Hemodiafiltration: Technical and Medical Insights
Abstract
:1. Introduction
2. Technical Insights of HDF
2.1. The Substitution Fluid
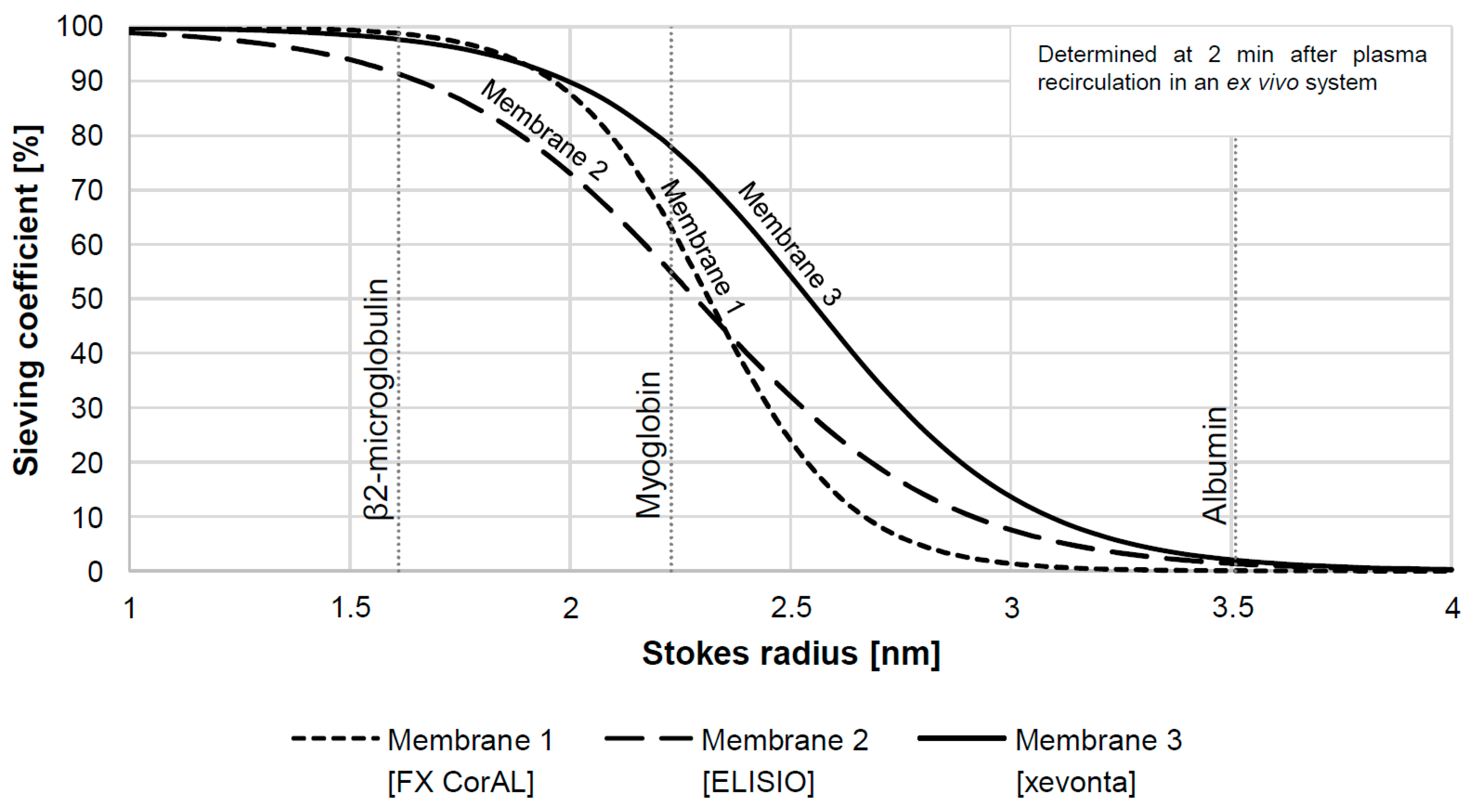
2.2. The Hemodiafilter
2.3. The Online HDF Machine
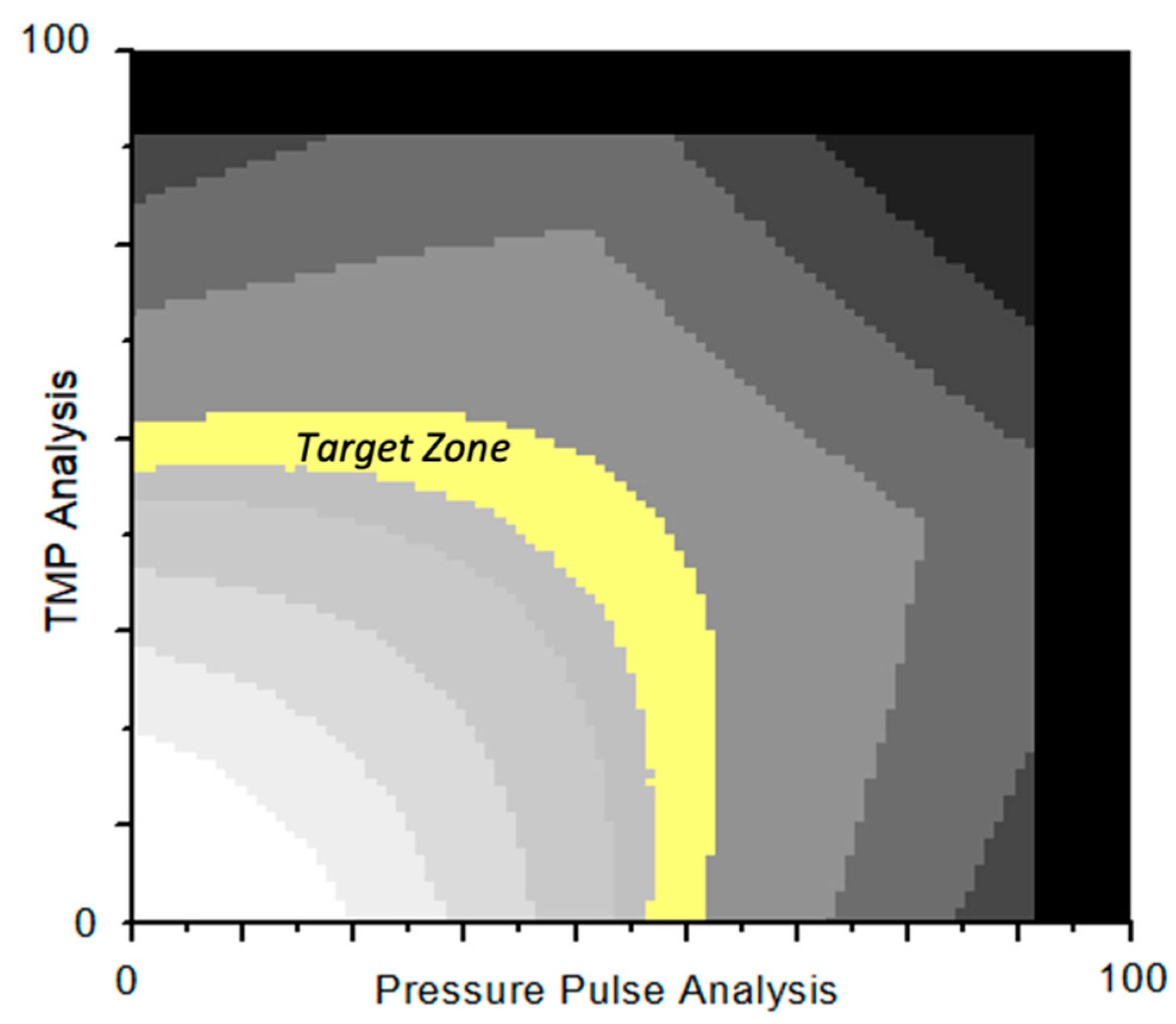
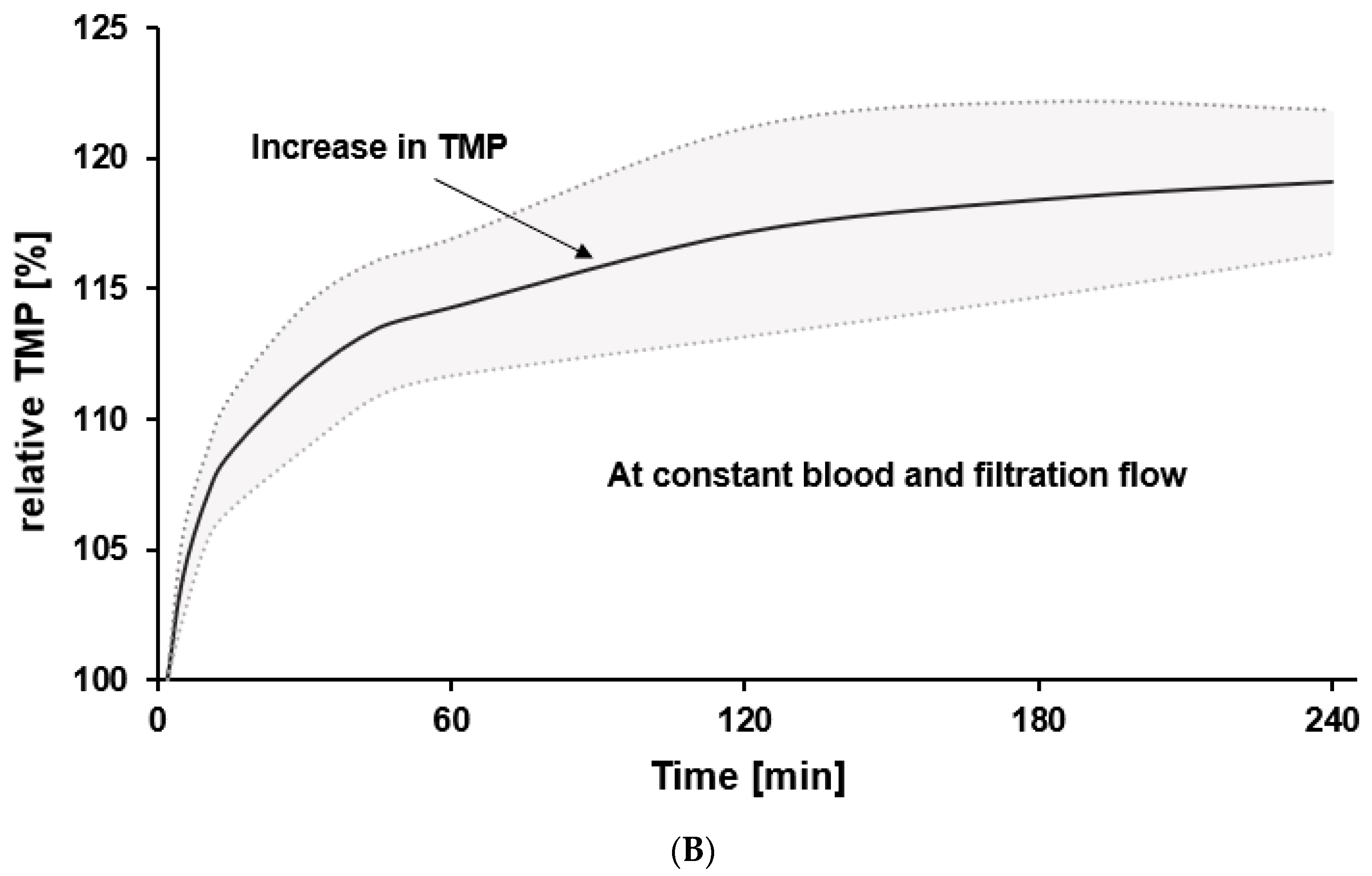
2.4. Impact of Protein Fouling of the Membrane on Substitution Volume
3. Medical Insights of HDF
3.1. Necessity of Advanced Treatment Options for ESKD Patients to Improve Outcomes
3.2. HDF vs. Other Modalities: Impact on Performances as Short-Term Surrogate Marker of Efficiency
3.3. Impact on Morbidity and Mortality as Hard Clinical Endpoint to Support Larger Use of HDF
3.4. Mechanisms for Beneficial Effects of HDF
4. Conclusions and Future Directions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Thurlow, J.S.; Joshi, M.; Yan, G.; Norris, K.C.; Agodoa, L.Y.; Yuan, C.M.; Nee, R. Global Epidemiology of End-Stage Kidney Disease and Disparities in Kidney Replacement Therapy. Am. J. Nephrol. 2021, 52, 98–107. [Google Scholar] [CrossRef]
- Bello, A.K.; Okpechi, I.G.; Osman, M.A.; Cho, Y.; Htay, H.; Jha, V.; Wainstein, M.; Johnson, D.W. Epidemiology of Haemodialysis Outcomes. Nat. Rev. Nephrol. 2022, 18, 378–395. [Google Scholar] [CrossRef] [PubMed]
- Go, A.S.; Chertow, G.M.; Fan, D.; McCulloch, C.E.; Hsu, C. Chronic Kidney Disease and the Risks of Death, Cardiovascular Events, and Hospitalization. N. Engl. J. Med. 2004, 351, 1296–1305. [Google Scholar] [CrossRef] [PubMed]
- Goodkin, D.A.; Bragg-Gresham, J.L.; Koenig, K.G.; Wolfe, R.A.; Akiba, T.; Andreucci, V.E.; Saito, A.; Rayner, H.C.; Kurokawa, K.; Port, F.K.; et al. Association of Comorbid Conditions and Mortality in Hemodialysis Patients in Europe, Japan, and the United States: The Dialysis Outcomes and Practice Patterns Study (DOPPS). J. Am. Soc. Nephrol. 2003, 14, 3270–3277. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Robinson, B.M.; Akizawa, T.; Jager, K.J.; Kerr, P.G.; Saran, R.; Pisoni, R.L. Factors Affecting Outcomes in Patients Reaching End-Stage Kidney Disease Worldwide: Differences in Access to Renal Replacement Therapy, Modality Use, and Haemodialysis Practices. Lancet 2016, 388, 294–306. [Google Scholar] [CrossRef] [PubMed]
- Cianciolo, G.; Donati, G.; La Manna, G.; Ferri, A.; Cuna, V.; Ubaldi, G.; Corsini, S.; Lanci, N.; Colì, L.; Stefoni, S. The Cardiovascular Burden of End-Stage Renal Disease Patients. Minerva Urol. Nefrol. 2010, 62, 51–66. [Google Scholar]
- Canaud, B.; Blankestijn, P.J.; Grooteman, M.P.C.; Davenport, A. Why and How High Volume Hemodiafiltration May Reduce Cardiovascular Mortality in Stage 5 Chronic Kidney Disease Dialysis Patients? A Comprehensive Literature Review on Mechanisms Involved. Semin. Dial. 2022, 35, 117–128. [Google Scholar] [CrossRef]
- Canaud, B.; Köhler, K.; Sichart, J.-M.; Möller, S. Global Prevalent Use, Trends and Practices in Haemodiafiltration. Nephrol. Dial. Transplant. 2020, 35, 398–407. [Google Scholar] [CrossRef]
- Ward, R.A.; Vienken, J.; Silverstein, D.M.; Ash, S.; Canaud, B. Kidney Health Initiative HDF Workgroup Regulatory Considerations for Hemodiafiltration in the United States. Clin. J. Am. Soc. Nephrol. 2018, 13, 1444–1449. [Google Scholar] [CrossRef] [Green Version]
- Ronco, C. Hemodiafiltration: Technical and Clinical Issues. Blood Purif. 2015, 40, 2–11. [Google Scholar] [CrossRef]
- Park, H.C.; Lee, Y.-K. Who Is the Winner, Pre-, Post-, or Mixed-Dilution Hemodiafiltration? Kidney Res. Clin. Pract. 2021, 40, 332–334. [Google Scholar] [CrossRef] [PubMed]
- Maduell, F.; Moreso, F.; Pons, M.; Ramos, R.; Mora-Macià, J.; Carreras, J.; Soler, J.; Torres, F.; Campistol, J.M.; Martinez-Castelao, A.; et al. High-Efficiency Postdilution Online Hemodiafiltration Reduces All-Cause Mortality in Hemodialysis Patients. J. Am. Soc. Nephrol. 2013, 24, 487–497. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Peters, S.A.E.; Bots, M.L.; Canaud, B.; Davenport, A.; Grooteman, M.P.C.; Kircelli, F.; Locatelli, F.; Maduell, F.; Morena, M.; Nubé, M.J.; et al. Haemodiafiltration and Mortality in End-Stage Kidney Disease Patients: A Pooled Individual Participant Data Analysis from Four Randomized Controlled Trials. Nephrol. Dial. Transplant. 2016, 31, 978–984. [Google Scholar] [CrossRef] [PubMed]
