The Role of Imaging of Lymphatic System to Prevent Cancer Related Lymphedema
Abstract
:1. Introduction
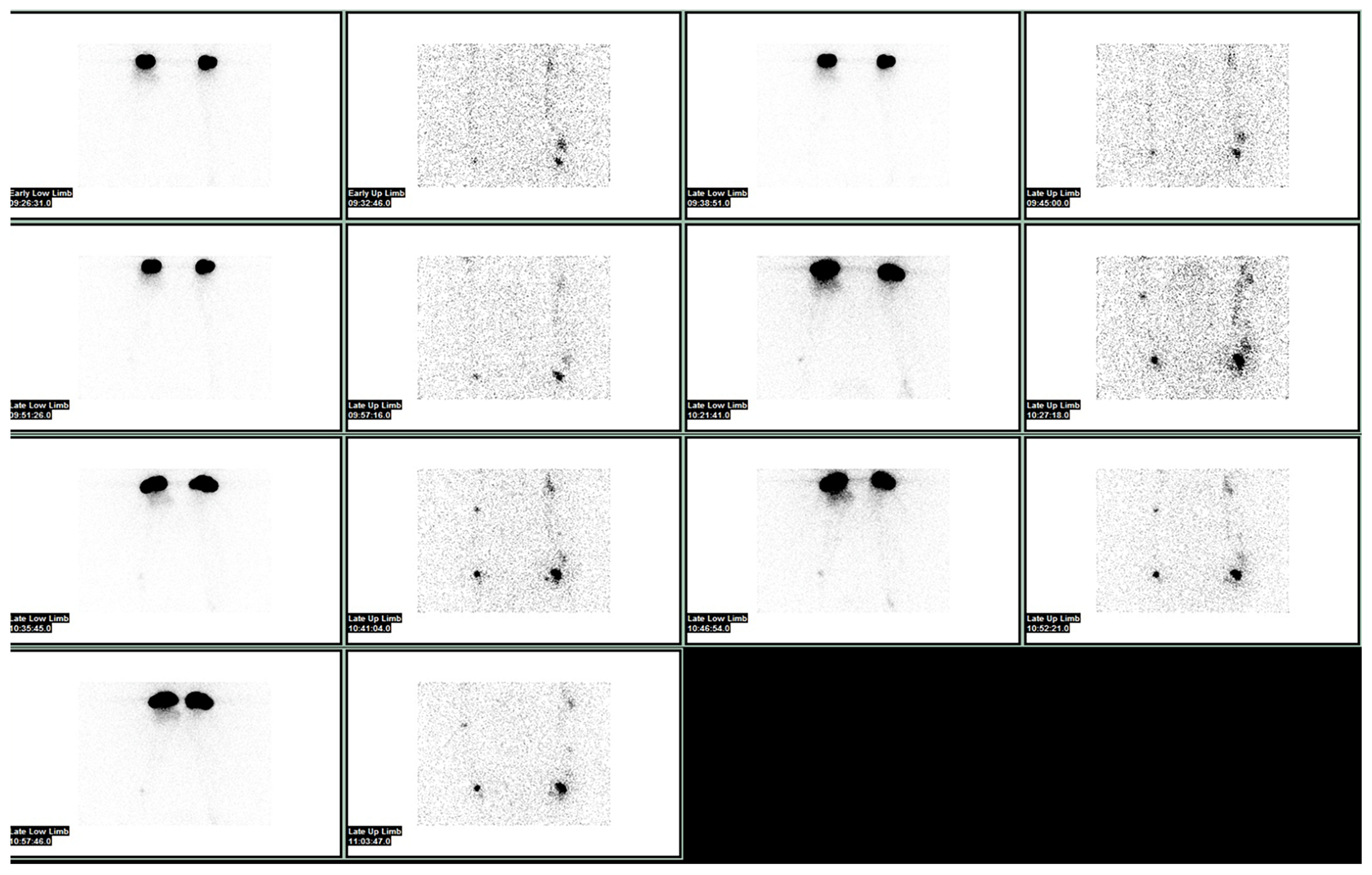
2. Lymphoscintigraphy: An Overview of the Gold Standard Method
The Quantitative Method: Alternative or Complement to Gold Standard?
