Does Liquid/Injectable Platelet-Rich Fibrin Help in the Arthrocentesis Treatment of Temporomandibular Joint Disorder Compared to Other Infusion Options? A Systematic Review of Randomized Clinical Trials
Abstract
1. Introduction
2. Materials and Methods
2.1. Focused Question
2.2. Eligibility Criteria
- P: Patients with TMD;
- I: Application of liquid PRF/i-PRF in the area of the TMJ;
- C: Any other treatment (e.g., hyaluronic acid (HA));
- O: Reduction of symptoms of temporomandibular disorder (e.g., noise, maximal mouth opening, pain);
- S: Randomized clinical trials.
2.3. Search Strategy
2.4. Study Selection and Data Extraction
2.5. Risk of Bias
3. Results
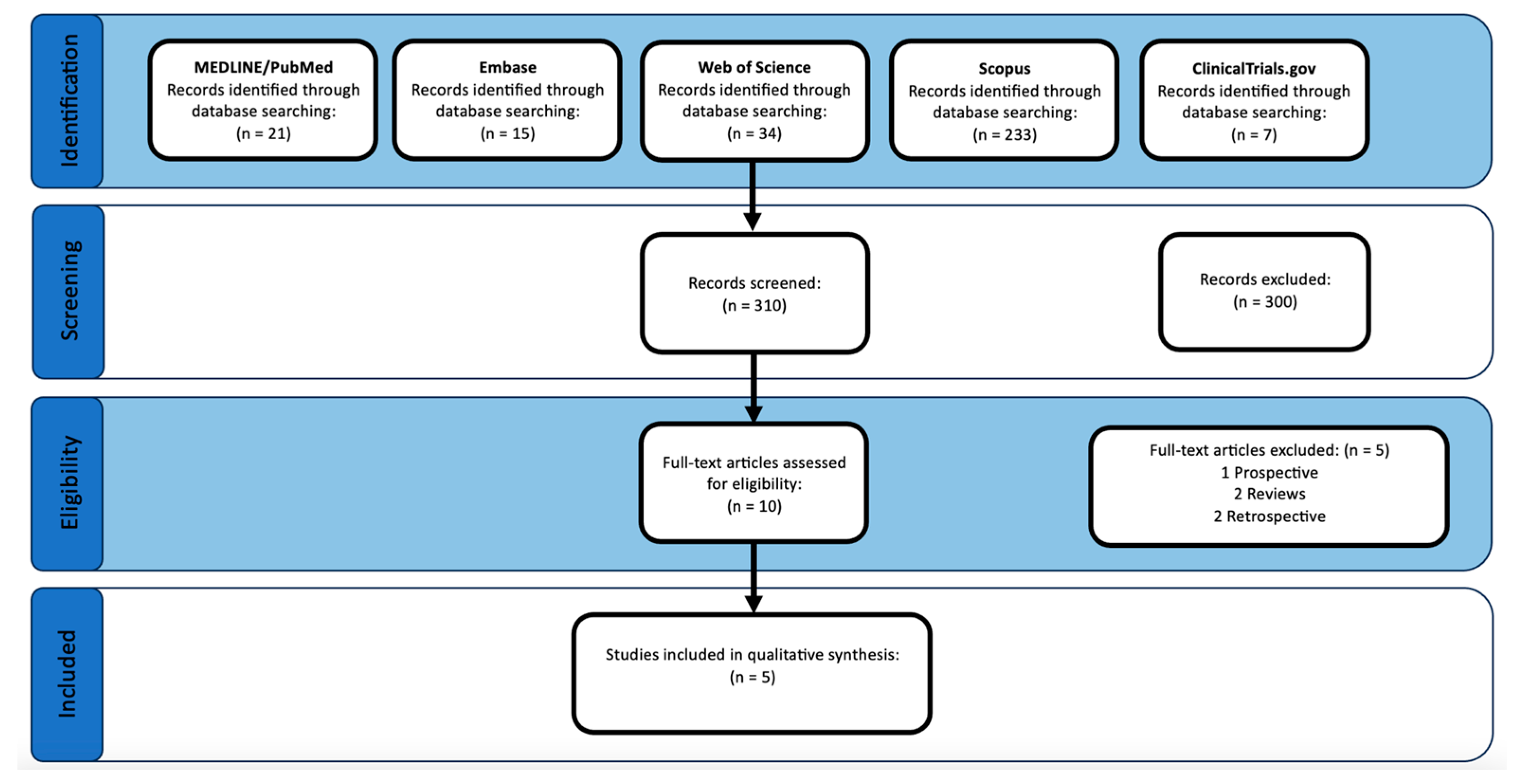
3.1. Study Selection
3.2. Inter-Rater Agreement on Risk of Bias
3.3. Study Characteristics
3.4. Treatment Procedures
3.5. Arthrocentesis (AC) Procedures
3.6. Blood Concentrate Procedures
3.7. Pain
3.8. Movement
3.9. Sounds and/or Clicking
3.10. Disc Position and Joint Effusion
3.11. Risk of Bias within Studies
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Bernardi, S.; Memè, L.; Belfioretti, C.; Bambini, F.; Gerardi, D.; Macchiarelli, G.; Bianchi, S.; Mummolo, S. Psoriatic Arthritis Involving TMJ: A Review on Pathogenesis and Consideration on Eventual Gender Differences. Dent. J. 2024, 12, 31. [Google Scholar] [CrossRef]
- De Leeuw, R.; Klasser, G.D. Orofacial Pain: Guidelines for Assessment, Diagnosis, and Management; Quintessence Publishing Company Incorporated: Hanover Park, IL, USA, 2018. [Google Scholar]
- Valesan, L.F.; Da-Cas, C.D.; Réus, J.C.; Denardin, A.C.S.; Garanhani, R.R.; Bonotto, D.; Januzzi, E.; de Souza, B.D.M. Prevalence of temporomandibular joint disorders: A systematic review and meta-analysis. Clin. Oral Investig. 2021, 25, 441–453. [Google Scholar] [CrossRef]
- Klasser, G.D.; Manfredini, D.; Goulet, J.P.; De Laat, A. Oro-facial pain and temporomandibular disorders classification systems: A critical appraisal and future directions. J. Oral Rehabil. 2018, 45, 258–268. [Google Scholar] [CrossRef]
- Tuncel, U. Repeated sodium hyaluronate injections following multiple arthrocenteses in the treatment of early stage reducing disc displacement of the temporomandibular joint: A preliminary report. J. Cranio-Maxillofac. Surg. 2012, 40, 685–689. [Google Scholar] [CrossRef]
- Gupta, S.; Sharma, A.K.; Purohit, J.; Goyal, R.; Malviya, Y.; Jain, S. Comparison between intra-articular platelet-rich plasma injection versus hydrocortisone with local anesthetic injections in temporomandibular disorders: A double-blind study. Natl. J. Maxillofac. Surg. 2018, 9, 205. [Google Scholar] [PubMed]
