Revolutionizing Patient Monitoring in Age-Related Macular Degeneration: A Comparative Study on the Necessity and Efficiency of the AMD VIEWER
Abstract
:1. Introduction
2. Materials and Methods
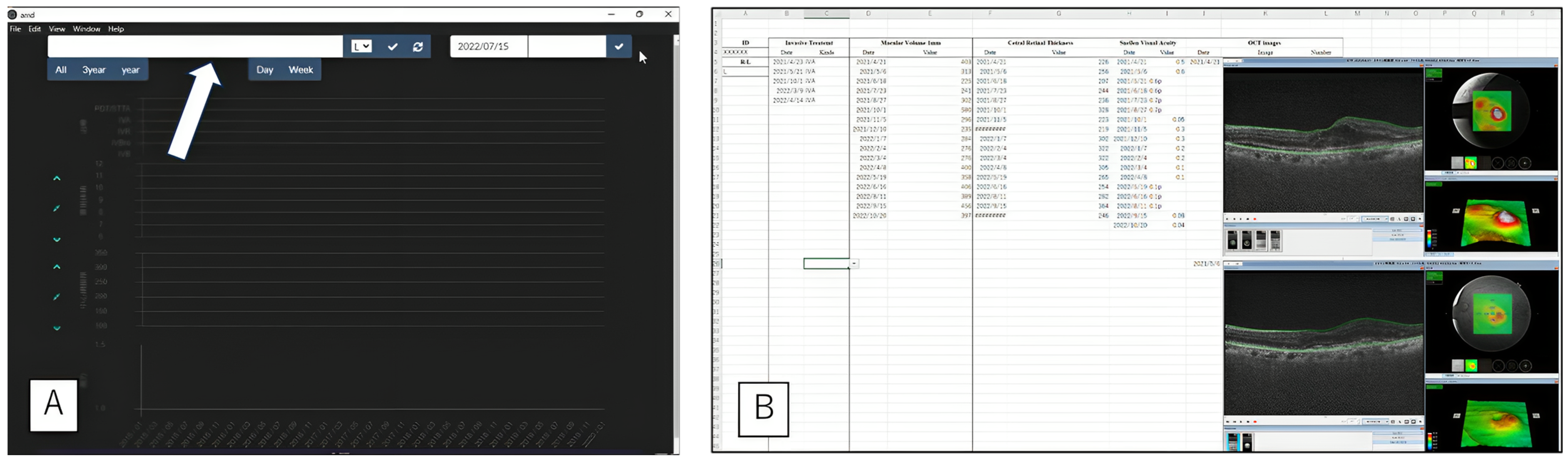
The AMD VIEWER
- System
- Main Application (Main App)
- OCT macular volume values
- OCT central retinal thickness
- Corrected 5-m visual acuity value
- OCT images
- A comparative of the clinic attendance frequency and minimum visual acuity in active and dropout groups of AMD patients
- Comparing time requirements and error rates between manual data entry and AMD VIEWER monitor display
- Evaluating the Usability of AMD VIEWER by Net Promoter Score (NPS)
- Statistical calculations
3. Results
3.1. AMD Patients
3.2. Efficiency of AMD VIEWER
3.3. Doctors’ Recommendation
4. Discussion
4.1. Principal Results
4.2. Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
References
- Adams, R.; Henry, K.E.; Sridharan, A.; Soleimani, H.; Zhan, A.; Rawat, N.; Johnson, L.; Hager, D.N.; Cosgrove, S.E.; Markowski, A.; et al. Prospective, multi-site study of patient outcomes after implementing the TREWS machine learning-based early warning system for sepsis. Nat. Med. 2022, 28, 1455–1460. [Google Scholar] [CrossRef] [PubMed]
- Li, E.; Donati, S.; Lindsley, K.B.; Krzystolik, M.G.; Virgili, G. Treatment regimens for administration of anti-vascular endothelial growth factor agents for neovascular age-related macular degeneration. Cochrane Database Syst. Rev. 2020, 2020, CD012208. [Google Scholar] [CrossRef]
- GBD 2019 Blindness; Vision Impairment Collaborators; Vision Loss Expert Group of the Global Burden of Disease Study. Causes of blindness and vision impairment in 2020 and trends over 30 years, and prevalence of avoidable blindness in relation to VISION 2020: The right to sight: An analysis for the global burden of disease study. Lancet Glob. Health 2021, 9, e144–e160. [Google Scholar] [CrossRef] [PubMed]
- Habib, A.E.; Abdel-Kader, A.A.; Eissa, I.M.; Awadein, A. Adherence to Intravitreal Anti-Vascular Endothelial Growth Factor (Anti-VEGF) drugs in diabetic macular edema in an egyptian population: A health belief model. Curr. Eye Res. 2019, 44, 303–310. [Google Scholar] [CrossRef] [PubMed]
- Hammer, C.H.; Ringel, S. The effects of amount of information provided and feedback of results on decision making efficiency. Hum. Factors 1965, 7, 513–519. [Google Scholar] [CrossRef] [PubMed]
- Pearce, I.; Amoaku, W.; Bailey, C.; Downey, L.; Gale, R.; Ghanchi, F.; Hamilton, R.; Mahmood, S.; Menon, G.; Nosek, J.; et al. The changing landscape for the management of patients with neovascular AMD: Brolucizumab in clinical practice. Eye 2022, 36, 1725–1734. [Google Scholar] [CrossRef] [PubMed]
- Taber, J.M.; Leyva, B.; Persoskie, A. Why do people avoid medical care? A qualitative study using national data. J. Gen. Intern. Med. 2015, 30, 290–297. [Google Scholar] [CrossRef] [PubMed]
- She, K.; Su, J.; Wang, Q.; Liu, Y.; Zhong, X.; Jin, X.; Zhao, Q.; Xiao, J.; Li, R.; Deng, H.; et al. Delivery of nVEGFi using AAV8 for the treatment of neovascular age-related macular degeneration. Mol. Ther. Methods Clin. Dev. 2022, 24, 210–221. [Google Scholar] [CrossRef] [PubMed]
