Concept for the Treatment of Class III Anomalies with a Skeletally Anchored Appliance Fabricated in the CAD/CAM Process—The MIRA Appliance
Abstract
:1. Introduction
2. Diagnosis
3. Treatment
3.1. Treatment Objectives
3.2. Treatment Alternatives
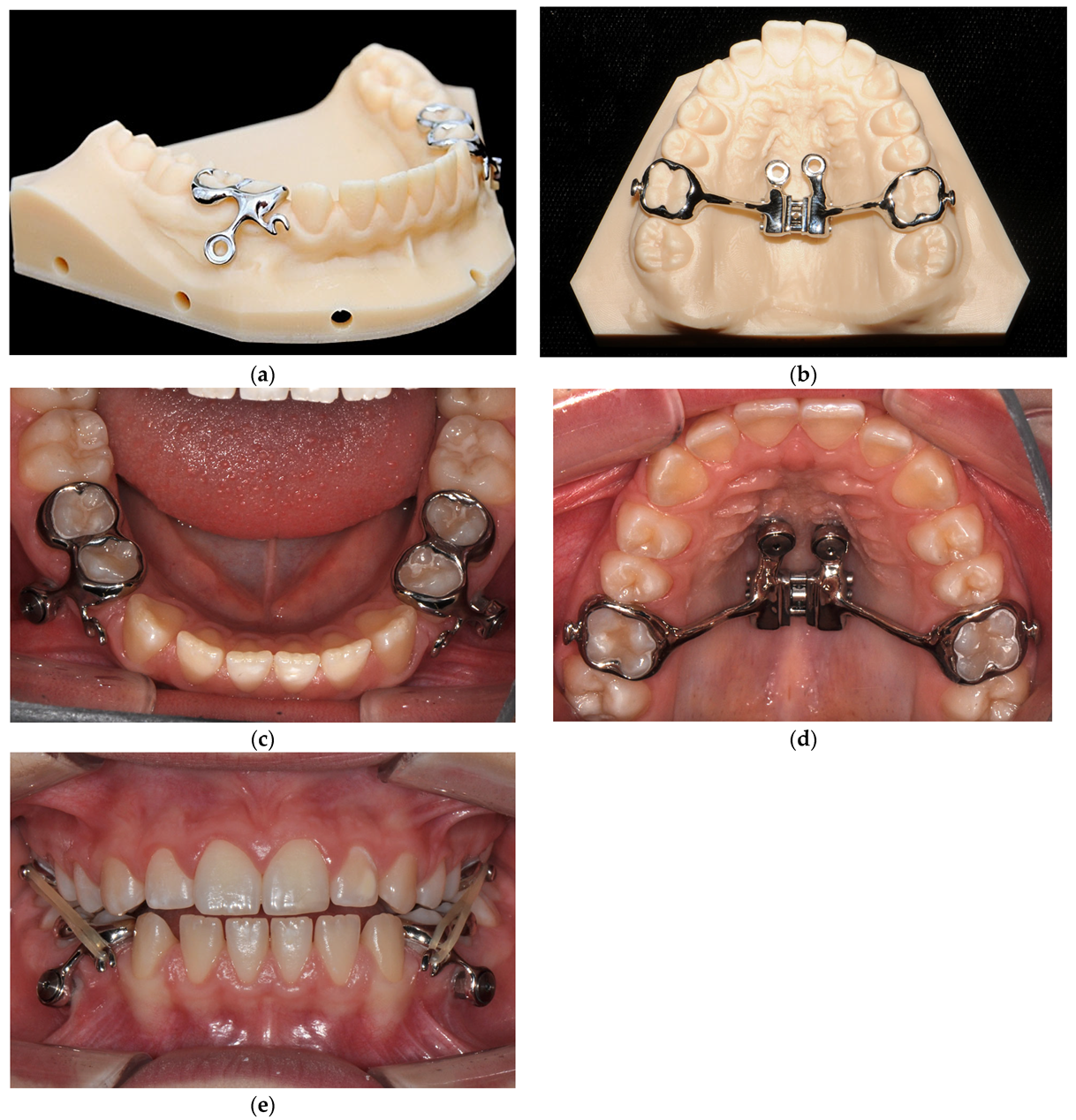
3.3. Treatment Progress
3.4. Treatment Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Tausche, E.; Luck, O.; Prein, J.; d’Hoedt, B.; Kubein-Meesenburg, D. The role of genetic factors in the development of skeletal Class III malocclusions: A retrospective cohort study. J. Orofac. Orthop. 2019, 80, 27–38. [Google Scholar]
- Al-Jewair, T.S.; Al-Jasser, R.; Al-Jamaan, A.; Alahmadi, H.; Al-Mutairi, M. Skeletal Class III malocclusion: A comprehensive review on diagnosis and management. J. Orthod. Sci. 2018, 7, 12. [Google Scholar] [CrossRef]
- DGKFO. DGZMK: Ideale Behandlungszeitpunkte Kieferorthopädischer Anomalien, Langversion 1.0, 2021, AWMF-Registriernummer: 083-038. Available online: https://www.awmf.org/leitlinien/detail/ll/083-038.html (accessed on 11 April 2022).
- De Toffol, L.; Pavoni, C.; Baccetti, T.; Franchi, L.; Cozza, P. Orthopedic treatment outcomes in Class III malocclusion. Angle Orthod. 2008, 78, 561–573. [Google Scholar] [CrossRef] [PubMed]
- Diedrich, P.; Berg, R. Kieferorthopädie, 4th ed.; Urban & Schwarzenberg: München, Germany, 2000. [Google Scholar]
- Tuncer, B.B.; Kaygisiz, E.; Tuncer, C.; Yüksel, S. Pharyngeal airway dimensions after chin cup treatment in Class III malocclusion subjects. J. Oral. Rehabil. 2009, 36, 110–117. [Google Scholar] [CrossRef] [PubMed]
- Hu, S.; An, K.; Peng, Y. Comparative efficacy of the bone-anchored maxillary protraction protocols for orthopaedic treatment in skeletal Class III malocclusion: A Bayesian network meta-analysis. Orthod. Craniofac. Res. 2022, 25, 243–250. [Google Scholar] [CrossRef]
- Tsui, W.K.; Chua, H.D.P.; Cheung, L.K. Bone anchor systems for orthodontic application: A systematic review. Int. J. Oral. Maxillofac. Surg. 2012, 41, 1427–1438. [Google Scholar] [CrossRef]
- De Clerck, H.; Geerinckx, V.; Siciliano, S. The Zygoma Anchorage System. J. Clin. Orthod. 2002, 36, 455–459. [Google Scholar]
- Miranda, F.; Bastos, J.C.D.C.; Dos Santos, A.M.; Vieira, L.S.; Aliaga-Del Castillo, A.; Janson, G.; Garib, D. Miniscrew-anchored maxillary protraction in growing Class III patients. J. Orthod. 2020, 47, 170–180. [Google Scholar] [CrossRef]