- Vingender, S.; Dőri, F.; Schmidt, P.; Hermann, P.; Vaszilkó, M.T. Evaluation of the efficiency of hyaluronic acid, PRP and I-PRF intra-articular injections in the treatment of internal derangement of the temporomandibular joint: A prospective study. J. Cranio-Maxillofac. Surg. 2023, 51, 1–6. [Google Scholar] [CrossRef]
- Yilmaz, O.; Korkmaz, Y.T.; Tuzuner, T. Comparison of treatment efficacy between hyaluronic acid and arthrocentesis plus hyaluronic acid in internal derangements of temporomandibular joint. J. Cranio-Maxillofac. Surg. 2019, 47, 1720–1727. [Google Scholar] [CrossRef]
- Nitzan, D.W.; Svidovsky, J.; Zini, A.; Zadik, Y. Effect of arthrocentesis on symptomatic osteoarthritis of the temporomandibular joint and analysis of the effect of preoperative clinical and radiologic features. J. Oral Maxillofac. Surg. 2017, 75, 260–267. [Google Scholar] [CrossRef] [PubMed]
- Choukroun, J.; Ghanaati, S. Reduction of relative centrifugation force within injectable platelet-rich-fibrin (PRF) concentrates advances patients’ own inflammatory cells, platelets and growth factors: The first introduction to the low speed centrifugation concept. Eur. J. Trauma Emerg. Surg. 2018, 44, 87–95. [Google Scholar] [CrossRef]
- Ghanaati, S.; Herrera-Vizcaino, C.; Al-Maawi, S.; Lorenz, J.; Miron, R.J.; Nelson, K.; Schwarz, F.; Choukroun, J.; Sader, R. Fifteen years of platelet rich fibrin in dentistry and oromaxillofacial surgery: How high is the level of scientific evidence? J. Oral Implantol. 2018, 44, 471–492. [Google Scholar] [CrossRef] [PubMed]
- Dohan, D.M.; Choukroun, J.; Diss, A.; Dohan, S.L.; Dohan, A.J.; Mouhyi, J.; Gogly, B. Platelet-rich fibrin (PRF): A second-generation platelet concentrate. Part II: Platelet-related biologic features. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endodontology 2006, 101, e45–e50. [Google Scholar] [CrossRef]
- Lektemur Alpan, A.; Torumtay Cin, G.; Kızıldağ, A.; Zavrak, N.; Özmen, Ö.; Arslan, Ş.; Mutlu, D. Evaluation of the effect of injectable platelet-rich fibrin (i-PRF) in wound healing and growth factor release in rats: A split-mouth study. Growth Factors 2024, 42, 36–48. [Google Scholar] [CrossRef]
- Cecerska-Heryć, E.; Goszka, M.; Serwin, N.; Roszak, M.; Grygorcewicz, B.; Heryć, R.; Dołęgowska, B. Applications of the regenerative capacity of platelets in modern medicine. Cytokine Growth Factor Rev. 2022, 64, 84–94. [Google Scholar] [CrossRef]
- Işık, G.; Kenç, S.; Koyuncu, B.Ö.; Günbay, S.; Günbay, T. Injectable platelet-rich fibrin as treatment for temporomandibular joint osteoarthritis: A randomized controlled clinical trial. J. Cranio-Maxillofac. Surg. 2022, 50, 576–582. [Google Scholar] [CrossRef]
