The Influence of Dynamic Taping on Landing Biomechanics after Fatigue in Young Football Athletes: A Randomized, Sham-Controlled Crossover Trial
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants
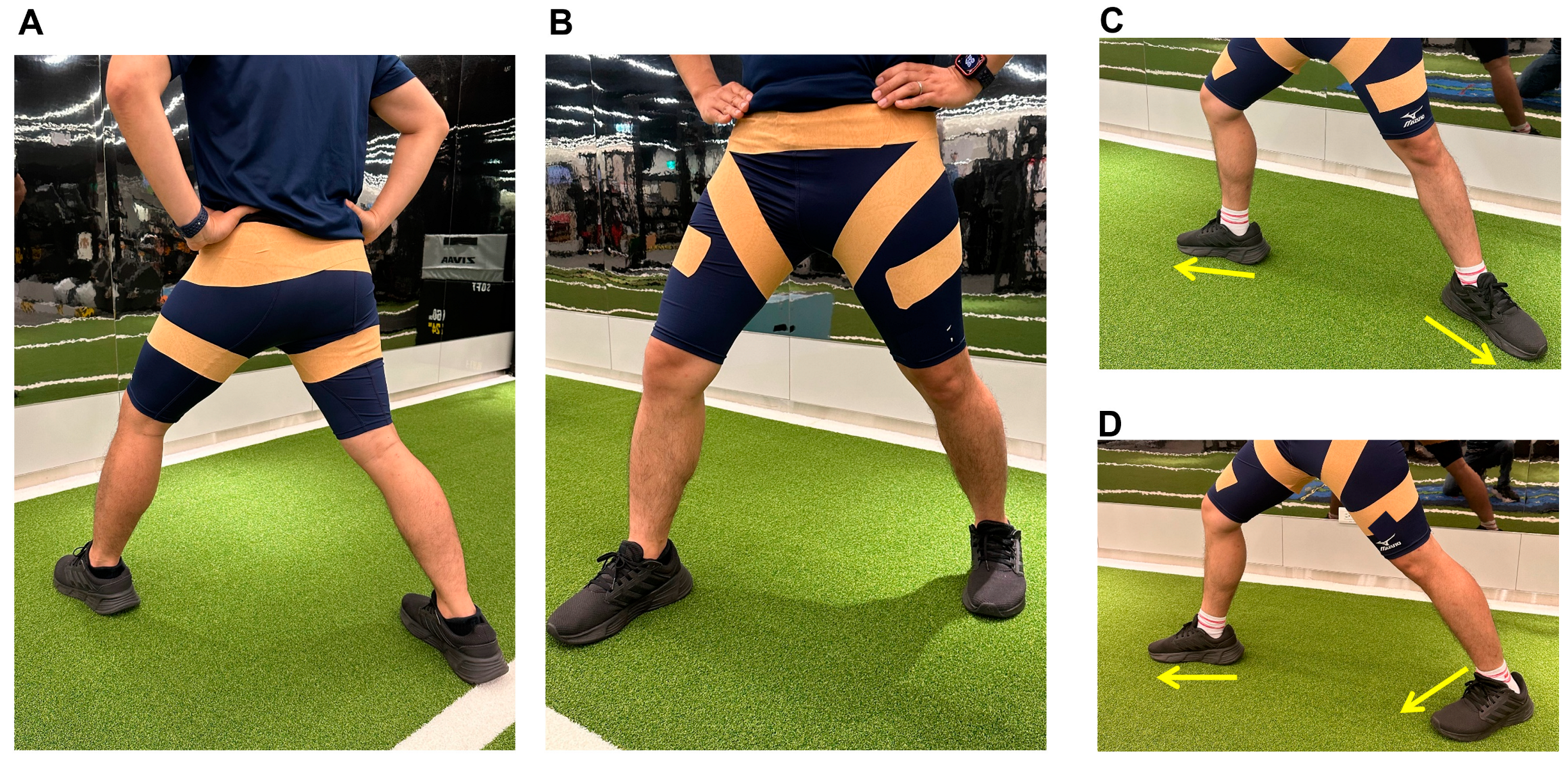
2.2. Dynamic Taping
2.3. Landing Error Scoring System
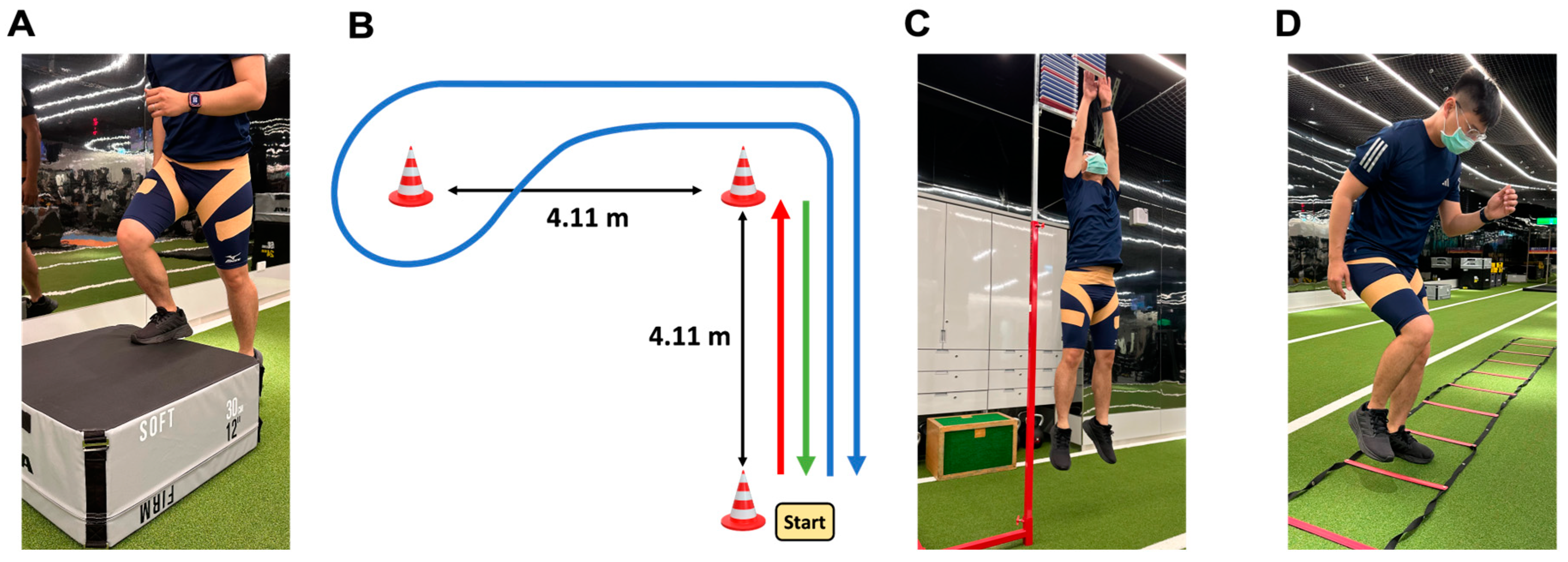
2.4. Functional Agility Short-Term Fatigue Protocol
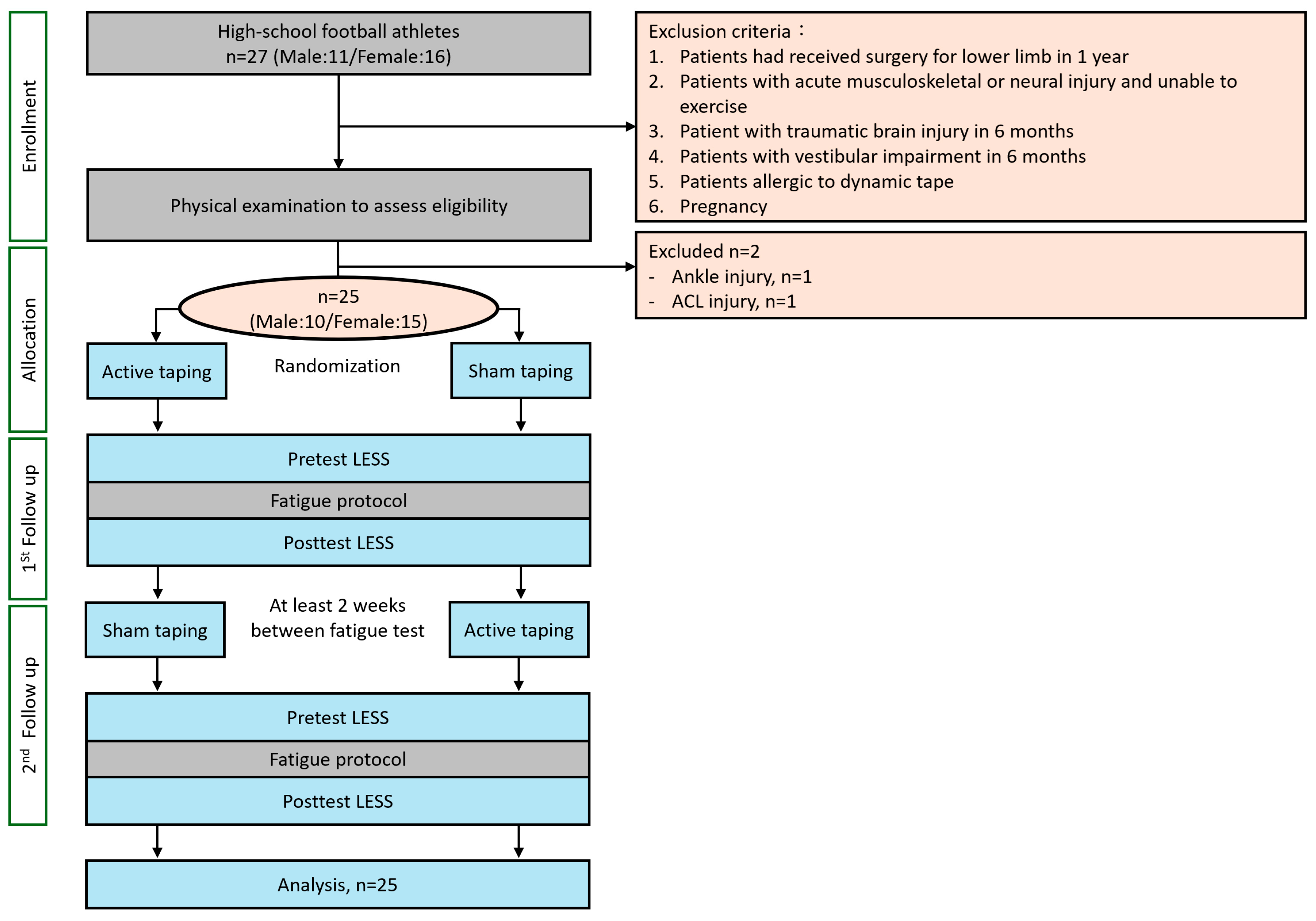
2.5. Research Design
2.6. Statistical Analyses
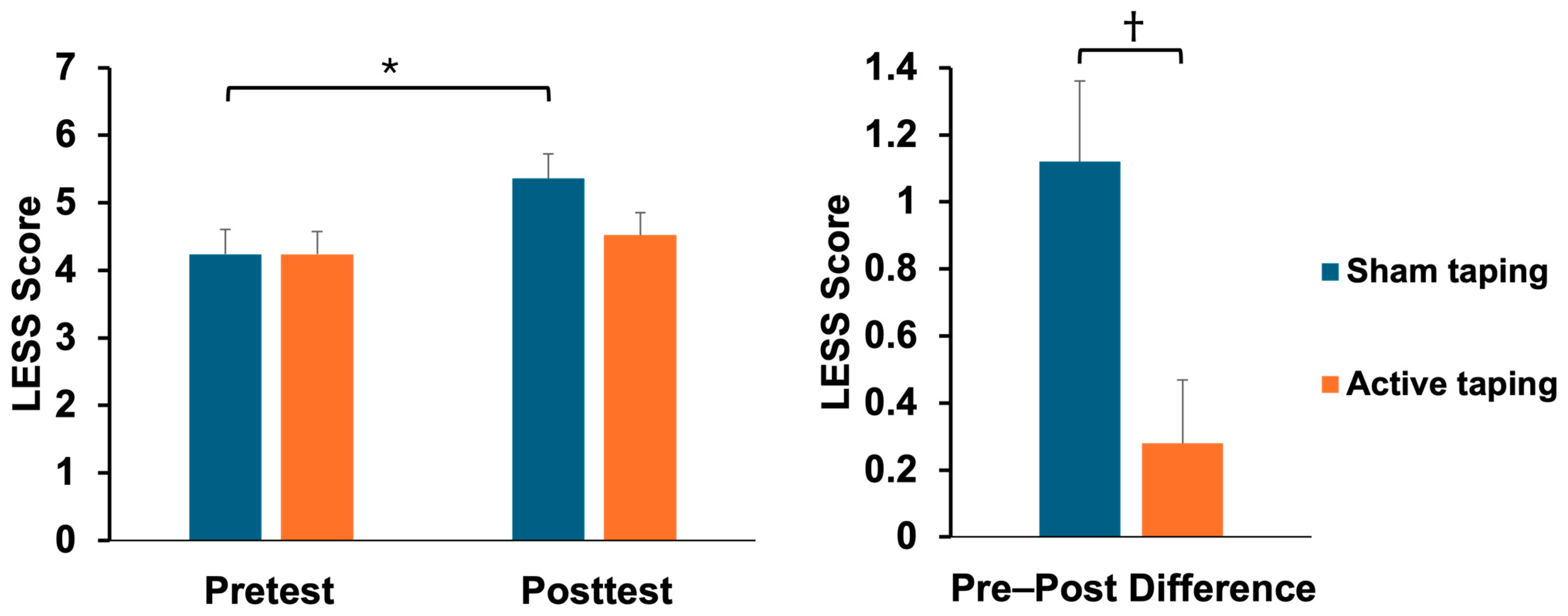
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Ardern, C.L.; Taylor, N.F.; Feller, J.A.; Webster, K.E. Fifty-five per cent return to competitive sport following anterior cruciate ligament reconstruction surgery: An updated systematic review and meta-analysis including aspects of physical functioning and contextual factors. Br. J. Sports Med. 2014, 48, 1543–1552. [Google Scholar] [CrossRef] [PubMed]
- Ardern, C.L.; Taylor, N.F.; Feller, J.A.; Webster, K.E. Return-to-sport outcomes at 2 to 7 years after anterior cruciate ligament reconstruction surgery. Am. J. Sports Med. 2012, 40, 41–48. [Google Scholar] [CrossRef] [PubMed]
- Takahashi, S.; Okuwaki, T. Epidemiological survey of anterior cruciate ligament injury in Japanese junior high school and high school athletes: Cross-sectional study. Res. Sports Med. 2017, 25, 266–276. [Google Scholar] [CrossRef] [PubMed]
- Barber Foss, K.D.; Myer, G.D.; Hewett, T.E. Epidemiology of basketball, soccer, and volleyball injuries in middle-school female athletes. Phys. Sportsmed. 2014, 42, 146–153. [Google Scholar] [CrossRef] [PubMed]
- Swenson, D.M.; Collins, C.L.; Best, T.M.; Flanigan, D.C.; Fields, S.K.; Comstock, R.D. Epidemiology of knee injuries among U.S. high school athletes, 2005/2006–2010/2011. Med. Sci. Sports Exerc. 2013, 45, 462–469. [Google Scholar] [CrossRef]
- Acevedo, R.J.; Rivera-Vega, A.; Miranda, G.; Micheo, W. Anterior Cruciate Ligament Injury: Identification of Risk Factors and Prevention Strategies. Curr. Sports Med. Rep. 2014, 13, 186–191. [Google Scholar] [CrossRef]
