Concurrent Validity of the Ergotex Device for Measuring Low Back Posture
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Instruments
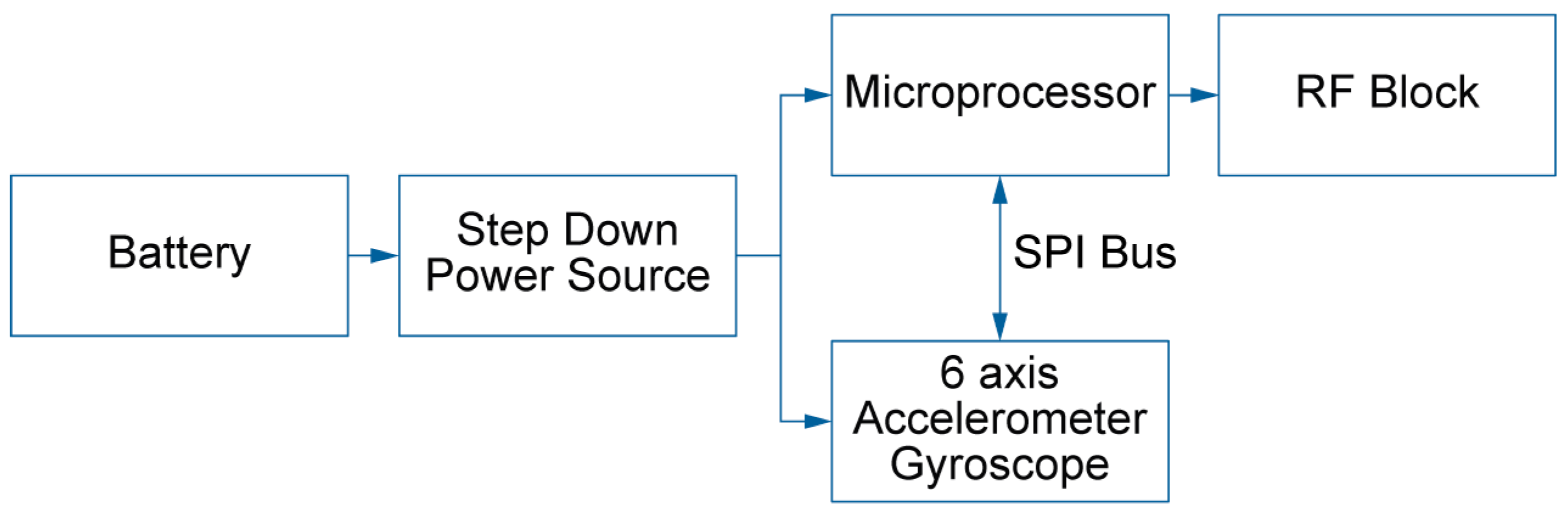
2.2.1. Ergotex
2.2.2. Optical Tracking System OptiTrack
2.3. Procedure
2.4. Participants
2.5. Statistical Analysis
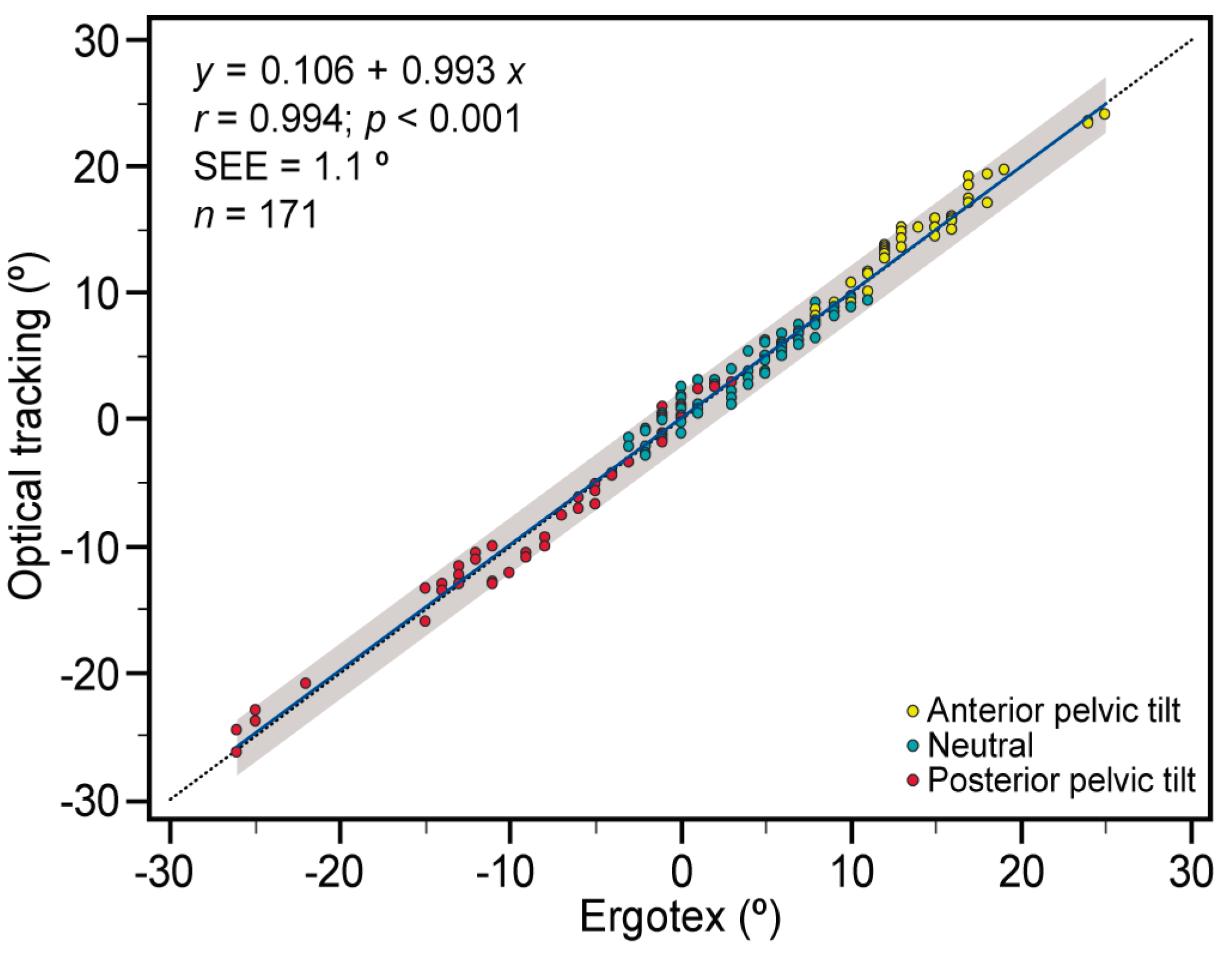
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Been, E.; Kalichman, L. Lumbar lordosis. Spine J. 2014, 14, 87–97. [Google Scholar] [CrossRef] [PubMed]
- Bailey, J.F.; Shefi, S.; Soudack, M.; Kramer, P.A.; Been, E. Development of pelvic incidence and lumbar lordosis in children and adolescents. Anat. Rec. 2019, 302, 2132–2139. [Google Scholar] [CrossRef] [PubMed]
- Roussouly, P.; Pinheiro-Franco, J.L. Sagittal parameters of the spine: Biomechanical approach. Eur. Spine J. 2011, 20, 578. [Google Scholar] [CrossRef] [PubMed]
- During, J.; Goudfrooij, H.; Keessen, W.; Beeker, T.W.; Crowe, A. Toward standards for posture: Postural characteristics of the lower back system in normal and pathologic conditions. Spine 1985, 10, 83–87. [Google Scholar] [CrossRef] [PubMed]
- Le Huec, J.; Aunoble, S.; Philippe, L.; Nicolas, P. Pelvic parameters: Origin and significance. Eur. Spine J. 2011, 20, 564–571. [Google Scholar] [CrossRef] [PubMed]
- Legaye, J.; Duval-Beaupere, G.; Hecquet, J.; Marty, C. Pelvic incidence: A fundamental pelvic parameter for three-dimensional regulation of spinal sagittal curves. Eur. Spine J. 1998, 7, 99–103. [Google Scholar] [CrossRef] [PubMed]
- Vaz, G.; Roussouly, P.; Berthonnaud, E.; Dimnet, J. Sagittal morphology and equilibrium of pelvis and spine. Eur. Spine J. 2002, 11, 80–87. [Google Scholar] [CrossRef]
- Levine, D.; Whittle, M.W. The effects of pelvic movement on lumbar lordosis in the standing position. J. Orthop. Sports Phys. Ther. 1996, 24, 130–135. [Google Scholar] [CrossRef]
- Keegan, J.J. Alterations of the lumbar curve related to posture and seating. J. Bone Jt. Surg. 1953, 35, 589–603. [Google Scholar] [CrossRef]
- Day, J.W.; Smidt, G.L.; Lehmann, T. Effect of pelvic tilt on standing posture. Phys. Ther. 1984, 64, 510–516. [Google Scholar] [CrossRef]
- Vrtovec, T.; Pernuš, F.; Likar, B. A review of methods for quantitative evaluation of spinal curvature. Eur. Spine J. 2009, 18, 593–607. [Google Scholar] [CrossRef] [PubMed]