- Ghoneim, N.I.; Mansour, N.A.; Elmaghraby, S.A.; Abdelsameaa, S.E. Treatment of temporomandibular joint disc displacement using arthrocentesis combined with injectable platelet rich fibrin versus arthrocentesis alone. J. Dent. Sci. 2022, 17, 468–475. [Google Scholar] [CrossRef] [PubMed]
- Işık, G.; Kenç, S.; Koyuncu, B.Ö.; Günbay, S.; Günbay, T. Does the Use of Injectable Platelet-Rich Fibrin After Arthrocentesis for Disc Displacement Without Reduction Improve Clinical Outcomes? J. Oral Maxillofac. Surg. 2023, 81, 689–697. [Google Scholar] [CrossRef] [PubMed]
- Higgins, J.P.; Altman, D.G.; Gøtzsche, P.C.; Jüni, P.; Moher, D.; Oxman, A.D.; Savovic, J.; Schulz, K.F.; Weeks, L.; Sterne, J.A. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ 2011, 343, d5928. [Google Scholar] [CrossRef] [PubMed]
- Karadayi, U.; Gursoytrak, B. Randomised controlled trial of arthrocentesis with or without PRF for internal derangement of the TMJ. J. Cranio-Maxillofac. Surg. 2021, 49, 362–367. [Google Scholar] [CrossRef]
- Sharma, P.; Aurora, J.K.; Dubey, K.; Tandon, P.; Tiwari, S. A comparative analysis between intra articular injections of injectable platelet rich fibrin versus platelet rich plasma in the management of temporomandibular disorders: A randomized control trial. Natl. J. Maxillofac. Surg. 2023, 14, 249–255. [Google Scholar] [CrossRef] [PubMed]
- Nitzan, D.W.; Dolwick, M.F. An alternative explanation for the genesis of closed-lock symptoms in the internal derangement process. J. Oral Maxillofac. Surg. 1991, 49, 810–815; discussion 815–816. [Google Scholar] [CrossRef] [PubMed]
- Gilheaney, Ó.; Stassen, L.F.; Walshe, M. Prevalence, Nature, and Management of Oral Stage Dysphagia in Adults With Temporomandibular Joint Disorders: Findings From an Irish Cohort. J. Oral Maxillofac. Surg. 2018, 76, 1665–1676. [Google Scholar] [CrossRef]
- González-Sánchez, B.; García Monterey, P.; Ramírez-Durán, M.D.V.; Garrido-Ardila, E.M.; Rodríguez-Mansilla, J.; Jiménez-Palomares, M. Temporomandibular Joint Dysfunctions: A Systematic Review of Treatment Approaches. J. Clin. Med. 2023, 12, 4156. [Google Scholar] [CrossRef]
- Chandra, L.; Goyal, M.; Srivastava, D. Minimally invasive intraarticular platelet rich plasma injection for refractory temporomandibular joint dysfunction syndrome in comparison to arthrocentesis. J. Fam. Med. Prim. Care 2021, 10, 254–258. [Google Scholar] [CrossRef]
- Yuce, E.; Komerik, N. Comparison of the Efficiacy of Intra-Articular Injection of Liquid Platelet-Rich Fibrin and Hyaluronic Acid After in Conjunction With Arthrocentesis for the Treatment of Internal Temporomandibular Joint Derangements. J. Craniofacial Surg. 2020, 31, 1870–1874. [Google Scholar] [CrossRef]