- Ok, E.; Asci, G.; Toz, H.; Ok, E.S.; Kircelli, F.; Yilmaz, M.; Hur, E.; Demirci, M.S.; Demirci, C.; Duman, S.; et al. Mortality and Cardiovascular Events in Online Haemodiafiltration (OL-HDF) Compared with High-Flux Dialysis: Results from the Turkish OL-HDF Study. Nephrol. Dial. Transplant. 2013, 28, 192–202. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Grooteman, M.P.C.; van den Dorpel, M.A.; Bots, M.L.; Penne, E.L.; van der Weerd, N.C.; Mazairac, A.H.A.; den Hoedt, C.H.; van der Tweel, I.; Lévesque, R.; Nubé, M.J.; et al. Effect of Online Hemodiafiltration on All-Cause Mortality and Cardiovascular Outcomes. J. Am. Soc. Nephrol. 2012, 23, 1087–1096. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mostovaya, I.M.; Blankestijn, P.J.; Bots, M.L.; Covic, A.; Davenport, A.; Grooteman, M.P.C.; Hegbrant, J.; Locatelli, F.; Vanholder, R.; Nubé, M.J. Clinical Evidence on Hemodiafiltration: A Systematic Review and a Meta-Analysis. Semin. Dial. 2014, 27, 119–127. [Google Scholar] [CrossRef]
- Vernooij, R.W.M.; Bots, M.L.; Strippoli, G.F.M.; Canaud, B.; Cromm, K.; Woodward, M.; Blankestijn, P.J. CONVINCE scientific committee CONVINCE in the Context of Existing Evidence on Haemodiafiltration. Nephrol. Dial. Transplant. 2022, 37, 1006–1013. [Google Scholar] [CrossRef]
- Caskey, F.J.; Procter, S.; MacNeill, S.J.; Wade, J.; Taylor, J.; Rooshenas, L.; Liu, Y.; Annaw, A.; Alloway, K.; Davenport, A.; et al. The High-Volume Haemodiafiltration vs High-Flux Haemodialysis Registry Trial (H4RT): A Multi-Centre, Unblinded, Randomised, Parallel-Group, Superiority Study to Compare the Effectiveness and Cost-Effectiveness of High-Volume Haemodiafiltration and High-Flux Haemodialysis in People with Kidney Failure on Maintenance Dialysis Using Linkage to Routine Healthcare Databases for Outcomes. Trials 2022, 23, 532. [Google Scholar] [CrossRef]
- Henderson, L.W. Biophysics of Ultrafiltration and Hemofiltration. In Replacement of Renal Function by Dialysis: A Textbook of dialysis; Maher, J.F., Ed.; Springer: Dordrecht, The Netherlands, 1989; pp. 300–326. ISBN 978-94-009-1087-4. [Google Scholar]
- Ronco, C.; Cruz, D. Hemodiafiltration History, Technology, and Clinical Results. Adv. Chronic Kidney Dis. 2007, 14, 231–243. [Google Scholar] [CrossRef]
- Canaud, B. Online Hemodiafiltration. Technical Options and Best Clinical Practices. Contrib. Nephrol. 2007, 158, 110–122. [Google Scholar] [CrossRef]
- Pstras, L.; Ronco, C.; Tattersall, J. Basic Physics of Hemodiafiltration. Semin. Dial. 2022, 35, 390–404. [Google Scholar] [CrossRef] [PubMed]
- Zawada, A.M.; Lang, T.; Ottillinger, B.; Kircelli, F.; Stauss-Grabo, M.; Kennedy, J.P. Impact of Hydrophilic Modification of Synthetic Dialysis Membranes on Hemocompatibility and Performance. Membranes 2022, 12, 932. [Google Scholar] [CrossRef] [PubMed]
- Zawada, A.M.; Melchior, P.; Schall, C.; Erlenkötter, A.; Lang, T.; Keller, T.; Stauss-Grabo, M.; Kennedy, J.P. Time-resolving Characterization of Molecular Weight Retention Changes among Three Synthetic High-flux Dialyzers. Artif. Organs 2022, 46, 1318–1327. [Google Scholar] [CrossRef] [PubMed]
- Röckel, A.; Hertel, J.; Fiegel, P.; Abdelhamid, S.; Panitz, N.; Walb, D. Permeability and Secondary Membrane Formation of a High Flux Polysulfone Hemofilter. Kidney Int. 1986, 30, 429–432. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kim, T.R.; Hadidi, M.; Motevalian, S.P.; Sunohara, T.; Zydney, A.L. Effects of Plasma Proteins on the Transport and Surface Characteristics of Polysulfone/Polyethersulfone and Asymmetric Cellulose Triacetate High Flux Dialyzers. Artif. Organs 2018, 42, 1070–1077. [Google Scholar] [CrossRef]
- Langsdorf, L.J.; Zydney, A.L. Effect of Blood Contact on the Transport Properties of Hemodialysis Membranes: A Two-Layer Membrane Model. Blood Purif. 1994, 12, 292–307. [Google Scholar] [CrossRef]
- Boschetti-de-Fierro, A.; Voigt, M.; Storr, M.; Krause, B. MCO Membranes: Enhanced Selectivity in High-Flux Class. Sci. Rep. 2015, 5, 18448. [Google Scholar] [CrossRef] [Green Version]
- Morti, S.M.; Zydney, A.L. Protein-Membrane Interactions during Hemodialysis: Effects on Solute Transport. ASAIO J. Am. Soc. Artif. Intern. Organs 1992 1998, 44, 319–326. [Google Scholar] [CrossRef]
- Santoro, A.; Ferramosca, E.; Mancini, E.; Monari, C.; Varasani, M.; Sereni, L.; Wratten, M. Reverse Mid-Dilution: New Way to Remove Small and Middle Molecules as Well as Phosphate with High Intrafilter Convective Clearance. Nephrol. Dial. Transplant. 2007, 22, 2000–2005. [Google Scholar] [CrossRef] [Green Version]
- Krieter, D.H.; Collins, G.; Summerton, J.; Spence, E.; Moragues, H.L.; Canaud, B. Mid-Dilution on-Line Haemodiafiltration in a Standard Dialyser Configuration. Nephrol. Dial. Transplant. 2005, 20, 155–160. [Google Scholar] [CrossRef] [Green Version]
