Survival Rates of Amalgam and Composite Resin Restorations from Big Data Real-Life Databases in the Era of Restricted Dental Mercury Use
Abstract
1. Introduction
2. Materials and Methods
Restorations and Failure File Data
- Single-surface restoration.
- Restoration of 2–3 surfaces.
- Restoration of 4–5 surfaces.
- Two restorations on the same tooth.
3. Results
4. Discussion
5. Limitations
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Shenoy, A. Is it the end of the road for dental amalgam? A critical review. J. Conserv. Dent. 2008, 11, 99–107. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Feldbau, E.V.; Frustino, J.L.; Migliorini, S.A. Chapter 8—Restorative Dentistry. In Dental Secrets, 4th ed.; Sonis, S.T., Ed.; Elsevier: Amsterdam, The Netherlands, 2015; pp. 147–200. ISBN 9780323262781. [Google Scholar]
- Bharti, R.; Wadhwani, K.K.; Tikku, A.P.; Chandra, A. Dental amalgam: An update. J. Conserv. Dent. 2010, 13, 204–208. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Chadwick, R.G.; Lloyd, C.H. Dental amalgam: The history and legacy you perhaps never knew? Br. Dent. J. 2022, 232, 633–637. [Google Scholar] [CrossRef] [PubMed]
- Leinfelder, K.F. Dental amalgam alloys. Curr. Opin. Dent. 1991, 1, 214–217. [Google Scholar] [PubMed]
- Marshall, S.J.; Marshall, G.W., Jr. Dental amalgam: The materials. Adv. Dent. Res. 1992, 6, 94–99. [Google Scholar] [CrossRef] [PubMed]
- ADA council on Scientific Affairs. Dental amalgam: Update on safety concerns. J. Am. Dent. Assoc. 1998, 129, 494–503. [Google Scholar] [CrossRef] [PubMed]
- Bellinger, D.C.; Daniel, D.; Trachtenberg, F.; Tavares, M.; McKinlay, S. Dental amalgam restorations and children’s neuropsychological function: The New England Children’s Amalgam Trial. Environ. Health Perspect. 2007, 115, 440–446. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- DeRouen, T.A.; Martin, M.D.; Leroux, B.G.; Townes, B.D.; Woods, J.S.; Leitão, J.; Castro-Caldas, A.; Luis, H.; Bernardo, M.; Rosenbaum, G.; et al. Neurobehavioral effects of dental amalgam in children: A randomized clinical trial. JAMA 2006, 295, 1784–1792. [Google Scholar] [CrossRef] [PubMed]
- Henshaw, D.L.; O’Carroll, M.J. European Commission: Scientific Committee on Emerging and Newly Identified Health Risks. In The Safety of Dental Amalgam and Alternative Dental Restoration Materials for Patients and Users; European Commission: Brussels, Belgium, 2008. [Google Scholar]