- Bell, R.D.; Shultz, S.J.; Wideman, L.; Henrich, V.C. Collagen gene variants previously associated with anterior cruciate ligament injury risk are also associated with joint laxity. Sports Health 2012, 4, 312–318. [Google Scholar] [CrossRef]
- Magnusson, K.; Turkiewicz, A.; Hughes, V.; Frobell, R.; Englund, M. High genetic contribution to anterior cruciate ligament rupture: Heritability ~69. Br. J. Sports Med. 2020, 55, 385–389. [Google Scholar] [CrossRef] [PubMed]
- Posthumus, M.; Collins, M.; van der Merwe, L.; O’Cuinneagain, D.; van der Merwe, W.; Ribbans, W.J.; Schwellnus, M.P.; Raleigh, S.M. Matrix metalloproteinase genes on chromosome 11q22 and the risk of anterior cruciate ligament (ACL) rupture. Scand. J. Med. Sci. Sports 2012, 22, 523–533. [Google Scholar] [CrossRef]
- Shen, L.; Jin, Z.G.; Dong, Q.R.; Li, L.B. Anatomical Risk Factors of Anterior Cruciate Ligament Injury. Chin. Med. J. 2018, 131, 2960–2967. [Google Scholar] [CrossRef]
- Li, F.; Qin, L.; Gong, X.; Huang, Z.; Wang, T.; Liu, Z.; Sandiford, S.; Yang, J.; Zhu, S.; Liang, X.; et al. The Chinese ACL injury population has a higher proportion of small ACL tibial insertion sizes than Western patients. Knee Surg. Sports Traumatol. Arthrosc. 2020, 28, 888–896. [Google Scholar] [CrossRef] [PubMed]
- Kızılgöz, V.; Sivrioğlu, A.K.; Aydın, H.; Ulusoy, G.R.; Çetin, T.; Tuncer, K. The Combined Effect of Body Mass Index and Tibial Slope Angles on Anterior Cruciate Ligament Injury Risk in Male Knees: A Case-Control Study. Clin. Med. Insights Arthritis Musculoskelet. Disord. 2019, 12, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Konopka, J.A.; Hsue, L.; Chang, W.; Thio, T.; Dragoo, J.L. The Effect of Oral Contraceptive Hormones on Anterior Cruciate Ligament Strength. Am. J. Sports Med. 2020, 48, 85–92. [Google Scholar] [CrossRef] [PubMed]
- Hewett, T.E.; Myer, G.D.; Ford, K.R.; Heidt, R.S., Jr.; Colosimo, A.J.; McLean, S.G.; van den Bogert, A.J.; Paterno, M.V.; Succop, P. Biomechanical measures of neuromuscular control and valgus loading of the knee predict anterior cruciate ligament injury risk in female athletes: A prospective study. Am. J. Sports Med. 2005, 33, 492–501. [Google Scholar] [CrossRef] [PubMed]
