Dual Transverse Arch Foot Orthosis Improves Gait Biomechanics in Females with Flexible Flatfoot
Abstract
1. Introduction
2. Materials and Methods
2.1. Subject Recruitment
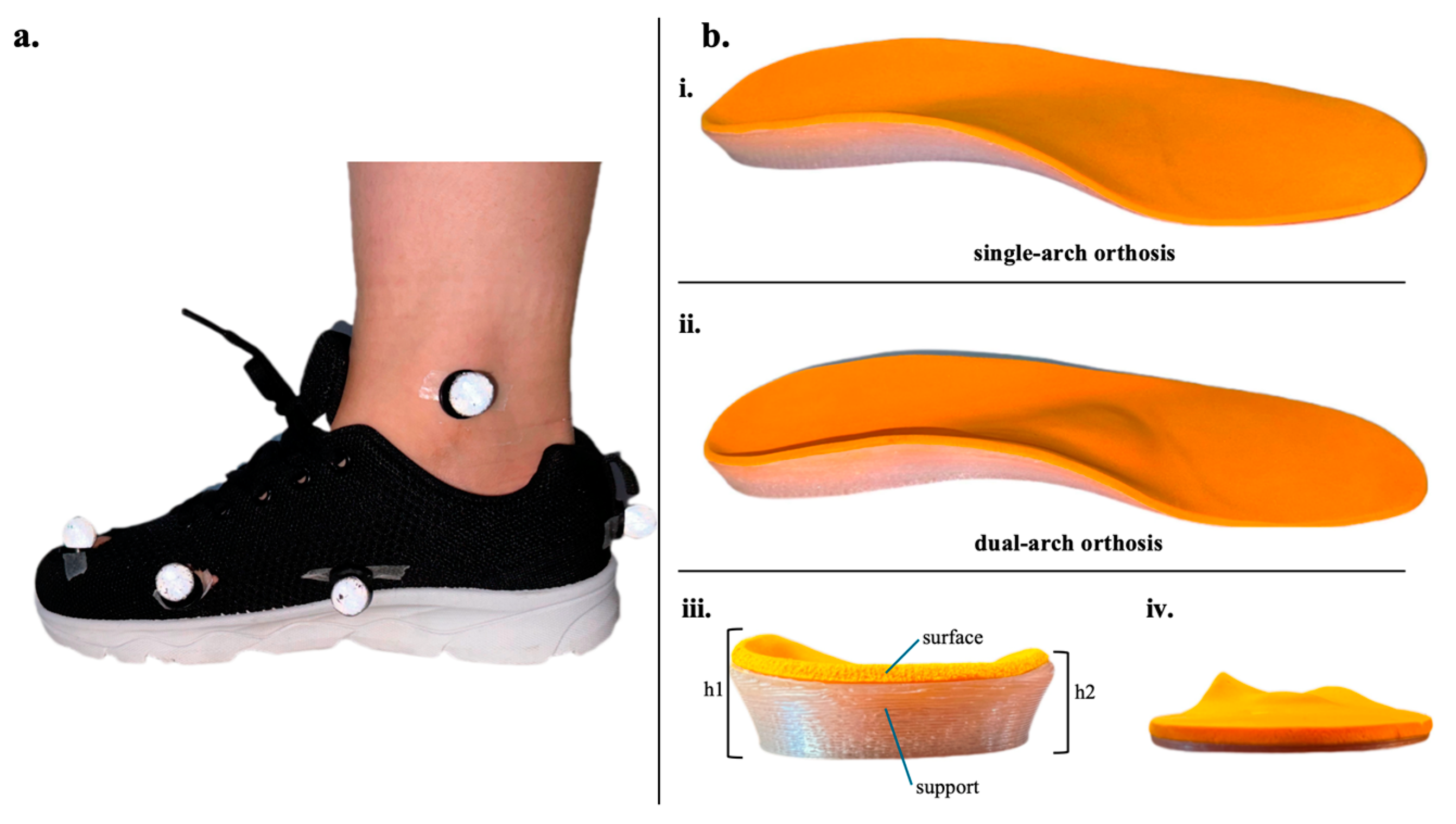
2.2. Foot Orthoses
2.3. Experimental Design
2.3.1. Kinematic and Kinetic Data Collection
2.3.2. Radiographic Analysis
2.4. Data Processing
2.5. Statistical Analysis
3. Results
3.1. Kinematics
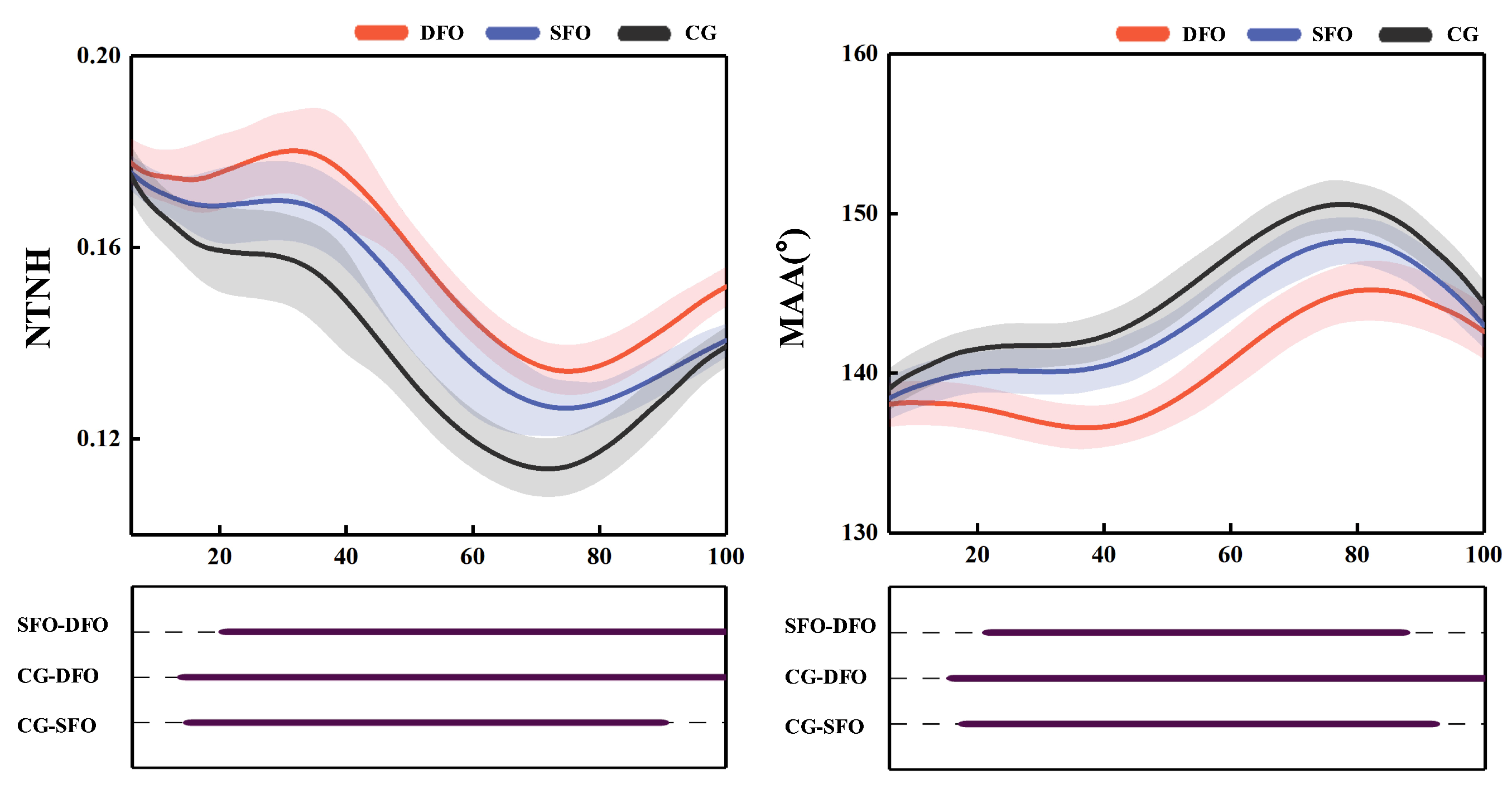
3.1.1. Normalized Truncated Navicular Height (NTNH)
3.1.2. Medial Arch Angle (MAA)
3.1.3. Lower Limb Position
3.2. Kinetics
3.2.1. Vertical Ground Reaction Force (vGRF)
3.2.2. Lower Limb Moments
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| SFO | single-arch foot orthoses |
| DFO | dual-arch foot orthoses |
| ROM | range of motion |
| FOs | foot orthoses |
| DFIS | dual fluoroscopic imaging system |
| vGRF | vertical ground reaction force |
| NTNH | normalized truncated navicular height |
| MAA | medial arch angle |
| SD | standard deviation |
References
- Ker, R.; Bennett, M.; Bibby, S.; Kester, R.; Alexander, R.M. The spring in the arch of the human foot. Nature 1987, 325, 147–149. [Google Scholar] [CrossRef] [PubMed]
- Zelik, K.E.; Kuo, A.D. Human walking isn’t all hard work: Evidence of soft tissue contributions to energy dissipation and return. J. Exp. Biol. 2010, 213, 4257–4264. [Google Scholar] [CrossRef] [PubMed]
- Bojsen-Møller, F. Calcaneocuboid joint and stability of the longitudinal arch of the foot at high and low gear push off. J. Anat. 1979, 129, 165. [Google Scholar] [PubMed]
- Gwani, A.S.; Asari, M.A.; Mohd Ismail, Z.I. How the three arches of the foot intercorrelate. Folia Morphol. 2017, 76, 682–688. [Google Scholar] [CrossRef] [PubMed]
- Venkadesan, M.; Yawar, A.; Eng, C.M.; Dias, M.A.; Singh, D.K.; Tommasini, S.M.; Haims, A.H.; Bandi, M.M.; Mandre, S.; Venkadesan, M.; et al. Stiffness of the human foot and evolution of the transverse arch. Nature 2020, 579, 97–100. [Google Scholar] [CrossRef]
- Hicks, J. The plantar aponeurosis and the arch. J. Anat. 1954, 88, 25–30. [Google Scholar] [PubMed]
- Atik, A.; Ozyurek, S. Flexible flatfoot. N. Clin. Istanb. 2014, 1, 57. [Google Scholar] [CrossRef]
- Deland, J.T.; de Asla, R.J.; Sung, I.H.; Ernberg, L.A.; Potter, H.G. Posterior tibial tendon insufficiency: Which ligaments are involved? Foot Ankle Int. 2005, 26, 427–435. [Google Scholar] [CrossRef]
