Development and Validation of an Artificial Intelligence Preoperative Planning and Patient-Specific Instrumentation System for Total Knee Arthroplasty
Abstract
:1. Introduction
2. Materials and Methods
2.1. Development and Construction of the Artificial Intelligence Preoperative Planning and Patient-Specific Instrumentation System for Total Knee Arthroplasty (AIJOINT)
2.1.1. CT Data Acquisition
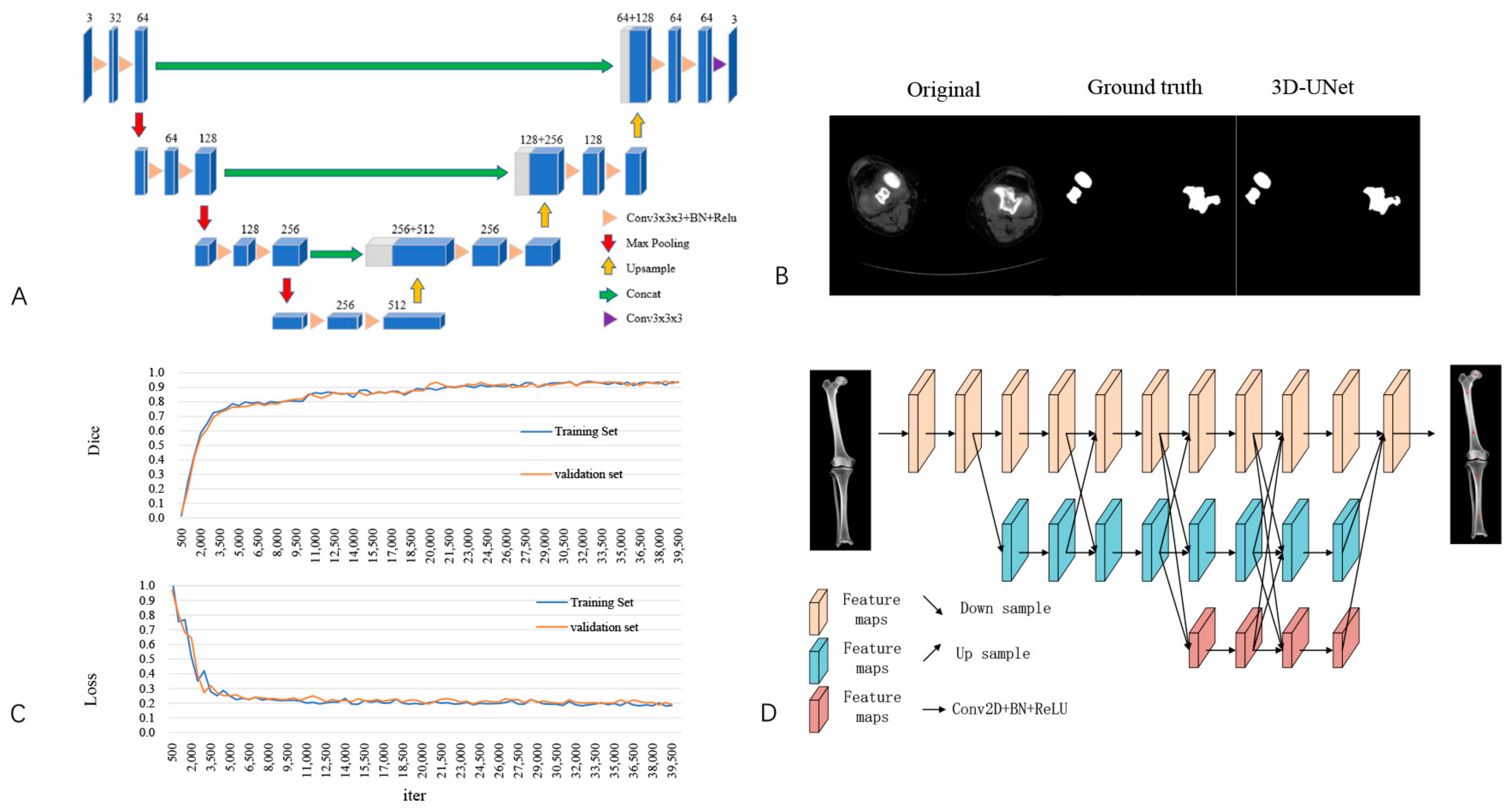
2.1.2. Image Segmentation
2.1.3. Identification of Feature Anatomic Landmarks
2.1.4. Preoperative Planning Module
2.1.5. PSI Design Module
2.2. Clinical Validation of the AIJOINT
2.2.1. Component Size Planning
2.2.2. PSI Design
2.2.3. Surgical Technique
2.2.4. Radiographic and Clinical Outcomes
2.3. Data Analyses
3. Results
3.1. Validation of Artificial Intelligence Algorithms
3.2. Accuracy of 3D and Acetate Templating Compared with the Final Component
3.3. Accuracy of PSI-Assisted Component Positioning
3.4. Perioperative Outcomes
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Villa, J.M.; Singh, V.; Higuera-Rueda, C.A. What’s new in adult reconstructive knee surgery. J. Bone. Joint. Surg. Am. 2023, 105, 89–97. [Google Scholar] [CrossRef] [PubMed]
- Singh, J.A.; Yu, S.; Chen, L.; Cleveland, J.D. Rates of total joint replacement in the United States: Future projections to 2020–2040 using the national inpatient sample. J. Rheumatol. 2019, 46, 1134–1140. [Google Scholar] [CrossRef] [PubMed]
- Gunaratne, R.; Pratt, D.N.; Banda, J.; Fick, D.P.; Khan, R.; Robertson, B.W. Patient dissatisfaction following total knee arthroplasty: A systematic review of the literature. J. Arthroplast. 2017, 32, 3854–3860. [Google Scholar] [CrossRef] [PubMed]
- Lee, G.C.; Lotke, P.A. Can surgeons predict what makes a good tka? Intraoperative surgeon impression of tka quality does not correlate with knee society scores. Clin. Orthop. Relat. Res. 2012, 470, 159–165. [Google Scholar] [CrossRef]
- Insall, J.N.; Binazzi, R.; Soudry, M.; Mestriner, L.A. Total knee arthroplasty. Clin. Orthop. Relat. Res. 1985, 192, 13–22. [Google Scholar] [CrossRef]
- Bargren, J.H.; Blaha, J.D.; Freeman, M.A. Alignment in total knee arthroplasty. Correlated biomechanical and clinical observations. Clin. Orthop. Relat. Res. 1983, 173, 178–183. [Google Scholar] [CrossRef]
- Lambrechts, A.; Wirix-Speetjens, R.; Maes, F.; Van Huffel, S. Artificial intelligence based patient-specific preoperative planning algorithm for total knee arthroplasty. Front. Robot. AI 2022, 9, 840282. [Google Scholar] [CrossRef]
- Trickett, R.W.; Hodgson, P.; Forster, M.C.; Robertson, A. The reliability and accuracy of digital templating in total knee replacement. J. Bone Jt. Surg. Br. 2009, 91, 903–906. [Google Scholar] [CrossRef]
- Ooka, N.; Campos, A.; Da, F.V.; Rodrigues, L.; Filho, E.B.; Franco, J.S.; Pires e Albuquerque, R.S.; Gameiro, V.S. Pre-operative templating for knee arthroplasty shows low accuracy with standard x-rays. Int. Orthop. 2018, 42, 1275–1282. [Google Scholar] [CrossRef]
