The Fluorescent Cell Line SW620-GFP Is a Valuable Model to Monitor Magnetic Hyperthermia
Abstract
:1. Introduction
2. Materials and Methods
2.1. Synthesis of SPIONs
2.2. Physical and Chemical Characterization of the SPIONs
2.3. Cell Line, Growing Conditions, and Relative Cell Viability (RCV)
2.4. Cytotoxicity and In Vitro Assays of Magnetic Hyperthermia
2.5. In Vivo Assays of Magnetic Hyperthermia
3. Results and Discussion
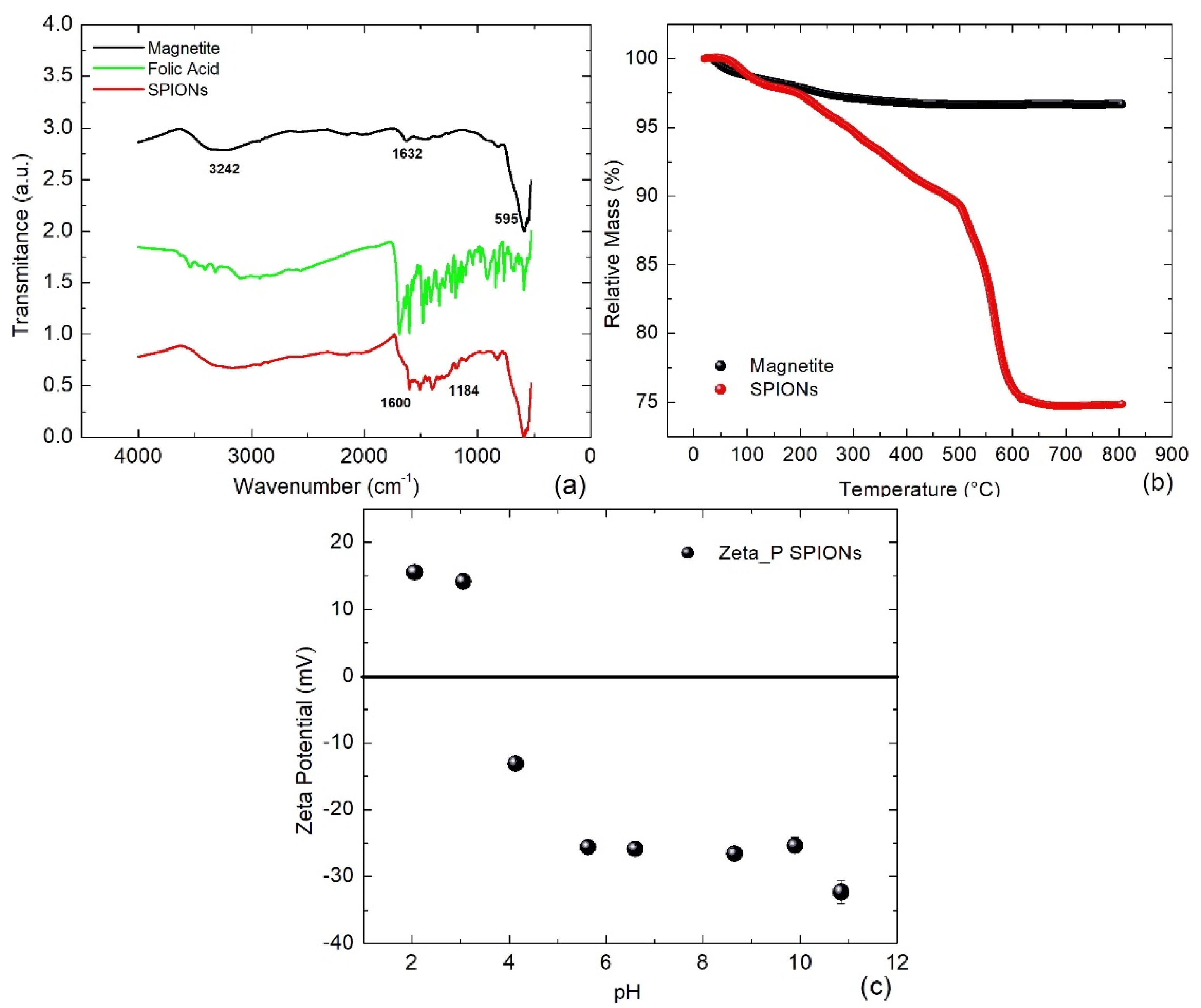
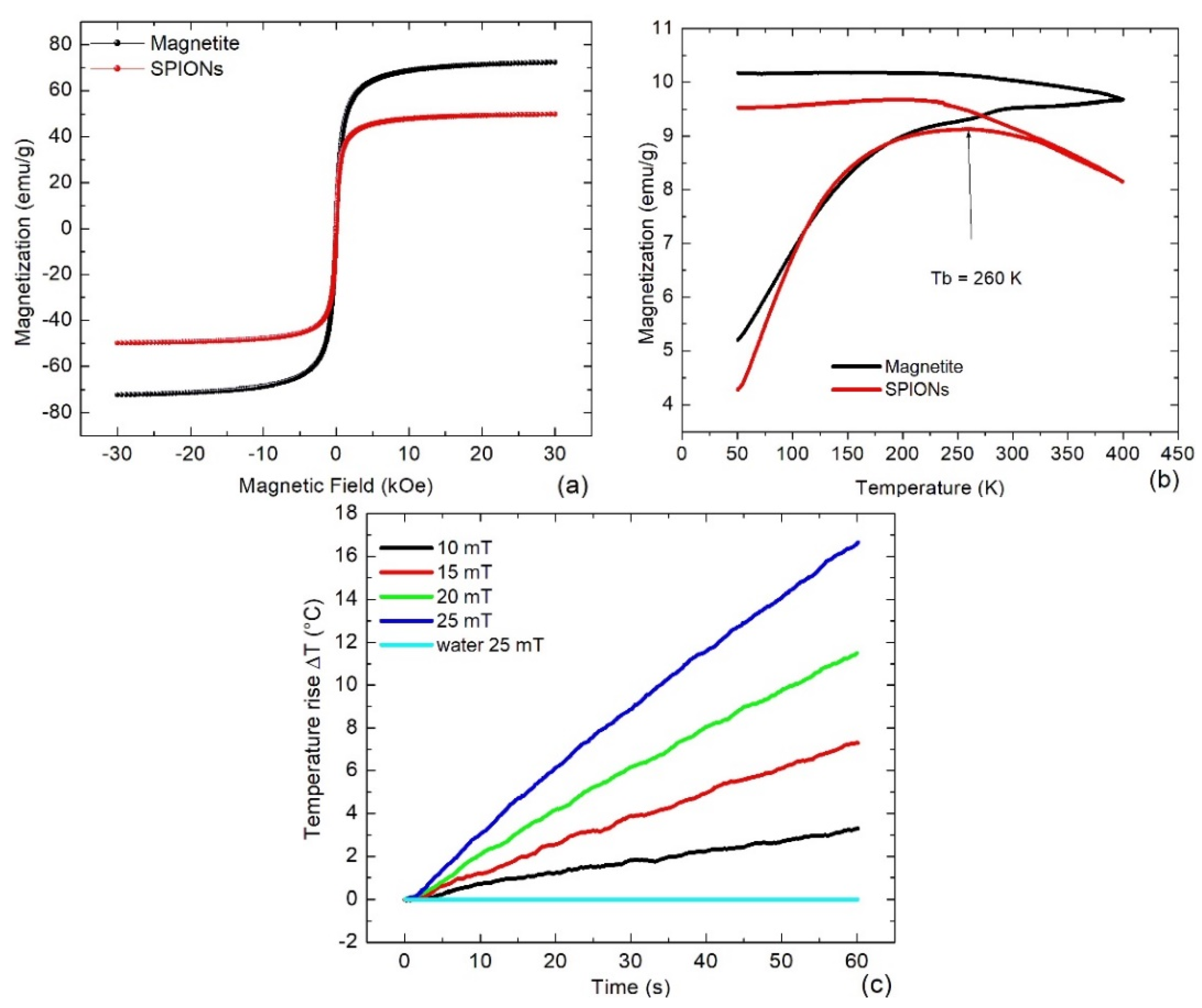
3.1. Physical and Chemical Characterization
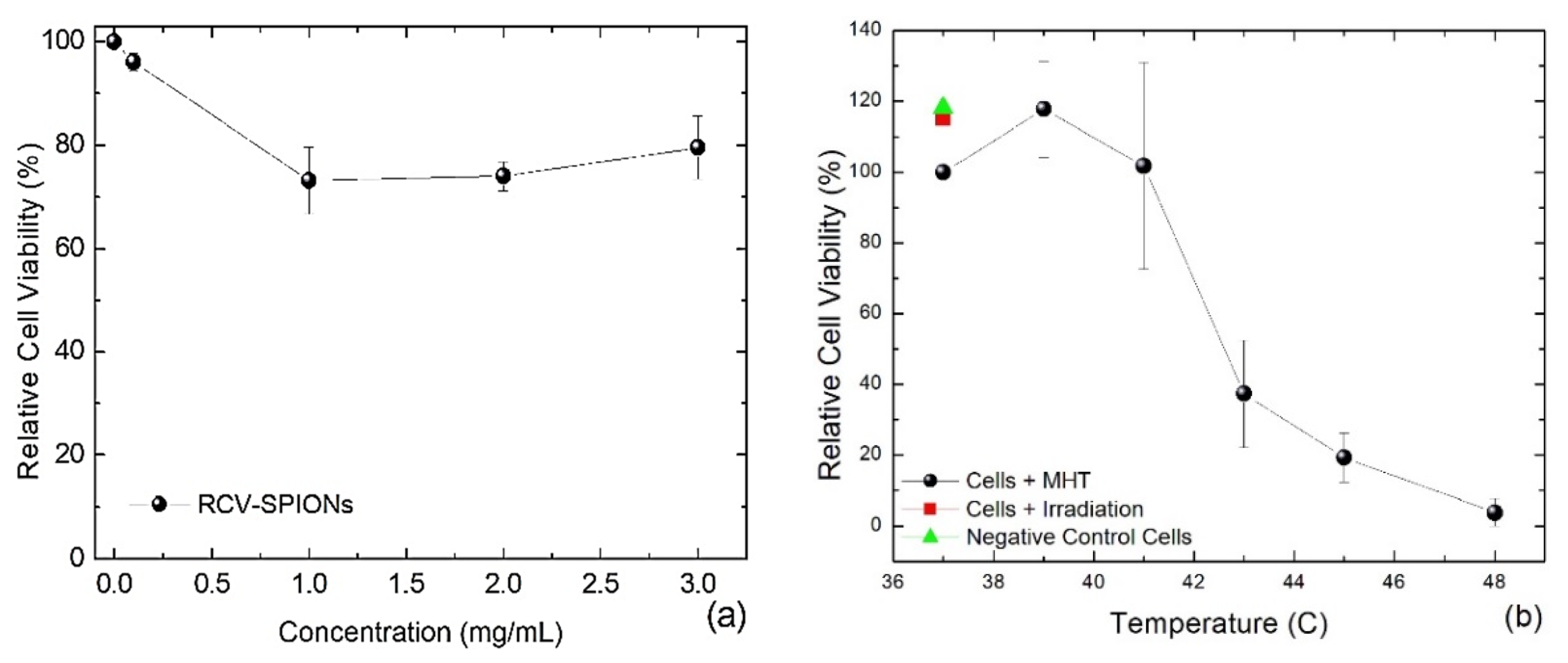
3.2. Results of Cytotoxicity and In Vitro Magnetic Hyperthermia
