Research Hotspots and Trends of Bone Xenograft in Clinical Procedures: A Bibliometric and Visual Analysis of the Past Decade
Abstract
:1. Introduction
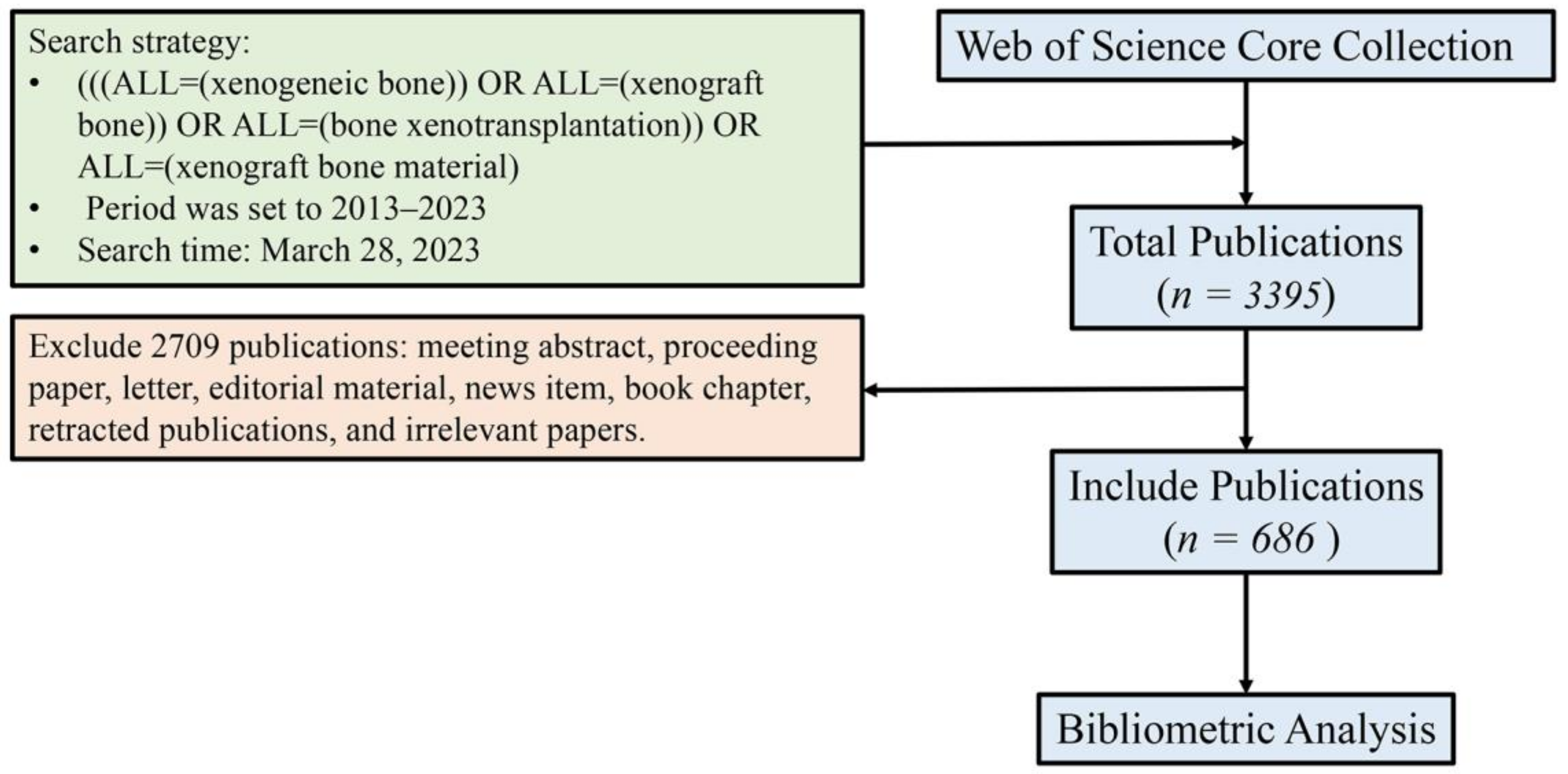
2. Materials and Methods
2.1. Data Collection
2.2. Bibliometric and Visualization Analysis
3. Results
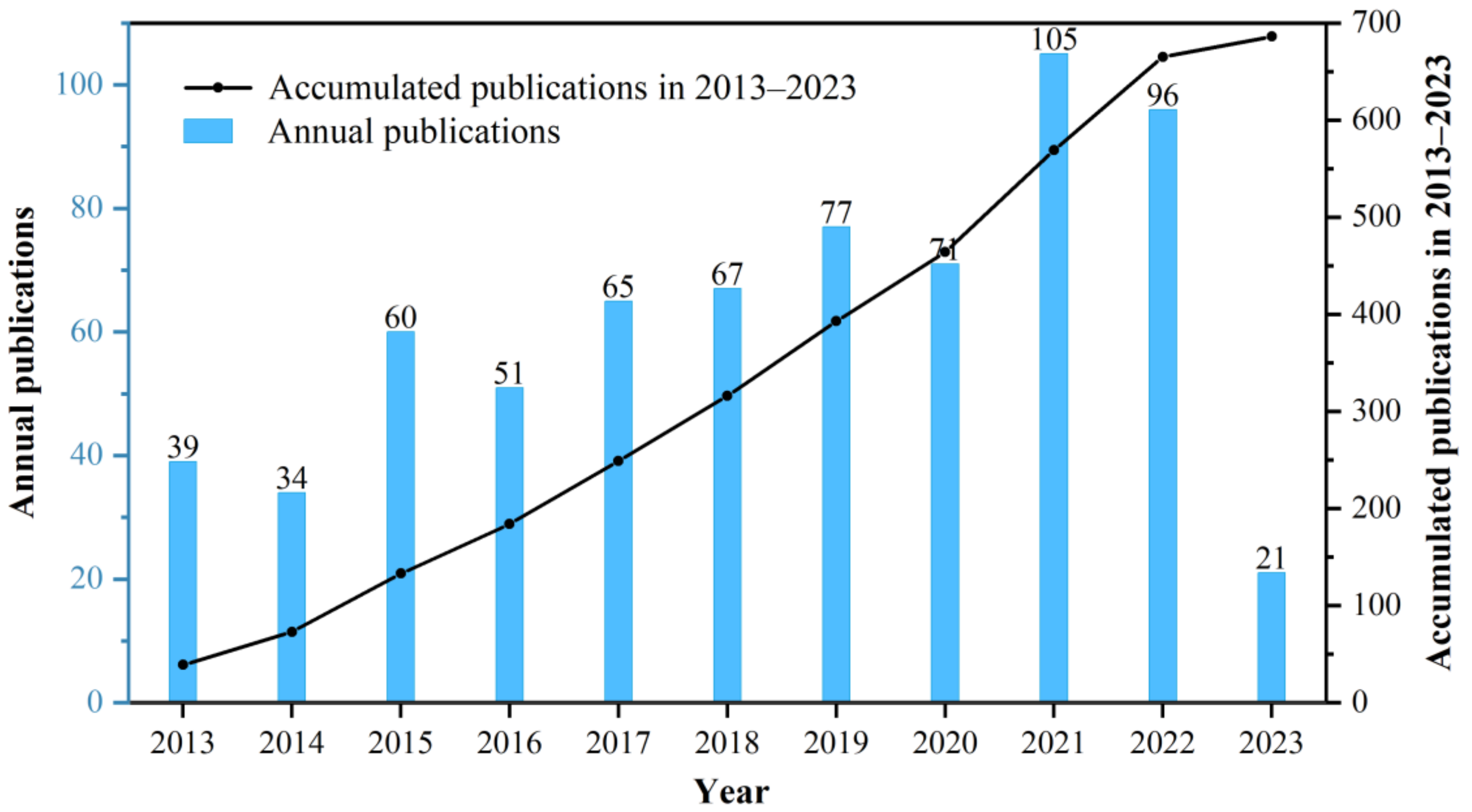
3.1. Publication of Annual Trend
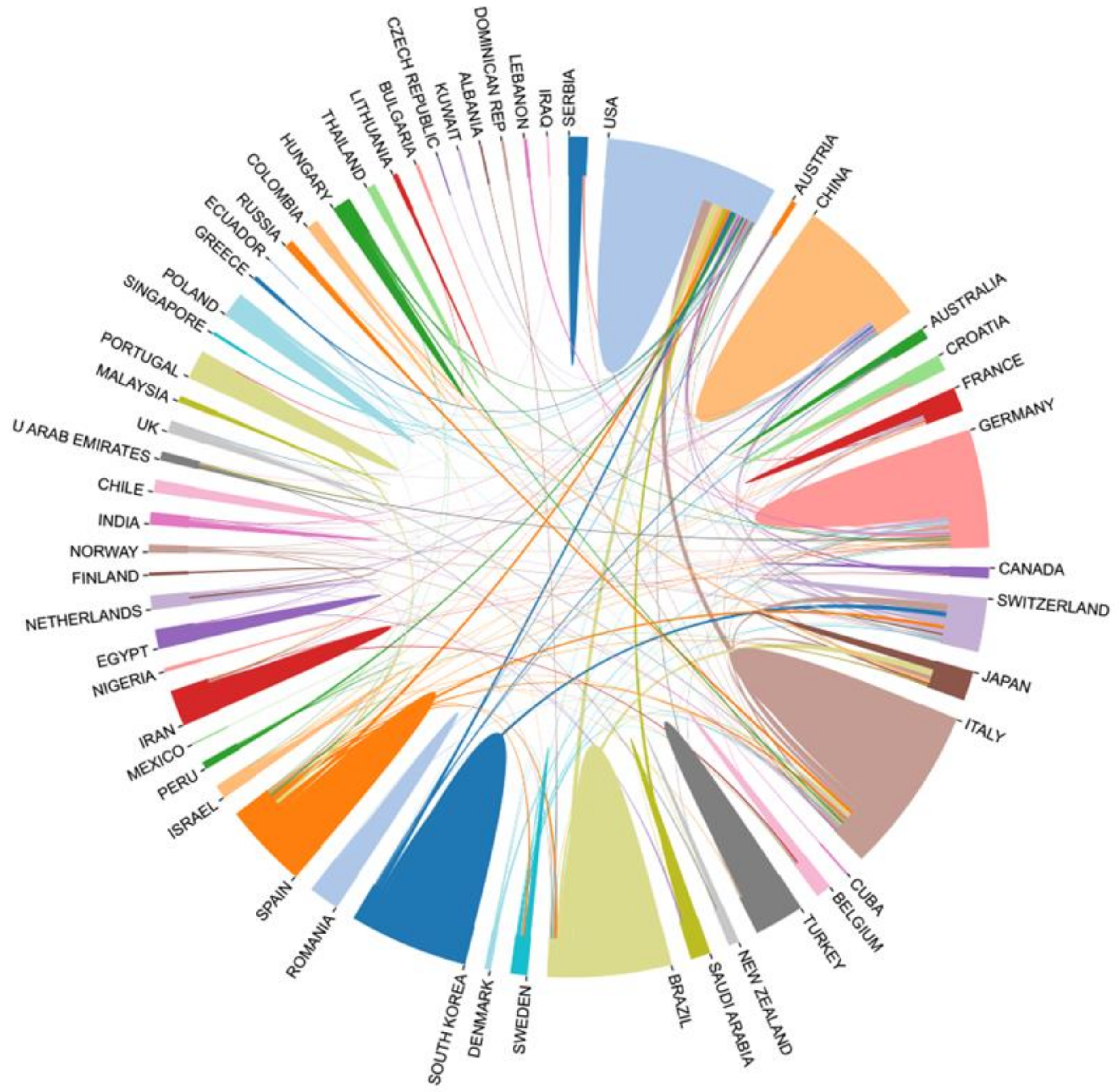
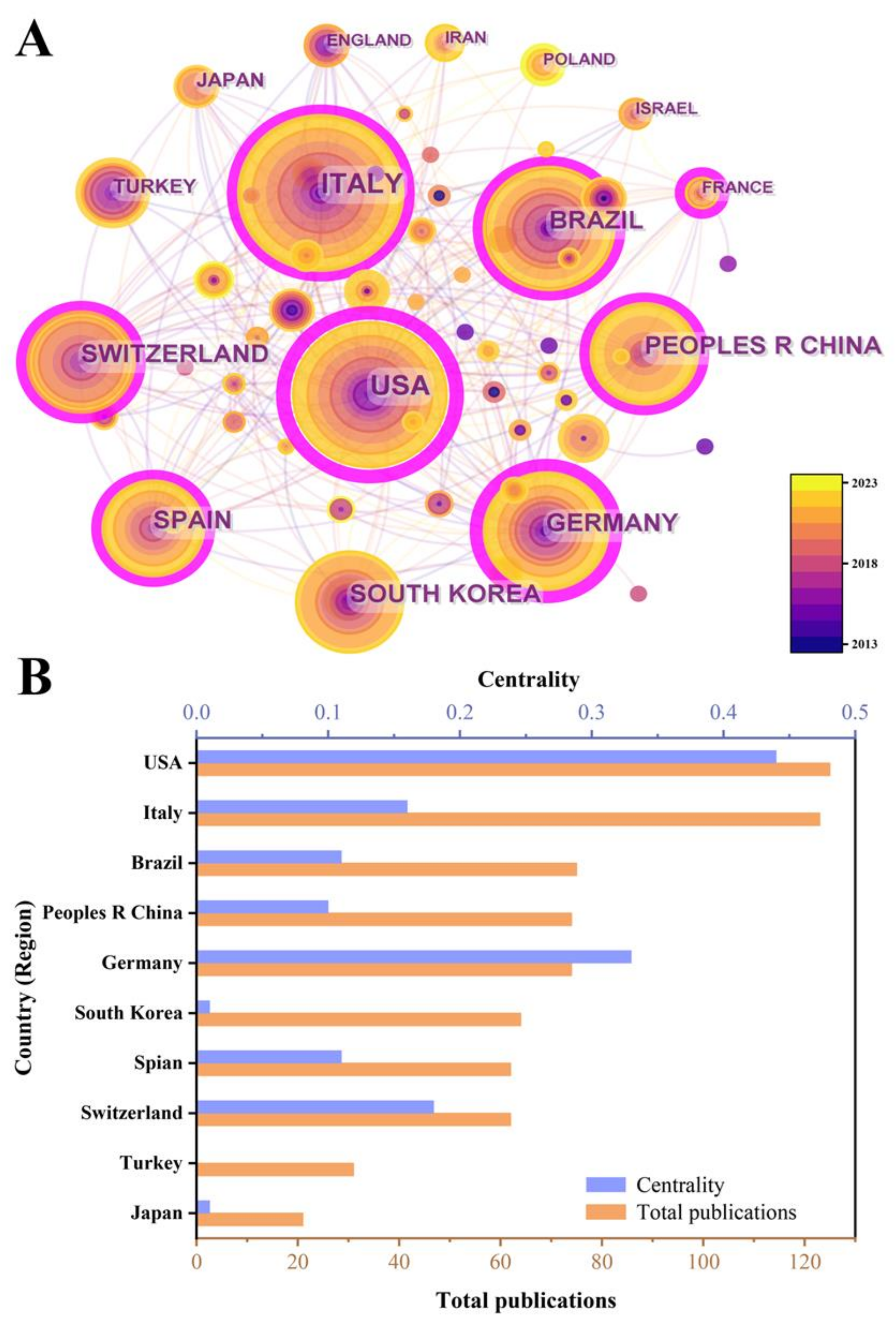
3.2. Analysis of National (Regional) Collaboration
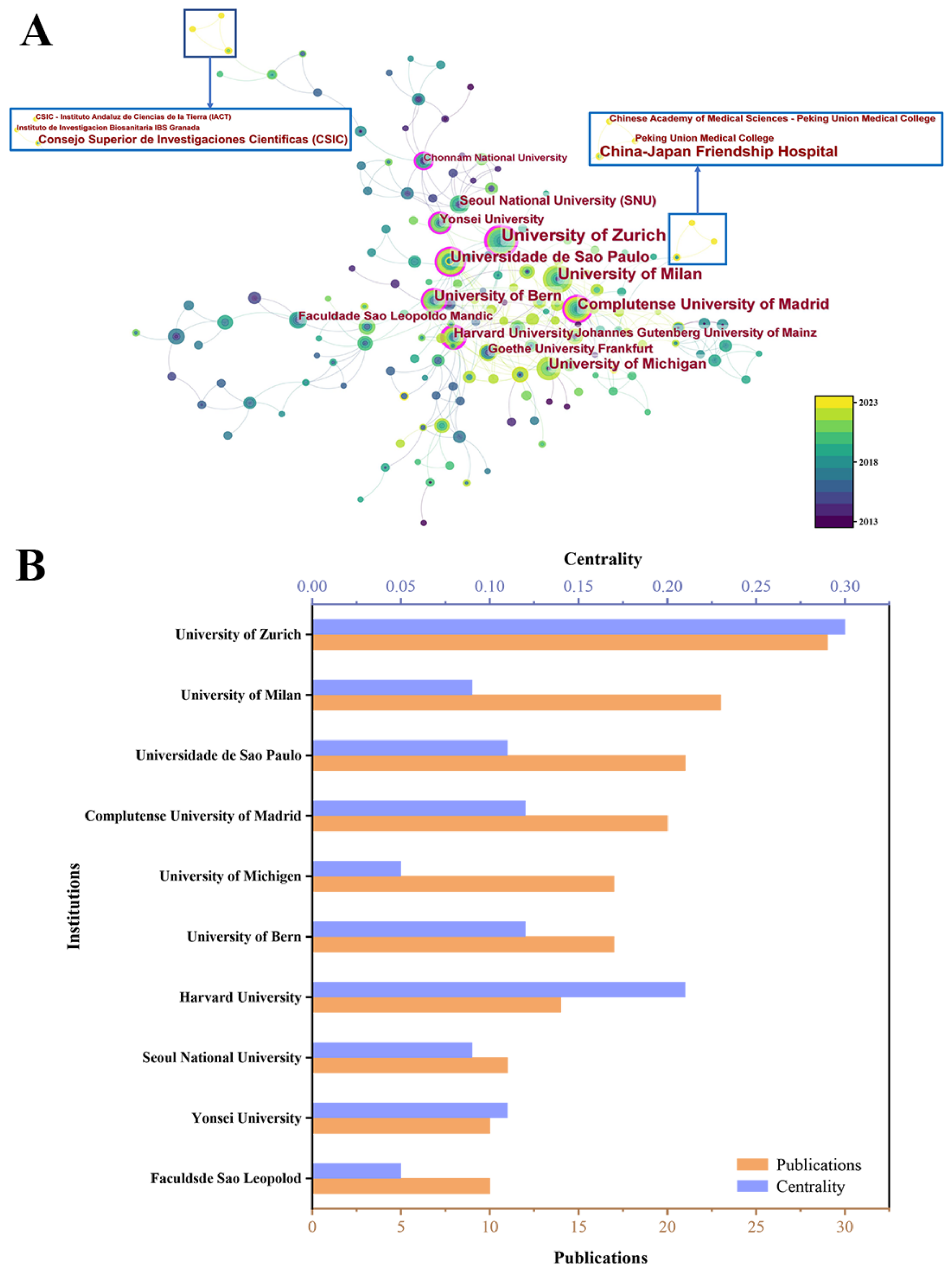
3.3. Analysis of Institution Collaboration
3.4. Analysis of Author Collaboration
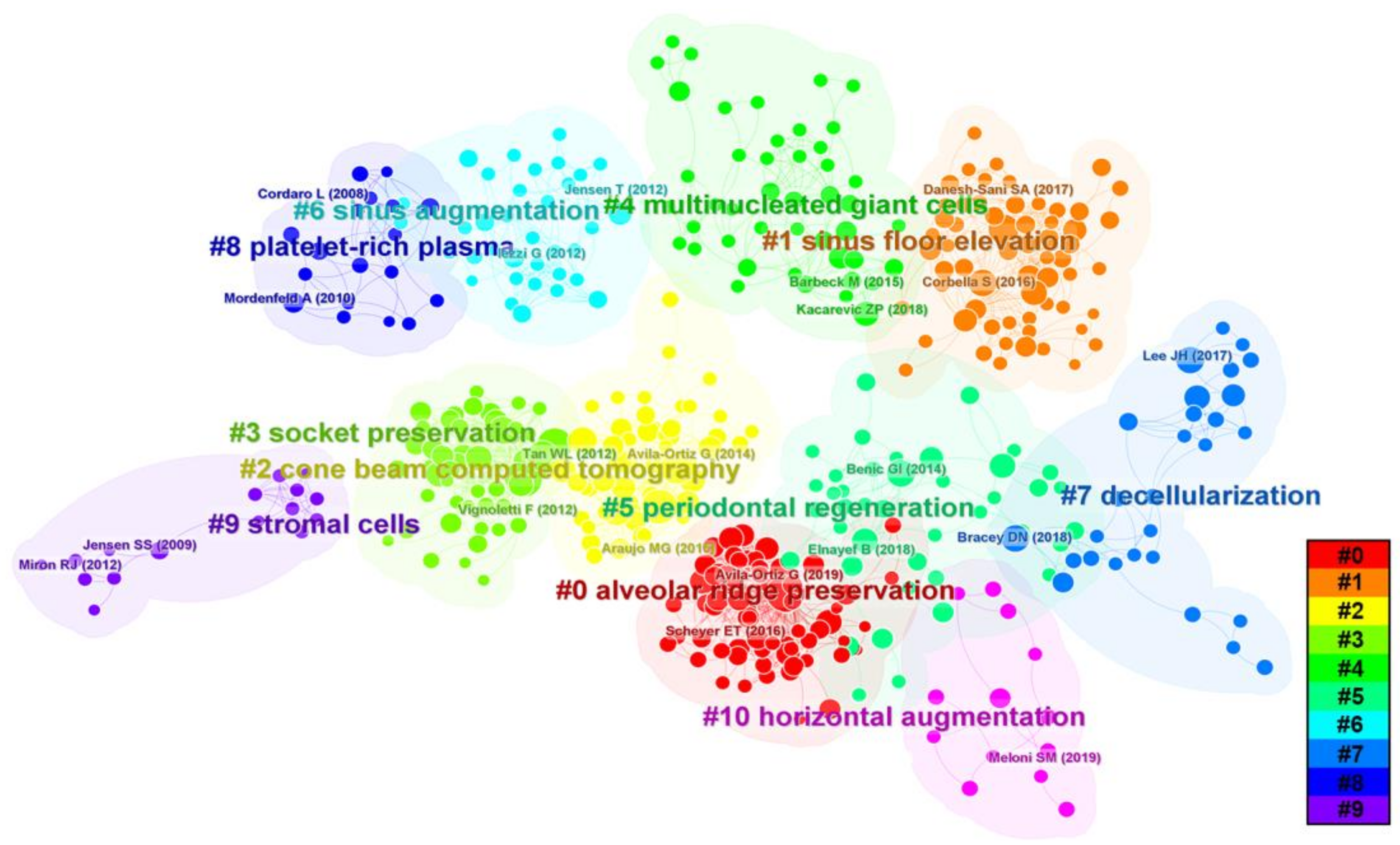
3.5. Analysis of Reference Burstiness and Clusters
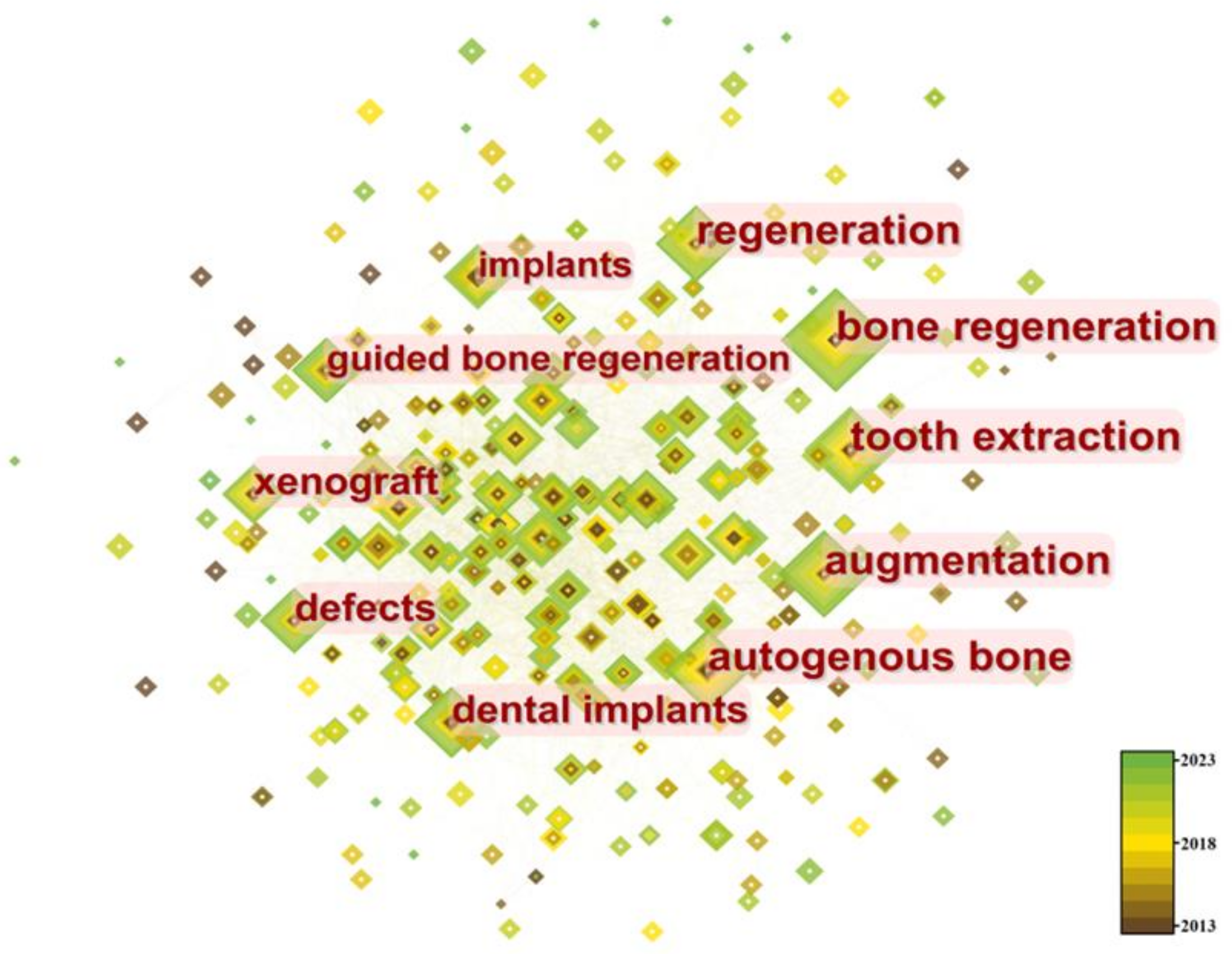
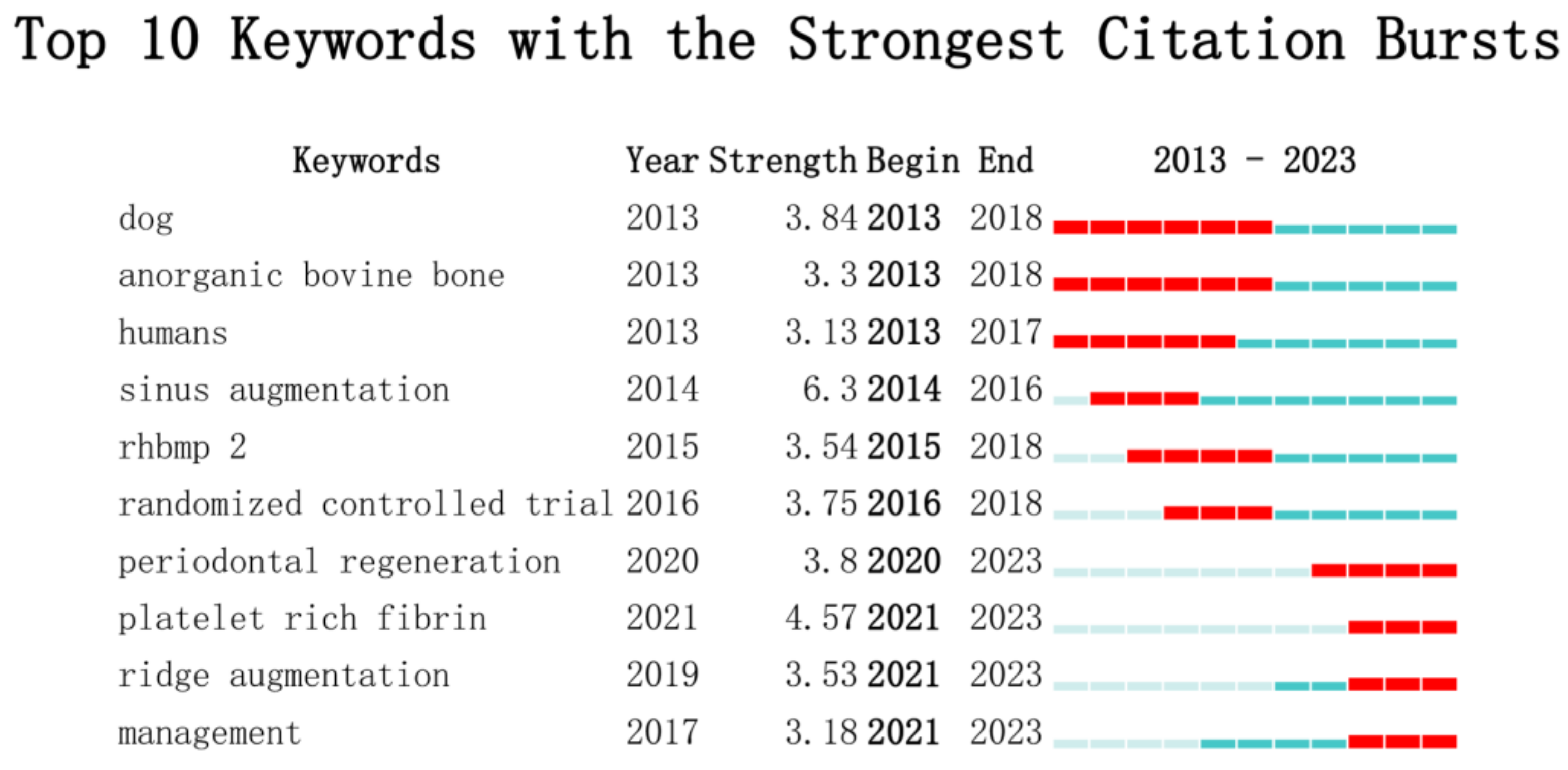
3.6. Analysis of Keyword Burstiness and Clusters
4. Discussion
4.1. Global Research Status of Bone Xenograft
4.2. Analysis of Hotspots and Trends in Bone Xenograft
4.3. Advantages and Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| WoS | web of science |
| WoSCC | web of science core collection |
| ARP | alveolar ridge preservation |
| MSFE | maxillary sinus floor elevation |
| PRF | platelet rich fibrin |
| MGCs | multinucleated giant cells |
| CBCT | cone beam computer tomography |
| 3D | three-dimensional |
| ECM | extracellular matrix |
| MSCs | Mesenchymal stem cells |
References
- Schlickewei, C.W.; Kleinertz, H.; Thiesen, D.M.; Mader, K.; Priemel, M.; Frosch, K.H.; Keller, J. Current and Future Concepts for the Treatment of Impaired Fracture Healing. Int. J. Mol. Sci. 2019, 20, 5805. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tang, D.; Tare, R.S.; Yang, L.Y.; Williams, D.F.; Ou, K.L.; Oreffo, R.O. Biofabrication of bone tissue: Approaches, challenges and translation for bone regeneration. Biomaterials 2016, 83, 363–382. [Google Scholar] [CrossRef] [PubMed]
- Minervini, G.; Franco, R.; Marrapodi, M.M.; di Blasio, M.; Isola, G.; Cicciu, M. Conservative treatment of temporomandibular joint condylar fractures: A systematic review conducted according to PRISMA guidelines and the Cochrane Handbook for Systematic Reviews of Interventions. J. Oral Rehabil. 2023. ahead of print. [Google Scholar] [CrossRef] [PubMed]
- Dec, P.; Modrzejewski, A.; Pawlik, A. Existing and Novel Biomaterials for Bone Tissue Engineering. Int. J. Mol. Sci. 2022, 24, 529. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Q.; Xiao, L.; Xiao, Y. Porous Nanomaterials Targeting Autophagy in Bone Regeneration. Pharmaceutics 2021, 13, 1572. [Google Scholar] [CrossRef]
- Tan, B.; Tang, Q.; Zhong, Y.; Wei, Y.; He, L.; Wu, Y.; Wu, J.; Liao, J. Biomaterial-based strategies for maxillofacial tumour therapy and bone defect regeneration. Int. J. Oral Sci. 2021, 13, 9. [Google Scholar] [CrossRef]
- Zhang, Q.; Xin, M.; Yang, S.; Wu, Q.; Xiang, X.; Wang, T.; Zhong, W.; Helder, M.N.; Jaspers, R.T.; Pathak, J.L.; et al. Silica nanocarrier-mediated intracellular delivery of rapamycin promotes autophagy-mediated M2 macrophage polarization to regulate bone regeneration. Mater. Today Bio 2023, 20, 100623. [Google Scholar] [CrossRef]