- Iorio, R.; Siegel, J.; Specht, L.M.; Tilzey, J.F.; Hartman, A.; Healy, W.L. A comparison of acetate vs. digital templating for preoperative planning of total hip arthroplasty: Is digital templating accurate and safe? J. Arthroplast. 2009, 24, 175–179. [Google Scholar] [CrossRef]
- Pietrzak, J.; Rowan, F.E.; Kayani, B.; Donaldson, M.J.; Huq, S.S.; Haddad, F.S. Preoperative ct-based three-dimensional templating in robot-assisted total knee arthroplasty more accurately predicts implant sizes than two-dimensional templating. J. Knee Surg. 2019, 32, 642–648. [Google Scholar] [CrossRef] [PubMed]
- Wen, L.; Wang, Z.; Ma, D.; Qu, T. Surgeon dominated design can improve the accuracy of patient-specific instruments in kinematically aligned tka. J. Pers. Med. 2022, 12, 1192. [Google Scholar] [CrossRef] [PubMed]
- Zarychta, P. Atlas-based segmentation in extraction of knee joint bone structures from ct and mr. Sensors 2022, 22, 8960. [Google Scholar] [CrossRef] [PubMed]
- Lei, K.; Liu, L.; Yang, P.; Xiong, R.; Yang, L.; He, R.; Guo, L. Robotics versus personalized 3d preoperative planning in total knee arthroplasty: A propensity score-matched analysis. J. Orthop. Surg. Res. 2022, 17, 227. [Google Scholar] [CrossRef] [PubMed]
- Liow, M.H.; Goh, G.S.; Pang, H.N.; Tay, D.K.; Lo, N.N.; Yeo, S.J. Computer-assisted stereotaxic navigation improves the accuracy of mechanical alignment and component positioning in total knee arthroplasty. Arch. Orthop. Trauma. Surg. 2016, 136, 1173–1180. [Google Scholar] [CrossRef]
- Meng, M.; Wang, J.; Sun, T.; Zhang, W.; Zhang, J.; Shu, L.; Li, Z. Clinical applications and prospects of 3d printing guide templates in orthopaedics. J. Orthop. Transl. 2022, 34, 22–41. [Google Scholar] [CrossRef]
- Victor, J.; Dujardin, J.; Vandenneucker, H.; Arnout, N.; Bellemans, J. Patient-specific guides do not improve accuracy in total knee arthroplasty: A prospective randomized controlled trial. Clin. Orthop. Relat. Res. 2014, 472, 263–271. [Google Scholar] [CrossRef]
- Chareancholvanich, K.; Narkbunnam, R.; Pornrattanamaneewong, C. A prospective randomised controlled study of patient-specific cutting guides compared with conventional instrumentation in total knee replacement. Bone Joint J. 2013, 95-B, 354–359. [Google Scholar] [CrossRef]
- Chen, X.; Li, S.; Wang, Y.; Liu, X.; Zhang, Y.; Qiu, G.; Qian, W. Artificially intelligent three-dimensionally -printed patient-specific instrument improves total hip arthroplasty accuracy. J. Arthroplast. 2022, 38, 2060–2067.e1. [Google Scholar] [CrossRef]
- Haug, C.J.; Drazen, J.M. Artificial intelligence and machine learning in clinical medicine, 2023. N. Engl. J. Med. 2023, 388, 1201–1208. [Google Scholar] [CrossRef]
- Cleland, J.; Li, C.; Jones, Y. Artificial intelligence needs clinical intelligence to succeed. JACC Heart Fail. 2020, 8, 588–591. [Google Scholar] [CrossRef]