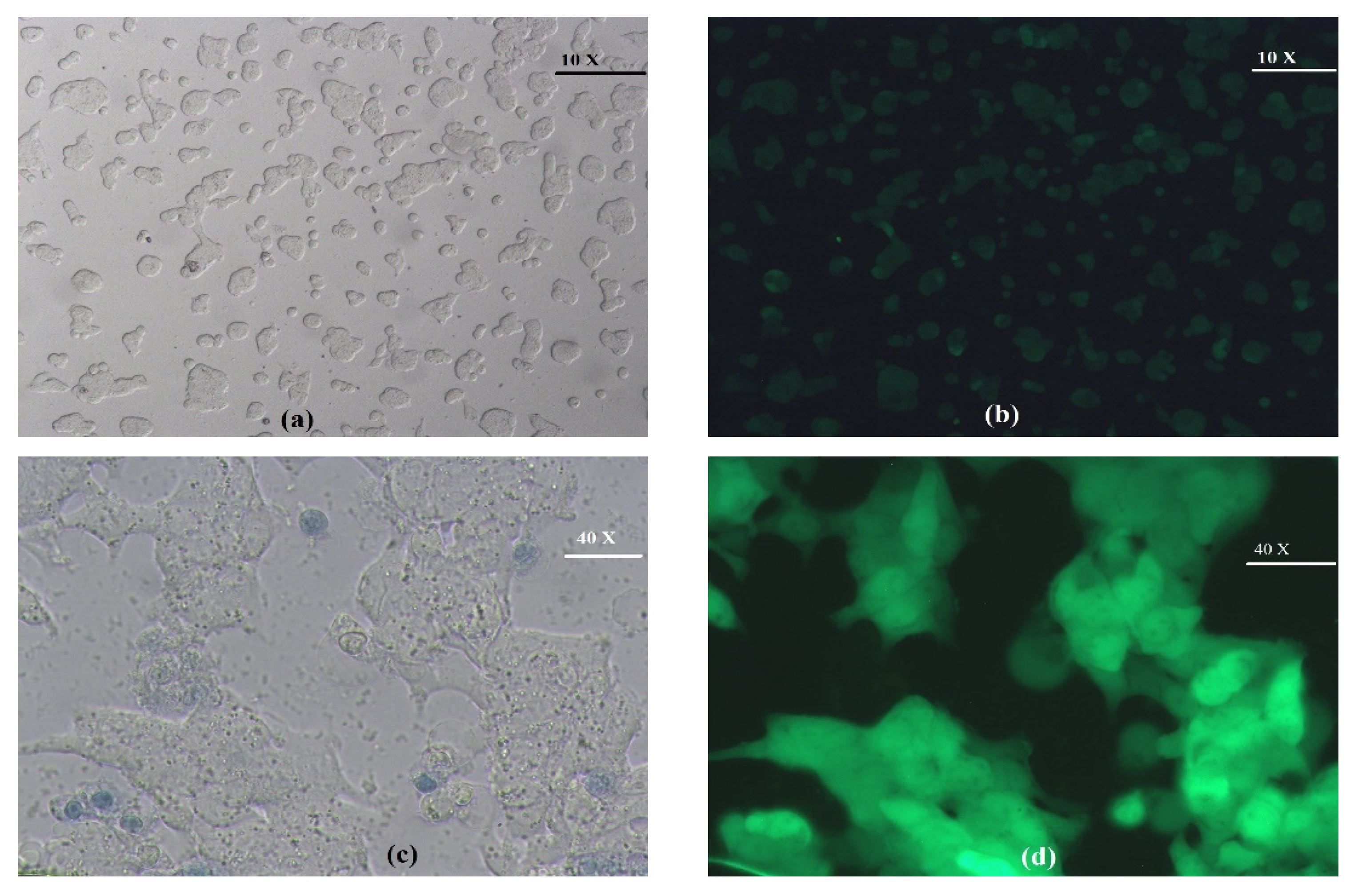
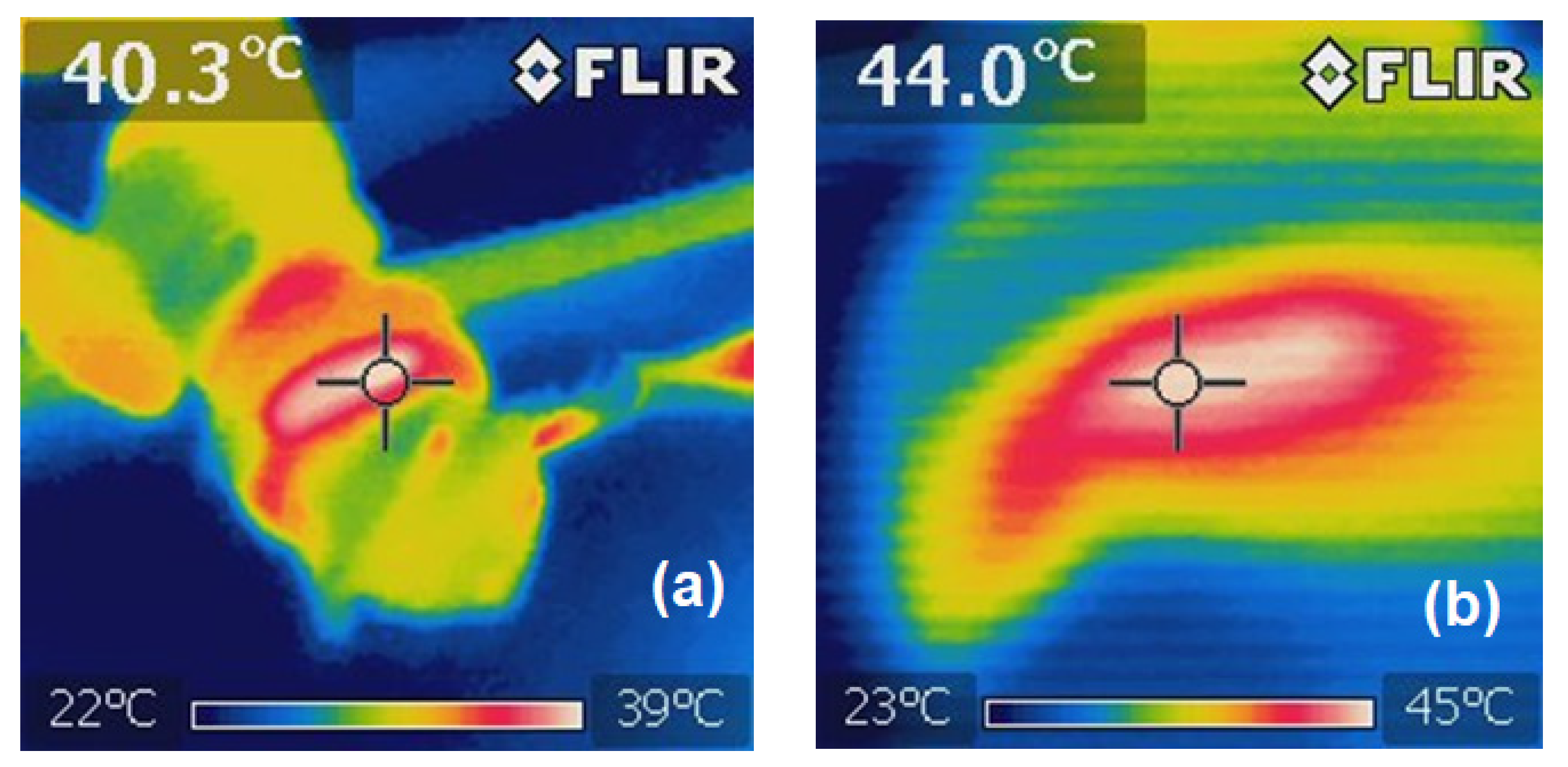
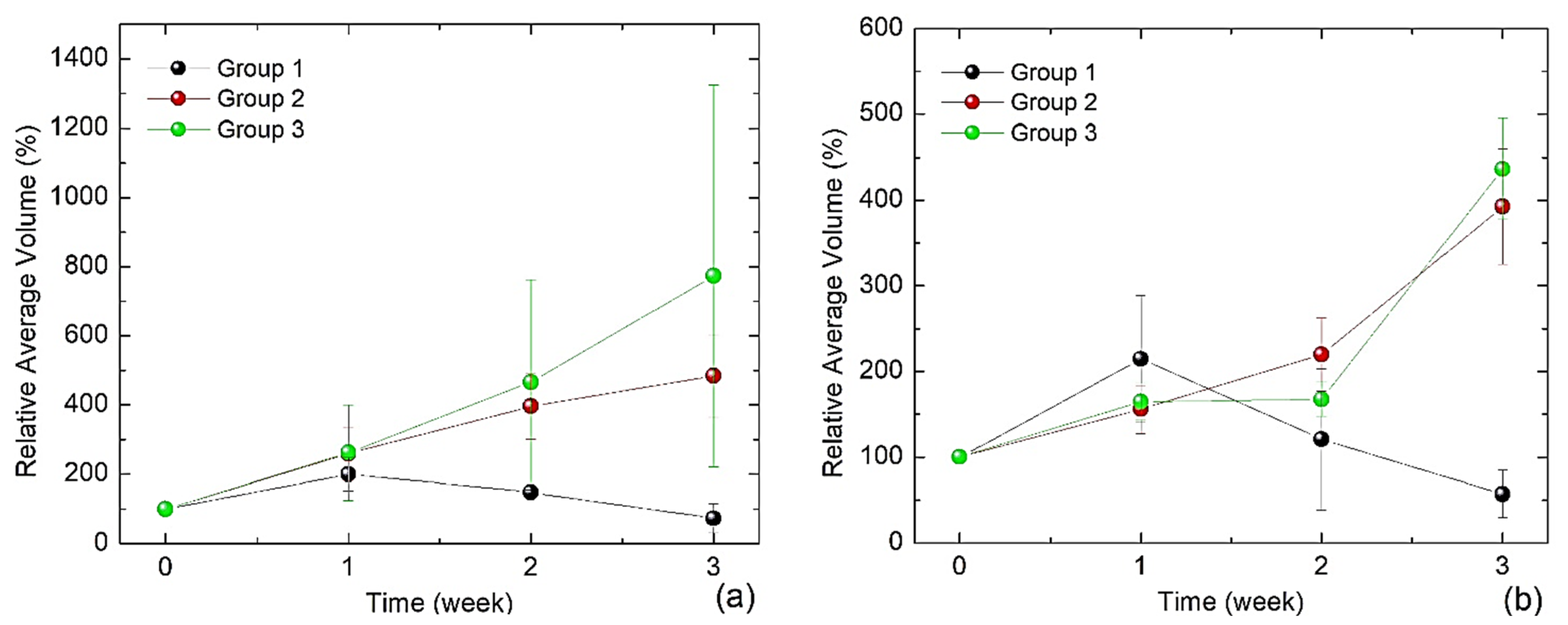
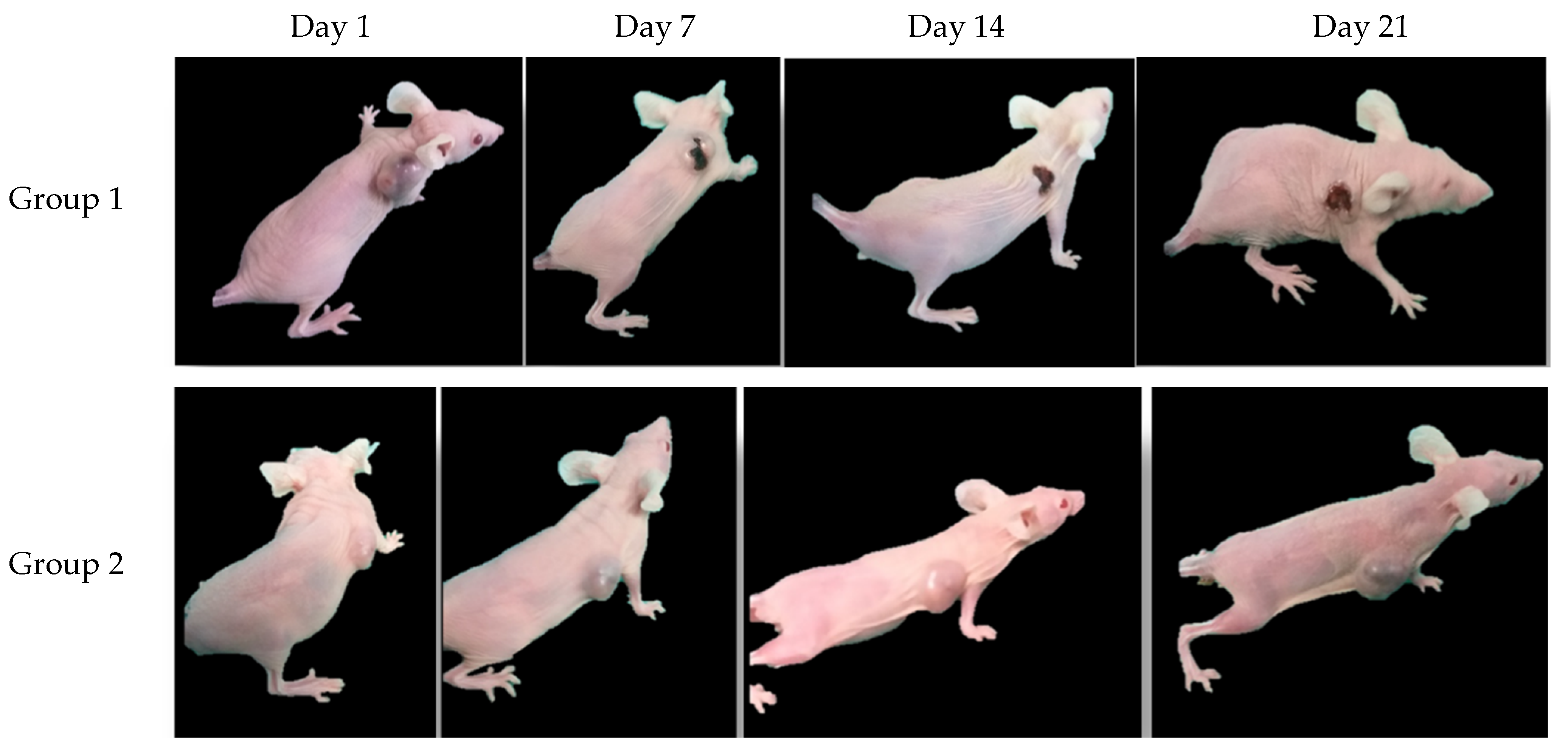
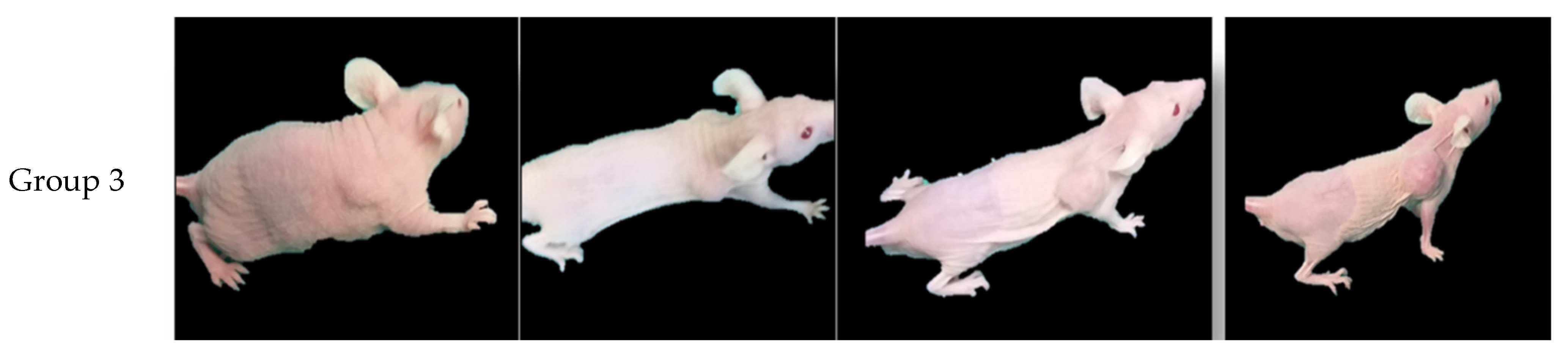