- Gera, S.; Cattaneo, P.M.; Hartig, L.E.; Cornelis, M.A. Computer-aided design and manufacturing of bone- and tooth-borne maxillary protraction with miniscrews and Class III elastics: Can we contemporize Class III treatments in growing patients? Am. J. Orthod. Dentofac. Orthop. 2021, 159, 125–132. [Google Scholar] [CrossRef]
- Willmann, J.H.; Nienkemper, M.; Tarraf, N.E.; Wilmes, B.; Drescher, D. Early Class III treatment with Hybrid-Hyrax-Facemask in comparison to Hybrid-Hyrax-Mentoplate-skeletal and dental outcomes. Prog. Orthod. 2018, 19, 42. [Google Scholar] [CrossRef]
- Wilmes, B.; Nienkemper, M.; Ludwig, B.; Kau, C.H.; Drescher, D. Early Class III treatment with a hybrid hyrax-mentoplate combination. J. Clin. Orthod. JCO 2011, 45, 15–39. Available online: https://pubmed.ncbi.nlm.nih.gov/21874777/ (accessed on 1 November 2022). [PubMed]
- Nucera, R.; Lo Giudice, A.; Bellocchio, A.M.; Spinuzza, P.; Caprioglio, A.; Perillo, L.; Matarese, G.; Cordasco, G. Bone and cortical bone thickness of mandibular buccal shelf for mini-screw insertion in adults. Angle Orthod. 2017, 87, 745–751. [Google Scholar] [CrossRef] [PubMed]
- Nucera, R.; Bellocchio, A.M.; Oteri, G.; Farah, A.J.; Rosalia, L.; Giancarlo, C.; Portelli, M. Bone and cortical bone characteristics of mandibular retromolar trigone and anterior ramus region for miniscrew insertion in adults. Am. J. Orthod. Dentofac. Orthop. 2019, 155, 330–338. [Google Scholar] [CrossRef]
- Mohammed, H.; Wafaie, K.; Rizk, M.Z.; Almuzian, M.; Sosly, R.; Bearn, D.R. Role of anatomical sites and correlated risk factors on the survival of orthodontic miniscrew implants: A systematic review and meta-analysis. Prog. Orthod. 2018, 19, 36. [Google Scholar] [CrossRef]
- Tepedino, M.; Cattaneo, P.M.; Niu, X.; Cornelis, M.A. Interradicular sites and cortical bone thickness for miniscrew insertion: A systematic review with meta-analysis. Am. J. Orthod. Dentofac. Orthop. 2020, 158, 783–798.e20. [Google Scholar] [CrossRef] [PubMed]
- Baccetti, T.; Franchi, L.; McNamara, J.A., Jr. An improved version of the cervical vertebral maturation (CVM) method for the assessment of mandibular growth. Angle Orthod. 2002, 72, 316–323. [Google Scholar] [PubMed]