3. New Emerging Techniques for Lymphedema Assessment in Real Clinical Practice
AI and Machine Learning: The Distant Future of Diagnostic Imaging
4. The Role of Imaging in the Prevention and Treatment of Lymphedema
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- McLaughlin, S.A.; Wright, M.J.; Morris, K.T.; Giron, G.L.; Sampson, M.R.; Brockway, J.P.; Hurley, K.E.; Riedel, E.R.; Van Zee, K.J. Prevalence of lymphedema in women with breast cancer 5 years after sentinel lymph node biopsy or axillary dissection: Objective measurements. J. Clin. Oncol. 2008, 26, 5213. [Google Scholar] [CrossRef]
- Petrek, J.A.; Senie, R.T.; Peters, M.; Rosen, P.P. Lymphedema in a cohort of breast carcinoma survivors 20 years after diagnosis. Cancer 2001, 92, 1368–1377. [Google Scholar] [CrossRef]
- Segerstrom, K.; Bjerle, P.; Graffman, S.; Nystrom, A. Factors that influ- ence the incidence of brachial oedema after treatment of breast cancer. Scand. J. Plast. Reconstr. Surg. Hand Surg. 1992, 26, 223–227. [Google Scholar] [CrossRef] [PubMed]
- Committee, E. The diagnosis and treatment of peripheral lymph- edema: 2016 consensus document of the International Society of Lymphology. Lymphology 2016, 49, 170–184. [Google Scholar]
- Monticone, M.; Ferriero, G.; Keeley, V.; Brunati, R.; Liquori, V.; Maggioni, S.; Restelli, M.; Giordano, A.; Franchignoni, F. Lymphedema quality of life questionnaire (LYMQOL): Cross-cultural adaptation and validation in Italian women with upper limb lymphedema after breast cancer. Disabil. Rehabil. 2022, 44, 4075–4080. [Google Scholar] [CrossRef]
- Cuccurullo, V.; Rapa, M.; Catalfamo, B.; Cascini, G.L. Role of Nuclear Sentinel Lymph Node Mapping Compared to New Alternative Imaging Methods. J. Pers. Med. 2023, 13, 1219. [Google Scholar] [CrossRef] [PubMed]
- Stout Gergich, N.L.; Pfalzer, L.A.; McGarvey, C.; Springer, B.; Gerber, L.H.; Soballe, P. Preoperative assessment enables the early diagnosis and successful treatment of lymphedema. Cancer 2008, 112, 2809–2819. [Google Scholar] [CrossRef]
- Spiegel, M.; Vesti, B.; Shore, A.; Franzeck, U.K.; Becker, F.; Bollinger, A. Pressure of lymphatic capillaries in human skin. Am. J. Physiol. Circ. Physiol. 1992, 262, H1208–H1210. [Google Scholar] [CrossRef] [PubMed]
- Vermeulen, K.; Vandamme, M.; Bormans, G.; Cleeren, F. Design and Challenges of Radiopharmaceuticals. Semin. Nucl. Med. 2019, 49, 339–356. [Google Scholar] [CrossRef]
- De Cicco, C.; Cremonesi, M.; Luini, A.; Bartolomei, M.; Grana, C.; Prisco, G.; Galimberti, V.; Calza, P.; Viale, G.; Veronesi, U.; et al. Lymphoscintigraphy and Radioguided Biopsy of the Sentinel Axillary Node in Breast Cancer. J. Nucl. Med. 1998, 39, 2080–2084. [Google Scholar]
- Ballinger, J.R. Challenges in Preparation of Albumin Nanoparticle-Based Radiopharmaceuticals. Molecules 2022, 27, 8596. [Google Scholar] [CrossRef]
- Partsch, H. Assessment of abnormal lymph drainage for the diagnosis of lymphedema by isotopic lymphangiography and by indirect lymphography. Clin. Dermatol. 1995, 13, 445–450. [Google Scholar] [CrossRef]
- McNeill, G.C.; Witte, M.H.; Witte, C.L.; Williams, W.H.; Hall, J.N.; Patton, D.D.; Pond, G.D.; Woolfenden, J.M. Whole-body lymphangioscintigraphy: Preferred method for initial assessment of the peripheral lymphatic system. Radiology 1989, 172, 495–502. [Google Scholar] [CrossRef]