- Mannion, A.F.; Knecht, K.; Balaban, G.; Dvorak, J.; Grob, D. A new skin-surface device for measuring the curvature and global and segmental ranges of motion of the spine: Reliability of measurements and comparison with data reviewed from the literature. Eur. Spine J. 2004, 13, 122–136. [Google Scholar] [CrossRef] [PubMed]
- Schmid, S.; Studer, D.; Hasler, C.; Romkes, J.; Taylor, W.R.; Lorenzetti, S.; Brunner, R. Quantifying spinal gait kinematics using an enhanced optical motion capture approach in adolescent idiopathic scoliosis. Gait Posture 2016, 44, 231–237. [Google Scholar] [CrossRef]
- Ranavolo, A.; Don, R.; Draicchio, F.; Bartolo, M.; Serrao, M.; Padua, L.; Cipolla, G.; Pierelli, F.; Iavicoli, S.; Sandrini, G. Modelling the spine as a deformable body: Feasibility of reconstruction using an optoelectronic system. Appl. Ergon. 2013, 44, 192–199. [Google Scholar] [CrossRef] [PubMed]
- Consmüller, T.; Rohlmann, A.; Weinland, D.; Druschel, C.; Duda, G.N.; Taylor, W.R. Comparative evaluation of a novel measurement tool to assess lumbar spine posture and range of motion. Eur. Spine J. 2012, 21, 2170–2180. [Google Scholar] [CrossRef]
- Taylor, W.R.; Consmüller, T.; Rohlmann, A. A novel system for the dynamic assessment of back shape. Med. Eng. Phys. 2010, 32, 1080–1083. [Google Scholar] [CrossRef] [PubMed]
- O’Sullivan, K.; O’Sullivan, L.; Campbell, A.; O’Sullivan, P.; Dankaerts, W. Towards monitoring lumbo-pelvic posture in real-life situations: Concurrent validity of a novel posture monitor and a traditional laboratory-based motion analysis system. Man. Ther. 2012, 17, 77–83. [Google Scholar] [CrossRef] [PubMed]
- Mieritz, R.M.; Bronfort, G.; Jakobsen, M.D.; Aagaard, P.; Hartvigsen, J. Reliability and measurement error of sagittal spinal motion parameters in 220 patients with chronic low back pain using a three-dimensional measurement device. Spine J. 2014, 14, 1835–1843. [Google Scholar] [CrossRef]
- Mitchell, T.; O’Sullivan, P.B.; Burnett, A.F.; Straker, L.; Smith, A. Regional differences in lumbar spinal posture and the influence of low back pain. BMC Musculoskelet. Disord. 2008, 9, 152. [Google Scholar] [CrossRef]
- Müller, R.; Ertelt, T.; Blickhan, R. Low back pain affects trunk as well as lower limb movements during walking and running. J. Biomech. 2015, 48, 1009–1014. [Google Scholar] [CrossRef]
- Rosário, J.L.P.d. Biomechanical assessment of human posture: A literature review. J. Bodyw. Mov. Ther. 2014, 18, 368–373. [Google Scholar] [CrossRef] [PubMed]