- Malloy, P.J.; Morgan, A.M.; Meinerz, C.M.; Geiser, C.F.; Kipp, K. Hip External Rotator Strength Is Associated With Better Dynamic Control of the Lower Extremity During Landing Tasks. J. Strength. Cond. Res. 2016, 30, 282–291. [Google Scholar] [CrossRef] [PubMed]
- Earl, J.E.; Monteiro, S.K.; Snyder, K.R. Differences in lower extremity kinematics between a bilateral drop-vertical jump and a single-leg step-down. J. Orthop. Sports Phys. Ther. 2007, 37, 245–252. [Google Scholar] [CrossRef] [PubMed]
- Lawrence, R.K., 3rd; Kernozek, T.W.; Miller, E.J.; Torry, M.R.; Reuteman, P. Influences of hip external rotation strength on knee mechanics during single-leg drop landings in females. Clin. Biomech. 2008, 23, 806–813. [Google Scholar] [CrossRef] [PubMed]
- Padua, D.A.; Marshall, S.W.; Boling, M.C.; Thigpen, C.A.; Garrett, W.E., Jr.; Beutler, A.I. The Landing Error Scoring System (LESS) Is a valid and reliable clinical assessment tool of jump-landing biomechanics: The JUMP-ACL study. Am. J. Sports Med. 2009, 37, 1996–2002. [Google Scholar] [CrossRef]
- Shultz, S.J.; Beynnon, B.D.; Schmitz, R.J. Sex differences in coupled knee motions during the transition from non-weight bearing to weight bearing. J. Orthop. Res. 2009, 27, 717–723. [Google Scholar] [CrossRef]
- Chappell, J.D.; Herman, D.C.; Knight, B.S.; Kirkendall, D.T.; Garrett, W.E.; Yu, B. Effect of fatigue on knee kinetics and kinematics in stop-jump tasks. Am. J. Sports Med. 2005, 33, 1022–1029. [Google Scholar] [CrossRef]
- Hughes, G.; Watkins, J. A risk-factor model for anterior cruciate ligament injury. Sports Med. 2006, 36, 411–428. [Google Scholar] [CrossRef] [PubMed]
- Sanna, G.; O’Connor, K.M. Fatigue-related changes in stance leg mechanics during sidestep cutting maneuvers. Clin. Biomech. 2008, 23, 946–954. [Google Scholar] [CrossRef] [PubMed]
- McLean, S.G.; Samorezov, J.E. Fatigue-induced ACL injury risk stems from a degradation in central control. Med. Sci. Sports Exerc. 2009, 41, 1661–1672. [Google Scholar] [CrossRef]
- McLean, S.G.; Fellin, R.E.; Suedekum, N.; Calabrese, G.; Passerallo, A.; Joy, S. Impact of fatigue on gender-based high-risk landing strategies. Med. Sci. Sports Exerc. 2007, 39, 502–514. [Google Scholar] [CrossRef] [PubMed]
