The Evolving Use of Magnets in Surgery: Biomedical Considerations and a Review of Their Current Applications
Abstract
:1. Introduction
| Year | Organ System | Medical Indication | Use of Magnets | Citation |
|---|---|---|---|---|
| 1975 | Esophagus | Esophageal atresia | Intermittent application of electromagnetic field to metal bougies that lengthen atretic esophageal pouches | Hendren and Hale, 1975 [1] |
| 1980 | Vascular | Need for arteriovenous fistula | Intravascular paired ring magnets for side-to-side anastomosis between two blood vessels | Obora et al., 1980 [4] |
| 1981 | Colorectal | Presence of colostomy | Internal–external paired magnetic ring system for colostomy closure | Jansen et al., 1981 [5] |
| 1989 | Urology | Urethral stricture | Intraurethral miniaturized magnets for stricturoplasty | Isakov et al., 1989 [6] |
| 1992 | Small intestine | Small bowel fistula | Intraluminal paired magnets to form compression anastomosis bypassing intestinal fistula | Stepanov et al., 1992 [7] |
| 1993 | Hepatobiliary | Biliary stricture | Paired magnets to form compression anastomosis between proximal common bile duct and stomach or duodenum | Saveliev et al., 1993 [8] |
2. Biomedical Considerations for Magnetic Surgical Devices
3. Core Functions of Magnetic Surgical Devices
3.1. Guidance System
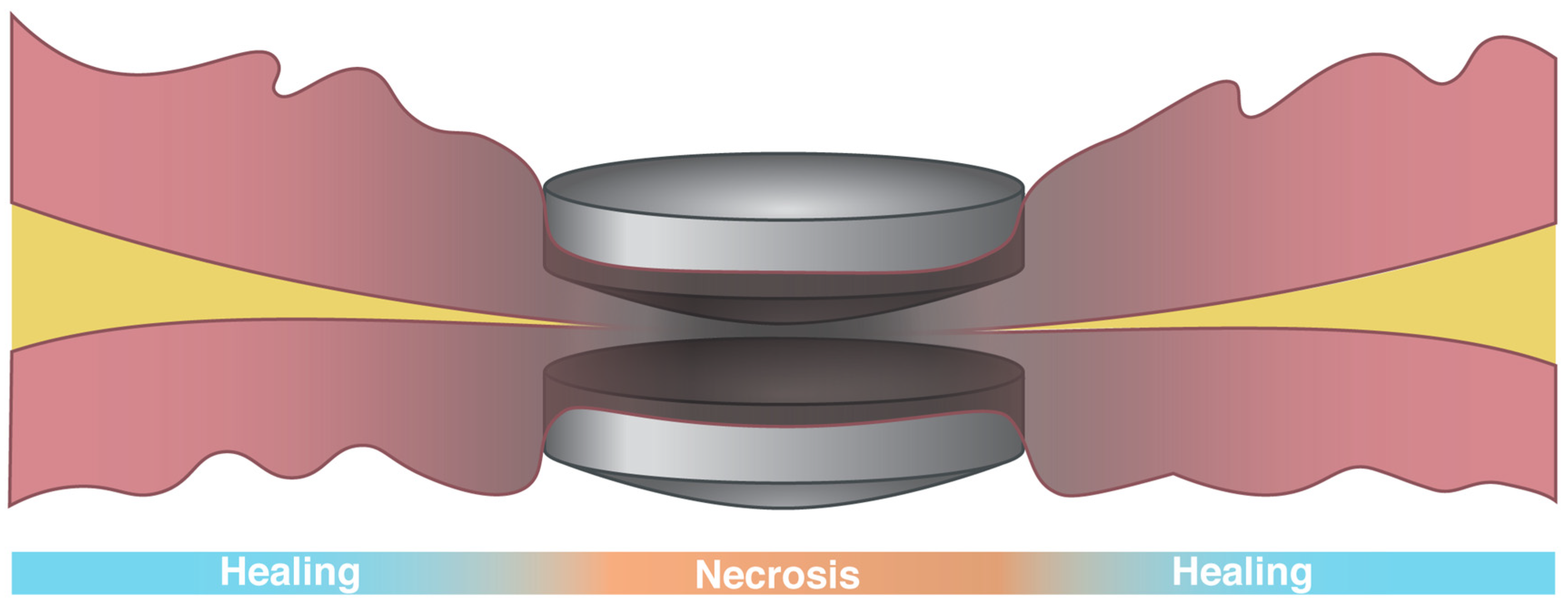
3.2. Magnetic Compression Anastomosis to Create New Connections
- Uretero-ileal anastomoses for urinary diversions in patients with neurogenic bladders [42];
- Colorectal anastomoses of disconnected colons and rectums in children with rectal atresia [41];
- Stricturoplasties, or intraluminal resections of obstructing strictures, to restore GI tract continuity;
- Small bowel non-anastomotic strictures [63];
3.3. Recreating a Physiologic Function
3.4. Use of Internal–External Paired Magnet Systems
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Hendren, W.H.; Hale, J.R. Electromagnetic bougienage to lengthen esophageal segments in congenital esophageal atresia. N. Engl. J. Med. 1975, 293, 428–432. [Google Scholar] [CrossRef] [PubMed]
- Trondsen, E.; Reiertsen, O.; Andersen, O.K.; Kjaersgaard, P. Laparoscopic and open cholecystectomy. A prospective, randomized study. Eur. J. Surg. 1993, 159, 217–221. [Google Scholar] [PubMed]
- Gagner, M. Magnetic Surgery, 1st ed.; Springer: Cham, Switzerland, 2022; p. 254. [Google Scholar] [CrossRef]
- Obora, Y.; Tamaki, N.; Matsumoto, S. Nonsuture microvascular anastomosis using magnet rings. Neurol. Med. Chir. 1980, 20, 497–505. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jansen, A.; Brummelkamp, W.H.; Davies, G.A.; Klopper, P.J.; Keeman, J.N. Clinical applications of magnetic rings in colorectal anastomosis. Surg. Gynecol. Obstet. 1981, 153, 537–545. [Google Scholar] [PubMed]
- Isakov, I.A.S.E.; Erokhin, A.P.; Nikolaev, V.V.; Vasi’lev, G.S. Surgical treatment of urethral strictures in children. Vestn. Khir. Im. II Grek. 1989, 142, 61–66. [Google Scholar] [PubMed]
- Stepanov, E.A.V.e.G.; Sharipov, N.A.; Rudakov, S.S.; Romakhin, I.A. Use of permanent magnets in digestive tract surgery in children. Vestn. Akad. Med. Nauk. SSSR 1992, 9, 6–11. [Google Scholar]
- Saveliev, V.S.; Avaliani, M.V.; Bashirov, A.D. Endoscopic magnetic cholecystodigestive anastomoses: Personal technique for palliative treatment of distal bile duct obstruction. J. Laparoendosc. Surg. 1993, 3, 99–112. [Google Scholar]
- Robinson, A.L. Powerful New Magnet Material Found: Several groups in Japan and the United States independently hit upon the same iron-based compound, which is already going to market. Science 1984, 223, 920–922. [Google Scholar] [CrossRef] [PubMed]
- Horikawa, T.; Yamazaki, M.; Matsuura, M.; Sugimoto, S. Recent progress in the development of high-performance bonded magnets using rare earth-Fe compounds. Sci. Technol. Adv. Mater. 2021, 22, 729–747. [Google Scholar] [CrossRef]
- Castle, E.; Sheridan, R.; Zhou, W.; Grasso, S.; Walton, A.; Reece, M.J. High coercivity, anisotropic, heavy rare earth-free Nd-Fe-B by Flash Spark Plasma Sintering. Sci. Rep. 2017, 7, 11134. [Google Scholar] [CrossRef] [Green Version]
- Kimura, T.; Goto, T.; Shintani, H.; Ishizaka, K.; Arima, T.; Tokura, Y. Magnetic control of ferroelectric polarization. Nature 2003, 426, 55–58. [Google Scholar] [CrossRef] [PubMed]
- Rim, K.T.; Koo, K.H.; Park, J.S. Toxicological evaluations of rare earths and their health impacts to workers: A literature review. Saf. Health Work 2013, 4, 12–26. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Donohue, V.E.; McDonald, F.; Evans, R. In vitro cytotoxicity testing of neodymium-iron-boron magnets. J. Appl. Biomater. 1995, 6, 69–74. [Google Scholar] [CrossRef] [PubMed]
- Croat, J.J. Current status and future outlook for bonded neodymium permanent magnets (invited). J. Appl. Phys. 1997, 81, 4804–4809. [Google Scholar] [CrossRef]
- Williams, D.F. On the mechanisms of biocompatibility. Biomaterials 2008, 29, 2941–2953. [Google Scholar] [CrossRef]
- Markides, H.; Rotherham, M.; El Haj, A.J. Biocompatibility and Toxicity of Magnetic Nanoparticles in Regenerative Medicine. J. Nanomater. 2012, 2012, 614094. [Google Scholar] [CrossRef] [Green Version]
- Geetha, M.; Singh, A.K.; Asokamani, R.; Gogia, A.K. Ti based biomaterials, the ultimate choice for orthopaedic implants—A review. Prog. Mater. Sci. 2009, 54, 397–425. [Google Scholar] [CrossRef]
- Martin, E.T.; Coman, J.A.; Shellock, F.G.; Pulling, C.C.; Fair, R.; Jenkins, K. Magnetic resonance imaging and cardiac pacemaker safety at 1.5-Tesla. J. Am. Coll. Cardiol. 2004, 43, 1315–1324. [Google Scholar] [CrossRef] [Green Version]