- Haeberle, H.S.; Helm, J.M.; Navarro, S.M.; Karnuta, J.M.; Schaffer, J.L.; Callaghan, J.J.; Mont, M.A.; Kamath, A.F.; Krebs, V.E.; Ramkumar, P.N. Artificial intelligence and machine learning in lower extremity arthroplasty: A review. J. Arthroplast. 2019, 34, 2201–2203. [Google Scholar] [CrossRef]
- Potocnik, J.; Foley, S.; Thomas, E. Current and potential applications of artificial intelligence in medical imaging practice: A narrative review. J. Med. Imaging Radiat. Sci. 2023, 54, 376–385. [Google Scholar] [CrossRef]
- Xue, T.; Wallin, T.J.; Menguc, Y.; Adriaenssens, S.; Chiaramonte, M. Machine learning generative models for automatic design of multi-material 3d printed composite solids. Extreme Mech. Lett. 2020, 41, 100992. [Google Scholar] [CrossRef]
- Song, S.Y.; Seo, M.S.; Kim, C.W.; Kim, Y.H.; Yoo, B.C.; Choi, H.J.; Seo, S.H.; Kang, S.W.; Song, M.G.; Nam, D.C.; et al. Ai-driven segmentation and automated analysis of the whole sagittal spine from x-ray images for spinopelvic parameter evaluation. Bioengineering 2023, 10, 1229. [Google Scholar] [CrossRef] [PubMed]
- Shen, X.; Luo, J.; Tang, X.; Chen, B.; Qin, Y.; Zhou, Y.; Xiao, J. Deep learning approach for diagnosing early osteonecrosis of the femoral head based on magnetic resonance imaging. J. Arthroplast. 2023, 38, 2044–2050. [Google Scholar] [CrossRef] [PubMed]
- Lei, K.; Liu, L.M.; Xiang, Y.; Chen, X.; Fan, H.Q.; Peng, Y.; Luo, J.M.; Guo, L. Clinical value of ct-based patient-specific 3d preoperative design combined with conventional instruments in primary total knee arthroplasty: A propensity score-matched analysis. J. Orthop. Surg. Res. 2020, 15, 591. [Google Scholar] [CrossRef] [PubMed]
- Peek, A.C.; Bloch, B.; Auld, J. How useful is templating for total knee replacement component sizing? Knee 2012, 19, 266–269. [Google Scholar] [CrossRef] [PubMed]
- Huang, S.Y.; Hsu, W.L.; Hsu, R.J.; Liu, D.W. Fully convolutional network for the semantic segmentation of medical images: A survey. Diagnostics 2022, 12, 2765. [Google Scholar] [CrossRef] [PubMed]
- Hong, J.H.; Hong, H.; Choi, Y.R.; Kim, D.H.; Kim, J.Y.; Yoon, J.H.; Yoon, S.H. Ct analysis of thoracolumbar body composition for estimating whole-body composition. Insights Imaging 2023, 14, 69. [Google Scholar] [CrossRef] [PubMed]
- Xia, L. Auxiliary diagnosis of lung cancer with magnetic resonance imaging data under deep learning. Comput. Math. Method Med. 2022, 2022, 1994082. [Google Scholar] [CrossRef] [PubMed]
- Gonzalez, M.H.; Mekhail, A.O. The failed total knee arthroplasty: Evaluation and etiology. J. Am. Acad. Orthop. Surg. 2004, 12, 436–446. [Google Scholar] [CrossRef] [PubMed]
- Dennis, D.A. Evaluation of painful total knee arthroplasty. J. Arthroplast. 2004, 19, 35–40. [Google Scholar] [CrossRef]
- Lesh, M.L.; Schneider, D.J.; Deol, G.; Davis, B.; Jacobs, C.R.; Pellegrini, V.J. The consequences of anterior femoral notching in total knee arthroplasty. A biomechanical study. J. Bone. Joint. Surg. Am. 2000, 82, 1096–1101. [Google Scholar] [CrossRef] [PubMed]
- Altintas, F.; Sener, N.; Ugutmen, E. Fracture of the tibial tray after total knee arthroplasty. J. Arthroplast. 1999, 14, 112–114. [Google Scholar] [CrossRef]