- Cortes, N.; Quammen, D.; Lucci, S.; Greska, E.; Onate, J. A functional agility short-term fatigue protocol changes lower extremity mechanics. J. Sports Sci. 2012, 30, 797–805. [Google Scholar] [CrossRef] [PubMed]
- Lucci, S.; Cortes, N.; Van Lunen, B.; Ringleb, S.; Onate, J. Knee and hip sagittal and transverse plane changes after two fatigue protocols. J. Sci. Med. Sport. 2011, 14, 453–459. [Google Scholar] [CrossRef] [PubMed]
- Quammen, D.; Cortes, N.; Van Lunen, B.L.; Lucci, S.; Ringleb, S.I.; Onate, J. Two different fatigue protocols and lower extremity motion patterns during a stop-jump task. J. Athl. Train. 2012, 47, 32–41. [Google Scholar] [CrossRef] [PubMed]
- Padua, D.A.; DiStefano, L.J.; Beutler, A.I.; de la Motte, S.J.; DiStefano, M.J.; Marshall, S.W. The Landing Error Scoring System as a Screening Tool for an Anterior Cruciate Ligament Injury-Prevention Program in Elite-Youth Soccer Athletes. J. Athl. Train. 2015, 50, 589–595. [Google Scholar] [CrossRef]
- Wesley, C.A.; Aronson, P.A.; Docherty, C.L. Lower Extremity Landing Biomechanics in Both Sexes After a Functional Exercise Protocol. J. Athl. Train. 2015, 50, 914–920. [Google Scholar] [CrossRef]
- Gokeler, A.; Eppinga, P.; Dijkstra, P.U.; Welling, W.; Padua, D.A.; Otten, E.; Benjaminse, A. Effect of fatigue on landing performance assessed with the landing error scoring system (less) in patients after ACL reconstruction. A pilot study. Int. J. Sports Phys. Ther. 2014, 9, 302–311. [Google Scholar]
- Van Melick, N.; van Rijn, L.; Nijhuis-van der Sanden, M.W.G.; Hoogeboom, T.J.; van Cingel, R.E.H. Fatigue affects quality of movement more in ACL-reconstructed soccer players than in healthy soccer players. Knee Surg. Sports Traumatol. Arthrosc. 2019, 27, 549–555. [Google Scholar] [CrossRef] [PubMed]
- McNeill, W.; Pedersen, C. Dynamic tape. Is it all about controlling load? J. Bodyw. Mov. Ther. 2016, 20, 179–188. [Google Scholar] [CrossRef] [PubMed]
- Robinson, N.A.; Spratford, W.; Welvaert, M.; Gaida, J.; Fearon, A.M. Does Dynamic Tape change the walking biomechanics of women with greater trochanteric pain syndrome? A blinded randomised controlled crossover trial. Gait Posture 2019, 70, 275–283. [Google Scholar] [CrossRef] [PubMed]
