Utilizing 3D Printing Technology to Create Prosthetic Irises: Proof of Concept and Workflow
Abstract
:1. Introduction
2. Materials and Methods
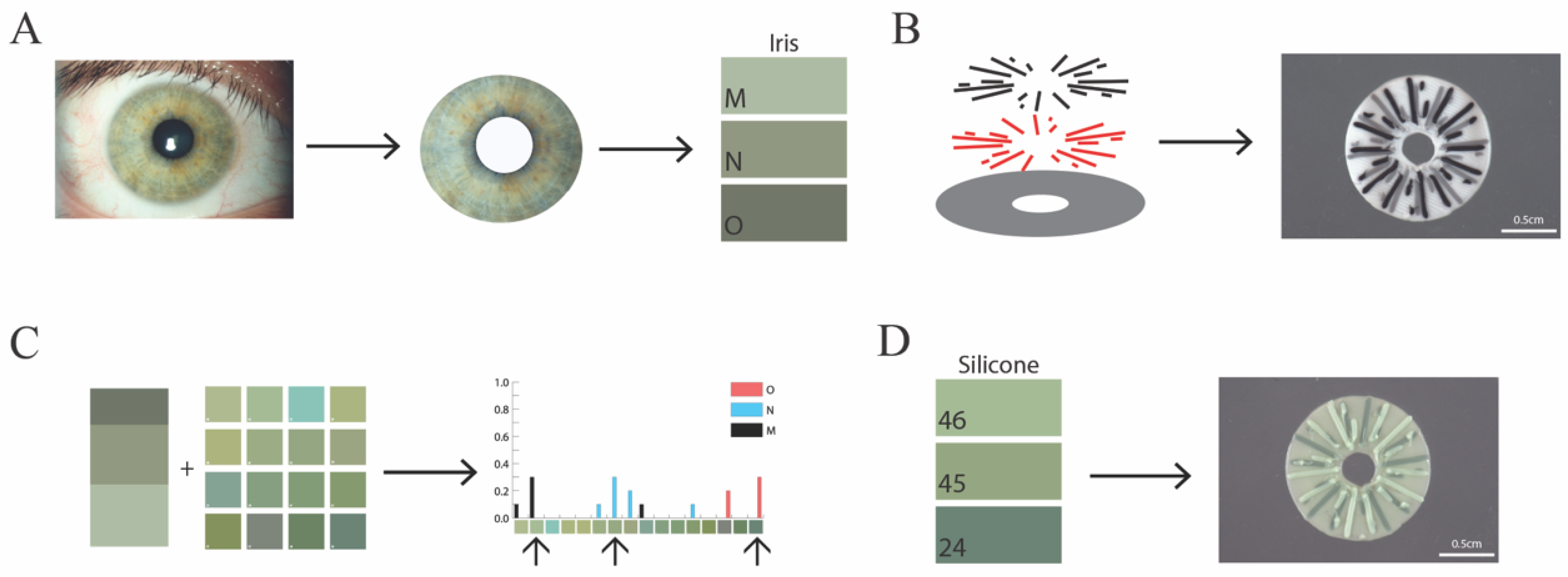
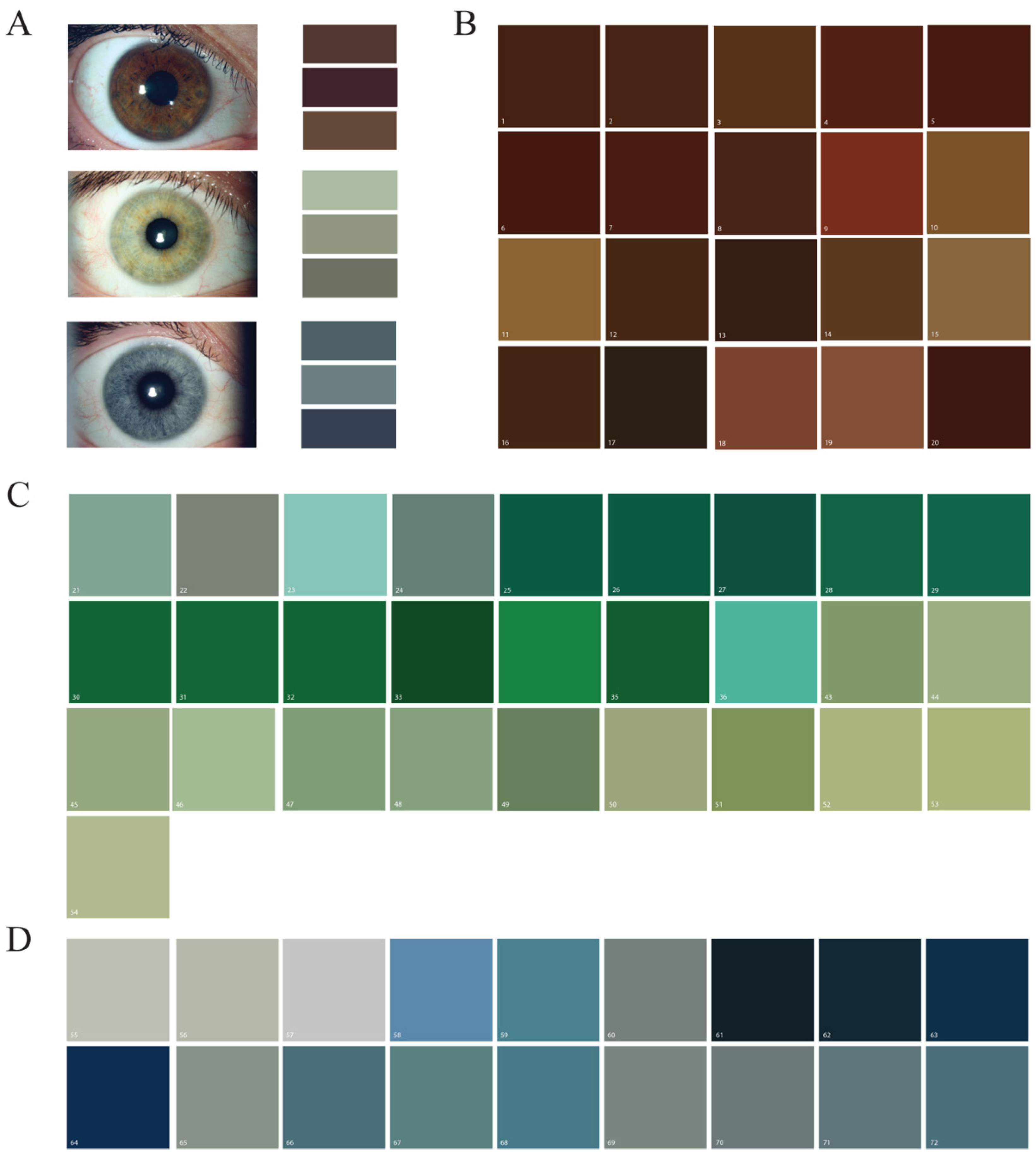
2.1. Reference Iris Imaging and Analysis
2.2. Silicone Pigment Mixing
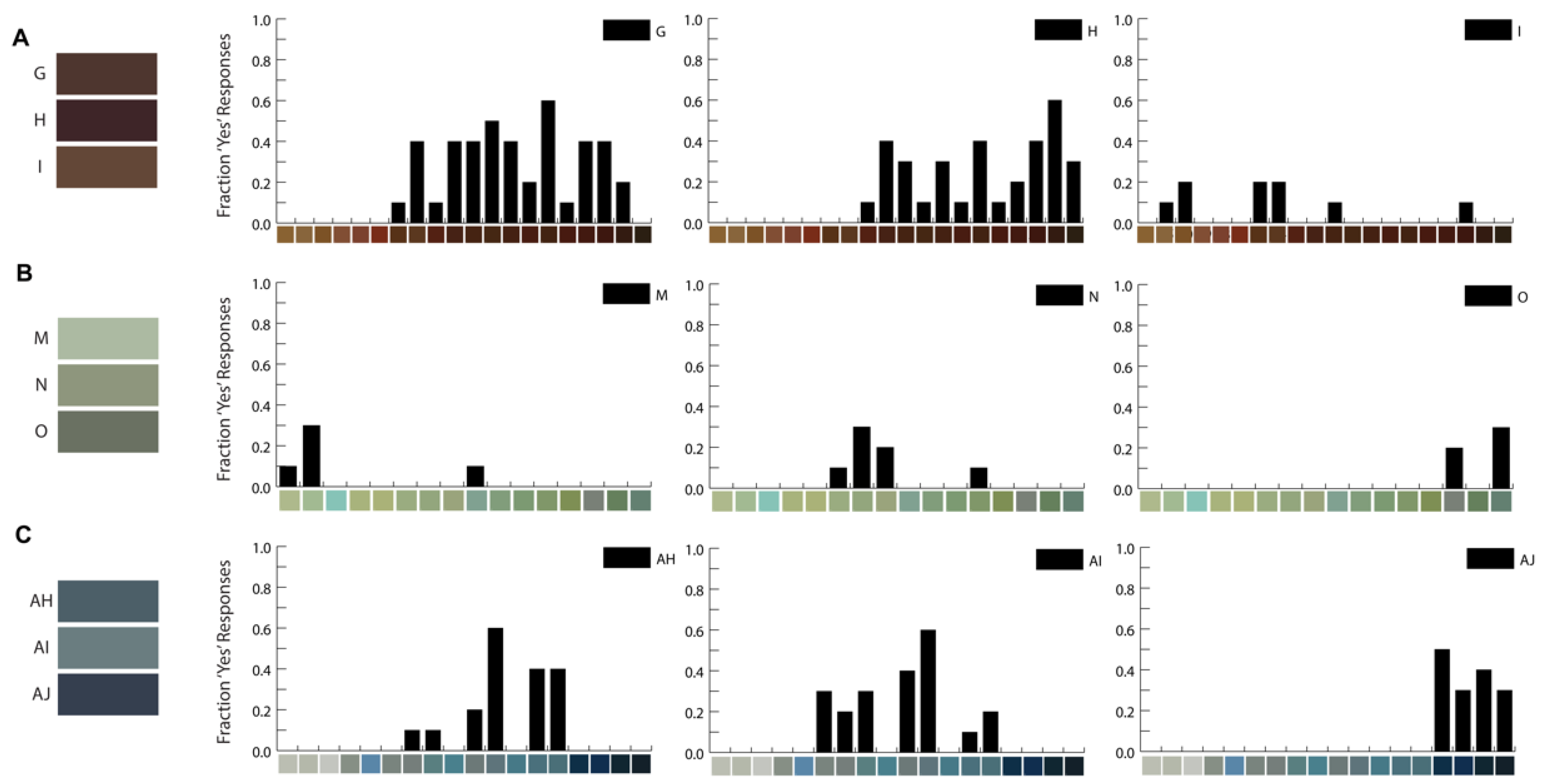
2.3. Color-Matching Survey
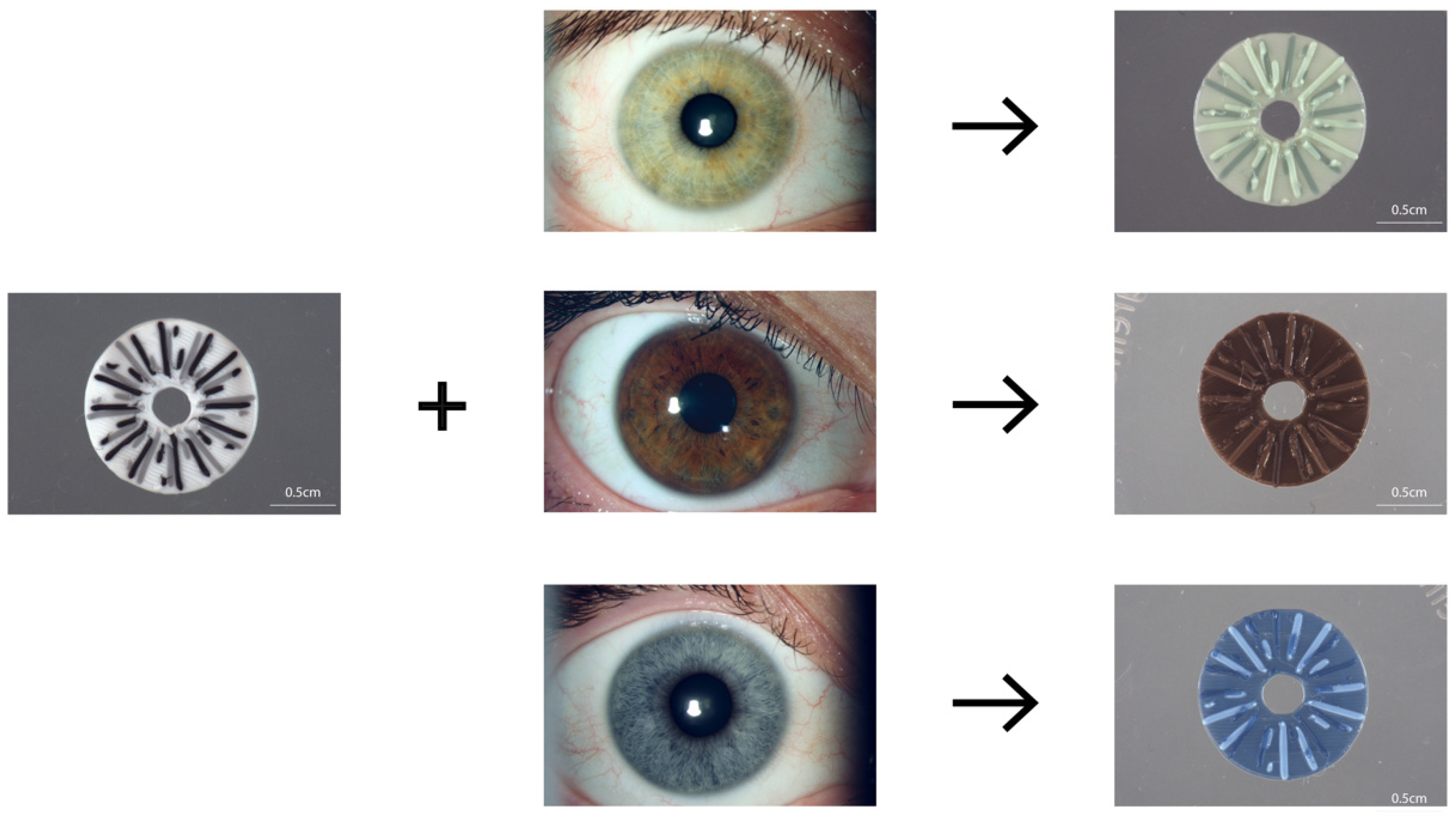
2.4. 3D Printing
3. Results
3.1. Manufacturing Silicone Pigments Based on Iris Photographs
3.2. Silicone Color-Matching Survey Results
3.3. 3D Printing of Colored Irises
4. Discussion
5. Conclusions and Future Directions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Kleisner, K.; Kočnar, T.; Rubešová, A.; Flegr, J. Eye Color Predicts but Does Not Directly Influence Perceived Dominance in Men. Personal. Individ. Differ. 2010, 49, 59–64. [Google Scholar] [CrossRef]
- Zuo, Y.; Kawabata, Y. Effects of Lip and Eye Color on the Emotion Categorization of Facial Expressions. Color Res. Appl. 2023. [Google Scholar] [CrossRef]
- Srinivasan, S.; Ting, D.S.J.; Snyder, M.E.; Prasad, S.; Koch, H.-R. Prosthetic Iris Devices. Can. J. Ophthalmol. 2014, 49, 6–17. [Google Scholar] [CrossRef]
- Vincent, S.J. The Use of Contact Lenses in Low Vision Rehabilitation: Optical and Therapeutic Applications. Clin. Exp. Optom. 2017, 100, 513–521. [Google Scholar] [CrossRef]