- Szuba, A.; Shin, W.S.; Strauss, H.W.; Rockson, S. The third circulation: Radionuclide lymphoscintigraphy in the evaluation of lymphedema. J. Nucl. Med. 2003, 44, 43–57. [Google Scholar] [PubMed]
- Villa, G.; Campisi, C.C.; Ryan, M.; Boccardo, F.; Di Summa, P.; Frascio, M.; Sambuceti, G. Procedural Recommendations for Lymphoscintigraphy in the Diagnosis of Peripheral Lymphedema: The Genoa Protocol. Nucl. Med. Mol. Imaging 2019, 53, 47–56. [Google Scholar] [CrossRef] [PubMed]
- Hassanein, A.H.; Maclellan, R.A.; Grant, F.D.; Greene, A.K. Diagnostic accuracy of lymphoscintigraphy for lymphedema and analysis of false negative tests. Plast. Reconstr. Surg.-Glob. Open 2017, 5, e1396. [Google Scholar] [CrossRef] [PubMed]
- Gloviczki, P.; Calcagno, D.; Schirger, A.; Pairolero, P.C.; Cherry, K.J.; Hallett, J.W.; Wahner, H.W. Noninvasive evaluation of the swollen extremity: Experiences with 190 lymphoscintigraphic examinations. J. Vasc. Surg. 1989, 9, 683–690. [Google Scholar] [CrossRef] [PubMed]
- Pappalardo, M.; Cheng, M.H. Lymphoscintigraphy for the diagnosis of extremity lymphedema: Current controversies regarding protocol, interpretation, and clinical application. J. Surg. Oncol. 2020, 121, 37–47. [Google Scholar] [CrossRef] [PubMed]
- Cheng, M.H.; Pappalardo, M.; Lin, C.; Kuo, C.F.; Lin, C.Y.; Chung, K.C. Validity of the novel Taiwan lymphoscintigraphy staging and correlation of cheng lymphedema grading for unilateral extremity lymphedema. Ann. Surg. 2018, 268, 513–525. [Google Scholar] [CrossRef]
- Cheng, M.H.; Chang, D.W.; Patel, K.M. Principles and Practice of Lymphedema Surgery; Elsevier: Oxford, UK, 2016. [Google Scholar]
- Campisi, C.C.; Ryan, M.; Villa, G.; Di Summa, P.; Cherubino, M.; Boccardo, F.; Campisi, C. Rationale for study of the deep subfascial lymphatic vessels during lymphoscintigraphy for the diagnosis of peripheral lymphedema. Clin. Nucl. Med. 2019, 44, 91–98. [Google Scholar] [CrossRef]
- Fujiyoshi, T.; Mikami, T.; Hashimoto, K.; Asano, S.; Adachi, E.; Kagimoto, S.; Yabuki, Y.; Kitayama, S.; Matsubara, S.; Maegawa, J.; et al. Pathological changes in the lymphatic system of patients with secondary lower limb lymphedema based on single photon-emission computed tomography/computed tomography/lymphoscintigraphy images. Lymphat. Res. Biol. 2021, 20, 144–152. [Google Scholar] [CrossRef] [PubMed]
- Sacks, G.A.; Sandler, M.P.; Born, M.L.; Claton, J.A.; Franklin, J.D.; Partain, C.L. Lymphoscintigraphy as an adjunctive procedure in the perioperative assessment of patients undergoing microlymphaticovenous anastomoses. Clin. Nucl. Med. 1983, 8, 309–311. [Google Scholar] [CrossRef] [PubMed]
- Kwon, H.R.; Hwang, J.H.; Mun, G.-H.; Hyun, S.H.; Moon, S.H.; Lee, K.-H.; Choi, J.Y. Predictive role of lymphoscintigraphy undergoing lymphovenous anastomosis in patients with lower extremity lymphedema: A preliminary study. BMC Med. Imaging 2021, 21, 188. [Google Scholar] [CrossRef]
- Yoo, J.N.; Cheong, Y.S.; Min, Y.S.; Lee, S.W.; Park, H.Y.; Jung, T.D. Validity of quantitative lymphoscintigraphy as a lymphedema assessment tool for patients with breast cancer. Ann. Rehabil. Med. 2015, 39, 931–940. [Google Scholar] [CrossRef] [PubMed]