- Schmidt, A.H. Autologous bone graft: Is it still the gold standard? Injury 2021, 52 (Suppl. S2), S18–S22. [Google Scholar] [CrossRef] [PubMed]
- Artas, G.; Gul, M.; Acikan, I.; Kirtay, M.; Bozoglan, A.; Simsek, S.; Yaman, F.; Dundar, S. A comparison of different bone graft materials in peri-implant guided bone regeneration. Braz. Oral Res. 2018, 32, e59. [Google Scholar] [CrossRef] [PubMed]
- Canullo, L.; del Fabbro, M.; Khijmatgar, S.; Panda, S.; Ravida, A.; Tommasato, G.; Sculean, A.; Pesce, P. Dimensional and histomorphometric evaluation of biomaterials used for alveolar ridge preservation: A systematic review and network meta-analysis. Clin. Oral Investig. 2022, 26, 141–158. [Google Scholar] [CrossRef] [PubMed]
- Ninkov, A.; Frank, J.R.; Maggio, L.A. Bibliometrics: Methods for studying academic publishing. Perspect. Med. Educ. 2022, 11, 173–176. [Google Scholar] [CrossRef] [PubMed]
- Thompson, D.F.; Walker, C.K. A descriptive and historical review of bibliometrics with applications to medical sciences. Pharmacotherapy 2015, 35, 551–559. [Google Scholar] [CrossRef]
- Barbeck, M.; Udeabor, S.; Lorenz, J.; Schlee, M.; Holthaus, M.G.; Raetscho, N.; Choukroun, J.; Sader, R.; Kirkpatrick, C.J.; Ghanaati, S. High-Temperature Sintering of Xenogeneic Bone Substitutes Leads to Increased Multinucleated Giant Cell Formation: In Vivo and Preliminary Clinical Results. J. Oral Implantol. 2015, 41, e212–e222. [Google Scholar] [CrossRef] [PubMed]
- Pizzicannella, J.; Cavalcanti, M.; Trubiani, O.; Diomede, F. MicroRNA 210 Mediates VEGF Upregulation in Human Periodontal Ligament Stem Cells Cultured on 3D Hydroxyapatite Ceramic Scaffold. Int. J. Mol. Sci. 2018, 19, 3916. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zhang, J.Y.; Liu, K.; Liu, R.X.; Xu, B.H. Safety and Efficacy of Midface Augmentation Using Bio-Oss Bone Powder and Bio-Gide Collagen Membrane in Asians. J. Clin. Med. 2023, 12, 959. [Google Scholar] [CrossRef]
- Galindo-Moreno, P.; Martin-Morales, N.; Olaechea, A.; Hernandez-Cortes, P.; Verdugo-Escamilla, C.; Martinez-Ruiz, F.; Carrillo-Galvez, A.B.; O’Valle, F.; Padial-Molina, M. Physico-chemical and biological characterization of a new bovine bone mineral matrix available for human usage. Clin. Implant. Dent. Relat. Res. 2023, 25, 370–380. [Google Scholar] [CrossRef] [PubMed]
- Araujo, M.G.; Lindhe, J. Dimensional ridge alterations following tooth extraction. An experimental study in the dog. J. Clin. Periodontol. 2005, 32, 212–218. [Google Scholar] [CrossRef]
- Tarnow, D.; Elian, N.; Fletcher, P.; Froum, S.; Magner, A.; Cho, S.C.; Salama, M.; Salama, H.; Garber, D.A. Vertical distance from the crest of bone to the height of the interproximal papilla between adjacent implants. J. Periodontol. 2003, 74, 1785–1788. [Google Scholar] [CrossRef] [Green Version]
- Avila-Ortiz, G.; Elangovan, S.; Kramer, K.W.; Blanchette, D.; Dawson, D.V. Effect of alveolar ridge preservation after tooth extraction: A systematic review and meta-analysis. J. Dent. Res. 2014, 93, 950–958. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Favero, V.; Lang, N.P.; Canullo, L.; Urbizo Velez, J.; Bengazi, F.; Botticelli, D. Sinus floor elevation outcomes following perforation of the Schneiderian membrane. An experimental study in sheep. Clin. Oral Implant. Res. 2016, 27, 233–240. [Google Scholar] [CrossRef]