- Burris, T.E.; Holmes-Higgin, D.K.; Silvestrini, T.A. Lamellar Intrastromal Corneal Tattoo for Treating Iris Defects (Artificial Iris). Cornea 1998, 17, 169–173. [Google Scholar] [CrossRef] [PubMed]
- Mayer, C.S.; Laubichler, A.E.; Khoramnia, R.; Tandogan, T.; Prahs, P.; Zapp, D.; Reznicek, L. Challenges and Complication Management in Novel Artificial Iris Implantation. J. Ophthalmol. 2018, 2018, 3262068. [Google Scholar] [CrossRef] [PubMed]
- Aslam, S.A.; Wong, S.C.; Ficker, L.A.; MacLaren, R.E. Implantation of the Black Diaphragm Intraocular Lens in Congenital and Traumatic Aniridia. Ophthalmology 2008, 115, 1705–1712. [Google Scholar] [CrossRef] [PubMed]
- Miller, K.M.; Kuo, A.; Olson, M.D.; Masket, S. Safety and Efficacy of Black Iris Diaphragm Intraocular Lens Implantation in Eyes with Large Iris Defects: Report 4. J. Cataract Refract. Surg. 2018, 44, 686–700. [Google Scholar] [CrossRef]
- Qiu, X.; Ji, Y.; Zheng, T.; Lu, Y. Long-Term Efficacy and Complications of Black Diaphragm Intraocular Lens Implantation in Patients with Traumatic Aniridia. Br. J. Ophthalmol. 2014, 99, 659–664. [Google Scholar] [CrossRef]
- Miller, K.M.; Nicoli, C.M.; Olson, M.D.; Shah, M.; Masket, S. Outcomes of Implantation of Modified Capsule Tension Rings with Multiple Black Occluder Paddles for Eyes with Congenital and Acquired Iris Defects: Report 3. J. Cataract Refract. Surg. 2016, 42, 870–878. [Google Scholar] [CrossRef]