- Hadziahmetovic, M.; Malek, G. Age-related macular degeneration revisited: From pathology and cellular stress to potential therapies. Front. Cell Dev. Biol. 2020, 8, 612812. [Google Scholar] [CrossRef] [PubMed]
- Okada, M.; Mitchell, P.; Finger, R.P.; Eldem, B.; Talks, S.J.; Hirst, C.; Paladini, L.; Barratt, J.; Wong, T.Y.; Loewenstein, A. Nonadherence or nonpersistence to intravitreal injection therapy for neovascular age-related macular degeneration: A mixed-methods systematic review. Ophthalmology 2021, 128, 234–247. [Google Scholar] [CrossRef] [PubMed]
- Reichheld, F.F. The one number you need to grow. Harv. Bus. Rev. 2003, 81, 46–54, 124, PMID:14712543. [Google Scholar]
- Lucero, K.S. Net Promoter Score (NPS): What Does Net Promoter Score Offer in the Evaluation of Continuing Medical Education? J. Eur. CME 2022, 11, 2152941, PMID:36465493; PMCID: PMC9718547. [Google Scholar] [CrossRef]
- Oluoch, T.; Santas, X.; Kwaro, D.; Were, M.; Biondich, P.; Bailey, C.; Abu-Hanna, A.; de Keizer, N. The effect of electronic medical record-based clinical decision support on HIV care in resource-constrained settings: A systematic review. Int. J. Med. Inform. 2012, 81, e83–e92. [Google Scholar] [CrossRef] [PubMed]
- Cho, S.C.; Park, K.H.; Park, S.J.; Joo, K.; Woo, S.J. Discontinuation of treatment and retreatment of neovascular age-related macular degeneration in the real-world: Bundang AMD cohort study report 5. Front. Med. 2023, 10, 1204026. [Google Scholar] [CrossRef] [PubMed]
- Ramakrishnan, M.S.; Yu, Y.; VanderBeek, B.L. Association of Visit Adherence and Visual Acuity in Patients With Neovascular Age-Related Macular Degeneration: Secondary Analysis of the Comparison of Age-Related Macular Degeneration Treatment Trial. JAMA Ophthalmol. 2020, 138, 237–242. [Google Scholar] [CrossRef] [PubMed]
- Hu, R.; Racette, L.; Chen, K.S.; Johnson, C.A. Functional assessment of glaucoma: Uncovering progression. Surv. Ophthalmol. 2020, 65, 639–661. [Google Scholar] [CrossRef] [PubMed]
- Shinozaki, A. Electronic medical records and machine learning in approaches to drug development. In Artificial Intelligence in Oncology Drug Discovery and Development; John, W.C., Belle, T., Eds.; IntechOpen: Rijeka, Croatia, 2020. [Google Scholar]
- Sparrow, J.M.; Grzeda, M.; Frost, A.; Liu, C.; Johnston, R.L.; Scanlon, P.; Pithara, C.; Elliott, D.; Donovan, J.; Joseph-Williams, N.; et al. Developing decision support tools incorporating personalised predictions of likely visual benefit versus harm for cataract surgery: Research programme. In Programme Grants for Applied Research; National Institute for Health and Care Research: Southampton, UK, 2022. [Google Scholar]
- Mathis, T.; Holz, F.G.; Sivaprasad, S.; Yoon, Y.H.; Eter, N.; Chen, L.-J.; Koh, A.; de Souza, E.C.; Staurenghi, G. Characterisation of macular neovascularisation subtypes in age-related macular degeneration to optimise treatment outcomes. Eye 2023, 37, 1758–1765. [Google Scholar] [CrossRef] [PubMed]