- Cheng, K.-W.; Peng, Y.; Chen, T.L.-W.; Zhang, G.; Cheung, J.C.-W.; Lam, W.-K.; Wong, D.W.-C.; Zhang, M. A three-dimensional printed foot orthosis for flexible flatfoot: An exploratory biomechanical study on arch support reinforcement and undercut. Materials 2021, 14, 5297. [Google Scholar] [CrossRef]
- Chinpeerasathian, C.; Sin Oo, P.; Siriphorn, A.; Pensri, P. Effect of foot orthoses on balance among individuals with flatfoot: A systematic review and meta-analysis. PLoS ONE 2024, 19, e0299446. [Google Scholar] [CrossRef]
- Van Boerum, D.H.; Sangeorzan, B.J. Biomechanics and pathophysiology of flat foot. Foot Ankle Clin. 2003, 8, 419–430. [Google Scholar] [CrossRef] [PubMed]
- Saraswat, P.; MacWilliams, B.A.; Davis, R.B.; D’Astous, J.L. Kinematics and kinetics of normal and planovalgus feet during walking. Gait Posture 2014, 39, 339–345. [Google Scholar] [CrossRef]
- Huang, Y.-C.; Wang, L.-Y.; Wang, H.-C.; Chang, K.-L.; Leong, C.-P. The relationship between the flexible flatfoot and plantar fasciitis: Ultrasonographic evaluation. Chang Gung Med. J. 2004, 27, 443–448. [Google Scholar] [PubMed]
- Buldt, A.K.; Forghany, S.; Landorf, K.B.; Levinger, P.; Murley, G.S.; Menz, H.B. Foot posture is associated with plantar pressure during gait: A comparison of normal, planus and cavus feet. Gait Posture 2018, 62, 235–240. [Google Scholar] [CrossRef] [PubMed]
- Messier, S.P.; Pittala, K.A. Etiologic factors associated with selected running injuries. Med. Sci. Sports Exerc. 1988, 20, 501–505. [Google Scholar] [CrossRef] [PubMed]
- Paton, J.S. The relationship between navicular drop and first metatarsophalangeal joint motion. J. Am. Podiatr. Med. Assoc. 2006, 96, 313–317. [Google Scholar] [CrossRef]
- Winkelmann, Z.K.; Anderson, D.; Games, K.E.; Eberman, L.E. Risk factors for medial tibial stress syndrome in active individuals: An evidence-based review. J. Athl. Train. 2016, 51, 1049–1052. [Google Scholar] [CrossRef] [PubMed]
- Khamis, S.; Yizhar, Z. Effect of feet hyperpronation on pelvic alignment in a standing position. Gait Posture 2007, 25, 127–134. [Google Scholar] [CrossRef]
- Elataar, F.F.; Abdelmajeed, S.F.; Abdellatif, N.M.; Mohammed, M.M. Core muscles’ endurance in flexible flatfeet: A cross-sectional study. J. Musculoskelet. Neuronal Interact. 2020, 20, 404. [Google Scholar] [PubMed]