- Lehman, G.J. Biomechanical assessments of lumbar spinal function. how low back pain sufferers differ from normals. implications for outcome measures research. Part I: Kinematic assessments of lumbar function. J. Manip. Physiol. Ther. 2004, 27, 57–62. [Google Scholar] [CrossRef] [PubMed]
- Bierma-Zeinstra, S.M.; van Gool, J.J.; Bernsen, R.M.; Njoo, K.H. Measuring the sacral inclination angle in clinical practice: Is there an alternative to radiographs? J. Manip. Physiol. Ther. 2001, 24, 505–508. [Google Scholar] [CrossRef] [PubMed]
- Papi, E.; Koh, W.S.; McGregor, A.H. Wearable technology for spine movement assessment: A systematic review. J. Biomech. 2017, 64, 186–197. [Google Scholar] [CrossRef]
- Mayer, T.G.; Kondraske, G.; Beals, S.B.; Gatchel, R.J. Spinal range of motion: Accuracy and sources of error with in-clinometric measurement. Spine 1997, 22, 1976–1984. [Google Scholar] [CrossRef] [PubMed]
- Bonato, P. Wearable sensors and systems. IEEE Eng. Med. Biol. Mag. 2010, 29, 25–36. [Google Scholar] [CrossRef] [PubMed]
- de Oliveira, T.S.; Candotti, C.T.; La Torre, M.; Pelinson, P.P.T.; Furlanetto, T.S.; Kutchak, F.M.; Loss, J.F. Validity and reproducibility of the measurements obtained using the flexicurve instrument to evaluate the angles of thoracic and lumbar curvatures of the spine in the sagittal plane. Rehabil. Res. Pract. 2012, 2012, 186156. [Google Scholar] [CrossRef]
- Poitras, I.; Dupuis, F.; Bielmann, M.; Campeau-Lecours, A.; Mercier, C.; Bouyer, L.J.; Roy, J. Validity and reliability of wearable sensors for joint angle estimation: A systematic review. Sensors 2019, 19, 1555. [Google Scholar] [CrossRef]
- Shull, P.B.; Jirattigalachote, W.; Hunt, M.A.; Cutkosky, M.R.; Delp, S.L. Quantified self and human movement: A review on the clinical impact of wearable sensing and feedback for gait analysis and intervention. Gait Posture 2014, 40, 11–19. [Google Scholar] [CrossRef]
- Fong, D.T.; Chan, Y. The use of wearable inertial motion sensors in human lower limb biomechanics studies: A systematic review. Sensors 2010, 10, 11556–11565. [Google Scholar] [CrossRef]
- Simpson, L.; Maharaj, M.M.; Mobbs, R.J. The role of wearables in spinal posture analysis: A systematic review. BMC Musculoskelet. Disord. 2019, 20, 55. [Google Scholar] [CrossRef] [PubMed]
- Hodges, P.W.; van den Hoorn, W. A vision for the future of wearable sensors in spine care and its challenges: Narrative review. J. Spine Surg. 2022, 8, 103–116. [Google Scholar] [CrossRef] [PubMed]
