. [Google Scholar] [CrossRef] [Green Version]
- Salvini, S.; Charbonnier, M.; Defoort, C.; Alquier, C.; Lairon, D. Functional Characterization of Three Clones of the Human Intestinal Caco-2 Cell Line for Dietary Lipid Processing. Br. J. Nutr. 2002, 87, 211–217. [Google Scholar] [CrossRef]
- Huet, C.; Sahuquillo-Merino, C.; Coudrier, E.; Louvard, D. Absorptive and Mucus-Secreting Subclones Isolated from a Multipotent Intestinal Cell Line (HT-29) Provide New Models for Cell Polarity and Terminal Differentiation. J. Cell Biol. 1987, 105, 345–357. [Google Scholar] [CrossRef] [Green Version]
- Mahler, G.J.; Shuler, M.L.; Glahn, R.P. Characterization of Caco-2 and HT29-MTX Cocultures in an in Vitro Digestion/Cell Culture Model Used to Predict Iron Bioavailability. J. Nutr. Biochem. 2009, 20, 494–502. [Google Scholar] [CrossRef]
- Béduneau, A.; Tempesta, C.; Fimbel, S.; Pellequer, Y.; Jannin, V.; Demarne, F.; Lamprecht, A. A Tunable Caco-2/HT29-MTX Co-Culture Model Mimicking Variable Permeabilities of the Human Intestine Obtained by an Original Seeding Procedure. Eur. J. Pharm. Biopharm. 2014, 87, 290–298. [Google Scholar] [CrossRef]
- Mitsou, E.; Dupin, A.; Sassi, A.H.; Monteil, J.; Sotiroudis, G.T.; Leal-Calderon, F.; Xenakis, A. Hydroxytyrosol Encapsulated in Biocompatible Water-in-Oil Microemulsions: How the Structure Affects in Vitro Absorption. Colloids Surf. B Biointerfaces 2019, 184, 110482. [Google Scholar] [CrossRef]
- Kiu, H.; Nicholson, S.E. Biology and Significance of the JAK/STAT Signalling Pathways. Growth Factors 2012, 30, 88–106. [Google Scholar] [CrossRef] [Green Version]
- Wakeman, D.; Schneider, J.E.; Liu, J.; Wandu, W.S.; Erwin, C.R.; Guo, J.; Stappenbeck, T.S.; Warner, B.W. Deletion of P38-Alpha MAPK within the Intestinal Epithelium Promotes Colon Tumorigenesis. Surgery 2012, 152, 286–293. [Google Scholar] [CrossRef] [Green Version]
- Heneghan, A.F.; Pierre, J.F.; Kudsk, K.A. JAK-STAT and Intestinal Mucosal Immunology. JAKSTAT 2013, 2, e25530. [Google Scholar] [CrossRef] [Green Version]
- Rodríguez-Ramiro, I.; Ramos, S.; Bravo, L.; Goya, L.; Martín, M.Á. Procyanidin B2 and a Cocoa Polyphenolic Extract Inhibit Acrylamide-Induced Apoptosis in Human Caco-2 Cells by Preventing Oxidative Stress and Activation of JNK Pathway. J. Nutr. Biochem. 2011, 22, 1186–1194. [Google Scholar] [CrossRef] [Green Version]
- Marion, R.; Coëffier, M.M.; Gargala, G.; Ducrotté, P.; Déchelotte, P.P. Glutamine and CXC Chemokines IL-8, Mig, IP-10 and I-TAC in Human Intestinal Epithelial Cells. Clin. Nutr. 2004, 23, 579–585. [Google Scholar] [CrossRef]
- Van De Walle, J.; Hendrickx, A.; Romier, B.; Larondelle, Y.; Schneider, Y.-J. Inflammatory Parameters in Caco-2 Cells: Effect of Stimuli Nature, Concentration, Combination and Cell Differentiation. Toxicol. In Vitro 2010, 24, 1441–1449. [Google Scholar] [CrossRef]