- International Commission on Non-Ionizing Radiation, P. Guidelines on limits of exposure to static magnetic fields. Health Phys. 2009, 96, 504–514. [Google Scholar] [CrossRef]
- Ryf, S.; Wolber, T.; Duru, F.; Luechinger, R. Interference of neodymium magnets with cardiac pacemakers and implantable cardioverter-defibrillators: An in vitro study. Technol. Health Care 2008, 16, 13–18. [Google Scholar] [CrossRef]
- Zamanian, A.; Hardiman, C.J. Electromagnetic radiation and human health: A review of sources and effects. High Freq. Electron. 2005, 4, 16–26. [Google Scholar]
- Timsit, J.F.; Rupp, M.; Bouza, E.; Chopra, V.; Kärpänen, T.; Laupland, K.; Lisboa, T.; Mermel, L.; Mimoz, O.; Parienti, J.J.; et al. A state of the art review on optimal practices to prevent, recognize, and manage complications associated with intravascular devices in the critically ill. Intensive Care Med. 2018, 44, 742–759. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hodges, N.L.; Denny, S.A.; Smith, G.A. Rare-Earth Magnet Ingestion-Related Injuries in the Pediatric Population: A Review. Am. J. Lifestyle Med. 2017, 11, 259–263. [Google Scholar] [CrossRef] [PubMed]
- Harrison, M.R.; Estefan-Ventura, D.; Fechter, R.; Moran, A.M., Jr.; Christensen, D. Magnetic Mini-Mover Procedure for pectus excavatum: I. Development, design, and simulations for feasibility and safety. J. Pediatr. Surg. 2007, 42, 81–85; discussion 85–86. [Google Scholar] [CrossRef] [PubMed]
- Mathus-Vliegen, E.M.; Duflou, A.; Spanier, M.B.; Fockens, P. Nasoenteral feeding tube placement by nurses using an electromagnetic guidance system (with video). Gastrointest. Endosc. 2010, 71, 728–736. [Google Scholar] [CrossRef] [PubMed]
- Smithard, D.; Barrett, N.A.; Hargroves, D.; Elliot, S. Electromagnetic Sensor-Guided Enteral Access Systems: A Literature Review. Dysphagia 2015, 30, 275–285. [Google Scholar] [CrossRef] [Green Version]
- McCutcheon, K.P.; Whittet, W.L.; Kirsten, J.L.; Fuchs, J.L. Feeding Tube Insertion and Placement Confirmation Using Electromagnetic Guidance: A Team Review. JPEN J. Parenter. Enter. Nutr. 2018, 42, 247–254. [Google Scholar] [CrossRef]
- Tomaszewski, K.J.; Ferko, N.; Hollmann, S.S.; Eng, S.C.; Richard, H.M.; Rowe, L.; Sproule, S. Time and resources of peripherally inserted central catheter insertion procedures: A comparison between blind insertion/chest X-ray and a real time tip navigation and confirmation system. Clin. Outcomes Res. 2017, 9, 115–125. [Google Scholar] [CrossRef] [Green Version]
- Mack, V.; Nißler, D.; Kasikci, D.; Malouhi, A.; Aschenbach, R.; Teichgräber, U. Magnetic Tracking and Electrocardiography-Guided Tip Confirmation System Versus Fluoroscopy for Placement of Peripherally Inserted Central Catheters: A Randomized, Noninferiority Comparison. Cardiovasc. Intervent. Radiol. 2020, 43, 1891–1897. [Google Scholar] [CrossRef]
- Sone, M. Image Guidance for PICC Insertion: Commentary to “Magnetic Tracking and Electrocardiography-Guided Tip Confirmation System Versus Fluoroscopy for Placement of Peripherally Inserted Central Catheters: A Randomized, Noninferiority Comparison”. Cardiovasc. Intervent. Radiol. 2020, 43, 1898–1899. [Google Scholar] [CrossRef] [PubMed]
- Lok, C.E.; Rajan, D.K.; Clement, J.; Kiaii, M.; Sidhu, R.; Thomson, K.; Buldo, G.; Dipchand, C.; Moist, L.; Sasal, J.; et al. Endovascular Proximal Forearm Arteriovenous Fistula for Hemodialysis Access: Results of the Prospective, Multicenter Novel Endovascular Access Trial (NEAT). Am. J. Kidney Dis. 2017, 70, 486–497. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Xu, Z.F.; Li, Z.J.; Sun, Y.L.; Zheng, Y.; Shi, H.Y.; Zhen, Y.N.; Wang, B.; Niu, H.X.; Wang, R.G. A novel spherical magnetic compression device for colorectal anastomosis in a Swine model. J. Laparoendosc. Adv. Surg. Tech. A 2015, 25, 323–329. [Google Scholar] [CrossRef] [PubMed]
- Cope, C. Creation of compression gastroenterostomy by means of the oral, percutaneous, or surgical introduction of magnets: Feasibility study in swine. J. Vasc. Interv. Radiol. 1995, 6, 539–545. [Google Scholar] [CrossRef] [PubMed]
- Chopita, N.; Vaillaverde, A.; Cope, C.; Bernedo, A.; Martinez, H.; Landoni, N.; Jmelnitzky, A.; Burgos, H. Endoscopic gastroenteric anastomosis using magnets. Endoscopy 2005, 37, 313–317. [Google Scholar] [CrossRef] [PubMed]
- Jamshidi, R.; Stephenson, J.T.; Clay, J.G.; Pichakron, K.O.; Harrison, M.R. Magnamosis: Magnetic compression anastomosis with comparison to suture and staple techniques. J. Pediatr. Surg. 2009, 44, 222–228. [Google Scholar] [CrossRef] [PubMed]
- Myers, C.; Yellen, B.; Evans, J.; DeMaria, E.; Pryor, A. Using external magnet guidance and endoscopically placed magnets to create suture-free gastro-enteral anastomoses. Surg. Endosc. 2010, 24, 1104–1109. [Google Scholar] [CrossRef] [PubMed]
- Pichakron, K.O.; Jelin, E.B.; Hirose, S.; Curran, P.F.; Jamshidi, R.; Stephenson, J.T.; Fechter, R.; Strange, M.; Harrison, M.R. Magnamosis II: Magnetic compression anastomosis for minimally invasive gastrojejunostomy and jejunojejunostomy. J. Am. Coll. Surg. 2011, 212, 42–49. [Google Scholar] [CrossRef] [PubMed]
- Gonzales, K.D.; Douglas, G.; Pichakron, K.O.; Kwiat, D.A.; Gallardo, S.G.; Encinas, J.L.; Hirose, S.; Harrison, M.R. Magnamosis III: Delivery of a magnetic compression anastomosis device using minimally invasive endoscopic techniques. J. Pediatr. Surg. 2012, 47, 1291–1295. [Google Scholar] [CrossRef]