- Menz, H.B.; Dufour, A.B.; Riskowski, J.L.; Hillstrom, H.J.; Hannan, M.T. Foot posture, foot function and low back pain: The Framingham Foot Study. Rheumatology 2013, 52, 2275–2282. [Google Scholar] [CrossRef]
- Ross, M.H.; Smith, M.; Plinsinga, M.L.; Vicenzino, B. Self-reported social and activity restrictions accompany local impairments in posterior tibial tendon dysfunction: A systematic review. J. Foot Ankle Res. 2018, 11, 49. [Google Scholar] [CrossRef] [PubMed]
- Desmyttere, G.; Hajizadeh, M.; Bleau, J.; Begon, M. Effect of foot orthosis design on lower limb joint kinematics and kinetics during walking in flexible pes planovalgus: A systematic review and meta-analysis. Clin. Biomech. 2018, 59, 117–129. [Google Scholar] [CrossRef]
- Banwell, H.A.; Thewlis, D.; Mackintosh, S. Adults with flexible pes planus and the approach to the prescription of customised foot orthoses in clinical practice: A clinical records audit. Foot 2015, 25, 101–109. [Google Scholar] [CrossRef] [PubMed]
- Liu, Y.; Fernandez, J. Randomized Controlled Trial of Gastrocnemius Muscle Analysis Using Surface Electromyography and Ultrasound in Different Striking Patterns of Young Women’s Barefoot Running. Phys. Act. Health 2024, 8, 223–233. [Google Scholar] [CrossRef]
- Desmyttere, G.; Hajizadeh, M.; Bleau, J.; Leteneur, S.; Begon, M. Anti-pronator components are essential to effectively alter lower-limb kinematics and kinetics in individuals with flexible flatfeet. Clin. Biomech. 2021, 86, 105390. [Google Scholar] [CrossRef]
- Kido, M.; Ikoma, K.; Hara, Y.; Imai, K.; Maki, M.; Ikeda, T.; Fujiwara, H.; Tokunaga, D.; Inoue, N.; Kubo, T. Effect of therapeutic insoles on the medial longitudinal arch in patients with flatfoot deformity: A three-dimensional loading computed tomography study. Clin. Biomech. 2014, 29, 1095–1098. [Google Scholar] [CrossRef]
- Karimi, M.; Tahmasebi, R.B.; Satvati, B.; Fatoye, F. Influence of foot insole on the gait performance in subjects with flat foot disorder. J. Mech. Med. Biol. 2019, 19, 1950050. [Google Scholar] [CrossRef]
- Wang, M.; Song, Y.; Zhao, X.; Wang, Y.; Zhang, M. Utilizing Anthropometric Measurements and 3D Scanning for Health Assessment in Clinical Practice. Phys. Act. Health 2024, 8, 182–196. [Google Scholar] [CrossRef]