- Fienitz, T.; Moses, O.; Klemm, C.; Happe, A.; Ferrari, D.; Kreppel, M.; Ormianer, Z.; Gal, M.; Rothamel, D. Histological and radiological evaluation of sintered and non-sintered deproteinized bovine bone substitute materials in sinus augmentation procedures. A prospective, randomized-controlled, clinical multicenter study. Clin. Oral Investig. 2017, 21, 787–794. [Google Scholar] [CrossRef]
- Vignoletti, F.; Matesanz, P.; Rodrigo, D.; Figuero, E.; Martin, C.; Sanz, M. Surgical protocols for ridge preservation after tooth extraction. A systematic review. Clin. Oral Implant. Res. 2012, 23 (Suppl. S5), 22–38. [Google Scholar] [CrossRef] [PubMed]
- Horvath, A.; Mardas, N.; Mezzomo, L.A.; Needleman, I.G.; Donos, N. Alveolar ridge preservation. A systematic review. Clin. Oral Investig. 2013, 17, 341–363. [Google Scholar] [CrossRef] [PubMed]
- Jung, R.E.; Philipp, A.; Annen, B.M.; Signorelli, L.; Thoma, D.S.; Hammerle, C.H.; Attin, T.; Schmidlin, P. Radiographic evaluation of different techniques for ridge preservation after tooth extraction: A randomized controlled clinical trial. J. Clin. Periodontol. 2013, 40, 90–98. [Google Scholar] [CrossRef] [PubMed]
- Avila-Ortiz, G.; Chambrone, L.; Vignoletti, F. Effect of alveolar ridge preservation interventions following tooth extraction: A systematic review and meta-analysis. J. Clin. Periodontol. 2019, 46 (Suppl. S21), 195–223. [Google Scholar] [CrossRef] [Green Version]
- Tan, W.L.; Wong, T.L.; Wong, M.C.; Lang, N.P. A systematic review of post-extractional alveolar hard and soft tissue dimensional changes in humans. Clin. Oral. Implant. Res. 2012, 23 (Suppl. S5), 1–21. [Google Scholar] [CrossRef]
- Pelegrine, A.A.; da Costa, C.E.; Correa, M.E.; Marques, J.F., Jr. Clinical and histomorphometric evaluation of extraction sockets treated with an autologous bone marrow graft. Clin. Oral Implants Res. 2010, 21, 535–542. [Google Scholar] [CrossRef]
- Wood, R.A.; Mealey, B.L. Histologic comparison of healing after tooth extraction with ridge preservation using mineralized versus demineralized freeze-dried bone allograft. J. Periodontol. 2012, 83, 329–336. [Google Scholar] [CrossRef]
- Mardas, N.; Chadha, V.; Donos, N. Alveolar ridge preservation with guided bone regeneration and a synthetic bone substitute or a bovine-derived xenograft: A randomized, controlled clinical trial. Clin. Oral Implants Res. 2010, 21, 688–698. [Google Scholar] [CrossRef]
- Haugen, H.J.; Lyngstadaas, S.P.; Rossi, F.; Perale, G. Bone grafts: Which is the ideal biomaterial? J. Clin. Periodontol. 2019, 46 (Suppl. S21), 92–102. [Google Scholar] [CrossRef]
- Zhao, R.; Yang, R.; Cooper, P.R.; Khurshid, Z.; Shavandi, A.; Ratnayake, J. Bone Grafts and Substitutes in Dentistry: A Review of Current Trends and Developments. Molecules 2021, 26, 3007. [Google Scholar] [CrossRef]
- Ratnayake, J.T.B.; Mucalo, M.; Dias, G.J. Substituted hydroxyapatites for bone regeneration: A review of current trends. J. Biomed. Mater. Res. B Appl. Biomater. 2017, 105, 1285–1299. [Google Scholar] [CrossRef]