- Wall, J.; Diana, M.; Leroy, J.; Deruijter, V.; Gonzales, K.D.; Lindner, V.; Harrison, M.; Marescaux, J. MAGNAMOSIS IV: Magnetic compression anastomosis for minimally invasive colorectal surgery. Endoscopy 2013, 45, 643–648. [Google Scholar] [CrossRef] [PubMed]
- Russell, K.W.; Rollins, M.D.; Feola, G.P.; Scaife, E.R. Magnamosis: A novel technique for the management of rectal atresia. BMJ Case Rep. 2014, 2014, bcr2013201330. [Google Scholar] [CrossRef]
- Graves, C.E.; Co, C.; Hsi, R.S.; Kwiat, D.; Imamura-Ching, J.; Harrison, M.R.; Stoller, M.L. Magnetic Compression Anastomosis (Magnamosis): First-In-Human Trial. J. Am. Coll. Surg. 2017, 225, 676–681 e671. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ryou, M.; Aihara, H.; Thompson, C.C. Minimally invasive entero-enteral dual-path bypass using self-assembling magnets. Surg. Endosc. 2016, 30, 4533–4538. [Google Scholar] [CrossRef] [PubMed]
- Machytka, E.; Buzga, M.; Zonca, P.; Lautz, D.B.; Ryou, M.; Simonson, D.C.; Thompson, C.C. Partial jejunal diversion using an incisionless magnetic anastomosis system: 1-year interim results in patients with obesity and diabetes. Gastrointest. Endosc. 2017, 86, 904–912. [Google Scholar] [CrossRef] [PubMed]
- Schlottmann, F.; Ryou, M.; Lautz, D.; Thompson, C.C.; Buxhoeveden, R. Sutureless Duodeno-Ileal Anastomosis with Self-Assembling Magnets: Safety and Feasibility of a Novel Metabolic Procedure. Obes. Surg. 2021, 31, 4195–4202. [Google Scholar] [CrossRef] [PubMed]
- Gumustop, D.; Seddon, D.; Gumustop, B.; Wang, J. A comparison of anastomosis strength between sutures, staples, and self-forming magnets. iGIE 2022, 1, 11–14. [Google Scholar] [CrossRef]
- Ore, A.S.; Althoff, A.; Kull, D.R.; Baldwin, T.J.; Van Eps, J.L.; Messaris, E. Comparative early histologic healing quality of magnetic versus stapled small bowel anastomosis. Surgery 2022, 17, 1060–1065. [Google Scholar] [CrossRef] [PubMed]
- Ore, A.S.; Askenasy, E.; Ryou, M.; Baldwin, T.; Thompson, C.C.; Messaris, E. Evaluation of sutureless anastomosis after ileostomy takedown using the self-forming magnet anastomosis system in a porcine model. Surg. Endosc. 2022, 36, 7664–7672. [Google Scholar] [CrossRef]
- Zaritzky, M.; Ben, R.; Zylberg, G.I.; Yampolsky, B. Magnetic compression anastomosis as a nonsurgical treatment for esophageal atresia. Pediatr. Radiol. 2009, 39, 945–949. [Google Scholar] [CrossRef]
- Zaritzky, M.; Ben, R.; Johnston, K. Magnetic gastrointestinal anastomosis in pediatric patients. J. Pediatr. Surg. 2014, 49, 1131–1137. [Google Scholar] [CrossRef]
- Dorman, R.M.; Vali, K.; Harmon, C.M.; Zaritzky, M.; Bass, K.D. Repair of esophageal atresia with proximal fistula using endoscopic magnetic compression anastomosis (magnamosis) after staged lengthening. Pediatr. Surg. Int. 2016, 32, 525–528. [Google Scholar] [CrossRef] [PubMed]
- Slater, B.J.; Borobia, P.; Lovvorn, H.N.; Raees, M.A.; Bass, K.D.; Almond, S.; Hoover, J.D.; Kumar, T.; Zaritzky, M. Use of Magnets as a Minimally Invasive Approach for Anastomosis in Esophageal Atresia: Long-Term Outcomes. J. Laparoendosc. Adv. Surg. Tech. A 2019, 29, 1202–1206. [Google Scholar] [CrossRef]
- Muensterer, O.J.; Sterlin, A.; Oetzmann von Sochaczewski, C.; Lindner, A.; Heimann, A.; Balus, A.; Dickmann, J.; Nuber, M.; Patel, V.H.; Manfredi, M.A.; et al. An experimental study on magnetic esophageal compression anastomosis in piglets. J. Pediatr. Surg. 2020, 55, 425–432. [Google Scholar] [CrossRef] [PubMed]
- Wolfe, E.; Zidane, M.; Hancock, B.J.; Lum Min, S.A.; Zaritzky, M.; Keijzer, R. Magnamosis for esophageal atresia is associated with anastomotic strictures requiring an increased number of dilatations. J. Pediatr. Surg. 2020, 55, 821–823. [Google Scholar] [CrossRef] [PubMed]
- Muensterer, O.J.; Evans, L.L.; Sterlin, A.; Sahlabadi, M.; Aribindi, V.; Lindner, A.; Konig, T.; Harrison, M.R. Novel Device for Endoluminal Esophageal Atresia Repair: First-in-Human Experience. Pediatrics 2021, 148, e2020049627. [Google Scholar] [CrossRef] [PubMed]
- Evans, L.L.; Chen, C.S.; Muensterer, O.J.; Sahlabadi, M.; Lovvorn, H.N.; Novotny, N.M.; Upperman, J.S.; Martinez, J.A.; Bruzoni, M.; Dunn, J.C.Y.; et al. The novel application of an emerging device for salvage of primary repair in high-risk complex esophageal atresia. J. Pediatr. Surg. 2022, 57, 810–818. [Google Scholar] [CrossRef] [PubMed]
- Mimuro, A.; Tsuchida, A.; Yamanouchi, E.; Itoi, T.; Ozawa, T.; Ikeda, T.; Nakamura, R.; Koyanagi, Y.; Nakamura, K. A novel technique of magnetic compression anastomosis for severe biliary stenosis. Gastrointest. Endosc. 2003, 58, 283–287. [Google Scholar] [CrossRef]
- Muraoka, N.; Uematsu, H.; Yamanouchi, E.; Kinoshita, K.; Takeda, T.; Ihara, N.; Matsunami, H.; Itoh, H. Yamanouchi magnetic compression anastomosis for bilioenteric anastomotic stricture after living-donor liver transplantation. J. Vasc. Interv. Radiol. 2005, 16, 1263–1267. [Google Scholar] [CrossRef] [PubMed]
- Matsuno, N.; Uchiyama, M.; Nakamura, Y.; Iwamoto, H.; Hama, K.; Ashizawa, T.; Nagao, T.; Yamanouchi, E. A nonsuture anastomosis using magnetic compression for biliary stricture after living donor liver transplantation. Hepatogastroenterology 2009, 56, 47–49. [Google Scholar]
- Jang, S.I.; Cho, J.H.; Lee, D.K. Magnetic Compression Anastomosis for the Treatment of Post-Transplant Biliary Stricture. Clin. Endosc. 2020, 53, 266–275. [Google Scholar] [CrossRef]
- Takamizawa, S.; Yamanouchi, E.; Muraji, T.; Nishijima, E.; Satoh, S.; Tsugawa, J. MCRA of an anastomotic stenosis after esophagoesophagostomy for long gap esophageal atresia: A case report. J. Pediatr. Surg. 2007, 42, 769–772. [Google Scholar] [CrossRef]
