An Innovative Thermal Imaging Prototype for Precise Breast Cancer Detection: Integrating Compression Techniques and Classification Methods
Abstract
:1. Introduction
2. Related Work
3. Methods and Materials
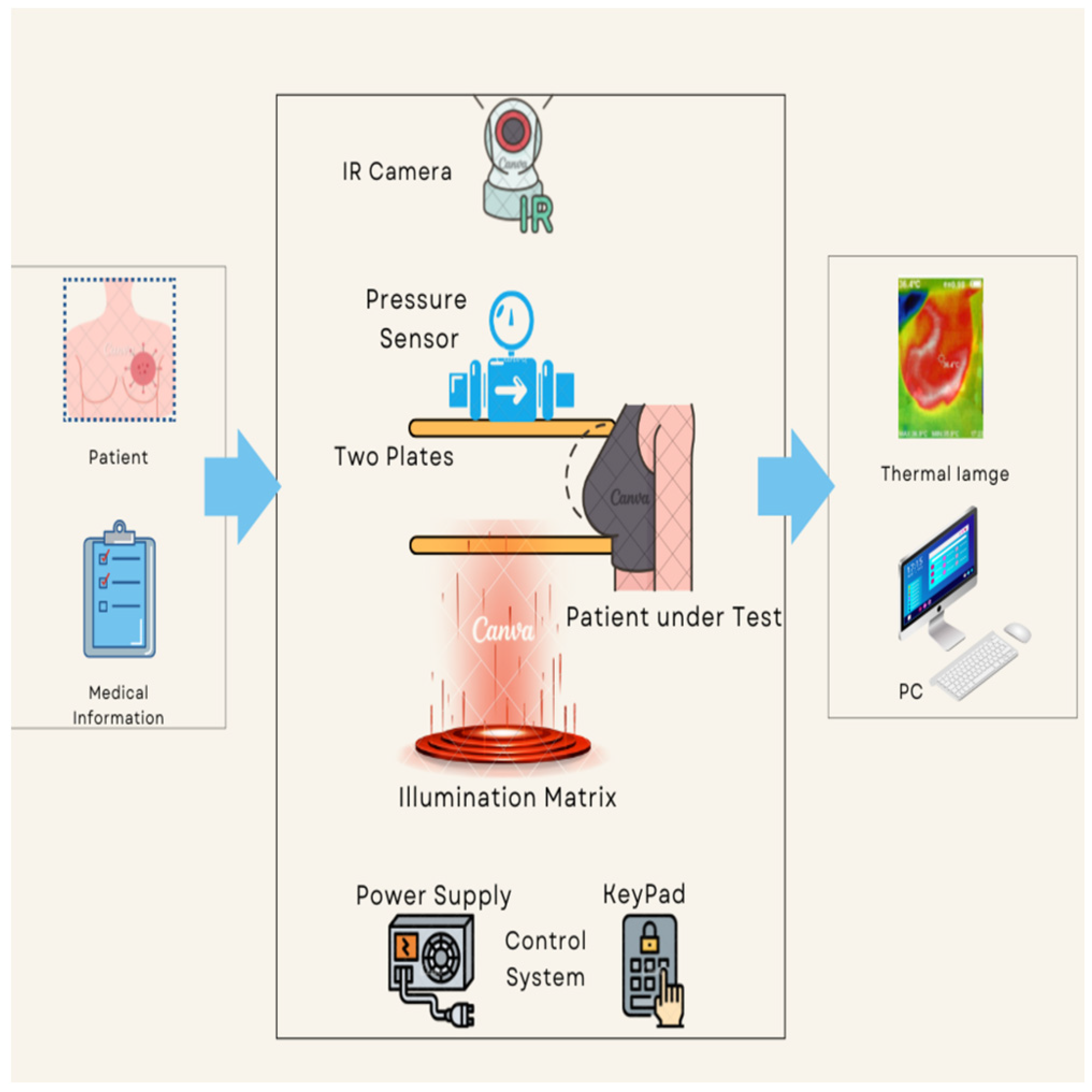
3.1. Design of the Proposed Imaging Prototype
- (a)
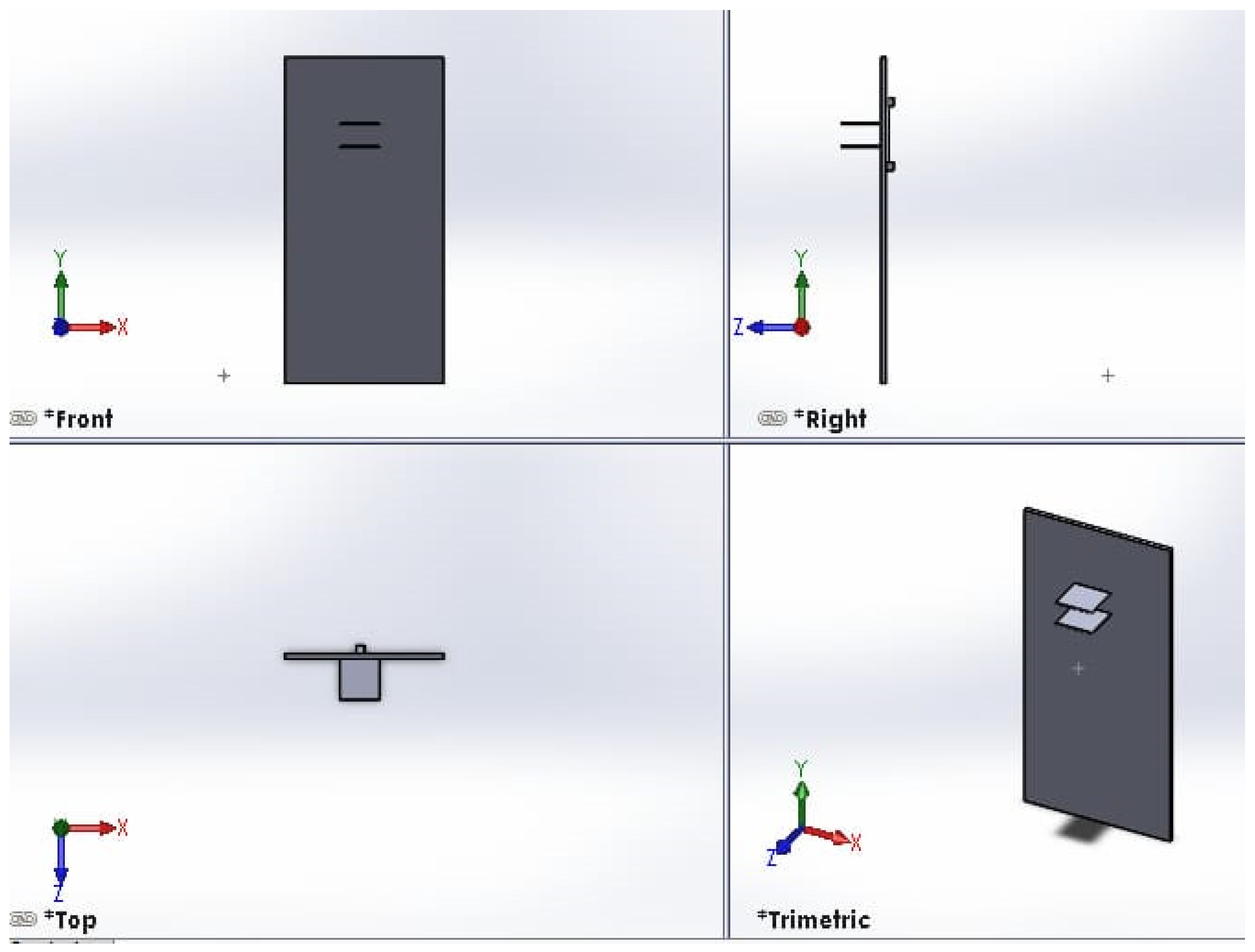
- Equipment body
- (b)
- Plates
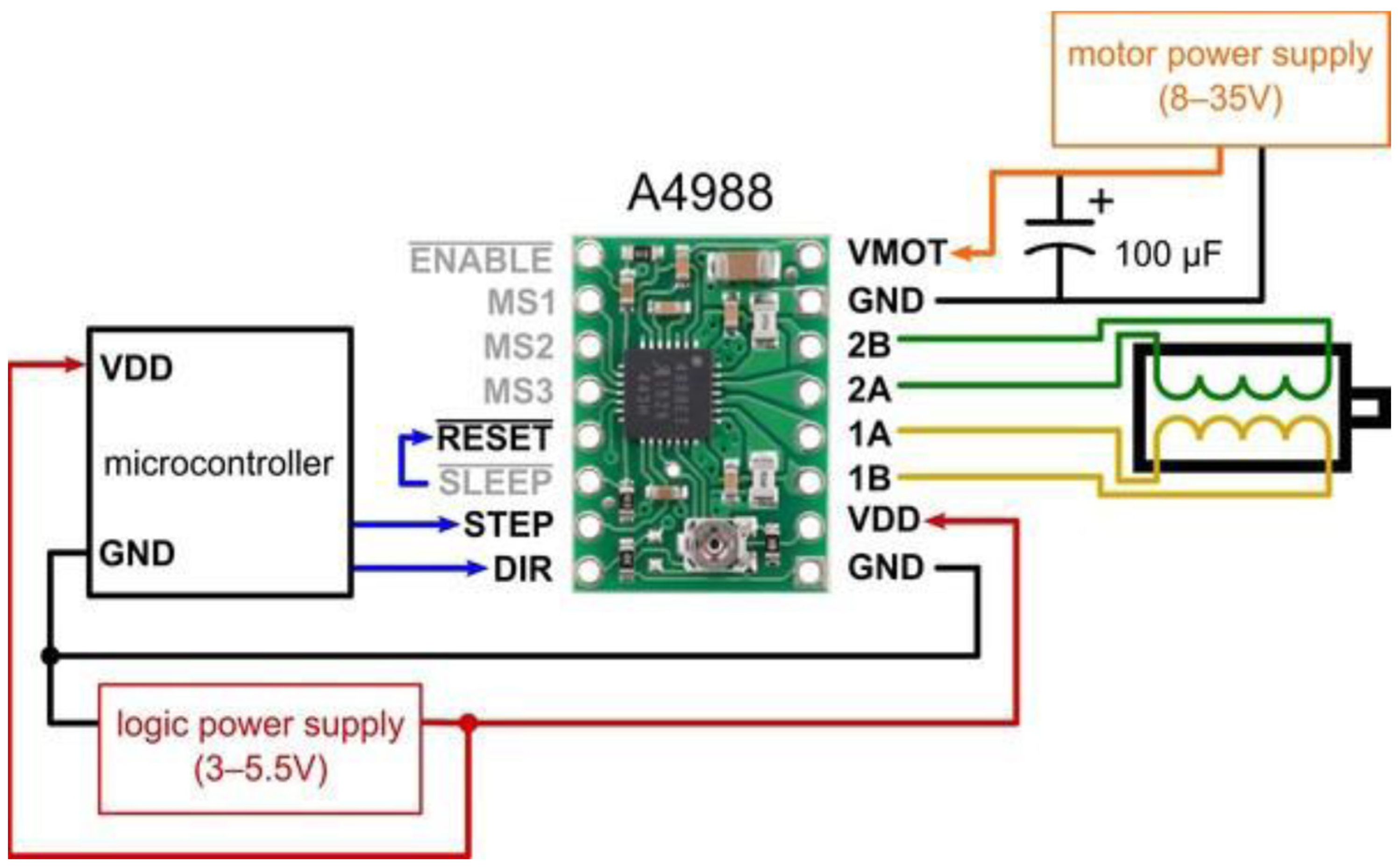
- (c)
- Motors, drivers, and controlling system:
- (d)
- Pressure sensor:
- (e)