- Lin, S.L.; Tsai, C.C.; Wu, S.L.; Ko, S.Y.; Chiang, W.F.; Yang, J.W. Effect of arthrocentesis plus platelet-rich plasma and platelet-rich plasma alone in the treatment of temporomandibular joint osteoarthritis: A retrospective matched cohort study (A STROBE-compliant article). Medicine 2018, 97, e0477. [Google Scholar] [CrossRef]
- Gurung, T.; Singh, R.K.; Mohammad, S.; Pal, U.S.; Mahdi, A.A.; Kumar, M. Efficacy of arthrocentesis versus arthrocentesis with sodium hyaluronic acid in temporomandibular joint osteoarthritis: A comparison. Natl. J. Maxillofac. Surg. 2017, 8, 41–49. [Google Scholar] [CrossRef] [PubMed]
- Gorrela, H.; Prameela, J.; Srinivas, G.; Reddy, B.V.B.; Sudhir, M.; Arakeri, G. Efficacy of Temporomandibular Joint Arthrocentesis with Sodium Hyaluronate in the Management of Temporomandibular Joint Disorders: A Prospective Randomized Control Trial. J. Maxillofac. Oral Surg. 2017, 16, 479–484. [Google Scholar] [CrossRef] [PubMed]
- Mourão, C.F.; Valiense, H.; Melo, E.R.; Mourão, N.B.; Maia, M.D. Obtention of injectable platelets rich-fibrin (i-PRF) and its polymerization with bone graft: Technical note. Rev. Col. Bras. Cir. 2015, 42, 421–423. [Google Scholar] [CrossRef] [PubMed]
- Strauss, F.J.; Nasirzade, J.; Kargarpoor, Z.; Stähli, A.; Gruber, R. Effect of platelet-rich fibrin on cell proliferation, migration, differentiation, inflammation, and osteoclastogenesis: A systematic review of in vitro studies. Clin. Oral Investig. 2020, 24, 569–584. [Google Scholar] [CrossRef] [PubMed]
- Wang, J.; Li, W.; He, X.; Li, S.; Pan, H.; Yin, L. Injectable platelet-rich fibrin positively regulates osteogenic differentiation of stem cells from implant hole via the ERK1/2 pathway. Platelets 2023, 34, 2159020. [Google Scholar] [CrossRef] [PubMed]
- Nakanishi, Y.; Matsushita, T.; Nagai, K.; Araki, D.; Hoshino, Y.; Kuroda, R. Fibrin clot and Leukocyte-rich platelet-rich fibrin show similar release kinetics and amount of growth factors: A pilot study. J. Orthop. Surg. Res. 2023, 18, 238. [Google Scholar] [CrossRef] [PubMed]
- Xu, J.; Ren, H.; Zhao, S.; Li, Q.; Li, C.; Bao, G.; Kang, H. Comparative effectiveness of hyaluronic acid, platelet-rich plasma, and platelet-rich fibrin in treating temporomandibular disorders: A systematic review and network meta-analysis. Head Face Med. 2023, 19, 39. [Google Scholar] [CrossRef] [PubMed]
| Database | Search Strategy |
|---|---|
| PubMed/MEDLINE | (((“Platelet-Rich Fibrin”[Mesh]) OR (((injectable[All Fields] OR “injectable”[All Fields] OR i[All Fields] OR liquid[All Fields] OR l[All Fields]) AND (“Platelet-Rich Fibrin”[Mesh] OR PRF[All Fields]))))) AND (((((“Temporomandibular Joint Disorders”[Mesh])) OR (temporomandibular[All Fields] disorder[All Fields])) OR (TMJ[All Fields] disorder[All Fields]))) |