- Vásquez-Ucho, P.A.; Villalba-Meneses, G.F.; Pila-Varela, K.O.; Villalba-Meneses, C.P.; Iglesias, I.; Almeida-Galárraga, D.A. Analysis and evaluation of the systems used for the assessment of the cervical spine function: A systematic review. J. Med. Eng. Technol. 2021, 45, 380–393. [Google Scholar] [CrossRef] [PubMed]
- Walmsley, C.P.; Williams, S.A.; Grisbrook, T.; Elliott, C.; Imms, C.; Campbell, A. Measurement of upper limb range of motion using wearable sensors: A systematic review. Sports Med. Open 2018, 4, 53. [Google Scholar] [CrossRef] [PubMed]
- Cuesta-Vargas, A.I.; Galán-Mercant, A.; Williams, J.M. The use of inertial sensors system for human motion analysis. Phys. Ther. Rev. 2010, 15, 462–473. [Google Scholar] [CrossRef] [PubMed]
- Picerno, P. 25 years of lower limb joint kinematics by using inertial and magnetic sensors: A review of methodolog-ical approaches. Gait Posture 2017, 51, 239–246. [Google Scholar] [CrossRef] [PubMed]
- Ismail, I.; Narayanan, A.L.T.; Wicaksono, D.H.B. Comparison of two sagittal pelvic tilt measurement protocols using newly calibrated novel pelvic sensor. In Proceedings of the 2011 2nd International Conference on Instrumentation Control and Automation, Bandung, Indonesia, 15–17 November 2011; pp. 184–187. [Google Scholar] [CrossRef]
- Bolink, S.A.A.N.; Naisas, H.; Senden, R.; Essers, H.; Heyligers, I.C.; Meijer, K.; Grimm, B. Validity of an inertial measurement unit to assess pelvic orientation angles during gait, sit–stand transfers and step-up transfers: Comparison with an optoelectronic motion capture system*. Med. Eng. Phys. 2016, 38, 225–231. [Google Scholar] [CrossRef]
- Beange, K.H.E.; Chan, A.D.C.; Beaudette, S.M.; Graham, R.B. Concurrent validity of a wearable IMU for objective assessments of functional movement quality and control of the lumbar spine. J. Biomech. 2019, 97, 109356. [Google Scholar] [CrossRef]
- Shin, S.; Yoo, W. Inertial Measurement unit-based evaluation of global and regional lumbar spine and pelvis alignment in standing individuals with a flat lumbar posture. J. Manip. Physiol. Ther. 2019, 42, 594–600. [Google Scholar] [CrossRef]
- Wang, X.; Qureshi, A.; Vepa, A.; Rahman, U.; Palit, A.; Williams, M.A.; King, R.; Elliott, M.T. A sensor-based screening tool for identifying high pelvic mobility in patients due to undergo total hip arthroplasty. Sensors 2020, 20, 6182. [Google Scholar] [CrossRef]