- Holik, A.-K.; Lieder, B.; Kretschy, N.; Somoza, M.M.; Ley, J.P.; Hans, J.; Somoza, V. The Advanced Glycation End Product Nϵ -Carboxymethyllysine and Its Precursor Glyoxal Increase Serotonin Release from Caco-2 Cells. J. Cell. Biochem. 2018, 119, 2731–2741. [Google Scholar] [CrossRef] [Green Version]
- Palumbo, P.; Lombardi, F.; Cifone, M.G.; Cinque, B. The Epithelial Barrier Model Shows That the Properties of VSL#3 Depend from Where It Is Manufactured. Endocr. Metab. Immune Disord. Drug Targets 2019, 19, 199–206. [Google Scholar] [CrossRef] [PubMed]
- Wikman-Larhed, A.; Artursson, P. Co-Cultures of Human Intestinal Goblet (HT29-H) and Absorptive (Caco-2) Cells for Studies of Drug and Peptide Absorption. Eur. J. Pharm. Sci. 1995, 3, 171–183. [Google Scholar] [CrossRef]
- Walter, E.; Janich, S.; Roessler, B.J.; Hilfinger, J.M.; Amidon, G.L. HT29-MTX/Caco-2 Cocultures as an in Vitro Model for the Intestinal Epithelium: In Vitro–in Vivo Correlation with Permeability Data from Rats and Humans. J. Pharm. Sci. 1996, 85, 1070–1076. [Google Scholar] [CrossRef] [PubMed]
- Hilgendorf, C.; Spahn-Langguth, H.; Regårdh, C.G.; Lipka, E.; Amidon, G.L.; Langguth, P. Caco-2 versus Caco-2/HT29-MTX Co-cultured Cell Lines: Permeabilities Via Diffusion, Inside- and Outside-Directed Carrier-Mediated Transport. J. Pharm. Sci. 2000, 89, 63–75. [Google Scholar] [CrossRef]
- Nollevaux, G.; Devillé, C.; El Moualij, B.; Zorzi, W.; Deloyer, P.; Schneider, Y.-J.; Peulen, O.; Dandrifosse, G. Development of a Serum-Free Co-Culture of Human Intestinal Epithelium Cell-Lines (Caco-2/HT29-5M21). BMC Cell Biol. 2006, 7, 20. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chen, X.-M.; Elisia, I.; Kitts, D.D. Defining Conditions for the Co-Culture of Caco-2 and HT29-MTX Cells Using Taguchi Design. J. Pharmacol. Toxicol. Methods 2010, 61, 334–342. [Google Scholar] [CrossRef] [PubMed]
- Kim, Y.S.; Ho, S.B. Intestinal Goblet Cells and Mucins in Health and Disease: Recent Insights and Progress. Curr. Gastroenterol. Rep. 2010, 12, 319–330. [Google Scholar] [CrossRef] [Green Version]
- Rodríguez-Ramiro, I.; Ramos, S.; López-Oliva, E.; Agis-Torres, A.; Bravo, L.; Goya, L.; Martín, M.A. Cocoa Polyphenols Prevent Inflammation in the Colon of Azoxymethane-Treated Rats and in TNF-α-Stimulated Caco-2 Cells. Br. J. Nutr. 2013, 110, 206–215. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Liu, T.; Zhang, L.; Joo, D.; Sun, S.-C. NF-ΚB Signaling in Inflammation. Signal Transduct. Target. Ther. 2017, 2, 17023. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Turco, L.; Catone, T.; Caloni, F.; Consiglio, E.D.; Testai, E.; Stammati, A. Caco-2/TC7 Cell Line Characterization for Intestinal Absorption: How Reliable Is This in Vitro Model for the Prediction of the Oral Dose Fraction Absorbed in Human? Toxicol. In Vitro 2011, 25, 13–20. [Google Scholar] [CrossRef]
- Caughlan, A.; Newhouse, K.; Namgung, U.; Xia, Z. Chlorpyrifos Induces Apoptosis in Rat Cortical Neurons That Is Regulated by a Balance Between P38 and ERK/JNK MAP Kinases. Toxicol. Sci. 2004, 78, 125–134. [Google Scholar] [CrossRef] [Green Version]