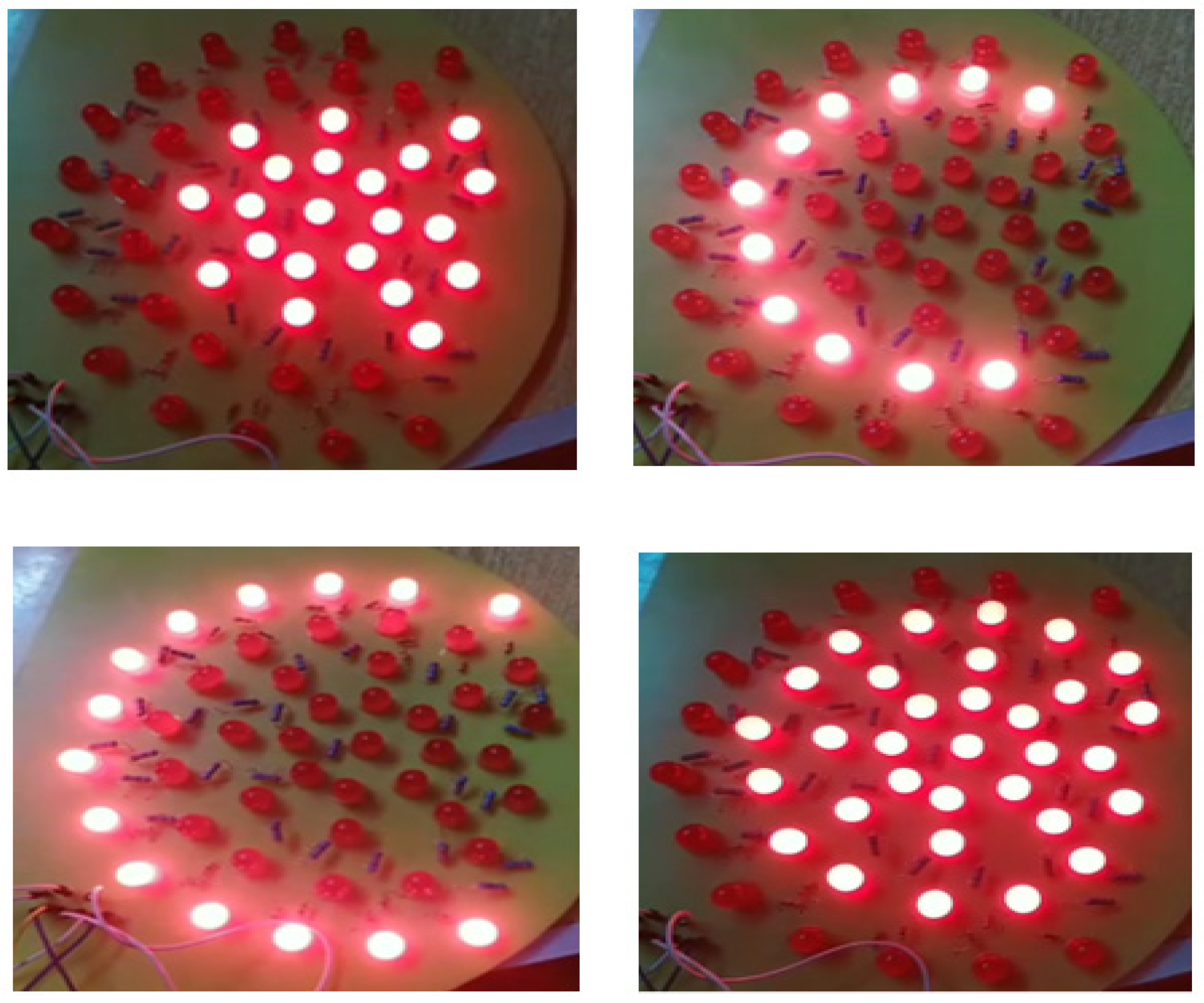
- Illumination source:
- (f)
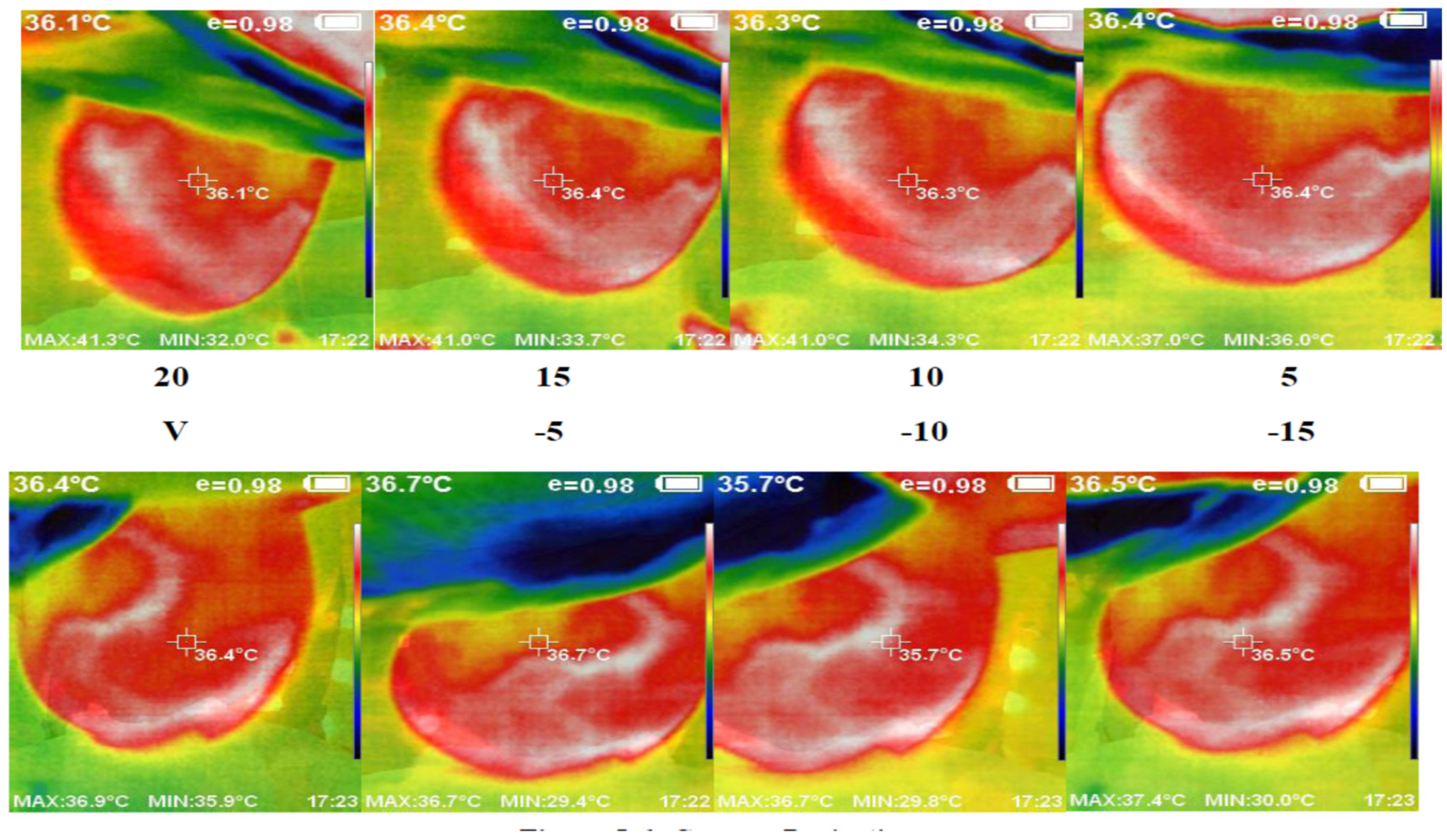
- Thermal camera
- Device distance to examination room light: The proximity of the examination room light to the device can cause unwanted reflections on the surface of the plates, resulting in blurred images. To mitigate this issue, the device must be placed at a sufficient distance, approximately 2 m, from the examination room light or in an indirect location.
- Camera charging percentage: Adequate charging of the camera is crucial to ensuring that the captured images exhibit suitable resolution. We recommend keeping the camera’s battery level above 30%.
- Adjust the size of the LED illumination matrix (or level of LED illumination) appropriately to match the imaged breast area, ensuring that it is smaller than the actual breast size. Using a larger illumination area than the breast area can result in overheating of the breast, leading to completely red thermal images, which in turn leads to incorrect data.