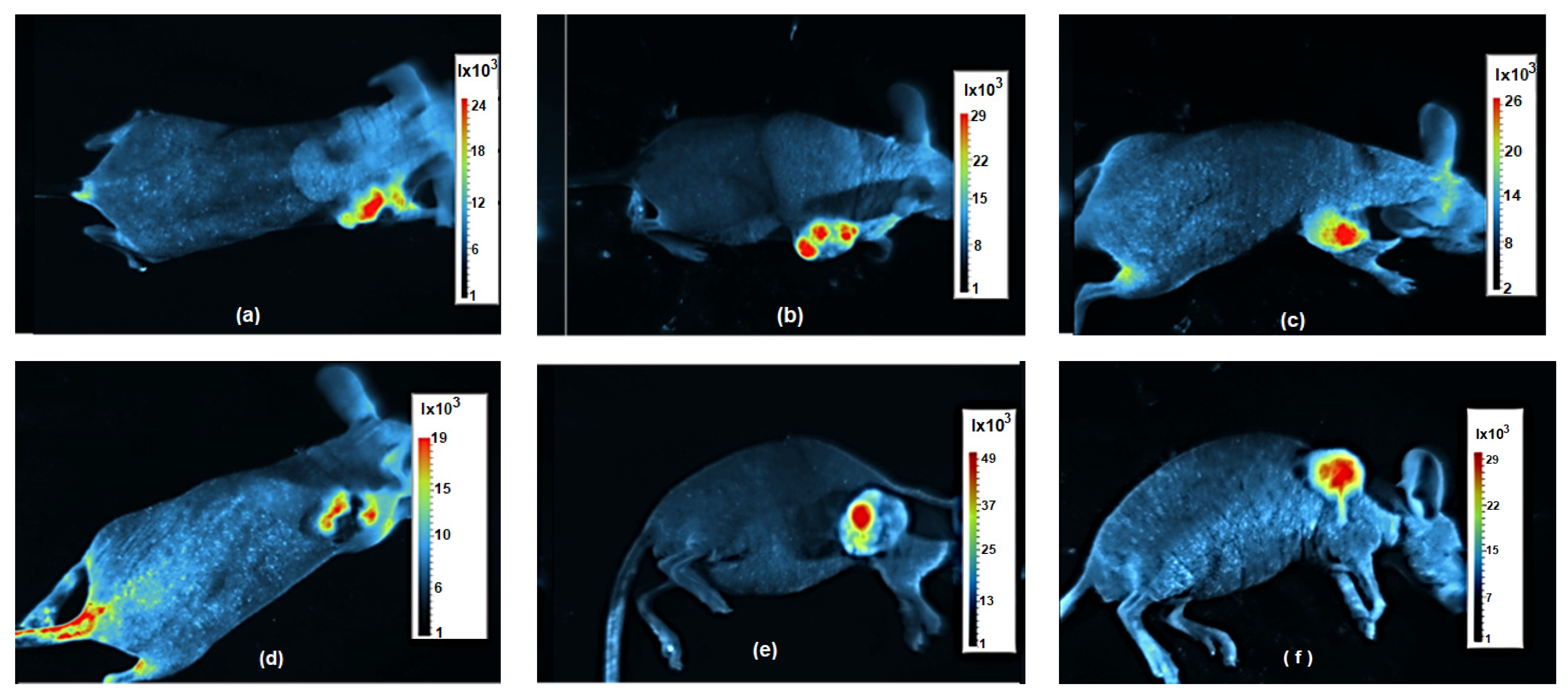
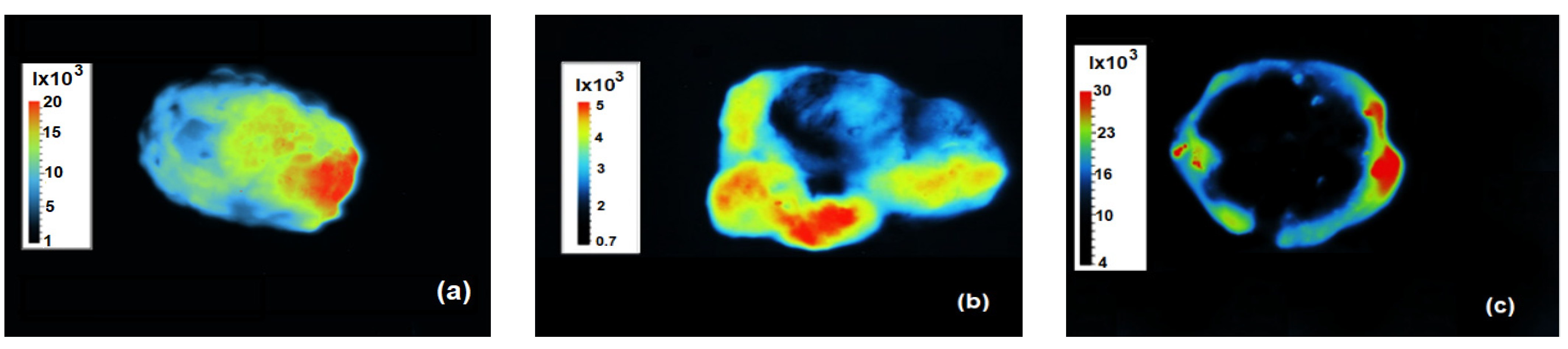
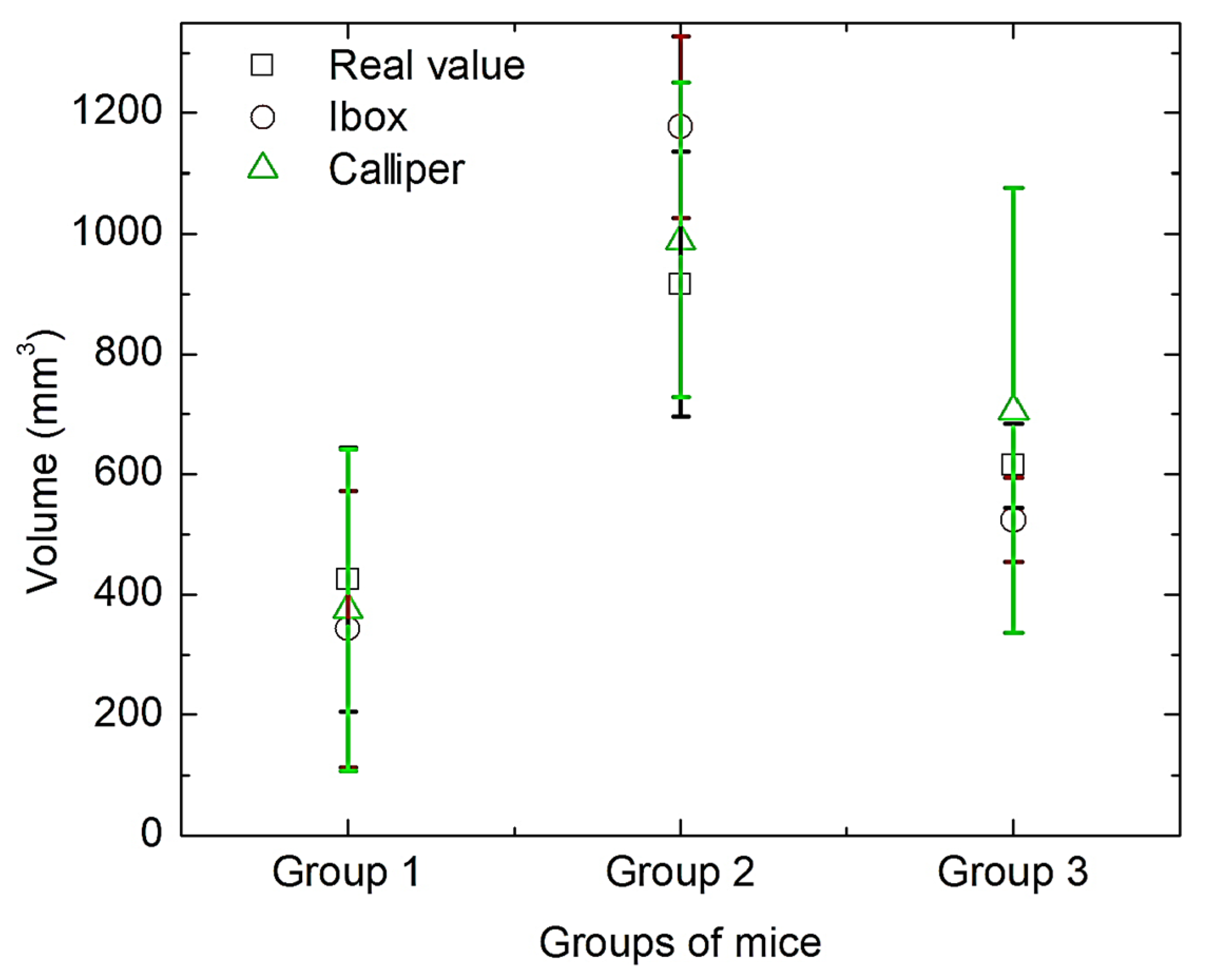
3.3. Results of In Vivo Magnetic Hyperthermia
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Study of Focal Ablation of the Prostate with NanoTherm® Therapy System for Intermediate-Risk Prostate Cancer. Available online: https://clinicaltrials.gov/study/NCT05010759 (accessed on 8 December 2023).