- Lin, H.; Wang, X.; Huang, M.; Li, Z.; Shen, Z.; Feng, J.; Chen, H.; Wu, J.; Gao, J.; Wen, Z.; et al. Research hotspots and trends of bone defects based on Web of Science: A bibliometric analysis. J. Orthop. Surg. Res. 2020, 15, 463. [Google Scholar] [CrossRef] [PubMed]
- Bracey, D.N.; Cignetti, N.E.; Jinnah, A.H.; Stone, A.V.; Gyr, B.M.; Whitlock, P.W.; Scott, A.T. Bone xenotransplantation: A review of the history, orthopedic clinical literature, and a single-center case series. Xenotransplantation 2020, 27, e12600. [Google Scholar] [CrossRef] [PubMed]
- Kim, H.J.; Chung, J.H.; Shin, S.Y.; Shin, S.I.; Kye, S.B.; Kim, N.K.; Kwon, T.G.; Paeng, J.Y.; Kim, J.W.; Oh, O.H.; et al. Efficacy of rhBMP-2/Hydroxyapatite on Sinus Floor Augmentation: A Multicenter, Randomized Controlled Clinical Trial. J. Dent. Res. 2015, 94 (Suppl. S9), 158S–165S. [Google Scholar] [CrossRef] [PubMed]
- Bow, A.; Anderson, D.E.; Dhar, M. Commercially available bone graft substitutes: The impact of origin and processing on graft functionality. Drug Metab. Rev. 2019, 51, 533–544. [Google Scholar] [CrossRef] [PubMed]
- Lai, V.J.; Michalek, J.E.; Liu, Q.Q.; Mealey, B.L. Ridge preservation following tooth extraction using bovine xenograft compared with porcine xenograft: A randomized controlled clinical trial. J. Periodontol. 2020, 91, 361–368. [Google Scholar] [CrossRef]
- Dos Santos, F.R.; Minto, B.W.; da Silva, S.W.G.; Coelho, L.D.; Rossignoli, P.P.; Costa, J.S.; Taba, M.; Dias, L.G.G.G. Caprine demineralized bone matrix (DBMc) in the repair of non-critical bone defects in rabbit tibias. A new bone xenograft. Acta Cir. Bras. 2020, 35, e202000801. [Google Scholar] [CrossRef] [PubMed]
- Gashtasbi, F.; Hasannia, S.; Hasannia, S.; Mahdi Dehghan, M.; Sarkarat, F.; Shali, A. Comparative study of impact of animal source on physical, structural, and biological properties of bone xenograft. Xenotransplantation 2020, 27, e12628. [Google Scholar] [CrossRef]
- Cardaropoli, D.; Tamagnone, L.; Roffredo, A.; Gaveglio, L.; Cardaropoli, G. Socket preservation using bovine bone mineral and collagen membrane: A randomized controlled clinical trial with histologic analysis. Int. J. Periodontics Restor. Dent. 2012, 32, 421–430. [Google Scholar]
- Tawil, G.; Barbeck, M.; Unger, R.; Tawil, P.; Witte, F. Sinus Floor Elevation Using the Lateral Approach and Window Repositioning and a Xenogeneic Bone Substitute as a Grafting Material: A Histologic, Histomorphometric, and Radiographic Analysis. Int. J. Oral Maxillofac. Implant. 2018, 33, 1089–1096. [Google Scholar] [CrossRef] [PubMed]
- Cook, D.C.; Mealey, B.L. Histologic comparison of healing following tooth extraction with ridge preservation using two different xenograft protocols. J. Periodontol. 2013, 84, 585–594. [Google Scholar] [CrossRef] [PubMed]
- Leventis, M.; Fairbairn, P.; Mangham, C.; Galanos, A.; Vasiliadis, O.; Papavasileiou, D.; Horowitz, R. Bone Healing in Rabbit Calvaria Defects Using a Synthetic Bone Substitute: A Histological and Micro-CT Comparative Study. Materials 2018, 11, 2004. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Scheyer, E.T.; Heard, R.; Janakievski, J.; Mandelaris, G.; Nevins, M.L.; Pickering, S.R.; Richardson, C.R.; Pope, B.; Toback, G.; Velasquez, D.; et al. A randomized, controlled, multicentre clinical trial of post-extraction alveolar ridge preservation. J. Clin. Periodontol. 2016, 43, 1188–1199. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tovar, N.; Jimbo, R.; Gangolli, R.; Perez, L.; Manne, L.; Yoo, D.; Lorenzoni, F.; Witek, L.; Coelho, P.G. Evaluation of bone response to various anorganic bovine bone xenografts: An experimental calvaria defect study. Int. J. Oral Maxillofac. Surg. 2014, 43, 251–260. [Google Scholar] [CrossRef] [PubMed]