- Wu, C.K.; Lin, Y.C.; Lai, C.P.; Wang, H.P.; Hsieh, T.H. Dynamic Taping Improves Landing Biomechanics in Young Volleyball Athletes. Int. J. Environ. Res. Public Health 2022, 19, 13716. [Google Scholar] [CrossRef] [PubMed]
- Cortes, N.; Greska, E.; Kollock, R.; Ambegaonkar, J.; Onate, J.A. Changes in lower extremity biomechanics due to a short-term fatigue protocol. J. Athl. Train. 2013, 48, 306–313. [Google Scholar] [CrossRef]
- Wilke, J.; Fleckenstein, J.; Krause, F.; Vogt, L.; Banzer, W. Sport-specific functional movement can simulate aspects of neuromuscular fatigue occurring in team sports. Sports Biomech. 2016, 15, 151–161. [Google Scholar] [CrossRef] [PubMed]
- Cohen, J. Statistical Power Analysis for the Behavioral Sciences; Routledge: New York, NY, USA, 2013. [Google Scholar]
- Fidai, M.S.; Okoroha, K.R.; Meldau, J.; Meta, F.; Lizzio, V.A.; Borowsky, P.; Redler, L.H.; Moutzouros, V.; Makhni, E.C. Fatigue Increases Dynamic Knee Valgus in Youth Athletes: Results From a Field-Based Drop-Jump Test. Arthroscopy 2020, 36, 214–222. [Google Scholar] [CrossRef] [PubMed]
- Koga, H.; Nakamae, A.; Shima, Y.; Bahr, R.; Krosshaug, T. Hip and Ankle Kinematics in Noncontact Anterior Cruciate Ligament Injury Situations: Video Analysis Using Model-Based Image Matching. Am. J. Sports Med. 2018, 46, 333–340. [Google Scholar] [CrossRef] [PubMed]
- Pointer, C.E.; Reems, T.D.; Hartley, E.M.; Hoch, J.M. The Ability of the Landing Error Scoring System to Detect Changes in Landing Mechanics: A Critically Appraised Topic. Int. J. Athl. Ther. Train. 2017, 22, 12–20. [Google Scholar] [CrossRef][Green Version]
- Della Villa, F.; Buckthorpe, M.; Grassi, A.; Nabiuzzi, A.; Tosarelli, F.; Zaffagnini, S.; Della Villa, S. Systematic video analysis of ACL injuries in professional male football (soccer): Injury mechanisms, situational patterns and biomechanics study on 134 consecutive cases. Br. J. Sports Med. 2020, 54, 1423–1432. [Google Scholar] [CrossRef]
- Lucarno, S.; Zago, M.; Buckthorpe, M.; Grassi, A.; Tosarelli, F.; Smith, R.; Della Villa, F. Systematic Video Analysis of Anterior Cruciate Ligament Injuries in Professional Female Soccer Players. Am. J. Sports Med. 2021, 49, 1794–1802. [Google Scholar] [CrossRef] [PubMed]