- Frisina, R.; Biasi, C.S.D.; Tozzi, L.; Gius, I.; Londei, D.; Gambato, C.; Midena, E. Reper Intraocular Lens with Artificial Iris: Implantation Techniques and Outcomes. Eur. J. Ophthalmol. 2021, 31, 1469–1474. [Google Scholar] [CrossRef] [PubMed]
- Spitzer, M.S.; Nessmann, A.; Wagner, J.; Yoeruek, E.; Bartz-Schmidt, K.U.; Szurman, P.; Szurman, G.B. Customized Humanoptics Silicone Iris Prosthesis in Eyes with Posttraumatic Iris Loss: Outcomes and Complications. Acta Ophthalmol. 2016, 94, 301–306. [Google Scholar] [CrossRef] [PubMed]
- Doroodgar, F.; Jabbarvand, M.; Niazi, F.; Niazi, S.; Sanginabadi, A. Implantation of ArtificialIris, a CustomFlex Irisprosthesis, in a Trauma Patient with an Artisan Lens. Medicine 2017, 96, e8405. [Google Scholar] [CrossRef]
- Weissbart, S.B.; Ayres, B.D. Management of Aniridia and Iris Defects: An Update on Iris Prosthesis Options. Curr. Opin. Ophthalmol. 2016, 27, 244–249. [Google Scholar] [CrossRef]
- Ayres, B.D.; Fant, B.S.; Landis, Z.C.; Miller, K.M.; Stulting, R.D.; Cionni, R.J.; Fram, N.R.; Hamilton, S.; Hardten, D.R.; Koch, D.D.; et al. Results of the United States Food and Drug Administration Clinical Trial of the CustomFlex Artificial Iris. Ophthalmology 2022, 129, 614–625. [Google Scholar] [CrossRef] [PubMed]
- Kobashi, H.; Kobayashi, M. 3D-Printed Eye Model: Simulation of Intraocular Pressure. PLoS ONE 2023, 18, e0282911. [Google Scholar] [CrossRef] [PubMed]