- Dos Anjos, T.L.; de Molon, R.S.; Paim, P.R.; Marcantonio, E.; Marcantonio, E., Jr.; Faeda, R.S. Implant stability after sinus floor augmentation with deproteinized bovine bone mineral particles of different sizes: A prospective, randomized and controlled split-mouth clinical trial. Int. J. Oral Maxillofac. Surg. 2016, 45, 1556–1563. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yang, S.; Lan, L.; Miron, R.J.; Wei, L.; Zhang, M.; Zhang, Y. Variability in Particle Degradation of Four Commonly Employed Dental Bone Grafts. Clin. Implant. Dent. Relat. Res. 2015, 17, 996–1003. [Google Scholar] [CrossRef]
- Djordjevic, F.; Mihailovic, B.; Mladenovic, R.; Dubovina, D.; Kostic, M.; Stanisic, J.; Vlahovic, Z. CBCT analysis of bone density in bicortical defects after augmentation with alloplastic and xenogeneic bone substitutes—A study on domestic pigs. Vojnosanit. Pregl. 2021, 78, 1200–1206. [Google Scholar] [CrossRef] [Green Version]
- Kotsakis, G.A.; Salama, M.; Chrepa, V.; Hinrichs, J.E.; Gaillard, P. A Randomized, Blinded, Controlled Clinical Study of Particulate Anorganic Bovine Bone Mineral and Calcium Phosphosilicate Putty Bone Substitutes for Socket Preservation. Int. J. Oral Max Impl. 2014, 29, 141–151. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mendoza-Azpur, G.; de la Fuente, A.; Chavez, E.; Valdivia, E.; Khouly, I. Horizontal ridge augmentation with guided bone regeneration using particulate xenogenic bone substitutes with or without autogenous block grafts: A randomized controlled trial. Clin. Implant. Dent. Relat. Res. 2019, 21, 521–530. [Google Scholar] [CrossRef] [PubMed]
- Alayan, J.; Ivanovski, S. A prospective controlled trial comparing xenograft/autogenous bone and collagen-stabilized xenograft for maxillary sinus augmentation-Complications, patient-reported outcomes and volumetric analysis. Clin. Oral Implant. Res. 2018, 29, 248–262. [Google Scholar] [CrossRef] [PubMed]
- Barbeck, M.; Booms, P.; Unger, R.; Hoffmann, V.; Sader, R.; Kirkpatrick, C.J.; Ghanaati, S. Multinucleated giant cells in the implant bed of bone substitutes are foreign body giant cells-New insights into the material-mediated healing process. J. Biomed. Mater. Res. A 2017, 105, 1105–1111. [Google Scholar] [CrossRef]
- Peric Kacarevic, Z.; Kavehei, F.; Houshmand, A.; Franke, J.; Smeets, R.; Rimashevskiy, D.; Wenisch, S.; Schnettler, R.; Jung, O.; Barbeck, M. Purification processes of xenogeneic bone substitutes and their impact on tissue reactions and regeneration. Int. J. Artif. Organs 2018, 41, 789–800. [Google Scholar] [CrossRef]
- Neishabouri, A.; Soltani Khaboushan, A.; Daghigh, F.; Kajbafzadeh, A.M.; Majidi Zolbin, M. Decellularization in Tissue Engineering and Regenerative Medicine: Evaluation, Modification, and Application Methods. Front. Bioeng. Biotechnol. 2022, 10, 805299. [Google Scholar] [CrossRef]