- Hafez, M.A.; Moholkar, K. Patient-specific instruments: Advantages and pitfalls. SICOT J. 2017, 3, 66. [Google Scholar] [CrossRef]
- Longstaff, L.M.; Sloan, K.; Stamp, N.; Scaddan, M.; Beaver, R. Good alignment after total knee arthroplasty leads to faster rehabilitation and better function. J. Arthroplast. 2009, 24, 570–578. [Google Scholar] [CrossRef]
- Howell, S.M.; Shelton, T.J.; Hull, M.L. Implant survival and function ten years after kinematically aligned total knee arthroplasty. J. Arthroplast. 2018, 33, 3678–3684. [Google Scholar] [CrossRef]
- Li, J.T.; Gao, X.; Li, X. Comparison of iassist navigation system with conventional techniques in total knee arthroplasty: A systematic review and meta-analysis of radiographic and clinical outcomes. Orthop. Surg. 2019, 11, 985–993. [Google Scholar] [CrossRef]
- Bouche, P.A.; Corsia, S.; Dechartres, A.; Resche-Rigon, M.; Nizard, R. Are there differences in accuracy or outcomes scores among navigated, robotic, patient-specific instruments or standard cutting guides in tka? A network meta-analysis. Clin. Orthop. Relat. Res. 2020, 478, 2105–2116. [Google Scholar] [CrossRef]
- Vide, J.; Freitas, T.P.; Ramos, A.; Cruz, H.; Sousa, J.P. Patient-specific instrumentation in total knee arthroplasty: Simpler, faster and more accurate than standard instrumentation-a randomized controlled trial. Knee Surg. Sports Traumatol. Arthrosc. 2017, 25, 2616–2621. [Google Scholar] [CrossRef] [PubMed]
- Huijbregts, H.J.; Khan, R.J.; Fick, D.P.; Hall, M.J.; Punwar, S.A.; Sorensen, E.; Reid, M.J.; Vedove, S.D.; Haebich, S. Component alignment and clinical outcome following total knee arthroplasty: A randomised controlled trial comparing an intramedullary alignment system with patient-specific instrumentation. Bone Joint J. 2016, 98-B, 1043–1049. [Google Scholar] [CrossRef] [PubMed]
- Lei, K.; Liu, L.; Chen, X.; Feng, Q.; Yang, L.; Guo, L. Navigation and robotics improved alignment compared with psi and conventional instrument, while clinical outcomes were similar in tka: A network meta-analysis. Knee Surg. Sports Traumatol. Arthrosc. 2022, 30, 721–733. [Google Scholar] [CrossRef] [PubMed]
- Kotela, A.; Kotela, I. Patient-specific computed tomography based instrumentation in total knee arthroplasty: A prospective randomized controlled study. Int. Orthop. 2014, 38, 2099–2107. [Google Scholar] [CrossRef] [PubMed]
- Gong, S.; Xu, W.; Wang, R.; Wang, Z.; Wang, B.; Han, L.; Chen, G. Patient-specific instrumentation improved axial alignment of the femoral component, operative time and perioperative blood loss after total knee arthroplasty. Knee Surg. Sports Traumatol. Arthrosc. 2019, 27, 1083–1095. [Google Scholar] [CrossRef]
- Thienpont, E.; Schwab, P.E.; Fennema, P. Efficacy of patient-specific instruments in total knee arthroplasty: A systematic review and meta-analysis. J. Bone. Joint. Surg. Am. 2017, 99, 521–530. [Google Scholar] [CrossRef]