- Famery, N.; Abdelmassih, Y.; El-Khoury, S.; Guindolet, D.; Cochereau, I.; Gabison, E.E. Artificial Chamber and 3D Printed Iris: A New Wet Lab Model for Teaching Descemet’s Membrane Endothelial Keratoplasty. Acta Ophthalmol. 2019, 97, e179–e183. [Google Scholar] [CrossRef]
- Zou, J.; Tan, W.; Li, F.; Zhou, G.; Li, L.; Xiong, S.; Wang, X.; Xu, H. Outcomes of a New 3-D Printing-assisted Personalized Macular Buckle Combined with Para Plana Vitrectomy for Myopic Foveoschisis. Acta Ophthalmol. 2021, 99, 688–694. [Google Scholar] [CrossRef]
- Navajas, E.V.; ten Hove, M. Three-Dimensional Printing of a Transconjunctival Vitrectomy Trocar-Cannula System. Ophthalmologica 2017, 237, 119–122. [Google Scholar] [CrossRef]
- Ruiters, S.; Sun, Y.; de Jong, S.; Politis, C.; Mombaerts, I. Computer-Aided Design and Three-Dimensional Printing in the Manufacturing of an Ocular Prosthesis. Br. J. Ophthalmol. 2016, 100, 879–881. [Google Scholar] [CrossRef] [PubMed]
- Ruiters, S.; Shujaat, S.; Vasconcelos, K.F.; Shaheen, E.; Jacobs, R.; Mombaerts, I. Three-dimensional Design of a Geometric Model for an Ocular Prosthesis in Ex Vivo Anophthalmic Socket Models. Acta Ophthalmol. 2021, 99, 221–226. [Google Scholar] [CrossRef]