| EMBASE | (‘platelet rich fibrin’/exp OR (((injectable OR ‘injectable’ OR i OR liquid OR l) AND (‘platelet rich fibrin’ OR prf)))) AND ((‘temporomandibular joint dysfunction’/exp) OR (temporomandibular AND disorder) OR (tmj AND disorder)) |
| Web of Science | TS=((injectable OR “injectable” OR i OR liquid OR l) AND (“platelet-rich fibrin” OR prf)) AND TS=(((“temporomandibular joint disorder *”) OR (temporomandibular AND disorder *) OR (tmj AND disorder *))) |
| Scopus | ((TITLE-ABS-KEY(injectable OR “injectable” OR i OR liquid OR l) AND TITLE-ABS-KEY(“platelet-rich fibrin” OR prf)) AND (TITLE-ABS-KEY((“temporomandibular joint disorder *”) OR (temporomandibular AND disorder *) OR (tmj AND disorder *)))) |
| ClinicalTrials.gov | (injectable OR “injectable” OR i OR liquid OR l) | (Platelet-Rich Fibrin OR PRF) AND (temporomandibular OR tmj) AND (disorder OR dysfunction) |
| Study (Year) | Patient Conditions | Treatment Groups | Number of Subjects (F, M, Mean Age) | Follow-Up (d = days, m = Months) | Interventions (i-PRF Treatment vs. Comparator Treatments) | Outcomes Measured | Main Results |
|---|---|---|---|---|---|---|---|
| Karadayim, Gursoytrak (2021) [19] | Internal derangement of the TMJ | i-PRF + AC vs. AC-only | E (i-PRF + AC): 18 (10 F, 8 M, 39.97). AC-only (18 9 F, 9 M, 39.67) | Preoperative, 10 d, 30 d, 3 m | AC followed immediately by 1 intraarticular injection of i-PRF. 1 treatment of AC. | Pain: VAS HCDS Movement: MIO | VAS (E mean: 5.83 ± 2.550, C mean: 2.94 ± 2.043, p < 0.001), HCDS (E mean: 1.361 ± 5.158, C mean: 9.22 ± 6.916, p: 0.039) |
| Ghoneim, et al. (2022) [16] | TMJ joint displacement | i-PRF + AC vs. AC-only | i-PRF + AC: 20 (16 F, 4 M, 26.45) AC-only 20 (13 F, 7 M, 28.60) | Preoperative, 7 d, 3 m, 6 m | AC followed immediately by 1 intraarticular injection of i-PRF. 1 treatment of AC. | Pain: VAS Sounds: presence or absence Movement: MIO, RLM, LLM | Significant reduction in pain, increase in MIO, and improvement in lateral movements in i-PRF group compared to AC group (p < 0.05) |
| Isik, et al. (2022) [15] | TMJ joint osteoarthritis | i-PRF + AC vs. AC-only | i-PRF + AC: 18 (16 F, 2 M, 44.67) AC-only (18, 17 F, 1 M, 45.72) | Preoperative, 1 m, 2 m, 3 m, 6 m, 12 m | AC plus 4 consecutive intraarticular injections of i-PRF on a weekly basis (AC-only performed with the first injection). 1 treatment of AC. | Pain, MMO, jaw movements | Significant differences in pain, MMO, and jaw movements over 12 months (p < 0.001) in the group with i-PRF injections |