- Camera position: To capture the entire size of the breast, it is important to initially adjust the camera position to be perpendicular to the middle line of the breast. This guarantees the capture of only partial images. The recommended distance between the camera and the breast is within the range of 20–55 cm.
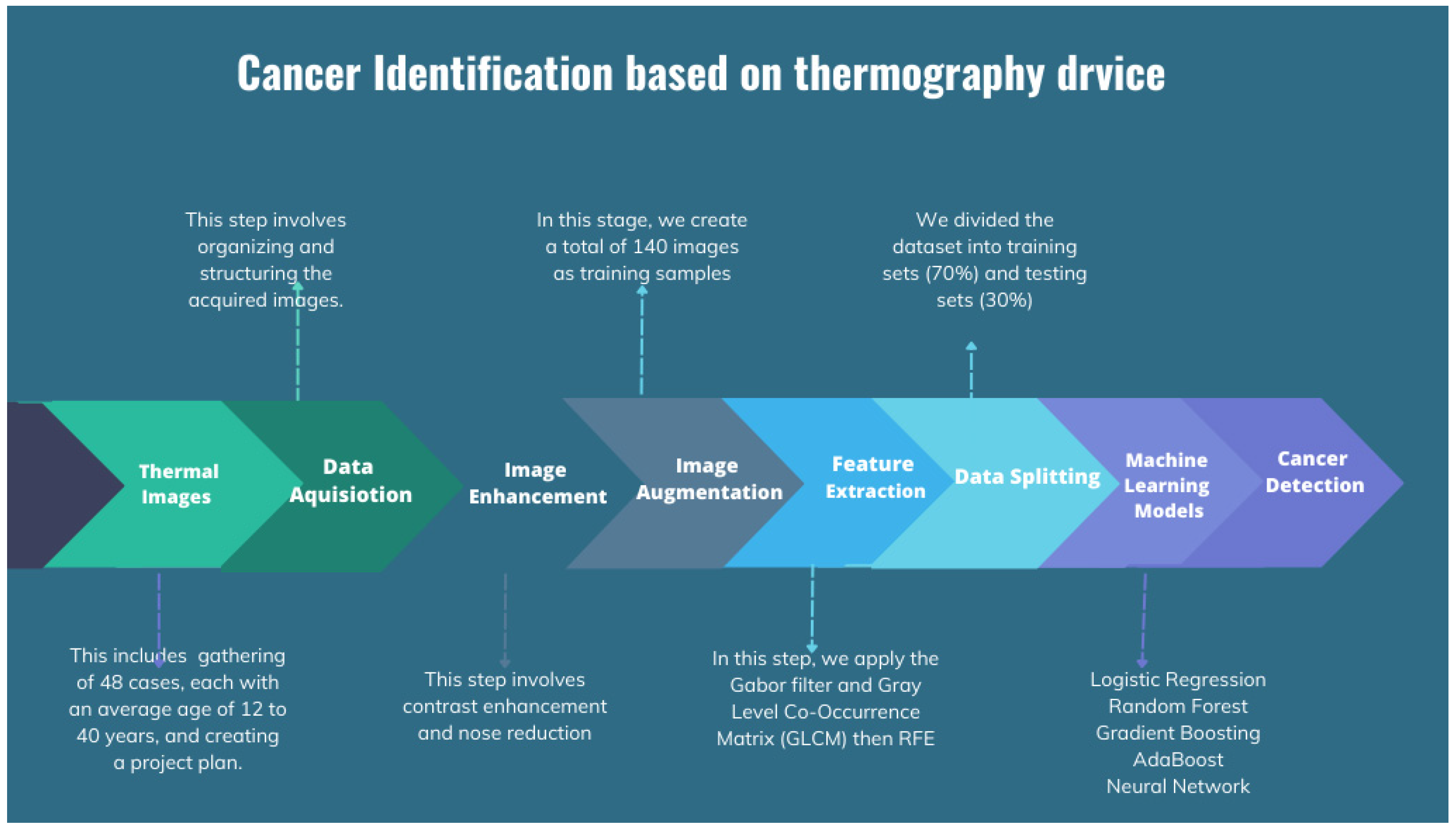
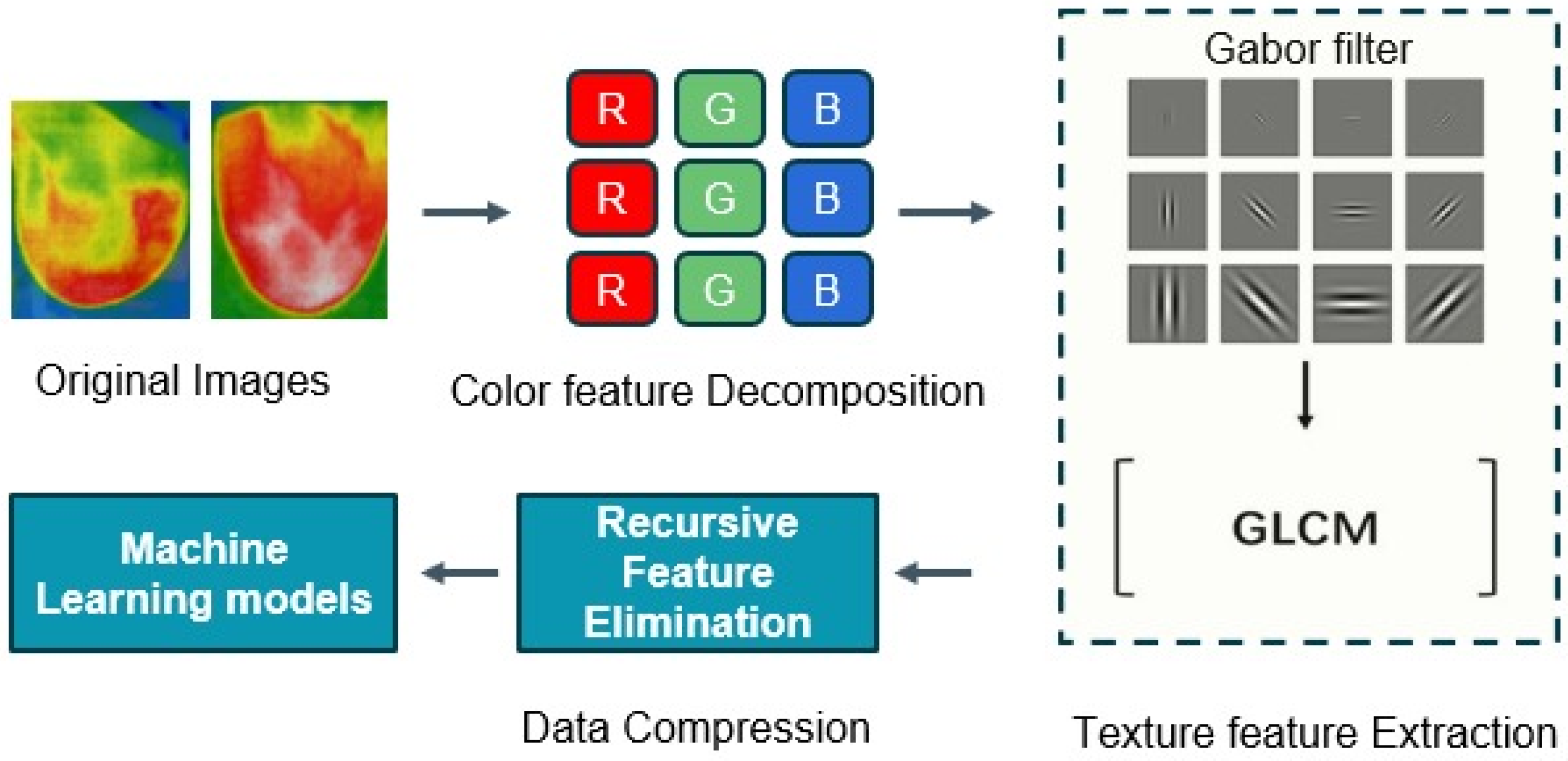
3.2. Classification of the Thermal Images
3.2.1. Data Acquisition and Dataset Description
3.2.2. Data Augmentation
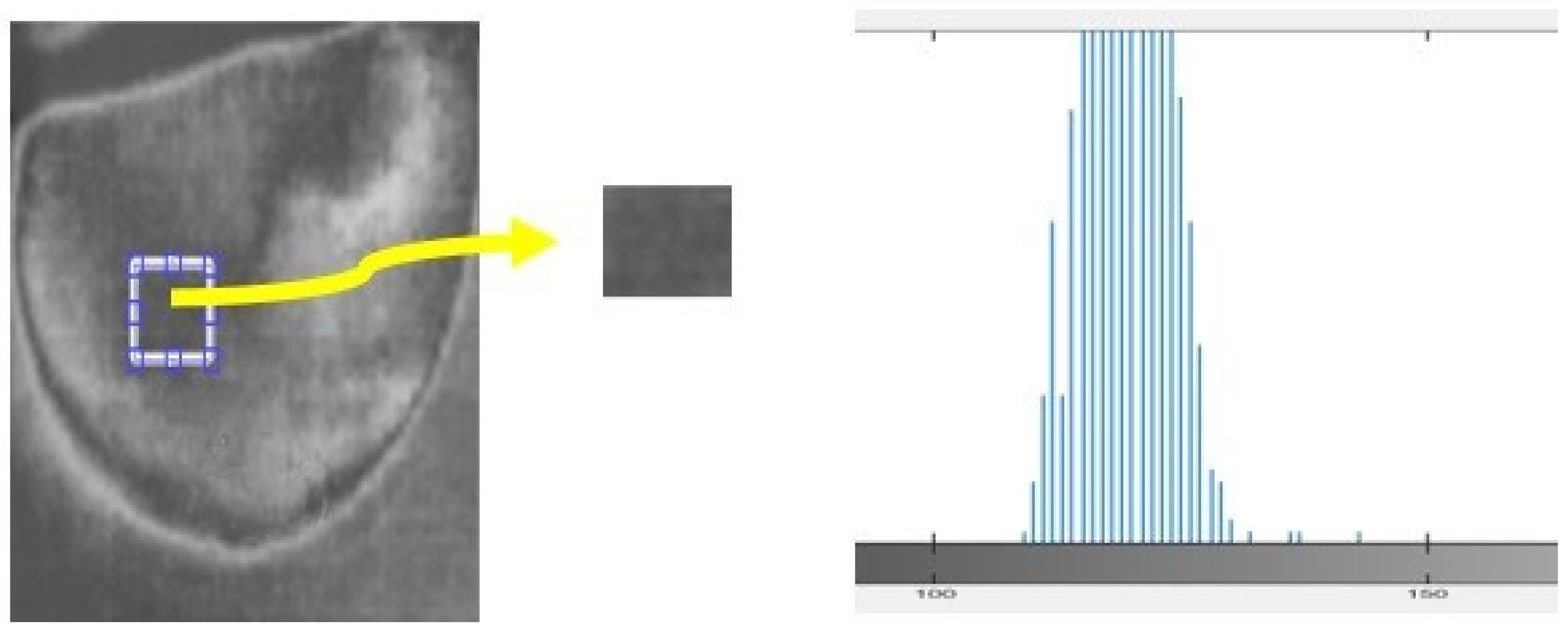
3.2.3. Feature Extraction
Gabor Filter
- Partition each region of interest (ROI) into sub-regions (windows);
- Separately, apply the Gabor filter bank to each window;
- Calculate features (mean, standard deviation, and skewness) based on the magnitude of Gabor filter bank responses.
Gray-Level Co-Occurrence Matrix (GLCM)
Recursive Feature Elimination (RFE)
3.2.4. Image Classification
4. Results and Discussion
5. Conclusions
Author Contributions
Funding
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Miller, K.D.; Ortiz, A.P.; Pinheiro, P.S.; Bandi, P.; Minihan, A.; Fuchs, H.E.; Tyson, D.M.; Tortolero-Luna, G.; Fedewa, S.A.; Jemal, A.M.; et al. Cancer statistics for the US Hispanic/Latino population, 2021. CA Cancer J. Clin. 2021, 71, 466–487. [Google Scholar] [CrossRef] [PubMed]
- Bhushan, A.; Gonsalves, A.; Menon, J.U. Current state of breast cancer diagnosis, treatment, and theranostics. Pharmaceutics 2021, 13, 723. [Google Scholar] [CrossRef] [PubMed]
- Ebeid, N.I. Egyptian Medicine in the Days of the Pharaohs; General Egyptian Book Organization: Cairo, Egypt, 1999. [Google Scholar]
- Siegel, R.L.; Giaquinto, A.N.; Jemal, A. Cancer statistics, 2024. CA Cancer J. Clin. 2024, 74, 12–49. [Google Scholar] [CrossRef] [PubMed]
- Narod, S. Tumour size predicts long-term survival among women with lymph node-positive breast Cancer. Curr. Oncol. 2012, 19, 249–253. [Google Scholar] [CrossRef] [PubMed]
- Chitapanarux, I.; Sripan, P.; Somwangprasert, A.; Charoentum, C.; Onchan, W.; Watcharachan, K.; Wongmaneerung, P.; Kongmebhol, P.; Jia-Mahasap, B.; Huntrakul, L. Stage-specific survival rate of breast cancer patients in northern Thailand in accordance with two different staging systems. Asian Pac. J. Cancer Prev. 2019, 20, 2699–2706. [Google Scholar] [CrossRef]
- Freeman, J.Q.; Li, J.L.; Fisher, S.G.; Yao, K.A.; David, S.P.; Huo, D. Declination of Treatment, Racial and Ethnic Disparity, and Overall Survival in US Patients with Breast Cancer. JAMA Netw. Open 2024, 7, e249449. [Google Scholar] [CrossRef] [PubMed]