- Woo, R.; Wong, C.M.; Trimble, Z.; Puapong, D.; Koehler, S.; Miller, S.; Johnson, S. Magnetic Compression Stricturoplasty For Treatment of Refractory Esophageal Strictures in Children: Technique and Lessons Learned. Surg. Innov. 2017, 24, 432–439. [Google Scholar] [CrossRef] [PubMed]
- Kamada, T.; Ohdaira, H.; Takeuchi, H.; Takahashi, J.; Marukuchi, R.; Suzuki, N.; Narihiro, S.; Hoshimoto, S.; Yoshida, M.; Yamanouchi, E.; et al. Magnetic compression anastomosis for non-anastomotic stenosis of the proximal jejunum after total gastrectomy with Roux-en-Y reconstruction: A case report. Surg. Case Rep. 2020, 6, 167. [Google Scholar] [CrossRef] [PubMed]
- Isozaki, T.; Murakami, K.; Yamanouchi, E.; Uesato, M.; Toyozumi, T.; Koide, Y.; Tsukamoto, S.; Sakata, H.; Hayano, K.; Kano, M.; et al. Magnetic compression anastomosis is effective in treating stenosis after esophageal cancer surgery: A case report. Surg. Case Rep. 2020, 6, 213. [Google Scholar] [CrossRef] [PubMed]
- Liu, H.; Yang, Z.; Lu, W.; Chen, Z.; Chen, L.; Han, S.; Wu, X.; Cai, T.; Cai, Y. Chemokines and chemokine receptors: A new strategy for breast cancer therapy. Cancer Med. 2020, 9, 3786–3799. [Google Scholar] [CrossRef] [Green Version]
- Kılıç, A.; Şişik, A. A novel method for treatment of persistent colorectal anastomotic strictures: Magnetic compression strictureplasty. J. Surg. Med. 2020, 4, 331–333. [Google Scholar] [CrossRef]
- Liu, S.; Fang, Y.; Lv, Y.; Zhao, J.; Luo, R.; Luo, R.; Cheng, J.; Yang, H.; Zhang, A.; Shen, Y.; et al. Magnetic compression stricturoplasty in patients with severe stricture after simultaneous esophageal atresia and duodenal obstruction repair: A case report. Exp. Ther. Med. 2022, 23, 93. [Google Scholar] [CrossRef] [PubMed]
- Falk, V.; Walther, T.; Stein, H.; Jacobs, S.; Walther, C.; Rastan, A.; Wimmer-Greinecker, G.; Mohr, F.W. Facilitated endoscopic beating heart coronary artery bypass grafting using a magnetic coupling device. J. Thorac. Cardiovasc. Surg. 2003, 126, 1575–1579. [Google Scholar] [CrossRef] [Green Version]
- Klima, U.; Falk, V.; Maringka, M.; Bargenda, S.; Badack, S.; Moritz, A.; Mohr, F.; Haverich, A.; Wimmer-Greinecker, G. Magnetic vascular coupling for distal anastomosis in coronary artery bypass grafting: A multicenter trial. J. Thorac. Cardiovasc. Surg. 2003, 126, 1568–1574. [Google Scholar] [CrossRef] [Green Version]
- Klima, U.; Maringka, M.; Bagaev, E.; Kirschner, S.; Haverich, A. Total magnetic vascular coupling for arterial revascularization. J. Thorac. Cardiovasc. Surg. 2004, 127, 602–603. [Google Scholar] [CrossRef] [Green Version]
- Wong, T.; Mayet, J.; Casula, R.P. Minimal invasive direct revascularisation of the left anterior descending artery using a novel magnetic vascular anastomotic device. Heart 2004, 90, 632. [Google Scholar] [CrossRef] [Green Version]
- Athanasiou, T.; Ashrafian, H.; Glenville, B.; Casula, R. Coronary artery bypass with the use of a magnetic distal anastomotic device: Surgical technique and preliminary experience. Heart. Surg. Forum 2004, 7, 356–359. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Falk, V.; Walther, T.; Jacobs, S.; Wolf, R.K.; Mohr, F.W. Facilitated MIDCAB using a magnetic coupling device. Ann. Thorac. Surg. 2005, 79, 691–693. [Google Scholar] [CrossRef] [PubMed]
- Vicol, C.; Eifert, S.; Oberhoffer, M.; Boekstegers, P.; Knez, A.; Christ, F.; Reichart, B. Early clinical results with a magnetic connector for distal coronary artery anastomoses. Ann. Thorac. Surg. 2005, 79, 1738–1742; discussion 1742–1743. [Google Scholar] [CrossRef] [PubMed]
- Klima, U.; Kofidis, T.; Beilner, J.; Maringka, M.; Kirschner, S.; Haverich, A. Anastomotic obstruction after magnetic vascular coupling after minimally invasive direct coronary artery bypass grafting. Ann. Thorac. Surg. 2006, 81, 728–729. [Google Scholar] [CrossRef]
- Vicol, C.; Eifert, S.; Oberhoffer, M.; Boekstegers, P.; Reichart, B. Mid-term patency after magnetic coupling for distal bypass anastomosis in coronary surgery. Ann. Thorac. Surg. 2006, 82, 1452–1456. [Google Scholar] [CrossRef] [PubMed]
- Charitou, A.; Panesar, S.S.; De, L.S.R.; Athanasiou, T. Novel use of a magnetic coupling device to repair damage of the internal thoracic artery. J. Card. Surg. 2006, 21, 89–91. [Google Scholar] [CrossRef] [PubMed]
- Lipham, J.C.; DeMeester, T.R.; Ganz, R.A.; Bonavina, L.; Saino, G.; Dunn, D.H.; Fockens, P.; Bemelman, W. The LINX(R) reflux management system: Confirmed safety and efficacy now at 4 years. Surg. Endosc. 2012, 26, 2944–2949. [Google Scholar] [CrossRef] [PubMed]
- Ganz, R.A.; Peters, J.H.; Horgan, S.; Bemelman, W.A.; Dunst, C.M.; Edmundowicz, S.A.; Lipham, J.C.; Luketich, J.D.; Melvin, W.S.; Oelschlager, B.K.; et al. Esophageal sphincter device for gastroesophageal reflux disease. N. Engl. J. Med. 2013, 368, 719–727. [Google Scholar] [CrossRef] [Green Version]
- Bonavina, L.; Saino, G.; Bona, D.; Sironi, A.; Lazzari, V. One hundred consecutive patients treated with magnetic sphincter augmentation for gastroesophageal reflux disease: 6 years of clinical experience from a single center. J. Am. Coll. Surg. 2013, 217, 577–585. [Google Scholar] [CrossRef]
- Smith, C.D.; DeVault, K.R.; Buchanan, M. Introduction of mechanical sphincter augmentation for gastroesophageal reflux disease into practice: Early clinical outcomes and keys to successful adoption. J. Am. Coll. Surg. 2014, 218, 776–781. [Google Scholar] [CrossRef]
- Bauer, M.; Meining, A.; Kranzfelder, M.; Jell, A.; Schirren, R.; Wilhelm, D.; Friess, H.; Feussner, H. Endoluminal perforation of a magnetic antireflux device. Surg. Endosc. 2015, 29, 3806–3810. [Google Scholar] [CrossRef] [PubMed]