- Zhang, Y.; Wu, D.; Zhao, X.; Pakvasa, M.; Tucker, A.B.; Luo, H.; Qin, K.H.; Hu, D.A.; Wang, E.J.; Li, A.J.; et al. Stem Cell-Friendly Scaffold Biomaterials: Applications for Bone Tissue Engineering and Regenerative Medicine. Front. Bioeng. Biotechnol. 2020, 8, 598607. [Google Scholar] [CrossRef] [PubMed]
- Pan, Q.X.; Gao, C.Y.; Wang, Y.Y.; Wang, Y.L.; Mao, C.; Wang, Q.; Economidou, S.N.; Douroumis, D.; Wen, F.; Tan, L.P.; et al. Investigation of bone reconstruction using an attenuated immunogenicity xenogenic composite scaffold fabricated by 3D printing. Bio-Des. Manuf. 2020, 3, 396–409. [Google Scholar] [CrossRef]
- Bracey, D.N.; Seyler, T.M.; Jinnah, A.H.; Smith, T.L.; Ornelles, D.A.; Deora, R.; Parks, G.D.; van Dyke, M.E.; Whitlock, P.W. A porcine xenograft-derived bone scaffold is a biocompatible bone graft substitute: An assessment of cytocompatibility and the alpha-Gal epitope. Xenotransplantation 2019, 26, e12534. [Google Scholar] [CrossRef] [PubMed]
- Bracey, D.N.; Seyler, T.M.; Jinnah, A.H.; Lively, M.O.; Willey, J.S.; Smith, T.L.; van Dyke, M.E.; Whitlock, P.W. A Decellularized Porcine Xenograft-Derived Bone Scaffold for Clinical Use as a Bone Graft Substitute: A Critical Evaluation of Processing and Structure. J. Funct. Biomater. 2018, 9, 45. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chen, Y.W.; Chen, M.Y.; Hsieh, D.J.; Periasamy, S.; Yen, K.C.; Chuang, C.T.; Wang, H.C.; Tseng, F.W.; Kuo, J.C.; Chien, H.H. Evaluating the bone-regenerative role of the decellularized porcine bone xenograft in a canine extraction socket model. Clin. Exp. Dent. Res. 2021, 7, 409–418. [Google Scholar] [CrossRef] [PubMed]
- Zhang, X.; Chen, X.; Hong, H.; Hu, R.; Liu, J.; Liu, C. Decellularized extracellular matrix scaffolds: Recent trends and emerging strategies in tissue engineering. Bioact. Mater. 2022, 10, 15–31. [Google Scholar] [CrossRef]
- Amirazad, H.; Dadashpour, M.; Zarghami, N. Application of decellularized bone matrix as a bioscaffold in bone tissue engineering. J. Biol. Eng. 2022, 16, 1. [Google Scholar] [CrossRef] [PubMed]
- Zheng, C.; Chen, J.; Liu, S.; Jin, Y. Stem cell-based bone and dental regeneration: A view of microenvironmental modulation. Int J. Oral Sci. 2019, 11, 23. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zimmermann, A.; Pelegrine, A.A.; Peruzzo, D.; Martinez, E.F.; Oliveira, R.D.E.; Aloise, A.C.; Ferreira, L.M. Adipose Mesenchymal Stem Cells Associated with Xenograft in a Guided Bone Regeneration Model: A Histomorphometric Study in Rabbit Calvaria. Int. J. Oral Max Impl. 2015, 30, 1415–1422. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Calori, G.M.; Mazza, E.; Colombo, M.; Mazzola, S.; Mineo, G.V.; Giannoudis, P.V. Treatment of AVN using the induction chamber technique and a biological-based approach: Indications and clinical results. Injury 2014, 45, 369–373. [Google Scholar] [CrossRef]
- Kloss, F.R.; Kammerer, P.W.; Kloss-Brandstatter, A. Risk Factors for Complications Following Staged Alveolar Ridge Augmentation and Dental Implantation: A Retrospective Evaluation of 151 Cases with Allogeneic and 70 Cases with Autogenous Bone Blocks. J. Clin. Med. 2023, 12, 6. [Google Scholar] [CrossRef] [PubMed]