- Noh, K.W.; Kim, B.; Choi, C.H.; Kim, T.-J.; Lee, J.-W.; Kim, B.-G.; Bae, D.-S.; Cho, W.K.; Park, W.; Lee, Y.-Y. Effect of waiting time from pathological diagnosis to definitive concurrent chemoradiation for cervical cancer on overall survival. Cancer Res. Treat. 2022, 54, 245–252. [Google Scholar] [CrossRef]
- Yaffe, M.J.; Mainprize, J.G. Risk of radiation-induced breast cancer from mammographic screening. Radiology 2011, 258, 98–105. [Google Scholar] [CrossRef]
- Juanpere, S.; Perez, E.; Huc, O.; Motos, N.; Pont, J.; Pedraza, S. Imaging of breast implants—A pictorial review. Insights Imaging 2011, 2, 653–670. [Google Scholar] [CrossRef]
- Iranmakani, S.; Mortezazadeh, T.; Sajadian, F.; Ghaziani, M.F.; Ghafari, A.; Khezerloo, D.; Musa, A.E. A review of various modalities in breast imaging: Technical aspects and clinical outcomes. Egypt. J. Radiol. Nucl. Med. 2020, 51, 1–22. [Google Scholar] [CrossRef]
- Hovda, T.; Tsuruda, K.; Hoff, S.R.; Sahlberg, K.K.; Hofvind, S. Radiological review of prior screening mammograms of screen-detected breast cancer. Eur. Radiol. 2021, 31, 2568–2579. [Google Scholar] [CrossRef] [PubMed]
- Gonzalez-Hernandez, J.-L.; Recinella, A.N.; Kandlikar, S.G.; Dabydeen, D.; Medeiros, L.; Phatak, P. Technology, application and potential of dynamic breast thermography for the detection of breast cancer. Int. J. Heat Mass Transf. 2018, 131, 558–573. [Google Scholar] [CrossRef]
- Mohamed, S.E.; Mohamed, W.A.; Abdelhalim, M.B.; Ahmed, K.E. Advanced enhancement techniques for breast cancer classification in mammographic images. Open Biomed. Eng. J. 2022, 16, e187412072209200. [Google Scholar] [CrossRef]
- Arabi, E.M.; Mohra, A.S.; Ahmed, K.S. High Accuracy Diagnosis for MRI Imaging of Alzheimer’s Disease using Xgboost. Open Biotechnol. J. 2022, 16, e187407072208300. [Google Scholar] [CrossRef]
- Boca, I.; Ciurea, A.I.; Ciortea, C.A.; Dudea, S.M. Pros and cons for automated breast ultrasound (ABUS): A narrative review. J. Pers. Med. 2021, 11, 703. [Google Scholar] [CrossRef] [PubMed]
- Singh, D.; Singh, A.K. Role of image thermography in early breast cancer detection-Past, present and future. Comput. Methods Programs Biomed. 2020, 183, 105074. [Google Scholar] [CrossRef] [PubMed]
- Owen, R.; Ramlakhan, S. Infrared thermography in paediatrics: A narrative review of clinical use. BMJ Paediatr. Open 2017, 1, e000080. [Google Scholar] [CrossRef]
- Lawson, M.B.; Partridge, S.C.; Hippe, D.S.; Rahbar, H.; Lam, D.L.; Lee, C.I.; Lowry, K.P.; Scheel, J.R.; Parsian, S.; Li, I.; et al. Comparative performance of contrast-enhanced mammography, abbreviated breast MRI, and standard breast MRI for breast cancer screening. Radiology 2023, 308, e230576. [Google Scholar] [CrossRef] [PubMed]