- Saino, G.; Bonavina, L.; Lipham, J.C.; Dunn, D.; Ganz, R.A. Magnetic Sphincter Augmentation for Gastroesophageal Reflux at 5 Years: Final Results of a Pilot Study Show Long-Term Acid Reduction and Symptom Improvement. J. Laparoendosc. Adv. Surg. Tech. A 2015, 25, 787–792. [Google Scholar] [CrossRef] [PubMed]
- Aiolfi, A.; Asti, E.; Bernardi, D.; Bonitta, G.; Rausa, E.; Siboni, S.; Bonavina, L. Early results of magnetic sphincter augmentation versus fundoplication for gastroesophageal reflux disease: Systematic review and meta-analysis. Int. J. Surg. 2018, 52, 82–88. [Google Scholar] [CrossRef] [PubMed]
- Bell, R.; Lipham, J.; Louie, B.E.; Williams, V.; Luketich, J.; Hill, M.; Richards, W.; Dunst, C.; Lister, D.; McDowell-Jacobs, L.; et al. Magnetic Sphincter Augmentation Superior to Proton Pump Inhibitors for Regurgitation in a 1-Year Randomized Trial. Clin. Gastroenterol. Hepatol. 2020, 18, 1736–1743 e1732. [Google Scholar] [CrossRef] [PubMed]
- Bortolotti, M.; Ugolini, G.; Grandis, A.; Montroni, I.; Mazzero, G. A novel magnetic device to prevent fecal incontinence (preliminary study). Int. J. Color. Dis. 2008, 23, 499–501. [Google Scholar] [CrossRef]
- Lehur, P.A.; McNevin, S.; Buntzen, S.; Mellgren, A.F.; Laurberg, S.; Madoff, R.D. Magnetic anal sphincter augmentation for the treatment of fecal incontinence: A preliminary report from a feasibility study. Dis. Colon. Rectum. 2010, 53, 1604–1610. [Google Scholar] [CrossRef]
- Barussaud, M.L.; Mantoo, S.; Wyart, V.; Meurette, G.; Lehur, P.A. The magnetic anal sphincter in faecal incontinence: Is initial success sustained over time? Color. Dis. 2013, 15, 1499–1503. [Google Scholar] [CrossRef] [PubMed]
- Jayne, D.G.; Williams, A.E.; Corrigan, N.; Croft, J.; Pullan, A.; Napp, V.; Kelly, R.; Meads, D.; Vargas-Palacios, A.; Martin, A.; et al. Sacral nerve stimulation versus the magnetic sphincter augmentation device for adult faecal incontinence: The SaFaRI RCT. Health Technol. Assess. 2021, 25, 1–96. [Google Scholar] [CrossRef]
- Ali-El-Dein, B.; El-Demerdash, R.; Kock, N.G.; Ghoneim, M.A. A magnetic device for increasing the urethral resistance to flow: An experimental study in female dogs. BJU Int. 2000, 85, 150–154. [Google Scholar] [CrossRef] [Green Version]
- Dominguez, G.; Durand, L.; De Rosa, J.; Danguise, E.; Arozamena, C.; Ferraina, P.A. Retraction and triangulation with neodymium magnetic forceps for single-port laparoscopic cholecystectomy. Surg. Endosc. 2009, 23, 1660–1666. [Google Scholar] [CrossRef]
- Rivas, H.; Robles, I.; Riquelme, F.; Vivanco, M.; Jimenez, J.; Marinkovic, B.; Uribe, M. Magnetic Surgery: Results From First Prospective Clinical Trial in 50 Patients. Ann. Surg. 2018, 267, 88–93. [Google Scholar] [CrossRef] [PubMed]
- Haskins, I.N.; Strong, A.T.; Allemang, M.T.; Bencsath, K.P.; Rodriguez, J.H.; Kroh, M.D. Magnetic surgery: First U.S. experience with a novel device. Surg. Endosc. 2018, 32, 895–899. [Google Scholar] [CrossRef] [PubMed]
- Morales-Conde, S.; Dominguez, G.; Gomez, J.C.; Socas, M.; Barranco, A.; Moreno, J.G.; Padillo, F.J. Magnetic-assisted single-port sleeve gastrectomy. Surg. Innov. 2013, 20, NP9–NP11. [Google Scholar] [CrossRef] [PubMed]
- Rahman, R.; Azagury, D.E. Novel technologies and techniques in bariatric surgery. Minerva Chir. 2017, 72, 125–139. [Google Scholar] [CrossRef] [PubMed]
- Davis, M.; Davalos, G.; Ortega, C.; Chen, S.; Schimpke, S.; Jain-Spangler, K.; Yoo, J.; Seymour, K.; Sudan, R.; Portenier, D.; et al. Magnetic Liver Retraction: An Incision-Less Approach for Less Invasive Bariatric Surgery. Obes. Surg. 2019, 29, 1068–1073. [Google Scholar] [CrossRef]
- Rassweiler, M.C.; Michel, M.S.; Ritter, M.; Honeck, P. Magnetic Ureteral Stent Removal Without Cystoscopy: A Randomized Controlled Trial. J. Endourol. 2017, 31, 762–766. [Google Scholar] [CrossRef] [PubMed]
- Sevcenco, S.; Eredics, K.; Lusuardi, L.; Klingler, H.C. Evaluation of pain perception associated with use of the magnetic-end ureteric double-J stent for short-term ureteric stenting. World J. Urol. 2018, 36, 475–479. [Google Scholar] [CrossRef] [PubMed]
- Harrison, M.R.; Curran, P.F.; Jamshidi, R.; Christensen, D.; Bratton, B.J.; Fechter, R.; Hirose, S. Magnetic mini-mover procedure for pectus excavatum II: Initial findings of a Food and Drug Administration-sponsored trial. J. Pediatr. Surg. 2010, 45, 185–191; discussion 191–192. [Google Scholar] [CrossRef] [PubMed]
- Harrison, M.R.; Gonzales, K.D.; Bratton, B.J.; Christensen, D.; Curran, P.F.; Fechter, R.; Hirose, S. Magnetic mini-mover procedure for pectus excavatum III: Safety and efficacy in a Food and Drug Administration-sponsored clinical trial. J. Pediatr. Surg. 2012, 47, 154–159. [Google Scholar] [CrossRef]
- Graves, C.E.; Hirose, S.; Raff, G.W.; Iqbal, C.W.; Imamura-Ching, J.; Christensen, D.; Fechter, R.; Kwiat, D.; Harrison, M.R. Magnetic Mini-Mover Procedure for pectus excavatum IV: FDA sponsored multicenter trial. J. Pediatr. Surg. 2017, 52, 913–919. [Google Scholar] [CrossRef]
- Rosenbluth, K.H.; Kwiat, D.A.; Harrison, M.R.; Kezirian, E.J. Hyoid bone advancement for improving airway patency: Cadaver study of a magnet-based system. Otolaryngol. Head Neck Surg. 2012, 146, 491–496. [Google Scholar] [CrossRef] [PubMed]