- McAllister, T.N.; Dusserre, N.; Maruszewski, M.; L’Heureux, N. Cell-based therapeutics from an economic perspective: Primed for a commercial success or a research sinkhole? Regen. Med. 2008, 3, 925–937. [Google Scholar] [CrossRef] [PubMed]
- Burdick, J.A.; Mauck, R.L.; Gorman, J.H., III; Gorman, R.C. Acellular biomaterials: An evolving alternative to cell-based therapies. Sci. Transl. Med. 2013, 5, 176ps174. [Google Scholar] [CrossRef] [Green Version]
- Jiang, S.; Wang, M.; He, J. A review of biomimetic scaffolds for bone regeneration: Toward a cell-free strategy. Bioeng. Transl. Med. 2021, 6, e10206. [Google Scholar] [CrossRef] [PubMed]
- Lekovic, V.; Milinkovic, I.; Aleksic, Z.; Jankovic, S.; Stankovic, P.; Kenney, E.B.; Camargo, P.M. Platelet-rich fibrin and bovine porous bone mineral vs. platelet-rich fibrin in the treatment of intrabony periodontal defects. J. Periodontal. Res. 2012, 47, 409–417. [Google Scholar] [CrossRef] [PubMed]
- Yon, J.; Lee, J.S.; Lim, H.C.; Kim, M.S.; Hong, J.Y.; Choi, S.H.; Jung, U.W. Pre-clinical evaluation of the osteogenic potential of bone morphogenetic protein-2 loaded onto a particulate porcine bone biomaterial. J. Clin. Periodontol. 2015, 42, 81–88. [Google Scholar] [CrossRef]
- Kuroshima, S.; Al-Salihi, Z.; Yamashita, J. Parathyroid hormone related to bone regeneration in grafted and nongrafted tooth extraction sockets in rats. Implant Dent. 2013, 22, 71–76. [Google Scholar] [CrossRef] [PubMed]
- Bashara, H.; Wohlfahrt, J.C.; Polyzois, I.; Lyngstadaas, S.P.; Renvert, S.; Claffey, N. The effect of permanent grafting materials on the preservation of the buccal bone plate after tooth extraction: An experimental study in the dog. Clin. Oral Implant. Res. 2012, 23, 911–917. [Google Scholar] [CrossRef]
- Bienz, S.P.; Payer, M.; Hjerppe, J.; Husler, J.; Jakse, N.; Schmidlin, P.R.; Hammerle, C.H.F.; Jung, R.E.; Thoma, D.S. Primary bone augmentation leads to equally stable marginal tissue conditions comparing the use of xenograft blocks infused with BMP-2 and autogenous bone blocks: A 3D analysis after 3 years. Clin. Oral Implant. Res. 2021, 32, 1433–1443. [Google Scholar] [CrossRef] [PubMed]
- Lim, H.C.; Paeng, K.W.; Jung, U.W.; Benic, G.I. Effectiveness of xenogeneic and synthetic bone-block substitute materials with/without recombinant human bone morphogenetic protein-2: A preclinical study using a rabbit calvarium model. J. Clin. Periodontol. 2021, 48, 1126–1136. [Google Scholar] [CrossRef]
- Song, J.Y.; Kim, S.G.; Park, N.R.; Choi, J.Y. Porcine Bone Incorporated with 4-Hexylresorcinol Increases New Bone Formation by Suppression of the Nuclear Factor Kappa B Signaling Pathway. J. Craniofac. Surg. 2018, 29, 1983–1990. [Google Scholar] [CrossRef]
- Dohan, D.M.; Choukroun, J.; Diss, A.; Dohan, S.L.; Dohan, A.J.; Mouhyi, J.; Gogly, B. Platelet-rich fibrin (PRF): A second-generation platelet concentrate. Part I: Technological concepts and evolution. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 2006, 101, e37–e44. [Google Scholar] [CrossRef] [PubMed]