- Peiravi, M.; Eslami, H.; Ansari, M.; Zare-Zardini, H. Magnetic hyperthermia: Potentials and limitations. J. Indian Chem. Soc. 2022, 1, 100269. [Google Scholar] [CrossRef]
- Rubia-Rodríguez, I.; Santana-Otero, A.; Spassov, S.; Tombácz, E.; Johansson, C.; De La Presa, P.; Teran, F.J.; Morales, M.D.; Veintemillas-Verdaguer, S.; Thanh, N.T.; et al. Whither magnetic hyperthermia? A tentative roadmap. Materials 2021, 14, 706. [Google Scholar] [CrossRef] [PubMed]
- Włodarczyk, A.; Gorgoń, S.; Radoń, A.; Bajdak-Rusinek, K. Magnetite nanoparticles in magnetic hyperthermia and cancer therapies: Challenges and perspectives. Nanomaterials 2022, 12, 1807. [Google Scholar] [CrossRef] [PubMed]
- Gavilán, H.; Avugadda, S.K.; Fernández-Cabada, T.; Soni, N.; Cassani, M.; Mai, B.T.; Chantrell, R.; Pellegrino, T. Magnetic nanoparticles and clusters for magnetic hyperthermia: Optimizing their heat performance and developing combinatorial therapies to tackle cancer. Chem. Soc. Rev. 2021, 50, 11614–11667. [Google Scholar] [CrossRef] [PubMed]
- Sun, R.; Chen, H.; Zheng, J.; Yoshitomi, T.; Kawazoe, N.; Yang, Y.; Chen, G. Composite scaffolds of gelatin and Fe3O4 nanoparticles for magnetic hyperthermia-based breast cancer treatment and adipose tissue regeneration. Adv. Healthc. Mater. 2023, 12, 2202604. [Google Scholar] [CrossRef]
- Zhang, Y.; Kohler, N.; Zhang, M. Surface modification of superparamagnetic magnetite nanoparticles and their intracellular uptake. Biomaterials 2002, 23, 1553–1561. [Google Scholar] [CrossRef] [PubMed]
- Mohapatra, S.; Mallick, S.K.; Maiti, T.K.; Ghosh, S.K.; Pramanik, P. Synthesis of highly stable folic acid conjugated magnetite nanoparticles for targeting cancer cells. Nanotechnology 2007, 18, 385102. [Google Scholar] [CrossRef]
- Khan, A.; Niroj, K.S. Folate-Conjugated Magnetite Nanoparticles for Targeted Drug Delivery and Hyperthermia Applications. ChemistrySelect 2022, 7, e202202012. [Google Scholar] [CrossRef]
- Jiang, Q.L.; Zheng, S.W.; Hong, R.Y.; Deng, S.M.; Guo, L.; Hu, R.L.; Gao, B.; Huang, M.; Cheng, L.F.; Liu, G.H.; et al. Folic acid-conjugated Fe3O4 magnetic nanoparticles for hyperthermia and MRI in vitro and in vivo. Appl. Surf. Sci. 2014, 307, 224–233. [Google Scholar] [CrossRef]
- Scialabba, C.; Puleio, R.; Peddis, D.; Varvaro, G.; Calandra, P.; Cassata, G.; Cicero, L.; Licciardi, M.; Giammona, G. Folate targeted coated SPIONs as efficient tool for MRI. Nano Res. 2017, 10, 3212–3227. [Google Scholar] [CrossRef]
- Shah, S.A.; Majeed, A.; Rashid, K.; Awan, S.U. PEG-coated folic acid-modified superparamagnetic MnFe2O4 nanoparticles for hyperthermia therapy and drug delivery. Mater. Chem. Phys. 2013, 138, 703–708. [Google Scholar] [CrossRef]
- Li, J.; Zheng, L.; Cai, H.; Sun, W.; Shen, M.; Zhang, G.; Shi, X. Polyethyleneimine-mediated synthesis of folic acid-targeted iron oxide nanoparticles for in vivo tumor MR imaging. Biomaterials 2013, 34, 8382–8392. [Google Scholar] [CrossRef] [PubMed]
- Hayashi, K.; Moriya, M.; Sakamoto, W.; Yogo, T. Chemoselective synthesis of folic acid− functionalized magnetite nanoparticles via click chemistry for magnetic hyperthermia. Chem. Mater. 2009, 21, 1318–1325. [Google Scholar] [CrossRef]
- Wang, Q.; Cheng, Y.; Wang, W.; Tang, X.; Yang, Y. Polyetherimide-and folic acid-modified Fe3O4 nanospheres for enhanced magnetic hyperthermia performance. J. Biomed. Mater. Res. Part B Appl. Biomater. 2023, 111, 795–804. [Google Scholar] [CrossRef] [PubMed]
- Fakhimikabir, H.; Tavakoli, M.B.; Zarrabi, A.; Amouheidari, A.; Rahgozar, S. Could FA-PG-SPIONs act as a hyperthermia sensitizing agent? An in vitro study. J. Therm. Biol. 2018, 78, 73–83. [Google Scholar] [CrossRef] [PubMed]
- Nikzamir, M.; Abolfazl, A.; Yunes, P. An overview on nanoparticles used in biomedicine and their cytotoxicity. J. Drug Deliv. Sci. Technol. 2021, 61, 102316. [Google Scholar] [CrossRef]
- Cortés-Llanos, B.; Ocampo, S.M.; De la Cueva, L.; Calvo, G.F.; Belmonte-Beitia, J.; Pérez, L.; Gorka, S.; Ayuso-Sacido, Á. Influence of coating and size of magnetic nanoparticles on cellular uptake for in vitro MRI. Nanomaterials 2021, 11, 2888. [Google Scholar] [CrossRef] [PubMed]