- Etheridge, T.; Liu, Z.; Nalbandyan, M.; Cleland, S.; Blodi, B.A.; Mares, J.A.; Bailey, S.; Wallace, R.; Gehrs, K.; Tinker, L.F.; et al. Association of macular thickness with age and age-related macular degeneration in the Carotenoids in Age-Related Eye Disease Study 2 (CAREDS2), an ancillary study of the women’s health initiative. Transl. Vis. Sci. Technol. 2021, 10, 39. [Google Scholar] [CrossRef] [PubMed]
- Yates, J.R., 3rd. Pivotal role of computers and software in mass spectrometry-SEQUEST and 20 years of tandem MS database searching. J. Am. Soc. Mass Spectrom. 2015, 26, 1804–1813. [Google Scholar] [CrossRef] [PubMed]
- Chen, C.; Lee, S.; Stevenson, H.W. Response Style and Cross-Cultural Comparisons of Rating Scales Among East Asian and North American Students. Psychol. Sci. 1995, 6, 170–175. [Google Scholar] [CrossRef]





| Total | Patients without Treatments | Patients with Treatments | Dropout Group | Active Group | p-Value (Dropout vs. Active) | |
|---|---|---|---|---|---|---|
| Number | 977 | 307 | 670 (including eight non-grouped patients a) | 315 | 347 | |
| Age | 76.1 (10.9) | 71.6 (12.9) | 78.1 (9.2) | 79.0 (8.8) | 77.3 (9.2) | p = 0.0124 by Tukey’s HSD test |
| Male (%) | 703 (72.0%) | 211 (68.7%) | 492 (73.4%) | 237 (75.2%) | 248 (71.5%) | p = 0.292 by Fisher’s exact test |
| Observation period (days) | 1609 (1457) | 902 (1183) | 1934 (1457) | 1650 (1376) | 2191 (1479) | p < 0.001 by Tukey’s HSD test |
| Consultations (times) | 34.9 (34.4) | 11.2 (14.4) | 45.7 (35.5) | 43.0 (35.5) | 48.4 (35.7) | p = 0.0491 by Tukey’s HSD test |
| Treatments (times) | 7.3 (11.7) | 0 | 10.6 (12.8) | 8.2 (9.3) | 12.9 (14.5) | p = 0.0491 by Tukey’s HSD test |
| Minimum corrected visual acuity (LogMAR b) | 0.726 (0.787) | 0.138 (0.395) | 1.00 (0.78) | 1.110 (0.782) | 0.890 (0.762) | p < 0.001 by Steel–Dwass test |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tabuchi, H.; Yamauchi, T.; Nagasawa, T.; Deguchi, H.; Tanabe, M.; Tanaka, H.; Yasukawa, T. Revolutionizing Patient Monitoring in Age-Related Macular Degeneration: A Comparative Study on the Necessity and Efficiency of the AMD VIEWER. Bioengineering 2023, 10, 1426. https://doi.org/10.3390/bioengineering10121426
Tabuchi H, Yamauchi T, Nagasawa T, Deguchi H, Tanabe M, Tanaka H, Yasukawa T. Revolutionizing Patient Monitoring in Age-Related Macular Degeneration: A Comparative Study on the Necessity and Efficiency of the AMD VIEWER. Bioengineering. 2023; 10(12):1426. https://doi.org/10.3390/bioengineering10121426
Chicago/Turabian StyleTabuchi, Hitoshi, Tomofusa Yamauchi, Toshihiko Nagasawa, Hodaka Deguchi, Mao Tanabe, Hayato Tanaka, and Tsutomu Yasukawa. 2023. "Revolutionizing Patient Monitoring in Age-Related Macular Degeneration: A Comparative Study on the Necessity and Efficiency of the AMD VIEWER" Bioengineering 10, no. 12: 1426. https://doi.org/10.3390/bioengineering10121426
APA StyleTabuchi, H., Yamauchi, T., Nagasawa, T., Deguchi, H., Tanabe, M., Tanaka, H., & Yasukawa, T. (2023). Revolutionizing Patient Monitoring in Age-Related Macular Degeneration: A Comparative Study on the Necessity and Efficiency of the AMD VIEWER. Bioengineering, 10(12), 1426. https://doi.org/10.3390/bioengineering10121426