- Vayalapra, S.; Wang, X.; Qureshi, A.; Vepa, A.; Rahman, U.; Palit, A.; Williams, M.A.; King, R.; Elliott, M.T. Repeatability of inertial measurement units for measuring pelvic mobility in patients undergoing total hip arthroplasty. Sensors 2022, 23, 377. [Google Scholar] [CrossRef] [PubMed]
- Perpiñá-Martínez, S.; Arguisuelas-Martínez, M.D.; Pérez-Domínguez, B.; Nacher-Moltó, I.; Martínez-Gramage, J. Differences between sexes and speed levels in pelvic 3D kinematic patterns during running using an inertial measurement unit (IMU). Int. J. Environ. Res. Public Health 2023, 20, 3631. [Google Scholar] [CrossRef] [PubMed]
- Buganè, F.; Benedetti, M.G.; D’Angeli, V.; Leardini, A. Estimation of pelvis kinematics in level walking based on a single inertial sensor positioned close to the sacrum: Validation on healthy subjects with stereophotogrammetric system. Biomed. Eng. Online 2014, 13, 146. [Google Scholar] [CrossRef] [PubMed]
- Lee, C.; Ahn, J.; Lee, B. A systematic review of the long-term effects of using smartphone-and tablet-based rehabilitation technology for balance and gait training and exercise programs. Bioengineering 2023, 10, 1142. [Google Scholar] [CrossRef]
- Cortell-Tormo, J.; Garcia-Jaen, M.; Ruiz-Fernandez, D.; Fuster-Lloret, V. Lumbatex: A wearable monitoring system based on inertial sensors to measure and control the lumbar spine motion. IEEE Trans. Neural Syst. Rehabil. Eng. A Publ. IEEE Eng. Med. Biol. Soc. 2019, 27, 1644–1653. [Google Scholar] [CrossRef]
- Ramey, L.; Osborne, C.; Kasitinon, D.; Juengst, S. Apps and mobile health technology in rehabilitation: The good, the bad, and the unknown. Phys. Med. Rehabil. Clin. N. Am. 2019, 30, 485–497. [Google Scholar] [CrossRef]
- Bergamini, E.; Ligorio, G.; Summa, A.; Vannozzi, G.; Cappozzo, A.; Sabatini, A.M. Estimating orientation using magnetic and inertial sensors and different sensor fusion approaches: Accuracy assessment in manual and locomotion tasks. Sensors 2014, 14, 18625–18649. [Google Scholar] [CrossRef]
- Teufl, W.; Miezal, M.; Taetz, B.; Fröhlich, M.; Bleser, G. Validity of inertial sensor based 3D joint kinematics of static and dynamic sport and physiotherapy specific movements. PLoS ONE 2019, 14, e0213064. [Google Scholar] [CrossRef]