- Lataste, J.-F.; Nilsson, L.-O. Infrared thermography. In Methods of Measuring Moisture in Building Materials and Structures: State-of-the-Art Report of the RILEM Technical Committee 248-MMB; Springer: Cham, Switzerland, 2018; pp. 49–54. [Google Scholar]
- Rakhunde, M.B.; Gotarkar, S.; Choudhari, S.G. Thermography as a breast cancer screening technique: A review article. Cureus 2022, 14, e31251. [Google Scholar] [CrossRef] [PubMed]
- Li, Y.; Zhao, J.; Lv, Z.; Pan, Z. Multimodal Medical Supervised Image Fusion Method by CNN. Front. Neurosci. 2021, 15, 638976. Available online: https://www.frontiersin.org/article/10.3389/fnins.2021.638976 (accessed on 24 June 2024). [CrossRef]
- Sahu, A.; Das, P.K.; Meher, S. An efficient deep learning scheme to detect breast cancer using mammogram and ultrasound breast images. Biomed. Signal Process. Control 2024, 87, 105377. [Google Scholar] [CrossRef]
- Barr, L.; Alamer, M.; Darbre, P.D. Measurement of concentrations of four chemical ultraviolet filters in human breast tissue at serial locations across the breast. J. Appl. Toxicol. 2018, 38, 1112–1120. [Google Scholar] [CrossRef] [PubMed]
- Zuluaga-Gomez, J.; Al Masry, Z.; Benaggoune, K.; Meraghni, S.; Zerhouni, N. A CNN-based methodology for breast cancer diagnosis using thermal images. Comput. Methods Biomech. Biomed. Eng. Imaging Vis. 2021, 9, 131–145. [Google Scholar] [CrossRef]
- Mammoottil, M.J.; Kulangara, L.J.; Cherian, A.S.; Mohandas, P.; Hasikin, K.; Mahmud, M. Detection of breast cancer from five-view thermal images using convolutional neural networks. J. Healthc. Eng. 2022, 2022, 295221. [Google Scholar] [CrossRef]
- Mishra, S.; Prakash, A.; Roy, S.K.; Sharan, P.; Mathur, N. Breast cancer detection using thermal images and deep learning. In Proceedings of the 7th International Conference on Computing for Sustainable Global Development (INDIACom), New Delhi, India, 12–14 March 2020; IEEE: New York, NY, USA, 2020; pp. 211–216. [Google Scholar]
- Zadeh, H.G.; Montazeri, A.; Kazerouni, I.A.; Haddadnia, J. Clustering and screening for breast cancer on thermal images using a combination of SOM and MLP. Comput. Methods Biomech. Biomed. Eng. Imaging Vis. 2017, 5, 68–76. [Google Scholar] [CrossRef]
- Prinzi, F.; Insalaco, M.; Orlando, A.; Gaglio, S.; Vitabile, S. A YOLO-based model for breast cancer detection in mammograms. Cognit. Comput. 2024, 16, 107–120. [Google Scholar] [CrossRef]