- Minamata Convention on Mercury. United States Environmental Protection Agency. Available online: https://www.mercuryconvention.org/sites/default/files/2021-06/minamata-convention-booklet-sep2019-en-pdf (accessed on 18 March 2024).
- Estrich, C.G.; Lipman, R.D.; Araujo, M.W.B. Dental amalgam restorations in nationally representative sample of US population aged ≥15 years: NHANES 2011–2016. J. Public Health Dent. 2021, 81, 327–330. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Khangura, S.D.; Seal, K.; Esfandiari, S.; Quiñonez, C.; Mierzwinski-Urban, M.; Mulla, S.M.; Laplante, S.; Tsoi, B.; Godfrey, C.; Weeks, L.; et al. Composite Resin Versus Amalgam for Dental Restorations: A Health Technology Assessment [Internet]; Canadian Agency for Drugs and Technologies in Health: Ottawa, ON, Canada, 2018. [PubMed]
- Rasines Alcaraz, M.G.; Veitz-Keenan, A.; Sahrmann, P.; Schmidlin, P.R.; Davis, D.; Iheozor-Ejiofor, Z. Direct composite resin fillings versus amalgam fillings for permanent or adult posterior teeth. Cochrane Database Syst. Rev. 2014, 3, CD005620, Erratum in Cochrane Database Syst. Rev. 2021, 8, CD005620. [Google Scholar] [CrossRef] [PubMed]
- Worthington, H.V.; Khangura, S.; Seal, K.; Mierzwinski-Urban, M.; Veitz-Keenan, A.; Sahrmann, P.; Schmidlin, P.R.; Davis, D.; Iheozor-Ejiofor, Z.; Rasines Alcaraz, M.G. Direct composite resin fillings versus amalgam fillings for permanent posterior teeth. Cochrane Database Syst. Rev. 2021, 8, CD005620. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Maciel, C.M.; Baroudi, K.; Costa, L.D.C.; Souto, T.C.V.; Pino Vitti, R. Longevity of Resin Composite and Amalgam Posterior Restorations: A Systematic Review. Eur. J. Prosthodont. Restor. Dent. 2022, 30, 267–275. [Google Scholar] [CrossRef] [PubMed]
- Bernardo, M.; Luis, H.; Martin, M.D.; Leroux, B.G.; Rue, T.; Leitão, J.; DeRouen, T.A. Survival and reasons for failure of amalgam versus composite posterior restorations placed in a randomized clinical trial. J. Am. Dent. Assoc. 2007, 138, 775–783. [Google Scholar] [CrossRef] [PubMed]
- Alhareky, M.; Tavares, M. Amalgam vs Composite Restoration, Survival, and Secondary Caries. J. Evid. Based Dent. Pract. 2016, 16, 107–109. [Google Scholar] [CrossRef] [PubMed]