- Shroff, R.; Smith, C.; Ranchin, B.; Bayazit, A.K.; Stefanidis, C.J.; Askiti, V.; Azukaitis, K.; Canpolat, N.; Ağbaş, A.; Aitkenhead, H.; et al. Effects of Hemodiafiltration versus Conventional Hemodialysis in Children with ESKD: The HDF, Heart and Height Study. J. Am. Soc. Nephrol. 2019, 30, 678–691. [Google Scholar] [CrossRef]
- Kikuchi, K.; Hamano, T.; Wada, A.; Nakai, S.; Masakane, I. Predilution Online Hemodiafiltration Is Associated with Improved Survival Compared with Hemodialysis. Kidney Int. 2019, 95, 929–938. [Google Scholar] [CrossRef]
- Canaud, B.; Lévesque, R.; Krieter, D.; Desmeules, S.; Chalabi, L.; Moragués, H.; Morena, M.; Cristol, J.-P. On-Line Hemodiafiltration as Routine Treatment of End-Stage Renal Failure: Why Pre- or Mixed Dilution Mode Is Necessary in On-Line Hemodiafiltration Today? Blood Purif. 2004, 22, 40–48. [Google Scholar] [CrossRef] [PubMed]
- Potier, J.; Bowry, S.; Canaud, B. Clinical Performance Assessment of CorDiax Filters in Hemodialysis and Hemodiafiltration. Contrib. Nephrol. 2017, 189, 237–245. [Google Scholar] [CrossRef] [PubMed]
- Potier, J.; Le Roy, F.; Faucon, J.P.; Besselièvre, T.; Renaudineau, E.; Farquet, C.; Soihan, P.; Touzard, D.; Djema, A.; Ilinca, T. Elevated Removal of Middle Molecules without Significant Albumin Loss with Mixed-Dilution Hemodiafiltration for Patients Unable to Provide Sufficient Blood Flow Rates. Blood Purif. 2013, 36, 78–83. [Google Scholar] [CrossRef]
- Ward, R.A. Basic Prerequisites for On-line, High-volume Hemodiafiltration. Semin. Dial. 2022, 35, 385–389. [Google Scholar] [CrossRef] [PubMed]
- Ward, R.A.; Beck, W.; Bernardo, A.A.; Alves, F.C.; Stenvinkel, P.; Lindholm, B. Hypoalbuminemia: A Price Worth Paying for Improved Dialytic Removal of Middle-Molecular-Weight Uremic Toxins? Nephrol. Dial. Transplant. 2019, 34, 901–907. [Google Scholar] [CrossRef]
- Canaud, B.; Barbieri, C.; Marcelli, D.; Bellocchio, F.; Bowry, S.; Mari, F.; Amato, C.; Gatti, E. Optimal Convection Volume for Improving Patient Outcomes in an International Incident Dialysis Cohort Treated with Online Hemodiafiltration. Kidney Int. 2015, 88, 1108–1116. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bowry, S.K.; Canaud, B. Achieving High Convective Volumes in On-Line Hemodiafiltration. Blood Purif. 2013, 35, 23–28. [Google Scholar] [CrossRef]
- Vega Vega, O.; Barraca Nunez, D.; Abad Esttebanez, S.; Bucalo, L.; Yuste, C.; López Gómez, J.M. FP457: Effects of a Reduced Inner Diameter of Hollow Fibers in Dialyzers in Online Hemodiafiltration. Nephrol. Dial. Transplant. 2012, 27, ii197–ii226. [Google Scholar] [CrossRef]
- Gayrard, N.; Ficheux, A.; Duranton, F.; Guzman, C.; Szwarc, I.; Vetromile, F.; Cazevieille, C.; Brunet, P.; Servel, M.-F.; Argilés, À.; et al. Consequences of Increasing Convection onto Patient Care and Protein Removal in Hemodialysis. PLoS ONE 2017, 12, e0171179. [Google Scholar] [CrossRef] [PubMed]
- Steckiph, D.; Calabrese, G.; Bertucci, A.; Mazzotta, A.; Vagelli, G.; Gonella, M. SP397—Improvement in Technology: Evaluation of the Biofeedback on TMP on Two Dialysis Systems. Nephrol. Dial. Transplant. 2013, 28, i202–i213. [Google Scholar] [CrossRef]
- Marcelli, D.; Scholz, C.; Ponce, P.; Sousa, T.; Kopperschmidt, P.; Grassmann, A.; Pinto, B.; Canaud, B. High-Volume Postdilution Hemodiafiltration Is a Feasible Option in Routine Clinical Practice. Artif. Organs 2015, 39, 142–149. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Teatini, U.; Steckiph, D.; Romei Longhena, G. Evaluation of a New Online Hemodiafiltration Mode with Automated Pressure Control of Convection. Blood Purif. 2011, 31, 259–267. [Google Scholar] [CrossRef] [PubMed]
- Ficheux, A.; Kerr, P.G.; Brunet, P.; Argiles, A. The Ultrafiltration Coefficient of a Dialyser (KUF) Is Not a Fixed Value, and It Follows a Parabolic Function: The New Concept of KUF Max. Nephrol. Dial. Transplant. 2011, 26, 636–640. [Google Scholar] [CrossRef] [PubMed]
- Kiguchi, T.; Ito, H.; Yamashita, A.C. Effect of Membrane Surface Area on Solute Removal Performance of Dialyzers with Fouling. Membranes 2022, 12, 684. [Google Scholar] [CrossRef]
- Huang, Z.; Gao, D.; Letteri, J.J.; Clark, W.R. Blood-Membrane Interactions during Dialysis. Semin. Dial. 2009, 22, 623–628. [Google Scholar] [CrossRef]
- Bosch, T.; Schmidt, B.; Samtleben, W.; Gurland, H.J. Effect of Protein Adsorption on Diffusive and Convective Transport through Polysulfone Membranes. Contrib. Nephrol. 1985, 46, 14–22. [Google Scholar] [CrossRef]