- Cornelis, M.A.; Scheffler, N.R.; Nyssen-Behets, C.; De Clerck, H.J.; Tulloch, J.C. Patients’ and orthodontists’ perceptions of miniplates used for temporary skeletal anchorage: A prospective study. Am. J. Orthod. Dentofac. Orthop. 2008, 133, 18–24. [Google Scholar] [CrossRef]
- De Clerck, H.; Cevidanes, L.; Baccetti, T. Dentofacial effects of bone-anchored maxillary protraction: A controlled study of consecutively treated Class III patients. Am. J. Orthod. Dentofac. Orthop. 2010, 138, 577–581. [Google Scholar] [CrossRef]
- Feng, X.; Li, J.; Li, Y.; Zhao, Z.; Zhao, S.; Wang, J. Effectiveness of TAD-anchored maxillary protraction in late mixed dentition: A systematic review. Angle Orthod. 2012, 82, 1107–1114. [Google Scholar] [CrossRef]
- Faco, R.; Yatabe, M.; Cevidanes, L.H.S.; Timmerman, H.; De Clerck, H.J.; Garib, D. Bone-anchored maxillary protraction in unilateral cleft lip and palate: A cephalometric appraisal. Eur. J. Orthod. 2019, 41, 537–543. [Google Scholar] [CrossRef]
- Kama, J.D.; Özer, T.; Baran, S. Orthodontic and orthopaedic changes associated with treatment in subjects with Class III malocclusions. Eur. J. Orthod. 2006, 28, 496–502. [Google Scholar] [CrossRef] [PubMed]
- Lin, H.C.; Chang, H.P.; Chang, H.F. Treatment effects of occipitomental anchorage appliance of maxillary protraction combined with chincup traction in children with class III malocclusion. J. Formos. Med. Assoc. 2007, 106, 380–391. [Google Scholar] [CrossRef] [PubMed]
- Cevidanes, L.; Baccetti, T.; Franchi, L.; McNamara, J.A., Jr.; De Clerck, H. Comparison of two protocols for maxillary protraction: Bone anchors versus face mask with rapid maxillary expansion. Angle Orthod. 2010, 80, 799–806. [Google Scholar] [CrossRef]
- Sahin, T.; Delforge, A.; Garreau, E.; Raoul, G.; Ferri, J. Orthopedic treatment of Class III malocclusions using skeletal anchorage: A bibliographical review. Int. Orthod. 2016, 14, 263–272. [Google Scholar] [CrossRef] [PubMed]
- De Guzmán-Barrera, J.R.; Martínez, C.S.; Boronat-Catalá, M.; Montiel-Company, J.M.; Paredes-Gallardo, V.; Gandía-Franco, J.L.; Almerich-Silla, J.M.; Bellot-Arcis, C. Effectiveness of interceptive treatment of class III malocclusions with skeletal anchorage: A systematic review and metaanalysis. PLoS ONE 2017, 12, e0173875. [Google Scholar] [CrossRef] [PubMed]