- Estrich, C.G.; Eldridge, L.A.; Lipman, R.D.; Araujo, M.W.B. Posterior dental restoration material choices in privately insured people in the United States, 2017 through 2019. J. Am. Dent. Assoc. 2023, 154, 393–402. [Google Scholar] [CrossRef] [PubMed]
- Beltrán-Aguilar, E.D.; Thornton-Evans, G.; Wei, L.; Bernal, J. Prevalence and mean number of teeth with amalgam and nonamalgam restorations, United States, 2015 through 2018. J. Am. Dent. Assoc. 2023, 154, 417–426. [Google Scholar] [CrossRef] [PubMed]
- Ajiboye, A.S.; Mossey, P.A.; IADR Science Information Committee; Fox, C.H. International Association for Dental Research Policy and Position Statements on the Safety of Dental Amalgam. J. Dent. Res. 2020, 99, 763–768. [Google Scholar] [CrossRef] [PubMed]
- FDI World Dental Federation. Alternative direct restorative materials to dental amalgam. Int. Dent. J. 2024, 74, 161–162. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Minamata Convention on Mercury. Report 197, Commonwealth of Australia. 2021. Available online: https://www.dcceew.gov.au/environment/protection/chemicals-management/mercury (accessed on 18 March 2024).
- Manhart, J.; Chen, H.; Hamm, G.; Hickel, R. Buonocore Memorial Lecture. Review of the clinical survival of direct and indirect restorations in posterior teeth of the permanent dentition. Oper Dent. 2004, 29, 481–508. [Google Scholar] [PubMed]
- Van Nieuwenhuysen, J.P.; D’Hoore, W.; Carvalho, J.; Qvist, V. Long-term evaluation of extensive restorations in permanent teeth. J. Dent. 2003, 31, 395–405. [Google Scholar] [CrossRef] [PubMed]
- Opdam, N.J.; Bronkhorst, E.M.; Cenci, M.S.; Huysmans, M.C.; Wilson, N.H. Age of failed restorations: A deceptive longevity parameter. J. Dent. 2011, 39, 225–230. [Google Scholar] [CrossRef] [PubMed]
- Pilcher, L.; Pahlke, S.; Urquhart, O.; O’Brien, K.K.; Dhar, V.; Fontana, M.; González-Cabezas, C.; Keels, M.A.; Mascarenhas, A.K.; Nascimento, M.M.; et al. Direct materials for restoring caries lesions: Systematic review and meta-analysis-a report of the American Dental Association Council on Scientific Affairs. J. Am. Dent. Assoc. 2023, 154, e1–e98. [Google Scholar] [CrossRef] [PubMed]
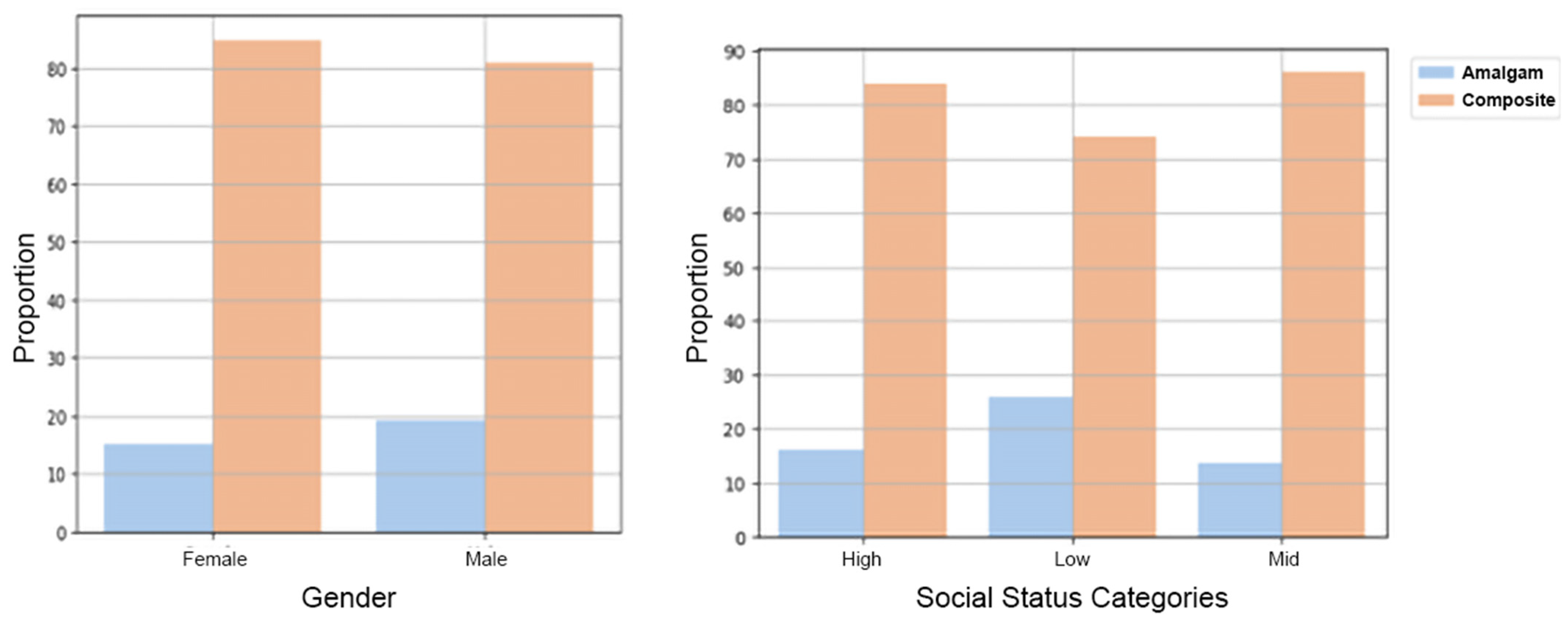
- Willershausen, B.; Witzel, S.; Schuster, S.; Kasaj, A. Influence of gender and social factors on oral health, treatment degree and choice of dental restorative materials in patients from a dental school. Int. J. Dent. Hyg. 2010, 8, 116–120. [Google Scholar] [CrossRef] [PubMed]