- Chiewvit, S.; Kumnerdnakta, S. Lymphoscintigraphic Findings That Predict Favorable Outcome after Lymphaticovenous Anastomosis. Lymphology 2017, 50, 1–8. [Google Scholar] [PubMed]
- Kim, P.; Lee, J.K.; Lim, O.K.; Park, H.K.; Park, K.D. Quantitative Lymphoscintigraphy to Predict the Possibility of Lymphedema Development After Breast Cancer Surgery: Retrospective Clinical Study. Ann. Rehabil. Med. 2017, 41, 1065–1075. [Google Scholar] [CrossRef]
- Szuba, A.; Strauss, W.; Sirsikar, S.P.; Rockson, S.G. Quantitative radionuclide lymphoscintigraphy predicts outcome of manual lymphatic therapy in breast cancer-related lymphedema of the upper extremity. Nucl. Med. Commun. 2002, 23, 1171–1175. [Google Scholar] [CrossRef]
- Keramida, G.; Wroe, E.; Winterman, N.; Aplin, M.; Peters, A.M. Lymphatic drainage efficiency: A new parameter of lymphatic function. Acta Radiol. 2018, 59, 1097–1101. [Google Scholar] [CrossRef]
- Bellin, M.F.; Beigelman, C.; Precetti-Morel, S. Iron oxide-enhanced MR lymphography: Initial experience. Eur. J. Radiol. 2000, 34, 257–264. [Google Scholar] [CrossRef]
- Neligan, P.C.; Kung, T.A.; Maki, J.H. MR lymphangiography in the treatment of lymphedema. J. Surg. Oncol. 2017, 115, 18–22. [Google Scholar] [CrossRef]
- Guerrini, S.; Gentili, F.; Mazzei, F.G.; Gennaro, P.; Volterrani, L.; Mazzei, M.A. Magnetic resonance lymphangiography: With or without contrast? Diagn. Interv. Radiol. 2020, 26, 587–595. [Google Scholar] [CrossRef] [PubMed]
- Borri, M.; Schmidt, M.A.; Gordon, K.D.; Wallace, T.A.; Hughes, J.C.; Scurr, E.D.; Koh, D.-M.; Leach, M.O.; Mortimer, P.S. Quantitative Contrast-Enhanced Magnetic Resonance Lymphangiography of the Upper Limbs in Breast Cancer Related Lymphedema: An Exploratory Study. Lymphat. Res. Biol. 2015, 13, 100–106. [Google Scholar] [CrossRef] [PubMed]
- Kim, G.; Smith, M.P.; Donohoe, K.J.; Johnson, A.R.; Singhal, D.; Tsai, L.L. MRI staging of upper extremity secondary lymphedema: Correlation with clinical measurements. Eur. Radiol. 2020, 30, 4686–4694. [Google Scholar] [CrossRef] [PubMed]
- Chang, D.W.; Suami, H.; Skoracki, R. A prospective analysis of 100 consecutive lymphovenous bypass cases for treatment of extremity lymphedema. Plast. Reconstr. Surg. 2013, 132, 1305–1314. [Google Scholar] [CrossRef] [PubMed]
- Nguyen, A.T.; Suami, H.; Hanasono, M.M.; Womack, V.A.; Wong, F.C.; Chang, E.I. Long-term outcomes of the minimally invasive free vascularized omental lymphatic flap for the treatment of lymphedema. J. Surg. Oncol. 2016, 115, 84–89. [Google Scholar] [CrossRef] [PubMed]
- Akita, S.; Mitsukawa, N.; Kazama, T.; Kuriyama, M.; Kubota, Y.; Omori, N.; Koizumi, T.; Kosaka, K.; Uno, T.; Satoh, K. Comparison of lymphoscintigraphy and indocyanine green lymphography for the diagnosis of extremity lymphoedema. J. Plast. Reconstr. Aesthetic Surg. 2013, 66, 792–798. [Google Scholar] [CrossRef]
- Suami, H.; Koelmeyer, L.; Mackie, H.; Boyages, J. Patterns of lymphatic drainage after axillary node dissection impact arm lymphoedema severity: A review of animal and clinical imaging studies. Surg. Oncol. 2018, 27, 743–750. [Google Scholar] [CrossRef]
- Pons, G.; Clavero, J.A.; Alomar, X.; Rodríguez-Bauza, E.; Tom, L.K.; Masia, J. Preoperative planning of lymphaticovenous anastomosis: The use of magnetic resonance lymphangiography as a complement to indocyanine green lymphography. J. Plast. Reconstr. Aesthetic Surg. 2019, 72, 884–891. [Google Scholar] [CrossRef]