- Kesztyüs, D.; Brucher, S.; Wilson, C.; Kesztyüs, T. Use of Infrared Thermography in Medical Diagnosis, Screening, and Disease Monitoring: A Scoping Review. Medicina 2023, 59, 2139. [Google Scholar] [CrossRef] [PubMed]
- Kurowski, P. Engineering Analysis with SolidWorks Simulation 2013; SDC Publications: Mission, KS, USA, 2013. [Google Scholar]
- Giovanelli, D.; Farella, E. Force sensing resistor and evaluation of technology for wearable body pressure sensing. J. Sens. 2016, 2016, 391850. [Google Scholar] [CrossRef]
- Cardone, D.; Merla, A. New frontiers for applications of thermal infrared imaging devices: Computational psychopshysiology in the neurosciences. Sensors vol. 2017, 17, 1042. [Google Scholar] [CrossRef]
- Pawar, S.D.; Sharma, K.K.; Sapate, S.G.; Yadav, G.Y. Segmentation of pectoral muscle from digital mammograms with depth-first search algorithm towards breast density classification. Biocybern. Biomed. Eng. 2021, 41, 1224–1241. [Google Scholar] [CrossRef]
- Xu, M.; Yoon, S.; Fuentes, A.; Park, D.S. A comprehensive survey of image augmentation techniques for deep learning. Pattern Recognit. 2023, 137, 109347. [Google Scholar] [CrossRef]
- Hussain, M.; Khan, S.; Muhammad, G.; Ahmad, I.; Bebis, G. Effective extraction of Gabor features for false positive reduction and mass classification in mammography. Appl. Math. 2014, 8, 397–412. [Google Scholar]
- Muzaffar, A.W.; Riaz, F.; Abuain, T.; Abu-Ain, W.A.K.; Hussain, F.; Farooq, M.U.; Azad, M.A. Gabor contrast patterns: A novel framework to extract features from texture images. IEEE Access 2023, 11, 60324–60334. [Google Scholar] [CrossRef]
- Zou, X.; Hu, Y.; Tian, Z.; Shen, K. Logistic regression model optimization and case analysis. In Proceedings of the IEEE 7th International Conference on Computer Science and Network Technology (ICCSNT), Dalian, China, 19–20 October 2019; IEEE: New York, NY, USA, 2019; pp. 135–139. [Google Scholar]
- Minnoor, M.; Baths, V. Diagnosis of breast cancer using random forests. Procedia Comput. Sci. 2023, 218, 429–437. [Google Scholar] [CrossRef]
- Mienye, I.D.; Sun, Y. A survey of ensemble learning: Concepts, algorithms, applications, and prospects. IEEE Access 2022, 10, 99129–99149. [Google Scholar] [CrossRef]
- Dinakaran, S.; Thangaiah, P.R.J. Ensemble method of effective AdaBoost algorithm for decision tree classifiers. Int. J. Artif. Intell. Tools 2017, 26, 1750007. [Google Scholar] [CrossRef]
- Sherif, F.F.; Ahmed, K.S. A Machine Learning Approach for Stroke Differential Diagnosis by Blood Biomarkers. J. Adv. Inf. Technol. 2024, 15, 1–9. [Google Scholar] [CrossRef]