- Khorasani, S.G.R.; Cham, M.B.; Sharifnezhad, A.; Saeedi, H.; Farahmand, B. Comparison of the immediate effects of prefabricated soft medical insoles and custom-molded rigid medical insoles on plantar pressure distribution in athletes with flexible flatfoot: A prospective study. Curr. Orthop. Pract. 2021, 32, 578–583. [Google Scholar] [CrossRef]
- Ho, M.; Nguyen, J.; Heales, L.; Stanton, R.; Kong, P.W.; Kean, C. The biomechanical effects of 3D printed and traditionally made foot orthoses in individuals with unilateral plantar fasciopathy and flat feet. Gait Posture 2022, 96, 257–264. [Google Scholar] [CrossRef]
- Hurd, W.J.; Kavros, S.J.; Kaufman, K.R. Comparative biomechanical effectiveness of over-the-counter devices for individuals with a flexible flatfoot secondary to forefoot varus. Clin. J. Sport Med. 2010, 20, 428–435. [Google Scholar] [CrossRef] [PubMed]
- Zifchock, R.A.; Davis, I. A comparison of semi-custom and custom foot orthotic devices in high-and low-arched individuals during walking. Clin. Biomech. 2008, 23, 1287–1293. [Google Scholar] [CrossRef]
- Yawar, A.; Korpas, L.; Lugo-Bolanos, M.; Mandre, S.; Venkadesan, M. Contribution of the transverse arch to foot stiffness in humans. arXiv 2017, arXiv:1706.04610. [Google Scholar]
- Zhang, L.; Zhang, Q.; Zhong, Y.; Hortobagyi, T.; Gu, Y. Effect of forefoot transverse arch stiffness on foot biomechanical response--based on finite element method. Front. Bioeng. Biotechnol. 2024, 12, 1387768. [Google Scholar] [CrossRef]
- Krüger, L.; Hedar, A.; Simon, A.; Spethmann, T.; Heinemann, A.; Viezens, L.; Lenz, A.L.; Amling, M.; Beil, F.T.; Hahn, M. Influence of the transverse tarsal arch on radiological components of progressive collapsing foot deformity. J. Orthop. Res. 2024, 42, 2752–2760. [Google Scholar] [CrossRef]
- Faul, F.; Erdfelder, E.; Lang, A.-G.; Buchner, A. G* Power 3: A flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav. Res. Methods 2007, 39, 175–191. [Google Scholar] [CrossRef] [PubMed]
- Bruening, D.A.; Frimenko, R.E.; Goodyear, C.D.; Bowden, D.R.; Fullenkamp, A.M. Sex differences in whole body gait kinematics at preferred speeds. Gait Posture 2015, 41, 540–545. [Google Scholar] [CrossRef] [PubMed]
- Cho, Y.; Park, J.-W.; Nam, K. The relationship between foot posture index and resting calcaneal stance position in elementary school students. Gait Posture 2019, 74, 142–147. [Google Scholar] [CrossRef]
- Jiang, X.; Yang, X.; Zhou, H.; Baker, J.S.; Gu, Y. Prolonged running using bionic footwear influences lower limb biomechanics. Healthcare 2021, 9, 236. [Google Scholar] [CrossRef]