- Dos Santos, R.F.; Araujo Peres, J.A.; Queiroz, M.S. Advances in separation methods for the use of platelet-rich fibrin in tissue repair: An integrative review. Gen. Dent. 2023, 71, 65–69. [Google Scholar] [PubMed]
- Yashwant, V.A.; Balu, P.; Kumar, R.S.; Ammayappan, P.; Murugaboopathy, V. Effectiveness of platelet rich fibrin versus demineralized bone xenograft in periodontally accelerated osteogenic orthodontics. Angle Orthod. 2022, 92, 180–188. [Google Scholar] [CrossRef] [PubMed]
- Carames, J.M.M.; Vieira, F.A.; Carames, G.B.; Pinto, A.C.; Francisco, H.C.O.; Marques, D. Guided Bone Regeneration in the Edentulous Atrophic Maxilla Using Deproteinized Bovine Bone Mineral (DBBM) Combined with Platelet-Rich Fibrin (PRF)-A Prospective Study. J. Clin. Med. 2022, 11, 894. [Google Scholar] [CrossRef] [PubMed]
- Tavelli, L.; Chen, C.J.; Barootchi, S.; Kim, D.M. Efficacy of biologics for the treatment of periodontal infrabony defects: An American Academy of Periodontology best evidence systematic review and network meta-analysis. J. Periodontol. 2022, 93, 1803–1826. [Google Scholar] [CrossRef] [PubMed]
- Dohle, E.; El Bagdadi, K.; Sader, R.; Choukroun, J.; James Kirkpatrick, C.; Ghanaati, S. Platelet-rich fibrin-based matrices to improve angiogenesis in an in vitro co-culture model for bone tissue engineering. J. Tissue Eng. Regen. Med. 2018, 12, 598–610. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chandra, R.V.; Vaishnavi, V.; YSH, S.C. Regenerative Capacity of Leukocyte-rich and Platelet-rich Fibrin in Indirect Sinus Elevation Procedure May be Dependent on Model-Specific Modification of the Centrifugation Cycle. Contemp. Clin. Dent. 2019, 10, 433–439. [Google Scholar] [CrossRef] [PubMed]
- Fujioka-Kobayashi, M.; Kono, M.; Katagiri, H.; Schaller, B.; Zhang, Y.; Sculean, A.; Miron, R.J. Histological comparison of Platelet rich fibrin clots prepared by fixed-angle versus horizontal centrifugation. Platelets 2021, 32, 413–419. [Google Scholar] [CrossRef] [PubMed]
- Dohan Ehrenfest, D.M.; Pinto, N.R.; Pereda, A.; Jimenez, P.; Corso, M.D.; Kang, B.S.; Nally, M.; Lanata, N.; Wang, H.L.; Quirynen, M. The impact of the centrifuge characteristics and centrifugation protocols on the cells, growth factors, and fibrin architecture of a leukocyte- and platelet-rich fibrin (L-PRF) clot and membrane. Platelets 2018, 29, 171–184. [Google Scholar] [CrossRef] [PubMed]



Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Li, J.; Zhao, Y.; Chen, S.; Wang, S.; Zhong, W.; Zhang, Q. Research Hotspots and Trends of Bone Xenograft in Clinical Procedures: A Bibliometric and Visual Analysis of the Past Decade. Bioengineering 2023, 10, 929. https://doi.org/10.3390/bioengineering10080929
Li J, Zhao Y, Chen S, Wang S, Zhong W, Zhang Q. Research Hotspots and Trends of Bone Xenograft in Clinical Procedures: A Bibliometric and Visual Analysis of the Past Decade. Bioengineering. 2023; 10(8):929. https://doi.org/10.3390/bioengineering10080929
Chicago/Turabian StyleLi, Jiayue, Yujue Zhao, Shili Chen, Simin Wang, Wen Zhong, and Qing Zhang. 2023. "Research Hotspots and Trends of Bone Xenograft in Clinical Procedures: A Bibliometric and Visual Analysis of the Past Decade" Bioengineering 10, no. 8: 929. https://doi.org/10.3390/bioengineering10080929