- Groot, A.L.W.; Remmers, J.S.; Hartong, D.T. Three-Dimensional Computer-Aided Design of a Full-Color Ocular Prosthesis with Textured Iris and Sclera Manufactured in One Single Print Job. 3D Print. Addit. Manuf. 2021, 8, 343–348. [Google Scholar] [CrossRef]
- Diehl, M.I.; Wolf, S.P.; Bindokas, V.P.; Schreiber, H. Automated Cell Cluster Analysis Provides Insight into Multi-Cell-Type Interactions between Immune Cells and Their Targets. Exp. Cell Res. 2020, 393, 112014. [Google Scholar] [CrossRef]
- Schindelin, J.; Arganda-Carreras, I.; Frise, E.; Kaynig, V.; Longair, M.; Pietzsch, T.; Preibisch, S.; Rueden, C.; Saalfeld, S.; Schmid, B.; et al. Fiji: An Open-Source Platform for Biological-Image Analysis. Nat. Methods 2012, 9, 676–682. [Google Scholar] [CrossRef]
- Nugent, R.; Stuetzle, W. Clustering with Confidence: A Binning Approach; Carnegie Mellon University: Pittsburgh, PA, USA, 2018. [Google Scholar] [CrossRef]
- Alam, M.d.S.; Sugavaneswaran, M.; Arumaikkannu, G.; Mukherjee, B. An Innovative Method of Ocular Prosthesis Fabrication by Bio-CAD and Rapid 3-D Printing Technology: A Pilot Study. Orbit 2017, 36, 223–227. [Google Scholar] [CrossRef]
- Kim, B.R.; Kim, S.H.; Ko, J.; Baek, S.W.; Park, Y.K.; Kim, Y.J.; Yoon, J.S. A Pilot Clinical Study of Ocular Prosthesis Fabricated by Three-Dimensional Printing and Sublimation Technique. Korean J. Ophthalmol. 2021, 35, 37–43. [Google Scholar] [CrossRef]