- Chen, Y.; Lu, Q.; Schneeberger, E.E.; Goodenough, D.A. Restoration of Tight Junction Structure and Barrier Function by Down-Regulation of the Mitogen-Activated Protein Kinase Pathway in Ras-Transformed Madin-Darby Canine Kidney Cells. Mol. Biol. Cell 2000, 11, 849–862. [Google Scholar] [CrossRef] [Green Version]
- Wang, Y.; Zhang, J.; Yi, X.; Yu, F.-S.X. Activation of ERK1/2 MAP Kinase Pathway Induces Tight Junction Disruption in Human Corneal Epithelial Cells. Exp. Eye Res. 2004, 78, 125–136. [Google Scholar] [CrossRef]
- Nakadai, A.; Li, Q.; Kawada, T. Chlorpyrifos Induces Apoptosis in Human Monocyte Cell Line U937. Toxicology 2006, 224, 202–209. [Google Scholar] [CrossRef]
- Zhang, Y.; Chang, Y.; Cao, H.; Xu, W.; Li, Z.; Tao, L. Potential Threat of Chlorpyrifos to Human Liver Cells via the Caspase-Dependent Mitochondrial Pathways. Food Agric. Immunol. 2018, 29, 294–305. [Google Scholar] [CrossRef] [Green Version]
- Zuckerman, A.J. IARC Monographs on the Evaluation of Carcinogenic Risks to Humans. J. Clin. Pathol. 1995, 48, 691. [Google Scholar] [CrossRef] [Green Version]
- Chen, W.; Feng, L.; Shen, Y.; Su, H.; Li, Y.; Zhuang, J.; Zhang, L.; Zheng, X. Myricitrin Inhibits Acrylamide-Mediated Cytotoxicity in Human Caco-2 Cells by Preventing Oxidative Stress. BioMed Res. Int. 2013, 2013, 724183. [Google Scholar] [CrossRef] [PubMed]
- Talbot, P.; Radziwill-Bienkowska, J.M.; Kamphuis, J.B.J.; Steenkeste, K.; Bettini, S.; Robert, V.; Noordine, M.-L.; Mayeur, C.; Gaultier, E.; Langella, P.; et al. Food-Grade TiO2 Is Trapped by Intestinal Mucus in Vitro but Does Not Impair Mucin O-Glycosylation and Short-Chain Fatty Acid Synthesis In Vivo: Implications for Gut Barrier Protection. J. Nanobiotechnol. 2018, 16, 53. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Aveleira, C.A.; Lin, C.-M.; Abcouwer, S.F.; Ambrósio, A.F.; Antonetti, D.A. TNF-α Signals Through PKCζ/NF-ΚB to Alter the Tight Junction Complex and Increase Retinal Endothelial Cell Permeability. Diabetes 2010, 59, 2872–2882. [Google Scholar] [CrossRef] [Green Version]
- Khalaf, H.; Demirel, I.; Bengtsson, T. Suppression of Inflammatory Gene Expression in T Cells by Porphyromonas Gingivalis Is Mediated by Targeting MAPK Signaling. Cell. Mol. Immunol. 2013, 10, 413–422. [Google Scholar] [CrossRef]
- Thalhamer, T.; McGrath, M.A.; Harnett, M.M. MAPKs and Their Relevance to Arthritis and Inflammation. Rheumatology 2007, 47, 409–414. [Google Scholar] [CrossRef] [Green Version]
- Lim, T.-G.; Lee, B.K.; Kwon, J.Y.; Jung, S.K.; Lee, K.W. Acrylamide Up-Regulates Cyclooxygenase-2 Expression through the MEK/ERK Signaling Pathway in Mouse Epidermal Cells. Food Chem. Toxicol. 2011, 49, 1249–1254. [Google Scholar] [CrossRef]
- Recio, L.; Friedman, M.; Marroni, D.; Maynor, T.; Chepelev, N.L. Impact of Acrylamide on Calcium Signaling and Cytoskeletal Filaments in Testes From F344 Rat. Int. J. Toxicol. 2017, 36, 124–132. [Google Scholar] [CrossRef] [Green Version]