- Bailey, O.; Stone, S.; Ternent, L.; Vernazza, C.R. Public Valuation of Direct Restorations: A Discrete Choice Experiment. J. Dent. Res. 2022, 101, 1572–1579. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]

| Comparison between Amalgam to Composite Failure Rate According to Subset | Odds Ratio | 95% Confidence Interval | p Value |
|---|---|---|---|
| Main effect for treatment type | 1.255 | (1.231,1.279) | <0.0001 |
| Premolar upper jaw | 1.650 | (1.562,1.743) | <0.0001 |
| Molar upper jaw | 1.641 | (1.587,1.697) | <0.0001 |
| Premolar lower jaw | 1.850 | (1.739,1.968) | <0.0001 |
| Molar lower jaw | 1.704 | (1.651,1.760) | <0/0001 |
| 1 surface | 1.500 | (1.404,1.601) | <0.0001 |
| 2–3 surfaces | 1.804 | (1.759,1.850) | <0.0001 |
| 4–5 surfaces/double | 1.182 | (1.071,1.306) | <0.0001 |
| Upper jaw | 1.796 | (1.742,1.842) | <0.0001 |
| Lower jaw | 1.887 | (1.831,1.945) | <0.0001 |
| Premolar | 1.789 | (1.714,1.867) | <0.0001 |
| Molar | 1.698 | (1.656,1.740) | <0.0001 |
| Treatment Type | First | N Restoration | N Fail | Percentage |
|---|---|---|---|---|
| Amalgam | 2014 | 21,869 | 5085 | 23.25 |
| Composite | 2014 | 46,272 | 10,412 | 22.50 |
| Amalgam | 2015 | 19,452 | 4352 | 22.37 |
| Composite | 2015 | 47,798 | 10,101 | 21.13 |
| Amalgam | 2016 | 18,454 | 3809 | 20.64 |
| Composite | 2016 | 59,069 | 11,571 | 19.58 |
| Amalgam | 2017 | 15,174 | 2744 | 18.08 |
| Composite | 2017 | 67,812 | 10,942 | 16.13 |
| Amalgam | 2018 | 13,498 | 1850 | 13.70 |
| Composite | 2018 | 73,396 | 9098 | 12.39 |
| Amalgam | 2019 | 10,236 | 1097 | 10.71 |
| Composite | 2019 | 83,353 | 7687 | 9.22 |
| Amalgam | 2020 | 7612 | 558 | 7.33 |
| Composite | 2020 | 81,902 | 4274 | 5.21 |
| Amalgam | 2021 | 6986 | 197 | 2.81 |
| Composite | 2021 | 96,069 | 1858 | 1.93 |
| All | all years | 668,952 | 85,635 | 12.80 |
| Amalgam | all years | 113,281 | 19,692 | 17.38 |
| Composite | all years | 555,671 | 65,943 | 11.86 |
| 1st Treatment Type | 2nd Treatment Type | N Fail | Mean | Std |
|---|---|---|---|---|
| Amalgam | Extraction | 998 | 32.379679 | 23.606581 |
| Amalgam | Restoration | 13,442 | 31.524709 | 23.437284 |
| Amalgam | Root Canal | 5252 | 26.046925 | 22.158989 |
| Composite | Extraction | 2187 | 27.207901 | 21.948151 |