- Clark, W.R.; Gao, D. Low-Molecular Weight Proteins in End-Stage Renal Disease: Potential Toxicity and Dialytic Removal Mechanisms. J. Am. Soc. Nephrol. 2002, 13 (Suppl. S1), S41–S47. [Google Scholar] [CrossRef]
- Boschetti-de-Fierro, A.; Voigt, M.; Storr, M.; Krause, B. Extended Characterization of a New Class of Membranes for Blood Purification: The High Cut-off Membranes. Int. J. Artif. Organs 2013, 36, 455–463. [Google Scholar] [CrossRef]
- Melchior, P.; Erlenkötter, A.; Zawada, A.M.; Delinski, D.; Schall, C.; Stauss-Grabo, M.; Kennedy, J.P. Complement Activation by Dialysis Membranes and Its Association with Secondary Membrane Formation and Surface Charge. Artif. Organs 2021, 45, 770–778. [Google Scholar] [CrossRef]
- Ehlerding, G.; Ries, W.; Kempkes-Koch, M.; Ziegler, E.; Erlenkötter, A.; Zawada, A.M.; Kennedy, J.P.; Ottillinger, B.; Stauss-Grabo, M.; Lang, T. Randomized Comparison of Three High-Flux Dialyzers during High-Volume Online Hemodiafiltration—The ComPERFORM Study. Clin. Kidney J. 2022, 15, 672–680. [Google Scholar] [CrossRef] [PubMed]
- Ehlerding, G.; Erlenkötter, A.; Gauly, A.; Griesshaber, B.; Kennedy, J.; Rauber, L.; Ries, W.; Schmidt-Gürtler, H.; Stauss-Grabo, M.; Wagner, S.; et al. Performance and Hemocompatibility of a Novel Polysulfone Dialyzer: A Randomized Controlled Trial. Kidney360 2021, 2, 937–947. [Google Scholar] [CrossRef] [PubMed]
- Hayama, M.; Yamamoto, K.; Kohori, F.; Uesaka, T.; Ueno, Y.; Sugaya, H.; Itagaki, I.; Sakai, K. Nanoscopic Behavior of Polyvinylpyrrolidone Particles on Polysulfone/Polyvinylpyrrolidone Film. Biomaterials 2004, 25, 1019–1028. [Google Scholar] [CrossRef] [PubMed]
- Zhu, L.; Song, H.; Wang, J.; Xue, L. Polysulfone Hemodiafiltration Membranes with Enhanced Anti-Fouling and Hemocompatibility Modified by Poly(Vinyl Pyrrolidone) via in Situ Cross-Linked Polymerization. Mater. Sci. Eng. C Mater. Biol. Appl. 2017, 74, 159–166. [Google Scholar] [CrossRef]
- Jiang, J.; Zhu, L.; Zhu, L.; Zhang, H.; Zhu, B.; Xu, Y. Antifouling and Antimicrobial Polymer Membranes Based on Bioinspired Polydopamine and Strong Hydrogen-Bonded Poly(N -Vinyl Pyrrolidone). ACS Appl. Mater. Interfaces 2013, 5, 12895–12904. [Google Scholar] [CrossRef]
- Ran, F.; Nie, S.; Zhao, W.; Li, J.; Su, B.; Sun, S.; Zhao, C. Biocompatibility of Modified Polyethersulfone Membranes by Blending an Amphiphilic Triblock Co-Polymer of Poly(Vinyl Pyrrolidone)-b-Poly(Methyl Methacrylate)-b-Poly(Vinyl Pyrrolidone). Acta Biomater. 2011, 7, 3370–3381. [Google Scholar] [CrossRef]
- Hayama, M.; Yamamoto, K.; Kohori, F.; Sakai, K. How Polysulfone Dialysis Membranes Containing Polyvinylpyrrolidone Achieve Excellent Biocompatibility? J. Membr. Sci. 2004, 234, 41–49. [Google Scholar] [CrossRef]
- Wang, H.; Yu, T.; Zhao, C.; Du, Q. Improvement of Hydrophilicity and Blood Compatibility on Polyethersulfone Membrane by Adding Polyvinylpyrrolidone. Fibers Polym. 2009, 10, 1–5. [Google Scholar] [CrossRef]
- Zawada, A.M.; Melchior, P.; Erlenkötter, A.; Delinski, D.; Stauss-Grabo, M.; Kennedy, J.P. Polyvinylpyrrolidone in Hemodialysis Membranes: Impact on Platelet Loss during Hemodialysis. Hemodial. Int. 2021, 25, 498–506. [Google Scholar] [CrossRef]
- Ahmadmehrabi, S.; Tang, W.H.W. Hemodialysis-Induced Cardiovascular Disease. Semin. Dial. 2018, 31, 258–267. [Google Scholar] [CrossRef] [PubMed]
- Ritz, E.; Bommer, J. Cardiovascular Problems on Hemodialysis: Current Deficits and Potential Improvement. Clin. J. Am. Soc. Nephrol. 2009, 4, S71–S78. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mavrakanas, T.A.; Charytan, D.M. Cardiovascular Complications in Chronic Dialysis Patients. Curr. Opin. Nephrol. Hypertens. 2016, 25, 536–544. [Google Scholar] [CrossRef]
- Cozzolino, M.; Mangano, M.; Stucchi, A.; Ciceri, P.; Conte, F.; Galassi, A. Cardiovascular Disease in Dialysis Patients. Nephrol. Dial. Transplant. 2018, 33, iii28–iii34. [Google Scholar] [CrossRef] [PubMed]
- Sánchez-Perales, C.; Vázquez-Ruiz de Castroviejo, E.; Segura-Torres, P.; Borrego-Utiel, F.; García-Cortés, M.J.; García-García, F.; Biechy-Baldan, M.M.; Gil-Cunquero, J.M.; Liébana-Cañada, A. Incidence of Acute Myocardial Infarction in the Evolution of Dialysis Patients. Nefrologia 2012, 32, 597–604. [Google Scholar] [CrossRef]
- gbe-bund 2019 Herzinfarkt Mortalität Morbidität und Letalität. Available online: https://www.gbe-bund.de/gbe/ergebnisse.prc_tab?fid=6770&suchstring=&query_id=&sprache=D&fund_typ=TAB&methode=&vt=&verwandte=1&page_ret=0&seite=1&p_lfd_nr=1&p_news=&p_sprachkz=D&p_uid=gast&p_aid=68501311&hlp_nr=2&p_janein=J (accessed on 1 August 2022).