- Zhang, Q.; Sun, D.; Wang, M.; Tafferner-Gulyás, V.; Chen, H.; Bíró, I.; Gu, Y. Effect of plantar fascia stiffness on plantar windlass mechanism and arch: Finite element method and dual fluoroscopic imaging system verification. Med. Eng. Phys. 2024, 134, 104259. [Google Scholar] [CrossRef] [PubMed]
- Delp, S.L.; Anderson, F.C.; Arnold, A.S.; Loan, P.; Habib, A.; John, C.T.; Guendelman, E.; Thelen, D.G. OpenSim: Open-source software to create and analyze dynamic simulations of movement. IEEE Trans. Biomed. Eng. 2007, 54, 1940–1950. [Google Scholar] [CrossRef] [PubMed]
- Menz, H.B.; Munteanu, S.E. Validity of 3 clinical techniques for the measurement of static foot posture in older people. J. Orthop. Sports Phys. Ther. 2005, 35, 479–486. [Google Scholar] [CrossRef] [PubMed]
- Murley, G.S.; Menz, H.B.; Landorf, K.B. A protocol for classifying normal-and flat-arched foot posture for research studies using clinical and radiographic measurements. J. Foot Ankle Res. 2009, 2, 22. [Google Scholar] [CrossRef] [PubMed]
- Bouysset, M.; Bonvoisin, B.; Lejeune, E.; Bouvier, M. Flattening of the rheumatoid foot in tarsal arthritis on X-ray. Scand. J. Rheumatol. 1987, 16, 127–133. [Google Scholar] [CrossRef] [PubMed]
- Hsu, C.-Y.; Wang, C.-S.; Lin, K.-W.; Chien, M.-J.; Wei, S.-H.; Chen, C.-S. Biomechanical analysis of the flatfoot with different 3D-printed insoles on the lower extremities. Bioengineering 2022, 9, 563. [Google Scholar] [CrossRef]
- Ye, D.; Sun, X.; Zhang, C.; Zhang, S.; Zhang, X.; Wang, S.; Fu, W. In vivo foot and ankle kinematics during activities measured by using a dual fluoroscopic imaging system: A narrative review. Front. Bioeng. Biotechnol. 2021, 9, 693806. [Google Scholar] [CrossRef]
- Jastifer, J.R.; Gustafson, P.A.; Gorman, R.R. Subtalar arthrodesis alignment: The effect on ankle biomechanics. Foot Ankle Int. 2013, 34, 244–250. [Google Scholar] [CrossRef] [PubMed]
- Ye, D.; Li, L.; Zhang, S.; Xiao, S.; Sun, X.; Wang, S.; Fu, W. Acute effect of foot strike patterns on in vivo tibiotalar and subtalar joint kinematics during barefoot running. J. Sport Health Sci. 2024, 13, 108–117. [Google Scholar] [CrossRef]
- Young, C.C.; Rutherford, D.S.; Niedfeldt, M.W. Treatment of plantar fasciitis. Am. Fam. Physician 2001, 63, 467–475. [Google Scholar]