- Brice, S.M.; Phillips, E.J.; Millett, E.L.; Hunter, A.; Philippa, B. Comparing inertial measurement units and marker-based biomechanical models during dynamic rotation of the torso. Eur. J. Sport Sci. 2020, 20, 767–775. [Google Scholar] [CrossRef]
- Cappozzo, A.; Catani, F.; Della Croce, U.; Leardini, A. Position and orientation in space of bones during movement: Anatomical frame definition and determination. Clin. Biomech. 1995, 10, 171–178. [Google Scholar] [CrossRef]
- Cutti, A.G.; Ferrari, A.; Garofalo, P.; Raggi, M.; Cappello, A.; Ferrari, A. ‘Outwalk’: A protocol for clinical gait analysis based on inertial and magnetic sensors. Med. Biol. Eng. Comput. 2010, 48, 17–25. [Google Scholar] [CrossRef] [PubMed]
- Hopkins, W.; Marshall, S.; Batterham, A.; Hanin, J. Progressive statistics for studies in sports medicine and exercise science. Med. Sci. Sports Exerc. 2009, 41, 3–12. [Google Scholar] [CrossRef] [PubMed]
- Bland, J.M.; Altman, D.G. Statistical methods for assessing agreement between two methods of clinical measurement. Lancet 1986, 327, 307–310. [Google Scholar] [CrossRef]
- Ludbrook, J. Confidence in Altman–Bland plots: A critical review of the method of differences. Clin. Exp. Pharmacol. Physiol. 2010, 37, 143–149. [Google Scholar] [CrossRef]
- Hopkins, W.G. Sportsci. Org. Sportscience 2018, 8, 1–7. [Google Scholar]
- Pyne, D. Measurement studies in sports science research. Int. J. Sports Physiol. Perform. 2008, 3, 409–410. [Google Scholar] [CrossRef]
- Hopkins, W.G. Spreadsheets for analysis of validity and reliability. Sportscience 2015, 19, 36–42. [Google Scholar]


| Optical Tracking | Ergotex | Mean Diff | ES | |
|---|---|---|---|---|
| Anterior pelvic tilt | 15.06 ± 4.33 | 14.71 ± 4.47 | 0.35 ± 0.92 * | 0.08 |
| +95% CI | 16.36 | 16.06 | 0.64 | 0.14 |
| −95% CI | 13.76 | 13.36 | 0.07 | −0.03 |
| Neutral | 3.65 ± 3.53 | 3.67 ± 3.96 | −0.02 ± 1.04 | 0.00 |
| +95% CI | 4.43 | 4.54 | 0.21 | 0.03 |
| −95% CI | 2.87 | 2.79 | −0.25 | −0.04 |
| Posterior pelvic tilt | −8.26 ± 7.65 | −8.27 ± 7.78 | −0.01 ± 1.19 | 0.00 |
| +95% CI | −5.98 | −5.93 | 0.35 | 0.06 |
| −95% CI | −10.57 | −10.61 | −0.37 | −0.06 |
| Overall | 3.51 ± 9.89 | 3.43 ± 9.90 | 0.08 ± 1.05 | 0.01 |
| +95% CI | 5.00 | 4.92 | 0.24 | 0.02 |
| −95% CI | 2.02 | 1.94 | −0.08 | −0.01 |
| Bias | +LoA | −LoA | Intercept | Slope | r | p | |
|---|---|---|---|---|---|---|---|
| Anterior pelvic tilt | 0.35 * | 2.17 | −1.46 | 0.84 | −0.04 | −0.16 | 0.31 |
| +95% CI | 0.63 | 2.64 | −0.98 | 1.84 | 0.03 | 0.14 | |