- USRDS 2018 Volume 2: ESRD in the United States. Available online: https://www.niddk.nih.gov/about-niddk/strategic-plans-reports/usrds/prior-data-reports/2018 (accessed on 15 December 2022).
- Kurz, P.; Monier-Faugere, M.C.; Bognar, B.; Werner, E.; Roth, P.; Vlachojannis, J.; Malluche, H.H. Evidence for Abnormal Calcium Homeostasis in Patients with Adynamic Bone Disease. Kidney Int. 1994, 46, 855–861. [Google Scholar] [CrossRef] [Green Version]
- London, G.M.; Marty, C.; Marchais, S.J.; Guerin, A.P.; Metivier, F.; de Vernejoul, M.-C. Arterial Calcifications and Bone Histomorphometry in End-Stage Renal Disease. J. Am. Soc. Nephrol. 2004, 15, 1943–1951. [Google Scholar] [CrossRef]
- Fouque, D.; Kalantar-Zadeh, K.; Kopple, J.; Cano, N.; Chauveau, P.; Cuppari, L.; Franch, H.; Guarnieri, G.; Ikizler, T.A.; Kaysen, G.; et al. A Proposed Nomenclature and Diagnostic Criteria for Protein-Energy Wasting in Acute and Chronic Kidney Disease. Kidney Int. 2008, 73, 391–398. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Giorda, C.B.; Carnà, P.; Salomone, M.; Picariello, R.; Costa, G.; Tartaglino, B.; Gnavi, R. Ten-Year Comparative Analysis of Incidence, Prognosis, and Associated Factors for Dialysis and Renal Transplantation in Type 1 and Type 2 Diabetes versus Non-Diabetes. Acta Diabetol. 2018, 55, 733–740. [Google Scholar] [CrossRef]
- Owen, W.F.; Lew, N.L.; Liu, Y.; Lowrie, E.G.; Lazarus, J.M. The Urea Reduction Ratio and Serum Albumin Concentration as Predictors of Mortality in Patients Undergoing Hemodialysis. N. Engl. J. Med. 1993, 329, 1001–1006. [Google Scholar] [CrossRef] [PubMed]
- Lowrie, E.G.; Lew, N.L. Death Risk in Hemodialysis Patients: The Predictive Value of Commonly Measured Variables and an Evaluation of Death Rate Differences Between Facilities. Am. J. Kidney Dis. 1990, 15, 458–482. [Google Scholar] [CrossRef]
- Tien, K.-J.; Lin, Z.-Z.; Chio, C.-C.; Wang, J.-J.; Chu, C.-C.; Sun, Y.-M.; Kan, W.-C.; Chien, C.-C. Epidemiology and Mortality of New-Onset Diabetes after Dialysis: Taiwan National Cohort Study. Diabetes Care 2013, 36, 3027–3032. [Google Scholar] [CrossRef] [Green Version]
- Bossola, M.; Tazza, L.; Giungi, S.; Luciani, G. Anorexia in Hemodialysis Patients: An Update. Kidney Int. 2006, 70, 417–422. [Google Scholar] [CrossRef] [Green Version]
- Lindsay, R.M.; Spanner, E.; Heidenheim, R.P.; LeFebvre, J.M.; Hodsman, A.; Baird, J.; Allison, M.E. Which Comes First, Kt/V or PCR--Chicken or Egg? Kidney Int. Suppl. 1992, 38, S32–S36. [Google Scholar] [PubMed]
- Davenport, A.; Peters, S.A.E.; Bots, M.L.; Canaud, B.; Grooteman, M.P.C.; Asci, G.; Locatelli, F.; Maduell, F.; Morena, M.; Nubé, M.J.; et al. Higher Convection Volume Exchange with Online Hemodiafiltration Is Associated with Survival Advantage for Dialysis Patients: The Effect of Adjustment for Body Size. Kidney Int. 2016, 89, 193–199. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nube, M.J. Why Is High Volume Online Post-dilution Hemodiafiltration Associated with Improved Survival? In Hemodiafiltration: Theory, Technology and Clinical Practice; Springer: Cham, Switzerland, 2016; pp. 239–254. [Google Scholar] [CrossRef]
- Canaud, B.; Blankestijn, P.J.; Davenport, A.; Bots, M.L. Reconciling and Closing the Loop Between Evidence-Based and Practice-Based Medicine: The Case for Hemodiafiltration. Am. J. Kidney Dis. 2016, 68, 176–179. [Google Scholar] [CrossRef] [Green Version]
- Daugirdas, J.T. Lower Cardiovascular Mortality with High-Volume Hemodiafiltration: A Cool Effect? Nephrol. Dial. Transplant. 2016, 31, 853–856. [Google Scholar] [CrossRef] [Green Version]
- Lin, C.-L.; Huang, C.-C.; Yu, C.-C.; Yang, H.-Y.; Chuang, F.-R.; Yang, C.-W. Reduction of Advanced Glycation End Product Levels by On-Line Hemodiafiltration in Long-Term Hemodialysis Patients. Am. J. Kidney Dis. 2003, 42, 524–531. [Google Scholar] [CrossRef]
- Maduell, F.; Navarro, V.; Cruz, M.C.; Torregrosa, E.; Garcia, D.; Simon, V.; Ferrero, J.A. Osteocalcin and Myoglobin Removal in On-Line Hemodiafiltration versus Low- and High-Flux Hemodialysis. Am. J. Kidney Dis. 2002, 40, 582–589. [Google Scholar] [CrossRef] [PubMed]
- Mandolfo, S.; Borlandelli, S.; Imbasciati, E. Leptin and Beta2-Microglobulin Kinetics with Three Different Dialysis Modalities. Int. J. Artif. Organs 2006, 29, 949–955. [Google Scholar] [CrossRef] [PubMed]
- Potier, J.; Queffeulou, G.; Bouet, J. Are All Dialyzers Compatible with the Convective Volumes Suggested for Postdilution Online Hemodiafiltration? Int. J. Artif. Organs 2016, 39, 460–470. [Google Scholar] [CrossRef] [PubMed]
- Dellepiane, S.; Marengo, M.; D’Arezzo, M.; Donati, G.; Fabbrini, P.; Lacquaniti, A.; Ronco, C.; Cantaluppi, V. The Next Evolution of HemoDialysis EXpanded: From a Delphi Questionnaire-Based Approach to the Real Life of Italian Dialysis Units. Blood Purif. 2022, 51, 943–952. [Google Scholar] [CrossRef]
- Maduell, F.; Broseta, J.J. Hemodiafiltration (HDF) versus Expanded Hemodialysis (HDx). Semin. Dial. 2022, 35, 436–439. [Google Scholar] [CrossRef]
- Maduell, F.; Broseta, J.J.; Rodas, L.; Montagud-Marrahi, E.; Rodriguez-Espinosa, D.; Hermida, E.; Arias-Guillén, M.; Fontseré, N.; Vera, M.; Gómez, M.; et al. Comparison of Solute Removal Properties Between High-Efficient Dialysis Modalities in Low Blood Flow Rate. Ther. Apher. Dial. 2020, 24, 387–392. [Google Scholar] [CrossRef] [PubMed]
- Maduell, F.; Broseta, J.J.; Gómez, M.; Racionero, P.; Montagud-Marrahi, E.; Rodas, L.; Arias-Guillén, M.; Fontseré, N.; Vera, M.; Rico, N. Determining Factors for Hemodiafiltration to Equal or Exceed the Performance of Expanded Hemodialysis. Artif. Organs 2020, 44, E448–E458. [Google Scholar] [CrossRef] [PubMed]
- Kim, T.H.; Kim, S.-H.; Kim, T.Y.; Park, H.Y.; Jung, K.S.; Lee, M.H.; Jhee, J.H.; Lee, J.E.; Choi, H.Y.; Park, H.C. Removal of Large Middle Molecules via Haemodialysis with Medium Cut-off Membranes at Lower Blood Flow Rates: An Observational Prospective Study. BMC Nephrol. 2019, 21, 2. [Google Scholar] [CrossRef]