- Huang, Y.; Zheng, S.; Lin, Y. Accuracy and Utility of Preoperative Ultrasound-Guided Axillary Lymph Node Biopsy for Invasive Breast Cancer: A Systematic Review and Meta-Analysis. Comput. Intell. Neurosci. 2022, 2022, 3307627. [Google Scholar] [CrossRef]
- Jang, S.; Lee, C.U.; Hesley, G.K.; Knudsen, J.M.; Brinkman, N.J.; Tran, N.V. Lymphatic Mapping Using US Microbubbles before Lymphaticovenous Anastomosis Surgery for Lymphedema. Radiology 2022, 304, 218–224. [Google Scholar] [CrossRef]
- Panico, A.; Gatta, G.; Salvia, A.; Grezia, G.D.; Fico, N.; Cuccurullo, V. Radiomics in Breast Imaging: Future Development. J. Pers. Med. 2023, 13, 862. [Google Scholar] [CrossRef]
- Son, H.; Lee, S.; Kim, K.; Koo, K.I.; Hwang, C.H. Deep learning-based quantitative estimation of lymphedema-induced fibrosis using three-dimensional computed tomography images. Sci. Rep. 2022, 12, 15371. [Google Scholar] [CrossRef]
- Nowak, S.; Henkel, A.; Theis, M.; Luetkens, J.; Geiger, S.; Sprinkart, A.M.; Pieper, C.C.; Attenberger, U.I. Deep learning for standardized, MRI-based quantification of subcutaneous and subfascial tissue volume for patients with lipedema and lymphedema. Eur. Radiol. 2023, 33, 884–892. [Google Scholar] [CrossRef]
- Goudarzi, S.; Whyte, J.; Boily, M.; Towers, A.; Kilgour, R.D.; Rivaz, H. Segmentation of Arm Ultrasound Images in Breast Cancer-Related Lymphedema: A Database and Deep Learning Algorithm. IEEE Trans. Biomed. Eng. 2023, 70, 2552–2563. [Google Scholar] [CrossRef] [PubMed]
- Eldaly, A.S.; Avila, F.R.; A Torres-Guzman, R.; Maita, K.; Garcia, J.P.; Serrano, L.P.; Forte, A.J. Artificial intelligence and lymphedema: State of the art. J. Clin. Transl. Res. 2022, 8, 234–242. [Google Scholar] [PubMed]
- Briganti, V.; Cuccurullo, V.; Di Stasio, G.D.; Mansi, L. Gamma emitters in pancreatic endocrine tumors imaging in the pet era: Is there a clinical space for 99mTc-peptides? Curr. Radiopharm. 2019, 12, 156–170. [Google Scholar] [CrossRef]
- Cuccurullo, V.; Manti, F.; De Risi, M.; Cascini, G.L. DG-CT/PET false positive case in hip prosthesis: A clue to avoid error. Radiol. Case Rep. 2021, 16, 2601–2604. [Google Scholar] [CrossRef] [PubMed]
- Cuccurullo, V.; Di Stasio, G.D.; Manti, F.; Arcuri, P.; Damiano, R.; Cascini, G.L. The Role of Molecular Imaging in a Muscle-Invasive Bladder Cancer Patient: A Narrative Review in the Era of Multimodality Treatment. Diagnostics 2021, 11, 863. [Google Scholar] [CrossRef]
- Parmeggiani, D.; Gambardella, C.; Patrone, R.; Polistena, A.; De Falco, M.; Ruggiero, R.; Cirocchi, R.; Sanguinetti, A.; Cuccurullo, V.; Accardo, M.; et al. Radioguided thyroidectomy for follicular tumors: Multicentric experience. Int. J. Surg. 2017, 41 (Suppl. S1), S75–S81. [Google Scholar] [CrossRef] [PubMed]
- Cuccurullo, V.; Di Stasio, G.D.; Mansi, L. Radioguided surgery with radiolabeled somatostatin analogs: Not only in GEP-NETs. Nucl. Med. Rev. 2017, 20, 49–56. [Google Scholar] [CrossRef]
- Cuccurullo, V.; Cioce, F.; Sica, A.; Gatta, G.; Rubini, G. Gastroenteric diseases in the third millennium: A rational approach to optimal imaging technique and patient selection. Recent. Progress. Med. 2012, 103, 426–430. [Google Scholar]