- Mohr, M.; Krustrup, P.; Bangsbo, J. Match performance of high-standard soccer players with special reference to development of fatigue. J. Sports Sci. 2003, 21, 519–528. [Google Scholar] [CrossRef] [PubMed]
- Daneshjoo, A.; Mokhtar, A.H.; Rahnama, N.; Yusof, A. The effects of comprehensive warm-up programs on proprioception, static and dynamic balance on male soccer players. PLoS ONE 2012, 7, e51568. [Google Scholar] [CrossRef]
- Joy, E.A.; Taylor, J.R.; Novak, M.A.; Chen, M.; Fink, B.P.; Porucznik, C.A. Factors influencing the implementation of anterior cruciate ligament injury prevention strategies by girls soccer coaches. J. Strength. Cond. Res. 2013, 27, 2263–2269. [Google Scholar] [CrossRef] [PubMed]
- Sheikhi, B.; Letafatkar, A.; Hogg, J.; Naseri-Mobaraki, E. The influence of kinesio taping on trunk and lower extremity motions during different landing tasks: Implications for anterior cruciate ligament injury. J. Exp. Orthop. 2021, 8, 25. [Google Scholar] [CrossRef] [PubMed]
- Limroongreungrat, W.; Boonkerd, C. Immediate effect of ACL kinesio taping technique on knee joint biomechanics during a drop vertical jump: A randomized crossover controlled trial. BMC Sports Sci. Med. Rehabil. 2019, 11, 32. [Google Scholar] [CrossRef]
- Castro-Méndez, A.; Palomo-Toucedo, I.C.; Pabón-Carrasco, M.; Ortiz-Romero, M.; Fernández-Seguín, L.M. The Short-Term Effect of Dynamic Tape versus the Low-Dye Taping Technique in Plantar Fasciitis: A Randomized Clinical Trial. Int. J. Environ. Res. Public Health 2022, 19, 16536. [Google Scholar] [CrossRef]
| Male (n = 10) | Female (n = 15) | p-Value | |
|---|---|---|---|
| Age (Year) | 16.40 ± 0.51 | 16.40 ± 0.52 | 1 |
| Body Height (cm) | 173.70 ± 3.16 | 161.43 ± 4.40 | <0.001 * |
| Body Weight (Kg) | 59.30 ± 5.33 | 55.92 ± 4.66 | 0.11 |
| BMI (Kg/cm2) | 19.67 ± 1.93 | 21.52 ± 2.30 | 0.048 * |
| Dominant Leg (Right/Left) | 9/1 | 15/0 |
| LESS | Sham Taping (n = 25) | p-Value | t-Value | Effect Size | Active Taping (n = 25) | p-Value | t-Value | Effect Size | Δ (Post–Pre) between Groups p-Value |