| Composite | Restoration | 50,935 | 27.187016 | 21.284104 |
| Composite | Root Canal | 12,821 | 19.715014 | 19.761084 |
| Amalgam | All Second Treatments | 19,692 | 30.107074 | 23.24094 |
| Composite | All Second Treatments | 65,943 | 25.734961 | 21.223939 |
| Restoration Type | Failure % at Eight Years | Mean Annual Failure Rates (%) | ||
|---|---|---|---|---|
| Factor | Amalgam | Composite | Amalgam | Composite |
| Surfaces: | ||||
| 1 Surface | 14.01 | 10.75 | 2.87 | 2.58 |
| 2–3 Surfaces | 17.56 | 12.03 | 3.39 | 2.84 |
| 4–5 Surfaces/Double Restoration | 18.51 | 17.86 | 4.01 | 4.81 |
| Teeth Group: | ||||
| Molar | 17.54 | 12.07 | 3.57 | 3.16 |
| Molar Upper Jaw | 16.39 | 11.36 | 3.29 | 3.03 |
| Molar Lower Jaw | 18.82 | 12.68 | 3.89 | 3.26 |
| Premolar | 16.75 | 11.60 | 3.45 | 2.94 |
| Premolar Upper Jaw | 15.51 | 11.02 | 3.14 | 2.82 |
| Premolar Lower Jaw | 18.59 | 12.40 | 3.91 | 3.11 |
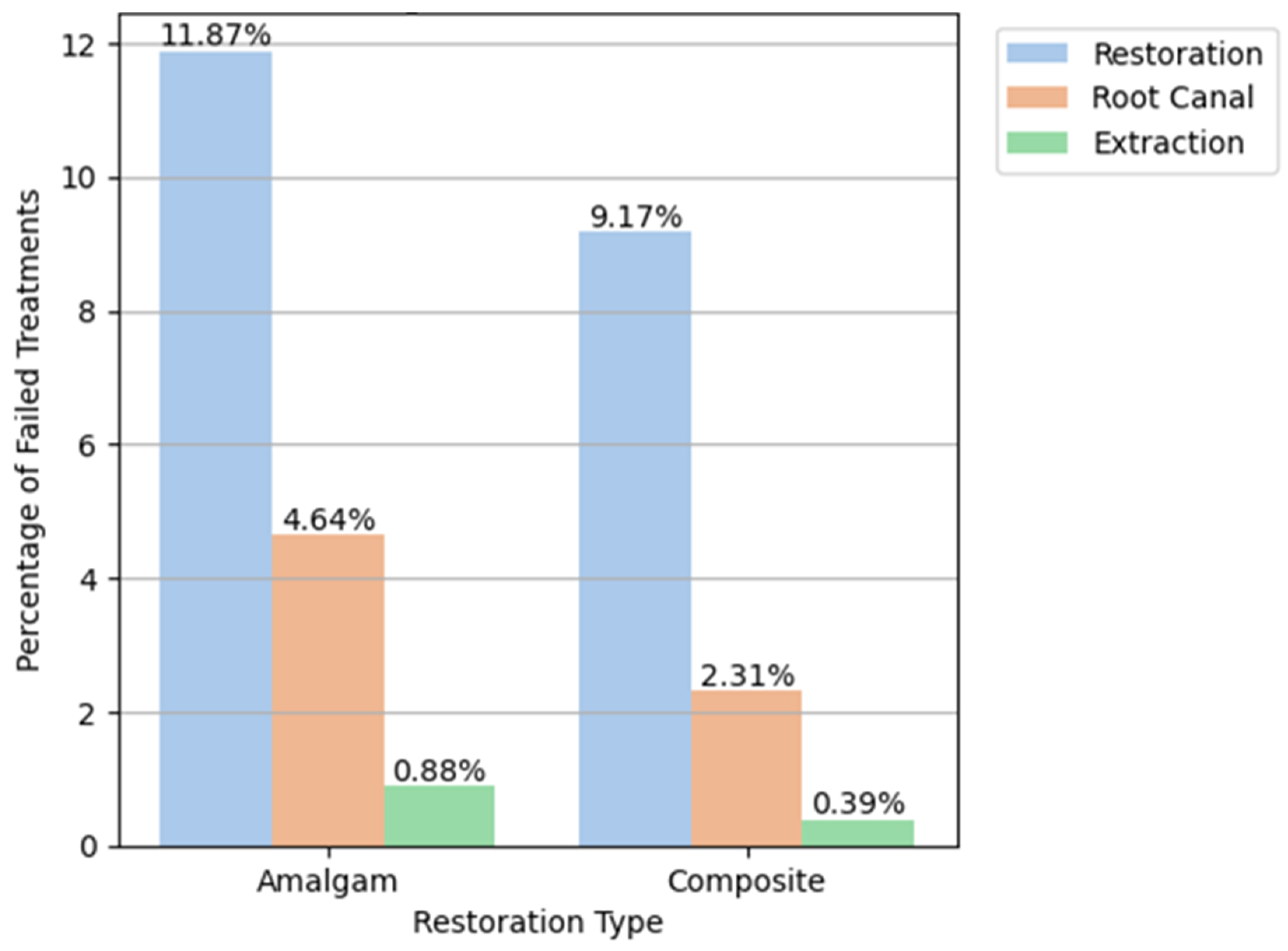
| Follow-Up Indicative Treatment: | ||||
| Repeated Restoration | 11.87 | 9.17 | 2.22 | 2.27 |
| Root Canal | 4.64 | 2.31 | 1.05 | 0.63 |
| Extraction | 0.88 | 0.39 | 0.18 | 0.10 |
| All | 17.38 | 11.87 | 3.55 | 3.06 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tobias, G.; Chackartchi, T.; Mann, J.; Haim, D.; Findler, M. Survival Rates of Amalgam and Composite Resin Restorations from Big Data Real-Life Databases in the Era of Restricted Dental Mercury Use. Bioengineering 2024, 11, 579. https://doi.org/10.3390/bioengineering11060579
Tobias G, Chackartchi T, Mann J, Haim D, Findler M. Survival Rates of Amalgam and Composite Resin Restorations from Big Data Real-Life Databases in the Era of Restricted Dental Mercury Use. Bioengineering. 2024; 11(6):579. https://doi.org/10.3390/bioengineering11060579
Chicago/Turabian StyleTobias, Guy, Tali Chackartchi, Jonathan Mann, Doron Haim, and Mordechai Findler. 2024. "Survival Rates of Amalgam and Composite Resin Restorations from Big Data Real-Life Databases in the Era of Restricted Dental Mercury Use" Bioengineering 11, no. 6: 579. https://doi.org/10.3390/bioengineering11060579
APA StyleTobias, G., Chackartchi, T., Mann, J., Haim, D., & Findler, M. (2024). Survival Rates of Amalgam and Composite Resin Restorations from Big Data Real-Life Databases in the Era of Restricted Dental Mercury Use. Bioengineering, 11(6), 579. https://doi.org/10.3390/bioengineering11060579