- Cuccurullo, V.; Di Stasio, G.; Prisco, M.; Mansi, L. Is there a clinical usefulness for radiolabeled somatostatin analogues beyond the consolidated role in NETs? Indian J. Radiol. Imaging 2017, 27, 509–516. [Google Scholar]
- Wijaya, W.A.; Peng, J.; He, Y.; Chen, J.; Cen, Y. Clinical application of axillary reverse mapping in patients with breast cancer: A systematic review and meta-analysis. Breast 2020, 53, 189–200. [Google Scholar] [CrossRef] [PubMed]
- Rajpurkar, P.; Lungren, M.P. The Current and Future State of AI Interpretation of Medical Images. N. Engl. J. Med. 2023, 388, 1981–1990. [Google Scholar] [CrossRef] [PubMed]
- Ciudad, P.; Bolletta, A.; Kaciulyte, J.; Losco, L.; Manrique, O.J.; Cigna, E.; Mayer, H.F.; Escandón, J.M. The breast cancer-related lymphedema multidisciplinary approach: Algorithm for conservative and multimodal surgical treatment. Microsurgery 2023, 43, 427–436. [Google Scholar] [CrossRef] [PubMed]
- Kaciulyte, J.; Garutti, L.; Spadoni, D.; Velazquez-Mujica, J.; Losco, L.; Ciudad, P.; Marcasciano, M.; Lo Torto, F.; Casella, D.; Ribuffo, D.; et al. Genital Lymphedema and How to Deal with It: Pearls and Pitfalls from over 38 Years of Experience with Unusual Lymphatic System Impairment. Medicina 2021, 57, 1175. [Google Scholar] [CrossRef]
- Forte, A.J.; Boczar, D.; Huayllani, M.T.; Lu, X.; Ciudad, P. Lymphoscintigraphy for Evaluation of Lymphedema Treatment: A Systematic Review. Cureus 2019, 11, e6363. [Google Scholar] [CrossRef] [PubMed]
- Yamamoto, T.; Yamamoto, N. Indocyanine Green Lymphography for Evaluation of Breast Lymphedema Secondary to Breast Cancer Treatments. J. Reconstr. Microsurg. 2022, 38, 630–636. [Google Scholar] [CrossRef]
- Salehi, B.P.; Sibley, R.C.; Friedman, R.; Kim, G.; Singhal, D.; Loening, A.M.; Tsai, L.L. MRI of Lymphedema. J. Magn. Reason. Imaging 2023, 57, 977–991. [Google Scholar] [CrossRef]
- Lahtinen, O.; Vanninen, R.; Rautiainen, S. Contrast-enhanced ultrasound: A new tool for imaging the superficial lymphatic vessels of the upper limb. Eur. Radiol. Exp. 2022, 6, 18. [Google Scholar] [CrossRef]

| Category | Normal Lymphatic Drainage | Partial Obstruction | Total Obstruction | ||||
|---|---|---|---|---|---|---|---|
| Score | L-0 | P-1 | P-2 | P-3 | T-4 | T-5 | T-6 |
| Proximal Lymph Node | + | +/↓ | ↓ | - | - | - | - |
| Intermediate Lymph Node | - | - | +/- | + | - | - | - |
| Lymphatic Ducts | + | +/Distal | Distal/Engorged | - | Engorged/- | Engorged/- | - |
| Dermal Backflow | - | - | + (Proximal/Distal) | + (Distal/Entire) | + (Distal) | + (Entire) | - |
| Grade | Circumferential Difference (%) | Episodes of Cellulitis (Time/Year) | Taiwan Lymphoscintigraphy Staging | ICG Lymphography | Treatment | |
|---|---|---|---|---|---|---|
| 0 | 0–9 | 0–1 | L-0, P-1, P-2 | Patent lymphatic ducts | CDT LVA | |
| I | IA | 10–19 | 1–2 | P-1, P-2, P-3 | Patent lymphatic ducts | LVA |
| IB | P-3, T-4 | Diffuse dermal backflow | VLN transfer | |||
| II | IIA | 20–29 | 2–3 | P-1, P-2, P-3 | Patent lymphatic ducts | LVA |
| IIB | P-3, T-4, T-5 | Diffuse dermal backflow | VLN transfer | |||
| III | 30–39 | 3–4 | P-3, T-4, T-5, T-6 | Not performed | VLN transfer +additional procedures | |
| IV | >40 | >4 | T-4, T-5, T-6 | Not performed | VLN transfer +additional procedures |
| Stage | 0 | 1 | 2 | 3 | 4 | 5 |
|---|---|---|---|---|---|---|