|---|---|---|---|---|---|---|---|---|---|
| Pretest | 4.24 ± 1.83 | 0.04 * | −2.07 | 0.61 | 4.24 ± 1.69 | 0.15 | −1.50 | 0.46 | |
| Posttest | 5.36 ± 2.00 | 4.52 ± 1.69 | |||||||
| Δ (Post–pre) | 1.12 ± 1.20 | 0.28 ± 0.94 | 0.007 † |
| LESS | Sham Taping | Active Taping | Δ (Post–Pre) between Groups p-Value | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Pretest (n = 25) | Posttest (n = 25) | Δ (Post–Pre) | p-Value | Pretest (n = 25) | Posttest (n = 25) | Δ (Post–Pre) | p-Value | ||
| #1 | 0.64 ± 0.49 | 0.56 ± 0.51 | −0.08 ± 0.49 | 0.43 | 0.40 ± 0.50 | 0.40 ± 0.50 | 0.00 ± 0.29 | 1.00 | 0.48 |
| #2 | 0.00 ± 0.00 | 0.00 ± 0.00 | 0.00 ± 0.00 | N/A | 0.00 ± 0.00 | 0.00 ± 0.00 | 0.00 ± 0.00 | N/A | N/A |
| #3 | 0.00 ± 0.00 | 0.04 ± 0.20 | 0.04 ± 0.20 | 0.33 | 0.00 ± 0.00 | 0.00 ± 0.00 | 0.00 ± 0.00 | N/A | 0.32 |
| #4 | 0.64 ± 0.49 | 0.68 ± 0.48 | 0.04 ± 0.35 | 0.57 | 0.64 ± 0.49 | 0.52 ± 0.51 | −0.12 ± 0.44 | 0.18 | 0.16 |
| #5 | 0.24 ± 0.44 | 0.40 ± 0.50 | 0.16 ± 0.47 | 0.10 | 0.24 ± 0.44 | 0.12 ± 0.33 | −0.12 ± 0.44 | 0.18 | 0.04 † |
| #6 | 0.04 ± 0.20 | 0.00 ± 0.00 | −0.04 ± 0.20 | 0.33 | 0.00 ± 0.00 | 0.00 ± 0.00 | 0.00 ± 0.00 | N/A | 0.32 |
| #7 | 0.00 ± 0.00 | 0.04 ± 0.20 | 0.04 ± 0.20 | 0.33 | 0.04 ± 0.20 | 0.04 ± 0.20 | 0.00 ± 0.00 | 1.00 | 0.32 |
| #8 | 0.48 ± 0.51 | 0.52 ± 0.51 | 0.04 ± 0.45 | 0.66 | 0.60 ± 0.50 | 0.52 ± 0.51 | −0.08 ± 0.49 | 0.42 | 0.38 |
| #9 | 0.00 ± 0.00 | 0.00 ± 0.00 | 0.00 ± 0.00 | N/A | 0.00 ± 0.00 | 0.00 ± 0.00 | 0.00 ± 0.00 | N/A | N/A |
| #10 | 0.08 ± 0.28 | 0.12 ± 0.33 | 0.04 ± 0.35 | 0.57 | 0.12 ± 0.33 | 0.08 ± 0.28 | −0.04 ± 0.20 | 0.32 | 0.33 |
| #11 | 0.16 ± 0.37 | 0.28 ± 0.46 | 0.12 ± 0.60 | 0.33 | 0.32 ± 0.48 | 0.40 ± 0.50 | 0.08 ± 0.57 | 0.49 | 0.81 |
| #12 | 0.00 ± 0.00 | 0.00 ± 0.00 | 0.00 ± 0.00 | N/A | 0.00 ± 0.00 | 0.00 ± 0.00 | 0.00 ± 0.00 | N/A | N/A |
| #13 | 0.00 ± 0.00 | 0.00 ± 0.00 | 0.00 ± 0.00 | N/A | 0.00 ± 0.00 | 0.00 ± 0.00 | 0.00 ± 0.00 | N/A | N/A |
| #14 | 0.28 ± 0.46 | 0.52 ± 0.51 | 0.24 ± 0.44 | 0.01 * | 0.28 ± 0.46 | 0.40 ± 0.50 | 0.12 ± 0.33 | 0.08 | 0.28 |
| #15 | 0.64 ± 0.49 | 0.80 ± 0.41 | 0.16 ± 0.47 | 0.10 | 0.56 ± 0.51 | 0.68 ± 0.48 | 0.12 ± 0.33 | 0.08 | 0.73 |