- Cheung, K.M.; Cheung, J.P.; Samartzis, D.; Mak, K.C.; Wong, Y.W.; Cheung, W.Y.; Akbarnia, B.A.; Luk, K.D. Magnetically controlled growing rods for severe spinal curvature in young children: A prospective case series. Lancet 2012, 379, 1967–1974. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jenks, M.; Craig, J.; Higgins, J.; Willits, I.; Barata, T.; Wood, H.; Kimpton, C.; Sims, A. The MAGEC system for spinal lengthening in children with scoliosis: A NICE Medical Technology Guidance. Appl. Health Econ. Health Policy 2014, 12, 587–599. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lorenz, H.M.; Badwan, B.; Hecker, M.M.; Tsaknakis, K.; Groenefeld, K.; Braunschweig, L.; Hell, A.K. Magnetically Controlled Devices Parallel to the Spine in Children with Spinal Muscular Atrophy. JB JS Open Access 2017, 2, e0036. [Google Scholar] [CrossRef]
- Subramanian, T.; Ahmad, A.; Mardare, D.M.; Kieser, D.C.; Mayers, D.; Nnadi, C. A six-year observational study of 31 children with early-onset scoliosis treated using magnetically controlled growing rods with a minimum follow-up of two years. Bone Jt. J. 2018, 100-B, 1187–1200. [Google Scholar] [CrossRef] [PubMed]
- Oetgen, M.E.; McNulty, E.M.; Matthews, A.L. Cost-Effectiveness of Magnetically Controlled Growing Rods: Who Really Benefits? Spine Deform. 2019, 7, 501–504. [Google Scholar] [CrossRef] [PubMed]
- Harshavardhana, N.S.; Noordeen, M.H.H.; Dormans, J.P. Cost Analysis of Magnet-driven Growing Rods for Early-onset Scoliosis at 5 Years. Spine 2019, 44, 60–67. [Google Scholar] [CrossRef] [PubMed]
- Guan, D.; Zhang, Y.; Xu, J. Clinical Outcome of Magnetically Controlled Growing Rod in Early-onset Scoliosis: A Systematic Review. Clin. Spine Surg. 2020, 33, 150–155. [Google Scholar] [CrossRef]
- Steichen, F.M.; Ravitch, M.M. History of mechanical devices and instruments for suturing. Curr. Probl. Surg. 1982, 19, 3–52. [Google Scholar] [CrossRef] [PubMed]
- Hardy, T.G., Jr.; Pace, W.G.; Maney, J.W.; Katz, A.R.; Kaganov, A.L. A biofragmentable ring for sutureless bowel anastomosis. An experimental study. Dis. Colon. Rectum. 1985, 28, 484–490. [Google Scholar] [CrossRef]
- Wullstein, C.; Gross, E. Compression anastomosis (AKA-2) in colorectal surgery: Results in 442 consecutive patients. Br. J. Surg. 2000, 87, 1071–1075. [Google Scholar] [CrossRef] [PubMed]
- Zhang, D.; Zheng, C.; Song, C. A modified method of using laparoscopic compression anastomosis clip for gastrointestinal anastomosis. Minim. Invasive Ther. Allied Technol. 2010, 19, 350–354. [Google Scholar] [CrossRef] [PubMed]
- Tabola, R.; Cirocchi, R.; Fingerhut, A.; Arezzo, A.; Randolph, J.; Grassi, V.; Binda, G.A.; D’Andrea, V.; Abraha, I.; Popivanov, G.; et al. A systematic analysis of controlled clinical trials using the NiTi CAR compression ring in colorectal anastomoses. Tech. Coloproctol. 2017, 21, 177–184. [Google Scholar] [CrossRef] [PubMed]
- Ryou, M.; Agoston, A.T.; Thompson, C.C. Endoscopic intestinal bypass creation by using self-assembling magnets in a porcine model. Gastrointest. Endosc. 2016, 83, 821–825. [Google Scholar] [CrossRef] [PubMed]
- Pedersen, R.N.; Calzolari, E.; Husby, S.; Garne, E. Oesophageal atresia: Prevalence, prenatal diagnosis and associated anomalies in 23 European regions. Arch. Dis. Child. 2012, 97, 227–232. [Google Scholar] [CrossRef] [Green Version]
- Zimmer, J.; Eaton, S.; Murchison, L.E.; De Coppi, P.; Ure, B.M.; Dingemann, C. State of Play: Eight Decades of Surgery for Esophageal Atresia. Eur. J. Pediatr. Surg. 2019, 29, 39–48. [Google Scholar] [CrossRef]
- Sterlin, A.; Evans, L.; Mahler, S.; Lindner, A.; Dickmann, J.; Heimann, A.; Sahlabadi, M.; Aribindi, V.; Harrison, M.R.; Muensterer, O.J. An experimental study on long term outcomes after magnetic esophageal compression anastomosis in piglets. J. Pediatr. Surg. 2022, 57, 34–40. [Google Scholar] [CrossRef]
- Morbiducci, U.; Lemma, M.; Ponzini, R.; Boi, A.; Bondavalli, L.; Antona, C.; Montevecchi, F.M.; Redaelli, A. Does the Ventrica magnetic vascular positioner (MVP) for coronary artery bypass grafting significantly alter local fluid dynamics? A numeric study. Int. J. Artif. Organs 2007, 30, 628–639. [Google Scholar] [CrossRef]
- Liu, S.Q.; Lei, P.; Cui, X.H.; Lv, Y.; Li, J.H.; Song, Y.L.; Zhao, G. Sutureless anastomoses using magnetic rings in canine liver transplantation model. J. Surg. Res. 2013, 185, 923–933. [Google Scholar] [CrossRef]
- Wang, H.H.; Ma, J.; Wang, S.P.; Ma, F.; Lu, J.W.; Xu, X.H.; Lv, Y.; Yan, X.P. Magnetic Anastomosis Rings to Create Portacaval Shunt in a Canine Model of Portal Hypertension. J. Gastrointest. Surg. 2019, 23, 2184–2192. [Google Scholar] [CrossRef] [PubMed]
- Yan, X.; Fan, C.; Ma, J.; Li, J.; Dong, D.; Wang, H.; Ma, F.; Zheng, X.; Lv, Y. Portacaval shunt established in six dogs using magnetic compression technique. PLoS ONE 2013, 8, e76873. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yan, X.P.; Liu, W.Y.; Ma, J.; Li, J.P.; Lv, Y. Extrahepatic portacaval shunt via a magnetic compression technique: A cadaveric feasibility study. World J. Gastroenterol. 2015, 21, 8073–8080. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.R.; Dempsey, D.T.; Richter, J.E. Trends and perioperative outcomes of inpatient antireflux surgery in the United States, 1993-2006. Dis. Esophagus 2011, 24, 215–223. [Google Scholar] [CrossRef] [PubMed]
- Wong, W.D.; Congliosi, S.M.; Spencer, M.P.; Corman, M.L.; Tan, P.; Opelka, F.G.; Burnstein, M.; Nogueras, J.J.; Bailey, H.R.; Devesa, J.M.; et al. The safety and efficacy of the artificial bowel sphincter for fecal incontinence: Results from a multicenter cohort study. Dis. Colon. Rectum. 2002, 45, 1139–1153. [Google Scholar] [CrossRef]
- Bridoux, V.; Gourcerol, G.; Leroi, A.M.; Ducrotte, P.; Michot, F.; Tuech, J.J. Response to Barussaud et al.: The magnetic anal sphincter in faecal incontinence, is initial success sustained over time? Color. Dis. 2014, 16, 145–146. [Google Scholar] [CrossRef] [PubMed]