- Cuvelier, C.; Tintillier, M.; Migali, G.; Van Ende, C.; Pochet, J.-M. Albumin Losses during Hemodiafiltration: All Dialyzers Are Not Created Equal—A Case Report. BMC Nephrol. 2019, 20, 392. [Google Scholar] [CrossRef] [Green Version]
- Lee, Y.; Jang, M.-J.; Jeon, J.; Lee, J.E.; Huh, W.; Choi, B.S.; Park, C.W.; Chin, H.J.; Kang, C.L.; Kim, D.K.; et al. Cardiovascular Risk Comparison between Expanded Hemodialysis Using Theranova and Online Hemodiafiltration (CARTOON): A Multicenter Randomized Controlled Trial. Sci. Rep. 2021, 11, 10807. [Google Scholar] [CrossRef]
- Mitchell, C.R.; Hornig, C.; Canaud, B. Systematic Review to Compare the Outcomes Associated with the Modalities of Expanded Hemodialysis (HDx) versus High-flux Hemodialysis and/or Hemodiafiltration (HDF) in Patients with End-stage Kidney Disease (ESKD). Semin. Dial. 2022, sdi.13130. [Google Scholar] [CrossRef]
- Moon, S.J.; Lee, J.E.; Kim, J.-K.; Yoon, S.Y.; Kang, S.W.; Choi, K.H.; Ha, S.K.; Park, H.-C. The Relationship Between Hemodialysis Modality and Insulin Resistance in Non-Diabetic Hemodialysis Patients. Blood Purif. 2015, 39, 224–229. [Google Scholar] [CrossRef]
- Stinghen, A.E.M.; Massy, Z.A.; Vlassara, H.; Striker, G.E.; Boullier, A. Uremic Toxicity of Advanced Glycation End Products in CKD. J. Am. Soc. Nephrol. 2016, 27, 354–370. [Google Scholar] [CrossRef] [Green Version]
- Imani, F.; Horii, Y.; Suthanthiran, M.; Skolnik, E.Y.; Makita, Z.; Sharma, V.; Sehajpal, P.; Vlassara, H. Advanced Glycosylation Endproduct-Specific Receptors on Human and Rat T-Lymphocytes Mediate Synthesis of Interferon Gamma: Role in Tissue Remodeling. J. Exp. Med. 1993, 178, 2165–2172. [Google Scholar] [CrossRef] [Green Version]
- Glorieux, G.; Helling, R.; Henle, T.; Brunet, P.; Deppisch, R.; Lameire, N.; Vanholder, R. In Vitro Evidence for Immune Activating Effect of Specific AGE Structures Retained in Uremia. Kidney Int. 2004, 66, 1873–1880. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- den Hoedt, C.H.; Bots, M.L.; Grooteman, M.P.C.; van der Weerd, N.C.; Mazairac, A.H.A.; Penne, E.L.; Levesque, R.; ter Wee, P.M.; Nubé, M.J.; Blankestijn, P.J.; et al. Online Hemodiafiltration Reduces Systemic Inflammation Compared to Low-Flux Hemodialysis. Kidney Int. 2014, 86, 423–432. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kempkes-Koch, M.; Stauss-Grabo, M.; Erlenkötter, A.; Rauber, L.; Kennedy, J.; Gauly, A.; Schmidt-Gürtler, H. MO387 Clinical Performance, Hemocompatibility and Safety of a New Dialyzer with a Modified Polysulfone Membrane. Nephrol. Dial. Transplant. 2021, 36, gfab082.0041. [Google Scholar] [CrossRef]
- Vanommeslaeghe, F.; Josipovic, I.; Boone, M.; Van Biesen, W.; Eloot, S. Impact of Intradialytic Fiber Clotting on Dialyzer Extraction and Solute Removal: A Randomized Cross-over Study. Sci. Rep. 2022, 12, 5717. [Google Scholar] [CrossRef]
- Penne, E.L.; Blankestijn, P.J.; Bots, M.L.; van den Dorpel, M.A.; Grooteman, M.P.; Nubé, M.J.; van der Tweel, I.; Ter Wee, P.M. The CONTRAST study group Effect of Increased Convective Clearance by On-Line Hemodiafiltration on All Cause and Cardiovascular Mortality in Chronic Hemodialysis Patients—The Dutch CONvective TRAnsport STudy (CONTRAST): Rationale and Design of a Randomised Controlled Trial [ISRCTN38365125]. Curr. Control. Trials Cardiovasc. Med. 2005, 6, 8. [Google Scholar] [CrossRef] [Green Version]
- Canaud, B.; Jausson, I.; Cristol, J. Clinical Tolerance of Online HDF and Impact on Morbidity and Cardiovascular Risk Factors in ESRD Patients of 65 and More Years Old. 2004. Project supported by a French National Grant from Health Ministry (PHRC national). 2004; manuscript in preparation to be submitted. [Google Scholar]
- Morena, M.; Jaussent, A.; Chalabi, L.; Leray-Moragues, H.; Chenine, L.; Debure, A.; Thibaudin, D.; Azzouz, L.; Patrier, L.; Maurice, F.; et al. Treatment Tolerance and Patient-Reported Outcomes Favor Online Hemodiafiltration Compared to High-Flux Hemodialysis in the Elderly. Kidney Int. 2017, 91, 1495–1509. [Google Scholar] [CrossRef]
- Couchoud, C.; Stengel, B.; Landais, P.; Aldigier, J.-C.; de Cornelissen, F.; Dabot, C.; Maheut, H.; Joyeux, V.; Kessler, M.; Labeeuw, M.; et al. The Renal Epidemiology and Information Network (REIN): A New Registry for End-Stage Renal Disease in France. Nephrol. Dial. Transplant. 2006, 21, 411–418. [Google Scholar] [CrossRef] [Green Version]
- Mercadal, L.; Franck, J.-E.; Metzger, M.; Urena Torres, P.; de Cornelissen, F.; Edet, S.; Béchade, C.; Vigneau, C.; Drüeke, T.; Jacquelinet, C.; et al. Hemodiafiltration Versus Hemodialysis and Survival in Patients With ESRD: The French Renal Epidemiology and Information Network (REIN) Registry. Am. J. Kidney Dis. 2016, 68, 247–255. [Google Scholar] [CrossRef]
- Locatelli, F.; Karaboyas, A.; Pisoni, R.L.; Robinson, B.M.; Fort, J.; Vanholder, R.; Rayner, H.C.; Kleophas, W.; Jacobson, S.H.; Combe, C.; et al. Mortality Risk in Patients on Hemodiafiltration versus Hemodialysis: A “real-World” Comparison from the DOPPS. Nephrol. Dial. Transplant. 2018, 33, 683–689. [Google Scholar] [CrossRef] [Green Version]
- Nubé, M.J.; Peters, S.A.E.; Blankestijn, P.J.; Canaud, B.; Davenport, A.; Grooteman, M.P.C.; Asci, G.; Locatelli, F.; Maduell, F.; Morena, M.; et al. Mortality Reduction by Post-Dilution Online-Haemodiafiltration: A Cause-Specific Analysis. Nephrol. Dial. Transplant. 2017, 32, 548–555. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Blankestijn, P.J.; Grooteman, M.P.; Nube, M.J.; Bots, M.L. Clinical Evidence on Haemodiafiltration. Nephrol. Dial. Transplant. 2018, 33, iii53–iii58. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Locatelli, F.; Altieri, P.; Andrulli, S.; Bolasco, P.; Sau, G.; Pedrini, L.A.; Basile, C.; David, S.; Feriani, M.; Montagna, G.; et al. Hemofiltration and Hemodiafiltration Reduce Intradialytic Hypotension in ESRD. J. Am. Soc. Nephrol. 2010, 21, 1798–1807. [Google Scholar] [CrossRef] [Green Version]