| AIJOINT Group (n = 20) | Conventional Group (n = 20) | p Value | |
|---|---|---|---|
| Age (years) | 67.95 ± 5.65 | 69.90 ± 4.71 | 0.643 |
| Sex (men/women) | 6/14 | 6/14 | 1.000 |
| BMI (kg/m2) | 25.11 ± 3.53 | 25.06 ± 3.09 | 0.630 |
| Side (left/right) | 9/11 | 9/11 | 1.000 |
| ASA score | 2.10 ± 0.72 | 2.05 ± 0.61 | 0.618 |
| AIJOINT Group (n = 42) | Conventional Group (n = 42) | p Value | |
|---|---|---|---|
| Femoral Component Size Between Preoperative Planning and Postoperative Results (n,%) | |||
| Same | 39 (92.9%) | 18 (42.9%) | 0.001 |
| ±1 size | 42 (100%) | 27 (64.3%) | 0.001 |
| ±2 sizes | 42 (100%) | 37 (88.1%) | 0.055 |
| Tibial Component Size Between Preoperative Planning and Postoperative Results (n,%) | |||
| Same | 39 (92.9%) | 20 (47.6%) | 0.001 |
| ±1 size | 42 (100%) | 28 (66.7%) | 0.001 |
| ±2 sizes | 42 (100%) | 36 (85.7%) | 0.026 |
| AIJOINT Group (n = 20) | Conventional Group (n = 20) | p Value | |
|---|---|---|---|
| Outlier of LDFA (°) | 1.45 ± 1.70 | 2.20 ± 1.96 | 0.204 |
| Outlier of MPTA (°) | 1.60 ± 1.82 | 2.65 ± 1.84 | 0.078 |
| Outlier of HKA (°) | 1.55 ± 1.43 | 3.35 ± 2.56 | 0.010 |
| Outlier of LDFA ≤ 3°(n, %) | 18(90.0%) | 16(80.0%) | 0.661 |
| Outlier of MPTA ≤ 3°(n, %) | 17(85.0%) | 15(75.0%) | 0.695 |
| Outlier of HKA ≤ 3°(n, %) | 18(90.0%) | 10(50.0%) | 0.014 |
| AIJOINT Group (n = 20) | Conventional Group (n = 20) | p Value | |
|---|---|---|---|
| Tourniquet time (min) | 65.10 ± 6.77 | 74.55 ± 5.86 | 0.719 |
| Length of stay (days) | 8.15 ± 1.35 | 7.60 ± 2.06 | 0.491 |
| Hb decreased (g/L) | 13.50 ± 5.78 | 18.85 ± 10.32 | 0.029 |
| DVT (n) | 0 | 0 | 1.000 |
| Incision complications (n) | 0 | 1 | 0.999 |
| Infection (n) | 0 | 0 | 1.000 |
| Pin-related complications(n) | 0 | - | - |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Li, S.; Liu, X.; Chen, X.; Xu, H.; Zhang, Y.; Qian, W. Development and Validation of an Artificial Intelligence Preoperative Planning and Patient-Specific Instrumentation System for Total Knee Arthroplasty. Bioengineering 2023, 10, 1417. https://doi.org/10.3390/bioengineering10121417
Li S, Liu X, Chen X, Xu H, Zhang Y, Qian W. Development and Validation of an Artificial Intelligence Preoperative Planning and Patient-Specific Instrumentation System for Total Knee Arthroplasty. Bioengineering. 2023; 10(12):1417. https://doi.org/10.3390/bioengineering10121417
Chicago/Turabian StyleLi, Songlin, Xingyu Liu, Xi Chen, Hongjun Xu, Yiling Zhang, and Wenwei Qian. 2023. "Development and Validation of an Artificial Intelligence Preoperative Planning and Patient-Specific Instrumentation System for Total Knee Arthroplasty" Bioengineering 10, no. 12: 1417. https://doi.org/10.3390/bioengineering10121417
APA StyleLi, S., Liu, X., Chen, X., Xu, H., Zhang, Y., & Qian, W. (2023). Development and Validation of an Artificial Intelligence Preoperative Planning and Patient-Specific Instrumentation System for Total Knee Arthroplasty. Bioengineering, 10(12), 1417. https://doi.org/10.3390/bioengineering10121417