| Isik, et al. (2023) [17] | TMJ disc displacement | AC + i-PRF vs. AC-only | AC + i-PRF: 38 (34 F, 4 M, 47.2) AC-only (38 35 F, 3 M, 46.8) | Preoperative, 1 m, 2 m, 3 m, 6 m, 12 m | AC plus 4 consecutive intraarticular injections of i-PRF on weekly basis (AC only performed with first injection). 1 treatment of AC. | Pain reduction, jaw movement | Treatment success: AC 73.7%, AC + i-PRF 100%, Pain and jaw movement: Significant improvement in AC + i-PRF (p < 0.001) |
| Sharma, et al. (2023) [20] | Internal derangement of the TMJ | AC + PRP: vs. AC + i-PRF | AC + PRP (7, Age: 20–50) AC + i-PRF: 7 (Age: 20–50) | Preoperative, 1 week after treatment for 6 m of treatment, 9 m | AC followed by i-PRF at 1-month intervals for 6 months. AC followed by PRP at 1-month intervals for 6 months. | Pain: VAS Movement: MMO, Lateral, Protrusive Sounds: presence or absence MRI Evaluation: Disc position JE | VAS, MMO, lateral movement, protrusive movement: Statistically significant improvements in both groups, more in i-PRF group (p < 0.05) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Nemeth, A.; Gurgel, B.V.; Lowenstein, A.; Juliasse, L.; Siroma, R.S.; Zhu, Z.; Shibli, J.A.; Mourão, C.F. Does Liquid/Injectable Platelet-Rich Fibrin Help in the Arthrocentesis Treatment of Temporomandibular Joint Disorder Compared to Other Infusion Options? A Systematic Review of Randomized Clinical Trials. Bioengineering 2024, 11, 247. https://doi.org/10.3390/bioengineering11030247
Nemeth A, Gurgel BV, Lowenstein A, Juliasse L, Siroma RS, Zhu Z, Shibli JA, Mourão CF. Does Liquid/Injectable Platelet-Rich Fibrin Help in the Arthrocentesis Treatment of Temporomandibular Joint Disorder Compared to Other Infusion Options? A Systematic Review of Randomized Clinical Trials. Bioengineering. 2024; 11(3):247. https://doi.org/10.3390/bioengineering11030247
Chicago/Turabian StyleNemeth, Alexander, Bruno Vasconcelos Gurgel, Adam Lowenstein, Luiz Juliasse, Rafael S. Siroma, Zoe Zhu, Jamil Awad Shibli, and Carlos Fernando Mourão. 2024. "Does Liquid/Injectable Platelet-Rich Fibrin Help in the Arthrocentesis Treatment of Temporomandibular Joint Disorder Compared to Other Infusion Options? A Systematic Review of Randomized Clinical Trials" Bioengineering 11, no. 3: 247. https://doi.org/10.3390/bioengineering11030247
APA StyleNemeth, A., Gurgel, B. V., Lowenstein, A., Juliasse, L., Siroma, R. S., Zhu, Z., Shibli, J. A., & Mourão, C. F. (2024). Does Liquid/Injectable Platelet-Rich Fibrin Help in the Arthrocentesis Treatment of Temporomandibular Joint Disorder Compared to Other Infusion Options? A Systematic Review of Randomized Clinical Trials. Bioengineering, 11(3), 247. https://doi.org/10.3390/bioengineering11030247