- Donauer, J.; Schweiger, C.; Rumberger, B.; Krumme, B.; Böhler, J. Reduction of Hypotensive Side Effects during Online-Haemodiafiltration and Low Temperature Haemodialysis. Nephrol. Dial. Transplant. 2003, 18, 1616–1622. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sande, F.M.V.D.; Kooman, J.P.; Konings, C.J.; Leunissen, K.M.L. Thermal Effects and Blood Pressure Response during Postdilution Hemodiafiltration and Hemodialysis: The Effect of Amount of Replacement Fluid and Dialysate Temperature. J. Am. Soc. Nephrol. 2001, 12, 1916–1920. [Google Scholar] [CrossRef]
- Baldamus, C.A.; Ernst, W.; Fassbinder, W.; Koch, K.M. Differing Haemodynamic Stability Due to Differing Sympathetic Response: Comparison of Ultrafiltration, Haemodialysis and Haemofiltration. Proc. Eur. Dial. Transpl. Assoc. Eur. Dial. Transpl. Assoc. 1980, 17, 205–212. [Google Scholar]
- Baldamus, C.A.; Ernst, W.; Lysaght, M.J.; Shaldon, S.; Koch, K.M. Hemodynamics in Hemofiltration. Int. J. Artif. Organs 1983, 6, 27–31. [Google Scholar]
- Rodriguez, A.; Morena, M.; Bargnoux, A.-S.; Chenine, L.; Leray-Moragues, H.; Cristol, J.P.; Canaud, B. Quantitative Assessment of Sodium Mass Removal Using Ionic Dialysance and Sodium Gradient as a Proxy Tool: Comparison of High-Flux Hemodialysis versus Online Hemodiafiltration. Artif. Organs 2021, 45, E280–E292. [Google Scholar] [CrossRef]
- Czifra, A.; Páll, A.; Kulcsár, J.; Barta, K.; Kertész, A.; Paragh, G.; Lőrincz, I.; Jenei, Z.; Agarwal, A.; Zarjou, A.; et al. Hemodialysis and Hemodiafiltration Differently Modulate Left Ventricular Diastolic Function. BMC Nephrol. 2013, 14, 76. [Google Scholar] [CrossRef] [Green Version]
- La Milia, V.; Ravasi, C.; Carfagna, F.; Alberghini, E.; Baragetti, I.; Buzzi, L.; Ferrario, F.; Furiani, S.; Barbone, G.S.; Pontoriero, G. Sodium Removal and Plasma Tonicity Balance Are Not Different in Hemodialysis and Hemodiafiltration Using High-Flux Membranes. J. Nephrol. 2019, 32, 461–469. [Google Scholar] [CrossRef] [PubMed]
- Carracedo, J.; Merino, A.; Nogueras, S.; Carretero, D.; Berdud, I.; Ramírez, R.; Tetta, C.; Rodríguez, M.; Martín-Malo, A.; Aljama, P. On-Line Hemodiafiltration Reduces the Proinflammatory CD14+CD16+ Monocyte-Derived Dendritic Cells: A Prospective, Crossover Study. J. Am. Soc. Nephrol. 2006, 17, 2315–2321. [Google Scholar] [CrossRef]
- Ağbaş, A.; Canpolat, N.; Çalışkan, S.; Yılmaz, A.; Ekmekçi, H.; Mayes, M.; Aitkenhead, H.; Schaefer, F.; Sever, L.; Shroff, R. Hemodiafiltration Is Associated with Reduced Inflammation, Oxidative Stress and Improved Endothelial Risk Profile Compared to High-Flux Hemodialysis in Children. PLoS ONE 2018, 13, e0198320. [Google Scholar] [CrossRef] [PubMed]
- Filiopoulos, V.; Hadjiyannakos, D.; Metaxaki, P.; Sideris, V.; Takouli, L.; Anogiati, A.; Vlassopoulos, D. Inflammation and Oxidative Stress in Patients on Hemodiafiltration. Am. J. Nephrol. 2008, 28, 949–957. [Google Scholar] [CrossRef]
- Susantitaphong, P.; Siribamrungwong, M.; Jaber, B.L. Convective Therapies versus Low-Flux Hemodialysis for Chronic Kidney Failure: A Meta-Analysis of Randomized Controlled Trials. Nephrol. Dial. Transplant. 2013, 28, 2859–2874. [Google Scholar] [CrossRef] [Green Version]
- Charitaki, E.; Belman, D.; Davenport, A. Treatment with Haemodiafiltration Stabilises Vascular Stiffness (Measured by Aortic Pulse Wave Velocity) Compared to Haemodialysis. Nephron Clin. Pract. 2014, 128, 185–191. [Google Scholar] [CrossRef]
- Ohtake, T.; Oka, M.; Ishioka, K.; Honda, K.; Mochida, Y.; Maesato, K.; Moriya, H.; Hidaka, S.; Kobayashi, S. Cardiovascular Protective Effects of On-Line Hemodiafiltration: Comparison with Conventional Hemodialysis. Ther. Apher. Dial. 2012, 16, 181–188. [Google Scholar] [CrossRef]
- Chan, C.T.; Hanly, P.; Gabor, J.; Picton, P.; Pierratos, A.; Floras, J.S. Impact of Nocturnal Hemodialysis on the Variability of Heart Rate and Duration of Hypoxemia during Sleep. Kidney Int. 2004, 65, 661–665. [Google Scholar] [CrossRef] [Green Version]
- Nistor, I.; Palmer, S.C.; Craig, J.C.; Saglimbene, V.; Vecchio, M.; Covic, A.; Strippoli, G.F.M. Convective versus Diffusive Dialysis Therapies for Chronic Kidney Failure: An Updated Systematic Review of Randomized Controlled Trials. Am. J. Kidney Dis. 2014, 63, 954–967. [Google Scholar] [CrossRef] [Green Version]
- Marcelli, D.; Bayh, I.; Merello, J.I.; Ponce, P.; Heaton, A.; Kircelli, F.; Chazot, C.; Di Benedetto, A.; Marelli, C.; Ladanyi, E.; et al. Dynamics of the Erythropoiesis Stimulating Agent Resistance Index in Incident Hemodiafiltration and High-Flux Hemodialysis Patients. Kidney Int. 2016, 90, 192–202. [Google Scholar] [CrossRef] [PubMed]
- Panichi, V.; Scatena, A.; Rosati, A.; Giusti, R.; Ferro, G.; Malagnino, E.; Capitanini, A.; Piluso, A.; Conti, P.; Bernabini, G.; et al. High-Volume Online Haemodiafiltration Improves Erythropoiesis-Stimulating Agent (ESA) Resistance in Comparison with Low-Flux Bicarbonate Dialysis: Results of the REDERT Study. Nephrol. Dial. Transplant. 2015, 30, 682–689. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Molina, P.; Vizcaíno, B.; Molina, M.D.; Beltrán, S.; González-Moya, M.; Mora, A.; Castro-Alonso, C.; Kanter, J.; Ávila, A.I.; Górriz, J.L.; et al. The Effect of High-Volume Online Haemodiafiltration on Nutritional Status and Body Composition: The ProtEin Stores PrEservaTion (PESET) Study. Nephrol. Dial. Transplant. 2018, 33, 1223–1235. [Google Scholar] [CrossRef] [PubMed]
- Savica, V.; Ciolino, F.; Monardo, P.; Mallamace, A.; Savica, R.; Santoro, D.; Bellinghieri, G. Nutritional Status in Hemodialysis Patients: Options for on-Line Convective Treatment. J. Ren. Nutr. 2006, 16, 237–240. [Google Scholar] [CrossRef] [PubMed]
- Thumfart, J.; Puttkamer, C.V.; Wagner, S.; Querfeld, U.; Müller, D. Hemodiafiltration in a Pediatric Nocturnal Dialysis Program. Pediatr. Nephrol. Berl. Ger. 2014, 29, 1411–1416. [Google Scholar] [CrossRef]