| Patent lymphatic vessels | ++++ | +++ | ++ | + | 0 | 0 |
| Dermal backflow | 0 | 1 | ++ | +++ | ++++ finger/toe pal/signs | 0 |
| Lymphatic vessel contractility | ++++ | +++ | ++ | + | 0 | 0 |
| Advantages | Disadvantages | Ref. | |
|---|---|---|---|
| Lymphoscintigraphy | Gold-standard method capable of assessing lymphodynamics and hallmark features such as dermal backflow underlying major staging systems. Can also define quantitative parameters such as transit time and amount of radiotracer accumulation and compare them with contralateral limb. Relatively low radiant dose (1 Sv), lower than other roentgendiagnostic methods. | Low spatial resolution in accurate identification of lymphatic vessels, even with SPECT-CT methods showing lower definition than other methods. Use of ionizing radiation and a dedicated nuclear medicine department. Relative high cost of radiotracer. | [58] |
| ICG lymphography | Real-time method with very high spatial resolution of the superficial lymphatic network that can accurately identify flow alterations such as the presence of dermal backflow. Ability to use the method in operative time to identify potential target vessels for LVA. Increased availability of the method due to small and portable NIR camera. | Inability to study lymphatic structures located more than 2–3 cm deep. High cost of contrast medium and operator-dependent method. | [59] |
| MRI lymphangiography | Best anatomical definition among methods of both superficial and deep lymphatic vessels essential for proper surgical planning. Possibility of not using contrast medium thanks to dedicated sequences such as STIR and DWI. Possibility to define quantitative parameters such as flow velocity and to integrate AI protocols. | Low availability of the method and possible artifacts as well as lack of standardized protocols. | [60] |
| Contrast enhancement ultrasound (CEUS) | Potential wide availability of the method with low cost. Transportability of the machine and possibility of real-time use during surgery. | Operator-dependent method with low spatial resolution with possibility of obtaining a limited number of parameters such as identification of large lymphatic vessels. | [61] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cuccurullo, V.; Rapa, M.; Catalfamo, B.; Gatta, G.; Di Grezia, G.; Cascini, G.L. The Role of Imaging of Lymphatic System to Prevent Cancer Related Lymphedema. Bioengineering 2023, 10, 1407. https://doi.org/10.3390/bioengineering10121407
Cuccurullo V, Rapa M, Catalfamo B, Gatta G, Di Grezia G, Cascini GL. The Role of Imaging of Lymphatic System to Prevent Cancer Related Lymphedema. Bioengineering. 2023; 10(12):1407. https://doi.org/10.3390/bioengineering10121407
Chicago/Turabian StyleCuccurullo, Vincenzo, Marco Rapa, Barbara Catalfamo, Gianluca Gatta, Graziella Di Grezia, and Giuseppe Lucio Cascini. 2023. "The Role of Imaging of Lymphatic System to Prevent Cancer Related Lymphedema" Bioengineering 10, no. 12: 1407. https://doi.org/10.3390/bioengineering10121407
APA StyleCuccurullo, V., Rapa, M., Catalfamo, B., Gatta, G., Di Grezia, G., & Cascini, G. L. (2023). The Role of Imaging of Lymphatic System to Prevent Cancer Related Lymphedema. Bioengineering, 10(12), 1407. https://doi.org/10.3390/bioengineering10121407