- Wong, M.T.; Meurette, G.; Stangherlin, P.; Lehur, P.A. The magnetic anal sphincter versus the artificial bowel sphincter: A comparison of 2 treatments for fecal incontinence. Dis. Colon. Rectum. 2011, 54, 773–779. [Google Scholar] [CrossRef]
- Wong, M.T.; Meurette, G.; Wyart, V.; Lehur, P.A. Does the magnetic anal sphincter device compare favourably with sacral nerve stimulation in the management of faecal incontinence? Color. Dis. 2012, 14, e323–e329. [Google Scholar] [CrossRef] [PubMed]
- Lehur, P.A.; Christoforidis, D.; Meurette, G. Artificial Sphincters to Treat Severe Fecal Incontinence: Currently in a Deadlock. Dis. Colon. Rectum. 2020, 63, 1017–1019. [Google Scholar] [CrossRef]
- Block, A.M.; Tamburini, L.M.; Zeng, F.; Mancini, M.R.; Jackson, C.A.; Antonacci, C.L.; Karsmarski, O.P.; Stelzer, J.W.; Wellington, I.J.; Lee, M.C. Surgical Treatment of Pediatric Scoliosis: Historical Origins and Review of Current Techniques. Bioengineering 2022, 9, 600. [Google Scholar] [CrossRef] [PubMed]
- Choi, E.; Yaszay, B.; Mundis, G.; Hosseini, P.; Pawelek, J.; Alanay, A.; Berk, H.; Cheung, K.; Demirkiran, G.; Ferguson, J.; et al. Implant Complications After Magnetically Controlled Growing Rods for Early Onset Scoliosis: A Multicenter Retrospective Review. J. Pediatr. Orthop. 2017, 37, e588–e592. [Google Scholar] [CrossRef]
- Graves, C.E.; Moyer, J.; Zobel, M.J.; Mora, R.; Smith, D.; O’Day, M.; Padilla, B.E. Intraoperative intercostal nerve cryoablation During the Nuss procedure reduces length of stay and opioid requirement: A randomized clinical trial. J. Pediatr. Surg. 2019, 54, 2250–2256. [Google Scholar] [CrossRef] [PubMed]
- Brana, I.; Calles, A.; LoRusso, P.M.; Yee, L.K.; Puchalski, T.A.; Seetharam, S.; Zhong, B.; de Boer, C.J.; Tabernero, J.; Calvo, E. Carlumab, an anti-C-C chemokine ligand 2 monoclonal antibody, in combination with four chemotherapy regimens for the treatment of patients with solid tumors: An open-label, multicenter phase 1b study. Target. Oncol. 2015, 10, 111–123. [Google Scholar] [CrossRef] [PubMed]
- Lurje, G.; Raptis, D.A.; Steinemann, D.C.; Amygdalos, I.; Kambakamba, P.; Petrowsky, H.; Lesurtel, M.; Zehnder, A.; Wyss, R.; Clavien, P.A.; et al. Cosmesis and Body Image in Patients Undergoing Single-port Versus Conventional Laparoscopic Cholecystectomy: A Multicenter Double-blinded Randomized Controlled Trial (SPOCC-trial). Ann. Surg. 2015, 262, 728–734; discussion 734–735. [Google Scholar] [CrossRef] [PubMed]

| Contact Duration | Type of Device | Nature of Body Contact | Recommended Endpoint Testing |
|---|---|---|---|
| Limited contact (≤24 h) | Surface device | Intact skin | C, S, and I |
| Mucosal membrane | C, S, and I | ||
| Breached or compromised surface | C, S, I, Sy, and P | ||
| External communicating device | Blood path, indirect | C, S, I, Sy, P, and H | |
| Tissue/bone/dentin | C, S, I, Sy, and P | ||
| Circulating blood | C, S, I, Sy, P, G, and H | ||
| Implant device | Tissue/bone | C, S, I, Sy, and P | |
| Blood | C, S, I, Sy, P, G, Im, and H | ||
| Prolonged contact (>24 h to ≤30 days) | Surface device | Intact skin | C, S, and I |
| Mucosal membrane | C, S, I, Sy, P, Sub, and Im | ||
| Breached or compromised surface | C, S, I, Sy, P, Sub, and Im | ||
| External communicating device | Blood path, indirect | C, S, I, Sy, P, Sub, and H | |
| Tissue/bone/dentin | C, S, I, Sy, P, Sub, G, and Im | ||
| Circulating blood | C, S, I, Sy, P, Sub, G, Im, and H | ||
| Implant device | Tissue/bone | C, S, I, Sy, P, Sub, G, and Im | |
| Blood | C, S, I, Sy, P, Sub, G, Im, and H | ||
| Long-term/ permanent contact (>30 days) | Surface device | Intact skin | C, S, and I |
| Mucosal membrane | C, S, I, Sy, P, Sub, G, Im, and Ct | ||
| Breached or compromised surface | C, S, I, Sy, P, Sub, G, Im, Ct, and Car | ||
| External communicating device | Blood path, indirect | C, S, I, Sy, P, Sub, G, Im, Ct, and Car | |
| Tissue/bone/dentin | C, S, I, Sy, P, Sub, G, Im, Ct, Car, and H | ||
| Circulating blood | C, S, I, Sy, P, Sub, G, Im, Ct, and Car | ||
| Implant device | Tissue/bone | C, S, I, Sy, P, Sub, G, Im, Ct, and Car | |
| Blood | C, S, I, Sy, P, Sub, G, Im, Ct, Car, and H |
| Core Function | Type of Magnet System | Use of Magnet System | Example of Devices Approved for Humanitarian or Commercial Use | Published Studies |
|---|---|---|---|---|
| GS | Electromagnetic tube/catheter tip and external receiver unit | Real-time transmission of nasoenteric tube location during placement | CORTRAK Enteral Access System (Avanos Medical, Inc., Alpharetta, Georgia, USA) | Mathus-Vliegen 2010 [26], Smithard 2015 [27], an McCutcheon 2017 [28] |
| Real-time transmission of peripherally inserted central venous catheter (PICC) location during placement | Sherlock 3CG Tip Confirmation System (Becton, Dickinson and Company, Franklin Lakes, NJ, USA) | Tomaszewski 2017 [29], Mack 2020 [30], and Sone 2020 [31] | ||
| Paired intravascular magnetic catheter tips | Mating of catheter tips aligns as well as holds an artery and vein together for percutaneous arteriovenous fistula creation | everlinQ endoAVF System (Becton, Dickinson and Company, Franklin Lakes, NJ, USA) | Lok 2017 [32] | |
| NC | Magnetic compression anastomosis between two paired intraluminal magnets (spherical, discoid, ring, and cylindrical) | Connecting two small intestine segments | Xu 2015 [33] | |