- Şar, Ç.; Arman-Özçirpici, A.; Uçkan, S.; Yazici, A.C. Comparative evaluation of maxillary protraction with or without skeletal anchorage. Am. J. Orthod. Dentofac. Orthop. 2011, 139, 636–649. [Google Scholar] [CrossRef]
- Meyns, J.; Brasil, D.M.; Mazzi-Chaves, J.F.; Politis, C.; Jacobs, R. The clinical outcome of skeletal anchorage in interceptive treatment (in growing patients) for class III malocclusion. Int. J. Oral. Maxillofac. Surg. 2018, 47, 1003–1010. [Google Scholar] [CrossRef]
- Yang, X.; Li, C.; Bai, D.; Su, N.; Chen, T.; Xu, Y.; Han, X. Treatment effectiveness of Fränkel function regulator on the Class III malocclusion: A systematic review and meta-analysis. Am. J. Orthod. Dentofac. Orthop. 2014, 146, 143–154. [Google Scholar] [CrossRef]
- Wendl, B.; Stampfl, M.; Muchitsch, A.P.; Droschl, H.; Winsauer, H.; Walter, A.; Wendl, M.; Wendl, T. Langfristige skelettale und dentale Auswirkungen der Klasse-III-Behandlung mit Gesichtsmaske vs. Kinnkappe: Eine retrospektive Untersuchung. J. Orofac. Orthop. 2017, 78, 293–299. [Google Scholar] [CrossRef]








Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hodecker, L.D.; Kühle, R.; Weichel, F.; Roser, C.J.; Lux, C.J.; Bauer, C.A.J. Concept for the Treatment of Class III Anomalies with a Skeletally Anchored Appliance Fabricated in the CAD/CAM Process—The MIRA Appliance. Bioengineering 2023, 10, 616. https://doi.org/10.3390/bioengineering10050616
Hodecker LD, Kühle R, Weichel F, Roser CJ, Lux CJ, Bauer CAJ. Concept for the Treatment of Class III Anomalies with a Skeletally Anchored Appliance Fabricated in the CAD/CAM Process—The MIRA Appliance. Bioengineering. 2023; 10(5):616. https://doi.org/10.3390/bioengineering10050616
Chicago/Turabian StyleHodecker, Lutz D., Reinald Kühle, Frederic Weichel, Christoph J. Roser, Christopher J. Lux, and Carolien A. J. Bauer. 2023. "Concept for the Treatment of Class III Anomalies with a Skeletally Anchored Appliance Fabricated in the CAD/CAM Process—The MIRA Appliance" Bioengineering 10, no. 5: 616. https://doi.org/10.3390/bioengineering10050616
APA StyleHodecker, L. D., Kühle, R., Weichel, F., Roser, C. J., Lux, C. J., & Bauer, C. A. J. (2023). Concept for the Treatment of Class III Anomalies with a Skeletally Anchored Appliance Fabricated in the CAD/CAM Process—The MIRA Appliance. Bioengineering, 10(5), 616. https://doi.org/10.3390/bioengineering10050616