- Vilas-Boas, V.; Félix, C.; Begoña, E. Magnetic hyperthermia for cancer treatment: Main parameters affecting the outcome of in vitro and in vivo studies. Molecules 2020, 25, 2874. [Google Scholar] [CrossRef]
- Cervantes, O.; Casillas, N.; Knauth, P.; Lopez, Z.; Virgen-Ortiz, A.; Lozano, O.; Enciso, D.I.M.; Alfonso, H.S.; Saray, R.S.; Luis, M.S.; et al. An easily prepared ferrofluid with high power absorption density and low cytotoxicity for biomedical applications. Mater. Chem. Phys. 2020, 245, 122752. [Google Scholar] [CrossRef]
- Sápi, J.; Kovács, L.; Drexler, D.A.; Kocsis, P.; Gajári, D.; Sápi, Z. Tumor volume estimation and quasi-continuous administration for most effective bevacizumab therapy. PLoS ONE 2015, 10, e0142190. [Google Scholar] [CrossRef]
- Stephanie, D.; Threatta, T.W.; Synoldb, J.W.; Jacqueline, K.B. In vivo anticancer activity of a rhodium metalloinsertorin the HCT116 xenograft tumor model. Proc. Natl. Acad. Sci. USA 2020, 117, 17535–17542. Available online: https://www.pnas.org/doi/epdf/10.1073/pnas.2006569117 (accessed on 2 May 2020).
- Rosales, R.S.; Casillas, N.S.; Topete, A.; Cervantes, O.; González, G.; Paz, J.A.; Cano, M.E. Evaluating physical changes of iron oxide nanoparticles due to surface modification with oleic acid. Chin. Phys. B 2020, 29, 100502. [Google Scholar] [CrossRef]
- Mazon, E.E.; Villa, M.E.; Hernández, S.A.; Córdova, F.T.; Ibarra, J.J.; Calleja, H.A.; Leyva, J.A.; Barrera, A.; Estrada, J.C.; Paz, J.A.; et al. A high-resolution frequency variable experimental setup for studying ferrofluids used in magnetic hyperthermia. Rev. Sci. Instrum. 2017, 88, 084705. [Google Scholar] [CrossRef] [PubMed]
- Ahn, T.; Kim, J.H.; Yang, H.M.; Lee, J.W.; Kim, J.D. Formation pathways of magnetite nanoparticles by coprecipitation method. J. Phys. Chem. C 2012, 116, 6069–6076. [Google Scholar] [CrossRef]
- Parın, F.N.; Ullah, S.; Yıldırım, K.; Hashmi, M.; Kim, I.S. Fabrication and characterization of electrospun folic acid/hybrid fibers: In vitro controlled release study and cytocompatibility assays. Polymers 2021, 13, 3594. [Google Scholar] [CrossRef]
- Cholico, F.A.; Sámano, A.H.; Castañeda, P.R.; Paz, J.A.; Quintero, L.H.; Cano, M.E. Analysis of the magnetic properties of core-shell iron oxide nanoparticles. Rev. Mex. Fís. 2022, 68, 68041004. [Google Scholar] [CrossRef]
- González, A.G.; Casillas, N.; López, Z.; Cervantes, O.; Knauth, P.; Hernández-Gutiérrez, R.; Topete-Camacho, A.; Rosales, S.; Quintero, L.H.; Paz, J.A.; et al. Tetrahydroxyquinone: A Suitable Coating for Ferrofluids Used in Magnetic Hyperthermia. Coatings 2022, 12, 1130. [Google Scholar] [CrossRef]
- Guzmán-Rocha, D.A.; Córdova-Fraga, T.; Bernal-Alvarado, J.J.; López, Z.; Cholico, F.A.; Quintero, L.H.; Paz, J.A.; Cano, M.E. A ferrofluid with high specific absorption rate prepared in a single step using a biopolymer. Materials 2022, 15, 788. [Google Scholar] [CrossRef]


Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rosales, S.; Hernández-Gutiérrez, R.; Oaxaca, A.; López, Z.; Casillas, N.; Knauth, P.; Quintero, L.H.; Paz, J.A.; Cholico, F.; Velásquez, C.; et al. The Fluorescent Cell Line SW620-GFP Is a Valuable Model to Monitor Magnetic Hyperthermia. Bioengineering 2024, 11, 638. https://doi.org/10.3390/bioengineering11070638
Rosales S, Hernández-Gutiérrez R, Oaxaca A, López Z, Casillas N, Knauth P, Quintero LH, Paz JA, Cholico F, Velásquez C, et al. The Fluorescent Cell Line SW620-GFP Is a Valuable Model to Monitor Magnetic Hyperthermia. Bioengineering. 2024; 11(7):638. https://doi.org/10.3390/bioengineering11070638
Chicago/Turabian StyleRosales, Saray, Rodolfo Hernández-Gutiérrez, Alma Oaxaca, Zaira López, Norberto Casillas, Peter Knauth, Luis H. Quintero, José A. Paz, Francisco Cholico, Celso Velásquez, and et al. 2024. "The Fluorescent Cell Line SW620-GFP Is a Valuable Model to Monitor Magnetic Hyperthermia" Bioengineering 11, no. 7: 638. https://doi.org/10.3390/bioengineering11070638