- Ko, J.; Kim, S.H.; Baek, S.W.; Chae, M.K.; Yoon, J.S. Semi-Automated Fabrication of Customized Ocular Prosthesis with Three–Dimensional Printing and Sublimation Transfer Printing Technology. Sci. Rep. 2019, 9, 2968. [Google Scholar] [CrossRef]
- Gius, I.; Tozzi, L.; Biasi, C.S.D.; Pizzolon, T.; Parolini, B.; Frisina, R. Artificial Iris: State of the Art. J. Cataract Refract. Surg. 2023, 49, 430–437. [Google Scholar] [CrossRef] [PubMed]
- Mironov, V.; Reis, N.; Derby, B. Review: Bioprinting: A Beginning. Tissue Eng. 2006, 12, 631–634. [Google Scholar] [CrossRef] [PubMed]
- Tan, G.; Ioannou, N.; Mathew, E.; Tagalakis, A.D.; Lamprou, D.A.; Yu-Wai-Man, C. 3D Printing in Ophthalmology: From Medical Implants to Personalised Medicine. Int. J. Pharm. 2022, 625, 122094. [Google Scholar] [CrossRef] [PubMed]
- Sommer, A.C.; Blumenthal, E.Z. Implementations of 3D Printing in Ophthalmology. Graefe’s Arch. Clin. Exp. Ophthalmol. 2019, 257, 1815–1822. [Google Scholar] [CrossRef]
- Tsui, J.K.S.; Bell, S.; da Cruz, L.; Dick, A.D.; Sagoo, M.S. Applications of Three-Dimensional Printing in Ophthalmology. Surv. Ophthalmol. 2022, 67, 1287–1310. [Google Scholar] [CrossRef]
- Sorkio, A.; Koch, L.; Koivusalo, L.; Deiwick, A.; Miettinen, S.; Chichkov, B.; Skottman, H. Human Stem Cell Based Corneal Tissue Mimicking Structures Using Laser-Assisted 3D Bioprinting and Functional Bioinks. Biomaterials 2018, 171, 57–71. [Google Scholar] [CrossRef] [PubMed]