| #16 | 0.32 ± 0.48 | 0.60 ± 0.50 | 0.28 ± 0.54 | 0.02 * | 0.32 ± 0.48 | 0.52 ± 0.51 | 0.20 ± 0.50 | 0.06 | 0.59 |
| #17 | 0.72 ± 0.46 | 0.80 ± 0.41 | 0.08 ± 0.40 | 0.33 | 0.72 ± 0.46 | 0.84 ± 0.37 | 0.12 ± 0.53 | 0.27 | 0.76 |
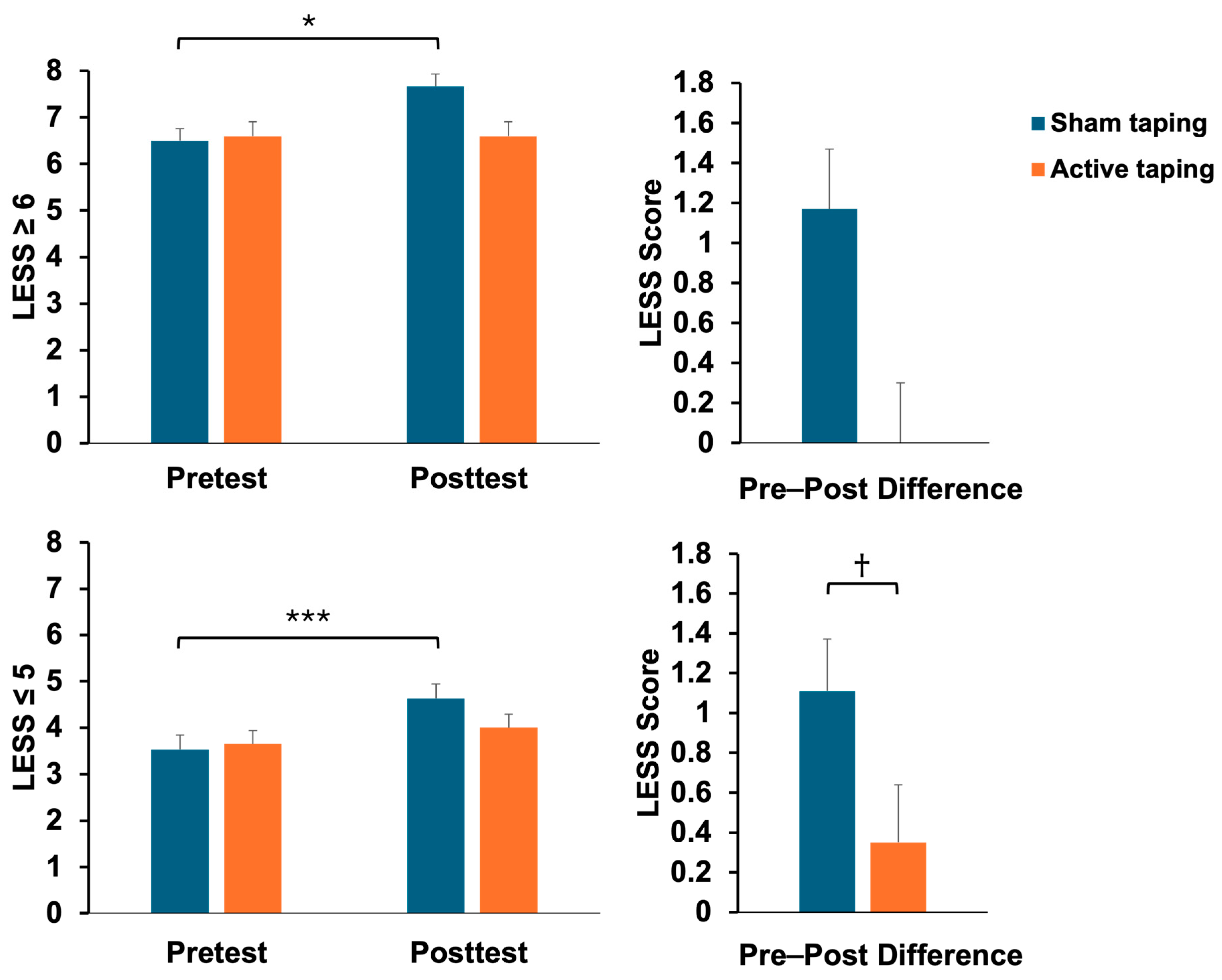
| LESS | Sham Taping (n = 25) | p-Value | t-Value | Effect Size | Active Taping (n = 25) | p-Value | t-Value | Effect Size | Δ (Post–Pre) between Groups p-Value |
|---|---|---|---|---|---|---|---|---|---|
| LESS ≥ 6 | |||||||||
| Pretest | 6.50 ± 0.84 | 0.03 * | −2.91 | 1.63 | 6.60 ± 0.86 | 1.00 | 0 | N/A | |
| Posttest | 7.67 ± 1.03 | 6.60 ± 1.14 | |||||||
| Δ (Post–pre) | 1.17 ± 0.98 | 0.00 ± 1.00 | 0.08 | ||||||
| LESS ≤ 5 | |||||||||
| Pretest | 3.53 ± 1.43 | <0.001 *** | −4.59 | 1.15 | 3.65 ± 1.27 | 0.17 | −1.73 | 0.51 | |
| Posttest | 4.63 ± 1.64 | 4.00 ± 1.38 | |||||||
| Δ (Post–pre) | 1.11 ± 1.50 | 0.35 ± 1.27 | 0.03 † |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wu, C.-K.; Lin, Y.-C.; Chen, Y.-L.; Chao, Y.-P.; Hsieh, T.-H. The Influence of Dynamic Taping on Landing Biomechanics after Fatigue in Young Football Athletes: A Randomized, Sham-Controlled Crossover Trial. Bioengineering 2024, 11, 631. https://doi.org/10.3390/bioengineering11060631
Wu C-K, Lin Y-C, Chen Y-L, Chao Y-P, Hsieh T-H. The Influence of Dynamic Taping on Landing Biomechanics after Fatigue in Young Football Athletes: A Randomized, Sham-Controlled Crossover Trial. Bioengineering. 2024; 11(6):631. https://doi.org/10.3390/bioengineering11060631
Chicago/Turabian StyleWu, Chih-Kuan, Yin-Chou Lin, Ya-Lin Chen, Yi-Ping Chao, and Tsung-Hsun Hsieh. 2024. "The Influence of Dynamic Taping on Landing Biomechanics after Fatigue in Young Football Athletes: A Randomized, Sham-Controlled Crossover Trial" Bioengineering 11, no. 6: 631. https://doi.org/10.3390/bioengineering11060631
APA StyleWu, C.-K., Lin, Y.-C., Chen, Y.-L., Chao, Y.-P., & Hsieh, T.-H. (2024). The Influence of Dynamic Taping on Landing Biomechanics after Fatigue in Young Football Athletes: A Randomized, Sham-Controlled Crossover Trial. Bioengineering, 11(6), 631. https://doi.org/10.3390/bioengineering11060631