- Alzubaidi, L.; Zhang, J.; Humaidi, A.J.; Al-Dujaili, A.; Duan, Y.; Al-Shamma, O.; Santamaría, J.; Fadhel, M.A.; Al-Amidie, M.; Farhan, L. Review of deep learning: Concepts, CNN architectures, challenges, applications, future directions. J. Big Data 2021, 8, 53. [Google Scholar] [CrossRef]


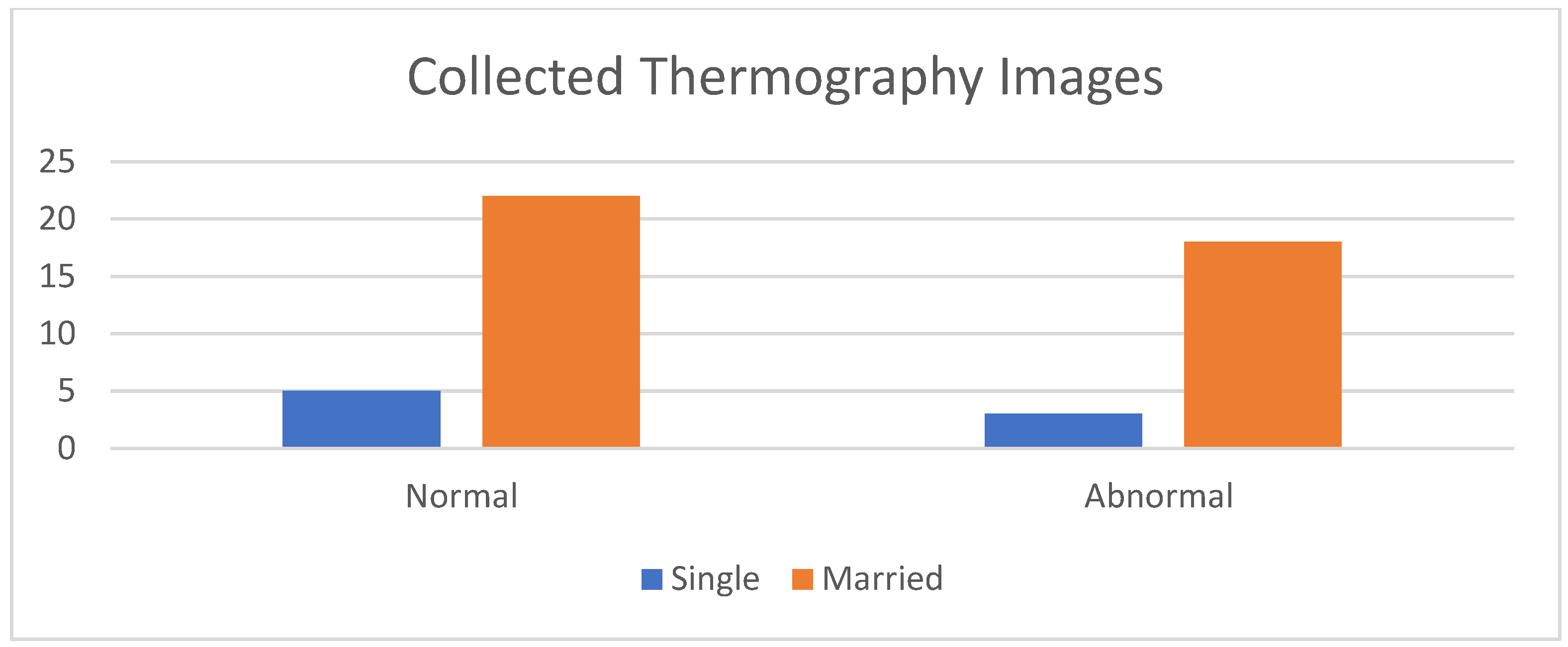



| Case No. | Age | Imaged Breast | Marital Status | Presence of Children | Imaging Modalities | Experts’ Diagnosis |
|---|---|---|---|---|---|---|
| 1 | 33 | Left | Married | 1 | No | Abnormal |
| 2 | 39 | Left | Married | 2 | Mammo | Normal |
| 3 | 39 | Right | Married | 1 | Mammo | Abnormal |
| 4 | 41 | Right | Single | 0 | No | Normal |
| 5 | 46 | Left | Married | 1 | No | Normal |
| 6 | 40 | Right | Married | 0 | Mammo, US | Abnormal |
| 7 | 38 | Left | Single | 0 | No | Normal |
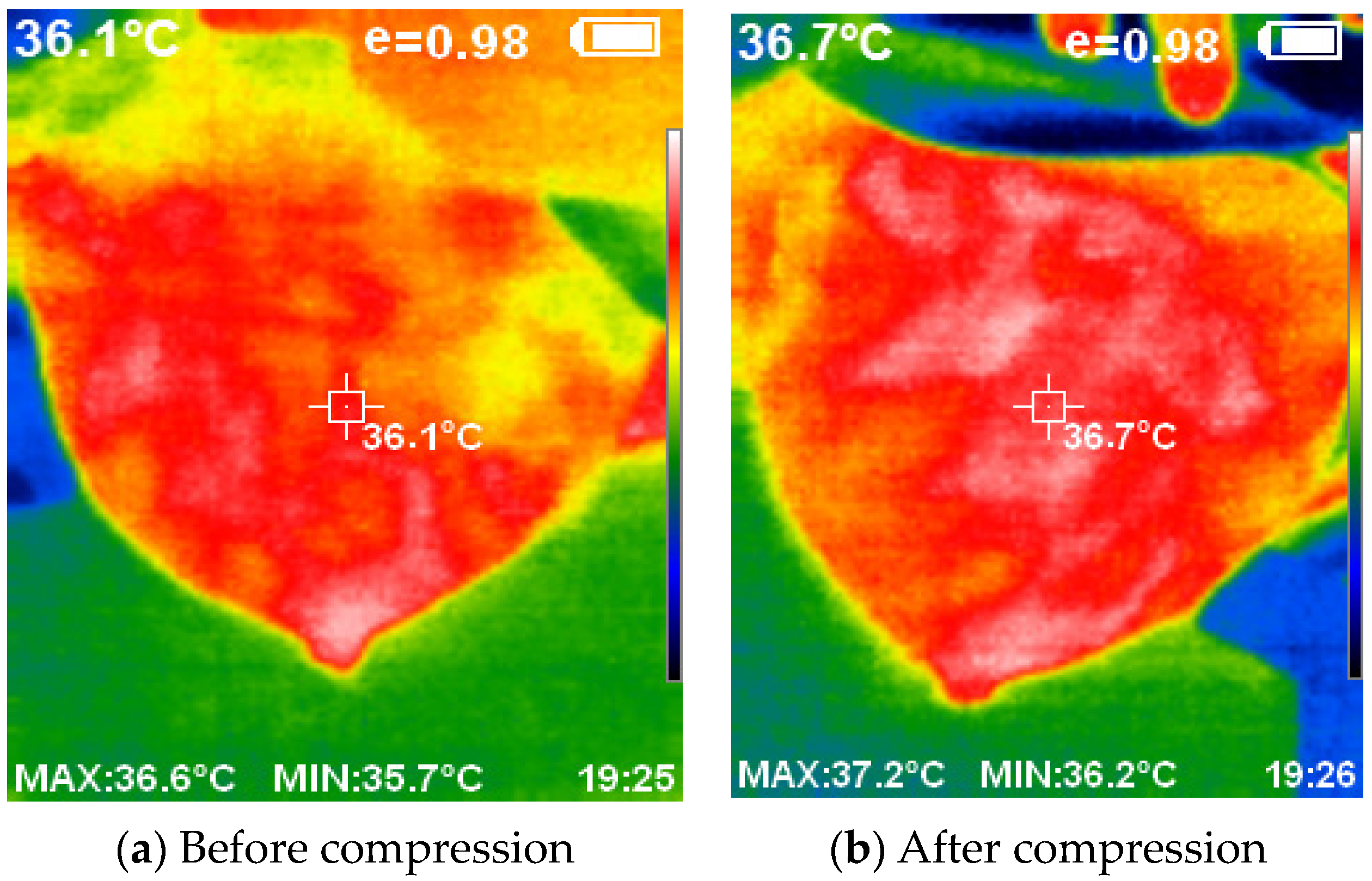
| Performance Measure | Gaussian | Weiner | Median |
|---|---|---|---|
| Mean square error (MSE) | 0.218 | 6.35 | 62.72 |
| Peak signal-to-noise ratio (PSNR) | 54.735 | 40.09 | 30.156 |
| Model | CA | F1-Score | Precision | Recall |
|---|---|---|---|---|
| Logistic Regression | 0.976 | 0.977 | 1.000 | 0.995 |
| Random Forest | 0.883 | 0.864 | 0.946 | 0.795 |
| Gradient Boosting | 0.830 | 0.826 | 0.792 | 0.864 |
| AdaBoost | 0.777 | 0.769 | 0.745 | 0.795 |
| Neural Network | 0.947 | 0.943 | 0.953 | 0.932 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ahmed, K.S.; Sherif, F.F.; Abdallah, M.S.; Cho, Y.-I.; ElMetwally, S.M. An Innovative Thermal Imaging Prototype for Precise Breast Cancer Detection: Integrating Compression Techniques and Classification Methods. Bioengineering 2024, 11, 764. https://doi.org/10.3390/bioengineering11080764
Ahmed KS, Sherif FF, Abdallah MS, Cho Y-I, ElMetwally SM. An Innovative Thermal Imaging Prototype for Precise Breast Cancer Detection: Integrating Compression Techniques and Classification Methods. Bioengineering. 2024; 11(8):764. https://doi.org/10.3390/bioengineering11080764
Chicago/Turabian StyleAhmed, Khaled S., Fayroz F. Sherif, Mohamed S. Abdallah, Young-Im Cho, and Shereen M. ElMetwally. 2024. "An Innovative Thermal Imaging Prototype for Precise Breast Cancer Detection: Integrating Compression Techniques and Classification Methods" Bioengineering 11, no. 8: 764. https://doi.org/10.3390/bioengineering11080764
APA StyleAhmed, K. S., Sherif, F. F., Abdallah, M. S., Cho, Y.-I., & ElMetwally, S. M. (2024). An Innovative Thermal Imaging Prototype for Precise Breast Cancer Detection: Integrating Compression Techniques and Classification Methods. Bioengineering, 11(8), 764. https://doi.org/10.3390/bioengineering11080764