- Isaacson, A.; Swioklo, S.; Connon, C.J. 3D Bioprinting of a Corneal Stroma Equivalent. Exp. Eye Res. 2018, 173, 188–193. [Google Scholar] [CrossRef]
- Debellemanière, G.; Flores, M.; Montard, M.; Delbosc, B.; Saleh, M. Three-Dimensional Printing of Optical Lenses and Ophthalmic Surgery: Challenges and Perspectives. J. Refract. Surg. 2015, 32, 201–204. [Google Scholar] [CrossRef] [PubMed]
- Lorber, B.; Hsiao, W.-K.; Martin, K.R. Three-Dimensional Printing of the Retina. Curr. Opin. Ophthalmol. 2016, 27, 262–267. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Prager, A.J.; Henning, N.; Burns, L.; Ramaprasad, A.; Basti, S.; Laronda, M.M. Utilizing 3D Printing Technology to Create Prosthetic Irises: Proof of Concept and Workflow. Bioengineering 2023, 10, 1287. https://doi.org/10.3390/bioengineering10111287
Prager AJ, Henning N, Burns L, Ramaprasad A, Basti S, Laronda MM. Utilizing 3D Printing Technology to Create Prosthetic Irises: Proof of Concept and Workflow. Bioengineering. 2023; 10(11):1287. https://doi.org/10.3390/bioengineering10111287
Chicago/Turabian StylePrager, Alisa J., Nathaniel Henning, Lauren Burns, Abhijit Ramaprasad, Surendra Basti, and Monica M. Laronda. 2023. "Utilizing 3D Printing Technology to Create Prosthetic Irises: Proof of Concept and Workflow" Bioengineering 10, no. 11: 1287. https://doi.org/10.3390/bioengineering10111287