- Wang, Z.; Bao, Z.; Ding, Y.; Xu, S.; Du, R.; Yan, J.; Li, L.; Sun, Z.; Shao, C.; Gu, W. Nε-Carboxymethyl-Lysine-Induced PI3K/Akt Signaling Inhibition Promotes Foam Cell Apoptosis and Atherosclerosis Progression. Biomed. Pharmacother. 2019, 115, 108880. [Google Scholar] [CrossRef] [PubMed]







| Function | Gene | Name | Sequences 5′-> 3′ or Reference |
|---|---|---|---|
| Housekeeping Genes | GAPDH | Glyceraldehyde 3 phosphate dehydrogenase | GTCAACGCTGAGAACGGGAA AAA TGAGCCCCAGCCTTCTC (Eurofins) |
| PPIA | Peptidyl-prolyl cis-trans isomerase A | CCTATCCTAGAGGTGGCGGA TCATCGCAGAAGGAACCAGAC (Eurofins) | |
| Inflammatory Genes | CXCL8 | C-X-C motif chemokine ligand 8 | AGAGTGATTGAGAGTGGACC ACTTCTCCACAACCCTCTG (Eurofins) |
| MAPK14 | Mitogen-activated protein kinase 14, also called p38-α | QT00079345 (QIAGEN) | |
| MAPK8 | Mitogen-activated protein kinase 8 | QT00091056 (QIAGEN) | |
| MAP3K1 | Mitogen-activated protein kinase-kinase-kinase 1 | QT00088998 (QIAGEN) | |
| MyD88 | Myeloid 88 | QT00203490 (QIAGEN) | |
| NF-κB | nuclear factor-kappa B | GGGGGCATCAAACCTGAAGA GGAGAGAAGTCCCCAAAGGC (Eurofins) | |
| STAT3 | Signal transducer and activator of transcription 3 | QT00068754 (QIAGEN) | |
| TNF-α | tumor necrosis factors α | QT00029162 (QIAGEN) | |
| Apoptosis Genes | CASP3 | Caspase 3 | QT00997997 (QIAGEN) |
| CASP9 | Caspase 9 | QT00036267(QIAGEN) | |
| Microvillly Gene | VIL1 | Villin 1 | AAGAAAGCCAATGAGCAGGAGAAG TTCTCAATGCGCCACACCTG (Eurofins) |
| Tight Junctions Genes | CLDN4 | Claudin 4 | GGCGTGGTGTTCCTGTTG AGCGGATTGTAGAAGTCTTGG (Eurofins) |
| TJP1 | Tight Junction Protein 1 | GAATGATGGTTGGTATGGTGCG TCAGAAGTGTGTCTACTGTCCG (Eurofins) | |
| OCLN | Occludin | QT00081844 (QIAGEN) | |
| Mucins Genes | MUC3 | Mucin 3 | QT02309335 (QIAGEN) |
| MUC5AC | Mucin 5AC | QT00088991 (QIAGEN) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Guibourdenche, M.; Haug, J.; Chevalier, N.; Spatz, M.; Barbezier, N.; Gay-Quéheillard, J.; Anton, P.M. Food Contaminants Effects on an In Vitro Model of Human Intestinal Epithelium. Toxics 2021, 9, 135. https://doi.org/10.3390/toxics9060135
Guibourdenche M, Haug J, Chevalier N, Spatz M, Barbezier N, Gay-Quéheillard J, Anton PM. Food Contaminants Effects on an In Vitro Model of Human Intestinal Epithelium. Toxics. 2021; 9(6):135. https://doi.org/10.3390/toxics9060135
Chicago/Turabian StyleGuibourdenche, Marion, Johanna Haug, Noëllie Chevalier, Madeleine Spatz, Nicolas Barbezier, Jérôme Gay-Quéheillard, and Pauline M. Anton. 2021. "Food Contaminants Effects on an In Vitro Model of Human Intestinal Epithelium" Toxics 9, no. 6: 135. https://doi.org/10.3390/toxics9060135
APA StyleGuibourdenche, M., Haug, J., Chevalier, N., Spatz, M., Barbezier, N., Gay-Quéheillard, J., & Anton, P. M. (2021). Food Contaminants Effects on an In Vitro Model of Human Intestinal Epithelium. Toxics, 9(6), 135. https://doi.org/10.3390/toxics9060135