| −95% CI | 0.07 | 1.69 | −1.94 | −0.15 | −0.09 | −0.43 | |
| Neutral | −0.02 | 2.01 | −2.05 | 0.41 | −0.12 | −0.41 | <0.001 |
| +95% CI | 0.21 | 2.41 | −1.66 | 0.70 | −0.06 | −0.22 | |
| −95% CI | −0.25 | 1.62 | −2.44 | 0.11 | −0.17 | −0.58 | |
| Posterior pelvic tilt | −0.01 | 2.32 | −2.33 | −0.16 | −0.02 | −0.12 | 0.44 |
| +95% CI | 0.35 | 2.94 | −1.72 | 0.37 | 0.37 | 0.18 | |
| −95% CI | −0.37 | 1.71 | −2.95 | −0.69 | −0.69 | −0.39 | |
| Overall | 0.08 | 2.16 | −2.00 | 0.08 | −0.001 | −0.01 | 0.89 |
| +95% CI | 0.24 | 2.43 | −1.72 | 0.26 | 0.015 | 0.14 | |
| −95% CI | −0.08 | 1.89 | −2.26 | −0.08 | −0.017 | −0.16 |
| Intercept | Slope | r | SEE | Stdz. SEE | |
|---|---|---|---|---|---|
| Anterior pelvic tilt | 1.13 | 0.95 | 0.994 ** | 0.91 | 0.21 (S) |
| +95% CI | 2.08 | 1.00 | 0.997 | 1.15 | 0.29 (S) |
| −95% CI | 0.19 | 0.88 | 0.990 | 0.75 | 0.16 (S) |
| Neutral | 0.49 | 0.86 | 0.968 ** | 0.89 | 0.26 (S) |
| +95% CI | 0.75 | 0.91 | 0.979 | 1.06 | 0.33 (M) |
| −95% CI | 0.21 | 0.81 | 0.951 | 0.77 | 0.21 (S) |
| Posterior pelvic tilt | −0.25 | 0.97 | 0.988 ** | 1.18 | 0.15 (S) |
| +95% CI | 0.27 | 0.27 | 0.994 | 1.50 | 0.21 (S) |
| −95% CI | −0.77 | −0.77 | 0.979 | 0.98 | 0.11 (S) |
| Overall | 0.11 | 0.99 | 0.994 ** | 1.06 | 0.11 (S) |
| +95% CI | 0.27 | 1.00 | 0.996 | 1.19 | 0.12 (S) |
| −95% CI | −0.06 | 0.97 | 0.992 | 0.96 | 0.09 (T) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
García-Luna, M.A.; Jimenez-Olmedo, J.M.; Pueo, B.; Manchado, C.; Cortell-Tormo, J.M. Concurrent Validity of the Ergotex Device for Measuring Low Back Posture. Bioengineering 2024, 11, 98. https://doi.org/10.3390/bioengineering11010098
García-Luna MA, Jimenez-Olmedo JM, Pueo B, Manchado C, Cortell-Tormo JM. Concurrent Validity of the Ergotex Device for Measuring Low Back Posture. Bioengineering. 2024; 11(1):98. https://doi.org/10.3390/bioengineering11010098
Chicago/Turabian StyleGarcía-Luna, Marco A., Jose M. Jimenez-Olmedo, Basilio Pueo, Carmen Manchado, and Juan M. Cortell-Tormo. 2024. "Concurrent Validity of the Ergotex Device for Measuring Low Back Posture" Bioengineering 11, no. 1: 98. https://doi.org/10.3390/bioengineering11010098
APA StyleGarcía-Luna, M. A., Jimenez-Olmedo, J. M., Pueo, B., Manchado, C., & Cortell-Tormo, J. M. (2024). Concurrent Validity of the Ergotex Device for Measuring Low Back Posture. Bioengineering, 11(1), 98. https://doi.org/10.3390/bioengineering11010098