- Pecoits-Filho, R.; Larkin, J.; Poli-de-Figueiredo, C.E.; Cuvello-Neto, A.L.; Barra, A.B.L.; Gonçalves, P.B.; Sheth, S.; Guedes, M.; Han, M.; Calice-Silva, V.; et al. Effect of Hemodiafiltration on Measured Physical Activity: Primary Results of the HDFIT Randomized Controlled Trial. Nephrol. Dial. Transplant. 2021, 36, 1057–1070. [Google Scholar] [CrossRef]
- Karkar, A.; Abdelrahman, M.; Locatelli, F. A Randomized Trial on Health-Related Patient Satisfaction Level with High-Efficiency Online Hemodiafiltration versus High-Flux Dialysis. Blood Purif. 2015, 40, 84–91. [Google Scholar] [CrossRef]
- Hazim, A.; Adarmouch, L.; Eloury, A.; Aasfara, J.; Asly, M.; Slassi, I. Hemodialysis-Related Headache: Still a Challenge in 2020? Effect of Conventional versus Online Hemodiafiltration from a Study in Casablanca, Morocco. Artif. Organs 2021, 45, 602–607. [Google Scholar] [CrossRef]
- Kantartzi, K.; Panagoutsos, S.; Mourvati, E.; Roumeliotis, A.; Leivaditis, K.; Devetzis, V.; Passadakis, P.; Vargemezis, V. Can Dialysis Modality Influence Quality of Life in Chronic Hemodialysis Patients? Low-Flux Hemodialysis versus High-Flux Hemodiafiltration: A Cross-over Study. Ren. Fail. 2013, 35, 216–221. [Google Scholar] [CrossRef]
- Vilar, E.; Fry, A.C.; Wellsted, D.; Tattersall, J.E.; Greenwood, R.N.; Farrington, K. Long-Term Outcomes in Online Hemodiafiltration and High-Flux Hemodialysis: A Comparative Analysis. Clin. J. Am. Soc. Nephrol. 2009, 4, 1944–1953. [Google Scholar] [CrossRef] [Green Version]
- Vilar, E.; Farrington, K. Emerging Importance of Residual Renal Function in End-Stage Renal Failure. Semin. Dial. 2011, 24, 487–494. [Google Scholar] [CrossRef]
- Davenport, A. Dialysis and Patient Factors Which Determine Convective Volume Exchange in Patients Treated by Postdilution Online Hemodiafiltration. Artif. Organs 2016, 40, 1121–1127. [Google Scholar] [CrossRef] [PubMed]
- Canaud, B.; Davenport, A. The Rationale and Clinical Potential of On-line Hemodiafiltration as Renal Replacement Therapy. Semin. Dial. 2022, 35, 380–384. [Google Scholar] [CrossRef] [PubMed]
- Suwabe, T.; Barrera-Flores, F.J.; Rodriguez-Gutierrez, R.; Ubara, Y.; Takaichi, K. Effect of Online Hemodiafiltration Compared with Hemodialysis on Quality of Life in Patients with ESRD: A Systematic Review and Meta-Analysis of Randomized Trials. PLoS ONE 2018, 13, e0205037. [Google Scholar] [CrossRef] [Green Version]
- Cromm, K.; Fischer, K.I. Striking New Path(Way)s-How a Conceptual Model of Patient Outcomes Can Help Us Advance Outcomes That Matter to Patients. Nephrol. Dial. Transplant. 2021, 36, 956–959. [Google Scholar] [CrossRef] [PubMed]
- Blankestijn, P.J.; Fischer, K.I.; Barth, C.; Cromm, K.; Canaud, B.; Davenport, A.; Grobbee, D.E.; Hegbrant, J.; Roes, K.C.; Rose, M.; et al. Benefits and Harms of High-Dose Haemodiafiltration versus High-Flux Haemodialysis: The Comparison of High-Dose Haemodiafiltration with High-Flux Haemodialysis (CONVINCE) Trial Protocol. BMJ Open 2020, 10, e033228. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nistor, I.; Palmer, S.C.; Craig, J.C.; Saglimbene, V.; Vecchio, M.; Covic, A.; Strippoli, G.F.M. Haemodiafiltration, Haemofiltration and Haemodialysis for End-Stage Kidney Disease. Cochrane Database Syst. Rev. 2015, CD006258. [Google Scholar] [CrossRef]


| Reference | Study Name | Number Patients | Countries | Study Design | Comparison | Mortality Endpoints |
|---|---|---|---|---|---|---|
| Grooteman et al., 2012 [15] | CONTRAST | 714 | Netherlands, Canada, Norway | Multicenter randomized controlled clinical trial | Online post-dilution HDF versus low-flux HD | All cause-mortality, Cardiovascular vs. non-cardiovascular mortality |
| Maduell et al., 2013 [12] | ESHOL | 906 | Spain | Multicenter randomized controlled clinical trial | Online post-dilution HDF versus high-flux HD | All cause-mortality, Cardiovascular vs. non-cardiovascular mortality |
| Ok et al., 2013 [14] | Turkish HDF study | 782 | Turkey | Multicenter randomized controlled clinical trial | Online post-dilution HDF versus high-flux HD | All cause-mortality, Cardiovascular vs. non-cardiovascular mortality |
| Canaud et al., 2004 [102] | French HDF study | 391 | France | Multicenter randomized controlled clinical trial | Online HDF versus high-flux HD | All cause-mortality, Cardiovascular vs. non-cardiovascular mortality |
| Endpoint | HR (95% Confidence Interval) | ||
|---|---|---|---|
| Low Volume < 19 L | Mid Volume 19–23 L | High Volume > 23 L | |
| All-cause mortality | 0.83 (0.66–1.03) | 0.93 (0.75–1.16) | 0.78 (0.62–0.98) |
| Cardiovascular mortality | 0.92 (0.65–1.30) | 0.71 (0.41–1.03) | 0.69 (0.47–1.00) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lang, T.; Zawada, A.M.; Theis, L.; Braun, J.; Ottillinger, B.; Kopperschmidt, P.; Gagel, A.; Kotanko, P.; Stauss-Grabo, M.; Kennedy, J.P.; et al. Hemodiafiltration: Technical and Medical Insights. Bioengineering 2023, 10, 145. https://doi.org/10.3390/bioengineering10020145
Lang T, Zawada AM, Theis L, Braun J, Ottillinger B, Kopperschmidt P, Gagel A, Kotanko P, Stauss-Grabo M, Kennedy JP, et al. Hemodiafiltration: Technical and Medical Insights. Bioengineering. 2023; 10(2):145. https://doi.org/10.3390/bioengineering10020145
Chicago/Turabian StyleLang, Thomas, Adam M. Zawada, Lukas Theis, Jennifer Braun, Bertram Ottillinger, Pascal Kopperschmidt, Alfred Gagel, Peter Kotanko, Manuela Stauss-Grabo, James P. Kennedy, and et al. 2023. "Hemodiafiltration: Technical and Medical Insights" Bioengineering 10, no. 2: 145. https://doi.org/10.3390/bioengineering10020145
APA StyleLang, T., Zawada, A. M., Theis, L., Braun, J., Ottillinger, B., Kopperschmidt, P., Gagel, A., Kotanko, P., Stauss-Grabo, M., Kennedy, J. P., & Canaud, B. (2023). Hemodiafiltration: Technical and Medical Insights. Bioengineering, 10(2), 145. https://doi.org/10.3390/bioengineering10020145