| Connecting two enteric segments (e.g., stomach, small intestine, and colon) | Magnamosis Magnetic Compression Anastomosis Device (Myka Labs, UCSF Surgical Innovations, San Francisco, CA, USA) | Cope 1995 [34], Chopita 2005 [35], Jamshidi 2009 [36], Myers 2010 [37], Pichakron 2011 [38], Gonzales 2012 [39], Wall 2013 [40], Russell 2014 [41], and Graves 2017 [42] | ||
| Connecting the proximal intestine to the distal intestine to create a bypass channel (i.e., bariatric surgery) | Self-Forming Magnetic Anastomosis Device (GI Windows Surgical, West Bridgewater, MA, USA) | Ryou 2016 [43], Machytka 2017 [44], Schlottman 2021 [45], Gumustop 2022 [46], and Ore 2022 [47,48] | ||
| Connecting the proximal and distal esophageal pouches in esophageal atresia (congenital disorder) | Magnamosis Connect-EA (Myka Labs, UCSF Surgical Innovations, San Francisco, CA, USA); Flourish Pediatric Esophageal Atresia Device (Cook Medical, Bloomington, IN, USA) | Zaritzky 2009 [49], Zaritzky 2014 [50], Dorman 2016 [51], Slater 2019 [52], Muensterer 2020 [53], Wolfe 2020 [54], Muensterer 2021 [55], and Evans 2022 [56] | ||
| Connecting the bile duct to the stomach or small intestine to bypass bile duct stricture | Mimuro 2003 [57], Muraoka 2005 [58], Matsuno 2009 [59], and Jang 2020 [60] | |||
| Resecting a strictured esophagus, small intestine, bile duct, or colon to allow luminal contents to pass through | Takamizawa 2007 [61], Woo 2017 [62], Kamada 2020 [63], Isozaki 2020 [64], Liu 2020 [65], Kılıç 2020 [66], and Liu 2022 [67] | |||
| Paired intravascular magnetic ports | Creation of anastomosis between two blood vessels (e.g., coronary artery bypass surgery) | Magnetic Vascular Positioner (MVP) Series 6000 Distal Anastomosis System (Ventrica, Inc., Fremont, CA, USA) | Falk 2003 [68], Klima 2003 [69], Klima 2004 [70], Wong 2004 [71], Athanasiou 2004 [72], Falk 2005 [73], Vicol 2005 [74], Klima 2006 [75], Vicol 2006 [76], and Charitou 2006 [77] | |
| PHYS | Magnetic beads interlinked with titanium wires to form a flexible ring | Placed around the distal esophagus to recreate a physiologic lower esophageal sphincter in gastroesophageal reflux disease (GERD) | LINX (Torax Medical, Inc., Shoreview, MN, USA) | Lipham 2012 [78], Ganz 2013 [79], Bonavina 2013 [80], Smith 2014 [81], Bauer 2015 [82], Saino 2015 [83], Aiolfi 2018 [84], and Bell 2020 [85] |
| Placed around the external anal sphincter to recreate physiologic sphincter function in fecal incontinence | FENIX Continence Restoration System (Torax Medical, Inc., Shoreview, MN, USA) | Bortolotti 2008 [86], Lehur 2010 [87], Barussaud 2013 [88], and Jayne 2021 [89] | ||
| Paired flat magnets | Placed anterior and posterior to the urethra to recreate urethral resistance in urinary incontinence | Ali-El-Dein 2000 [90] | ||
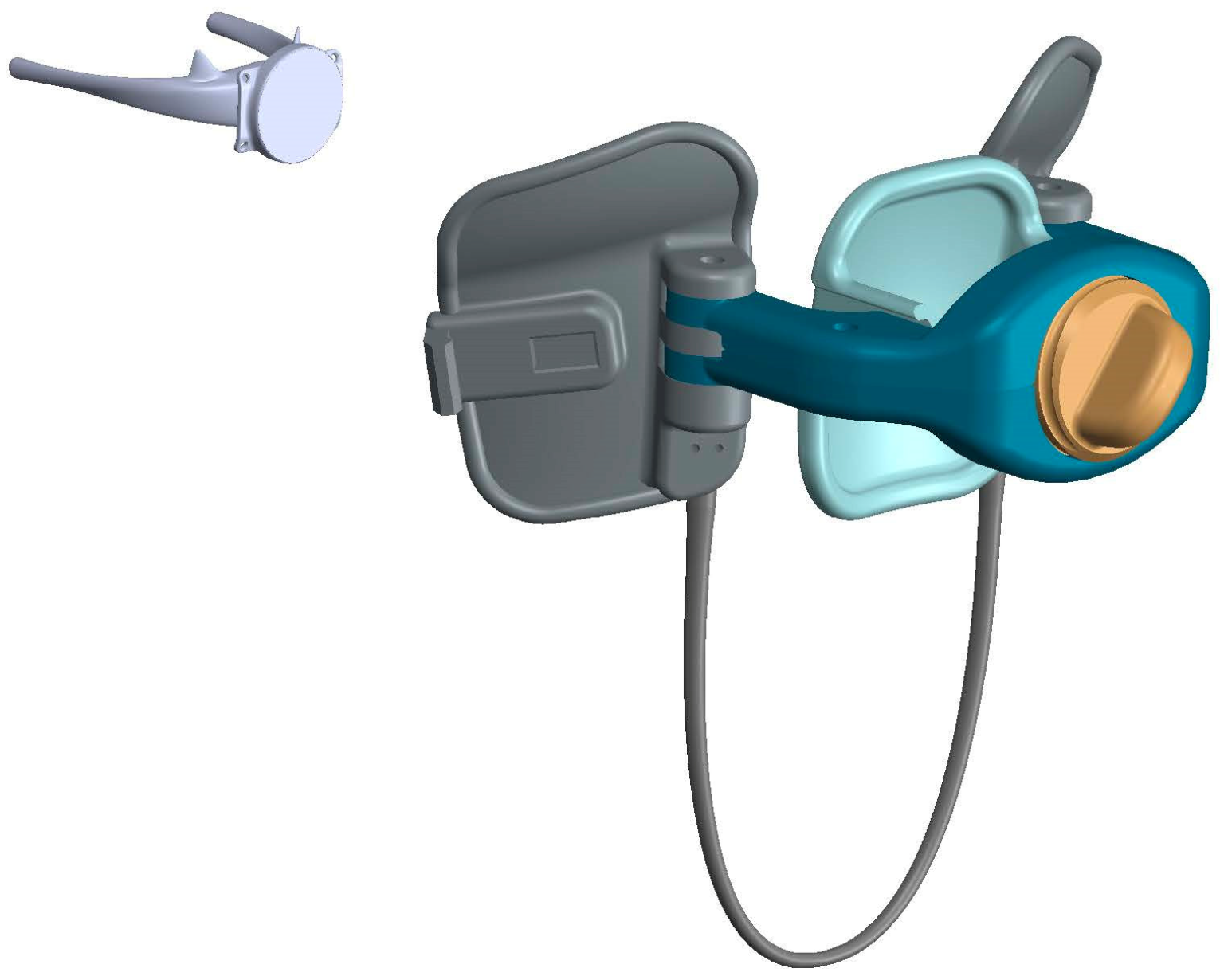
| IE | Detachable internal magnetic grasper controlled by an external magnet | Retraction of the gallbladder during cholecystectomy | Levita Magnetic Surgical System (Levita Magnetics, Inc., Menlo Park, CA, USA) | Dominguez 2009 [91], Rivas 2018 [92], and Haskins 2018 [93] |
| Retraction of the liver, stomach, or omentum during bariatric surgery | Morales-Conde 2013 [94], Rahman 2017 [95], and Davis 2019 [96] | |||
| Internal ureteral stent with a distal magnetic tip | Bedside removal of a stent by mating an internal stent tip with an introduced urethral magnetic catheter retrieval device | Magnetic Blackstar (Urovision-Urotech, Achenmuhle, Germany) | Rassweiler 2017 [97], Sevcenco 2018 [98] | |
| Implanted magnet and custom-fitted external brace with a paired magnet | Gradual chest wall remodeling in the pectus excavatum (congenital disorder) | Magnetic Mini-Mover (3MP): Magnimplant and Magnatract (Hayes Manufacturing, Sunnyvale, CA and Hantel Technologies, Hayward, CA, USA) | Harrison 2007 [25], Harrison 2010 [99], Harrison 2012 [100], and Graves 2017 [101] | |
| Hyoid bone advancement to maintain airway patency during sleep in obstructive sleep apnea (OSA) | Magnetic Apnea Prevention Device (Mag-Nap) (Mag-Nap, Inc., UCSF Surgical Innovations, San Francisco, CA, USA) | Rosenbluth 2011 [102] | ||
| Implanted distractable spinal rods with a magnetic lengthening mechanism driven by external magnetic remote control | Non-invasive spinal adjustment allows for the growth of a child with early onset scoliosis (congenital disorder) | MAGEC System (NuVasive, Inc., San Diego, CA, USA) | Cheung 2012 [103], Jenks 2014 [104], Lorenz 2017 [105], Subramanian 2018 [106], Oetgen 2019 [107], Harshavardhana 2019 [108], and Guan 2020 [109] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lee, W.G.; Evans, L.L.; Johnson, S.M.; Woo, R.K. The Evolving Use of Magnets in Surgery: Biomedical Considerations and a Review of Their Current Applications. Bioengineering 2023, 10, 442. https://doi.org/10.3390/bioengineering10040442
Lee WG, Evans LL, Johnson SM, Woo RK. The Evolving Use of Magnets in Surgery: Biomedical Considerations and a Review of Their Current Applications. Bioengineering. 2023; 10(4):442. https://doi.org/10.3390/bioengineering10040442
Chicago/Turabian StyleLee, William G., Lauren L. Evans, Sidney M. Johnson, and Russell K. Woo. 2023. "The Evolving Use of Magnets in Surgery: Biomedical Considerations and a Review of Their Current Applications" Bioengineering 10, no. 4: 442. https://doi.org/10.3390/bioengineering10040442
APA StyleLee, W. G., Evans, L. L., Johnson, S. M., & Woo, R. K. (2023). The Evolving Use of Magnets in Surgery: Biomedical Considerations and a Review of Their Current Applications. Bioengineering, 10(4), 442. https://doi.org/10.3390/bioengineering10040442