- Aranda, Y.; Munuera, P.V. Plantar fasciitis and its relationship with hallux limitus. J. Am. Podiatr. Med. Assoc. 2014, 104, 263–268. [Google Scholar] [CrossRef]
- Ataabadi, P.A.; Abbassi, A.; Letafatkar, A.; Vanwanseele, B. The effects of foot orthosis and low-dye tape on lower limb joint angles and moments during running in individuals with pes planus. Gait Posture 2022, 96, 154–159. [Google Scholar] [CrossRef] [PubMed]
- Alsaafin, N.; Saad, N.; Mohammad Zadeh, S.A.; Hegazy, F.A. Effect of different foot orthosis inverted angles on walking kinematics in females with flexible flatfeet. J. Multidiscip. Healthc. 2023, 16, 2613–2623. [Google Scholar] [CrossRef] [PubMed]
- Kim, M.-K.; Lee, Y.-S. Kinematic analysis of the lower extremities of subjects with flat feet at different gait speeds. J. Phys. Ther. Sci. 2013, 25, 531–533. [Google Scholar] [CrossRef] [PubMed]
- Levinger, P.; Murley, G.S.; Barton, C.J.; Cotchett, M.P.; McSweeney, S.R.; Menz, H.B. A comparison of foot kinematics in people with normal-and flat-arched feet using the Oxford Foot Model. Gait Posture 2010, 32, 519–523. [Google Scholar] [CrossRef]
- Raza, A.; Mahmood, I.; Sultana, T. Evaluation of weight-bearing, walking stability, and gait symmetry in patients undergoing restoration following hip joint fractures. Int. J. Biomed. Eng. Technol. 2025, 47, 195–213. [Google Scholar] [CrossRef]






| Variables | Value |
|---|---|
| Surface material | Sponge |
| Support material | Thermoplastic polyurethane |
| Inner support height (mm) | 28 |
| Outer support height (mm) | 20 |
| Transverse arch support height (mm) | 13.5 |
| Variables | Mean ± SD |
|---|---|
| Age (years) | 28.0 5.0 |
| Height (cm) | 162.0 4.0 |
| Weight (kg) | 56.2 3.2 |
| Walking (m/s), CG | 1.2 0.1 |
| Walking (m/s), SFO | 1.3 0.1 |
| Walking (m/s), DFO | 1.3 0.2 |
| Jogging (m/s), CG | 2.5 0.1 |
| Jogging (m/s), SFO | 2.6 0.1 |
| Jogging (m/s), DFO | 2.7 0.1 |
| Variables | Results | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Mean ± SD | CG vs. SFO | CG vs. DFO | SFO vs. DFO | ||||||||||
| CG | SFO | DFO | 95% Confidence Interval | p | 95% Confidence Interval | p | 95% Confidence Interval | p | |||||
| MAA | Maximum angle (°) | 152.49 | 1.43 | 150.24 | 1.43 | 147.96 | 1.87 | (−2.56, −1.96) | <0.001 | (−4.85, −4.22) | <0.001 | (−2.71, −1.84) | <0.001 |
| ROM (°) | 9.22 | 0.48 | 8.69 | 0.81 | 8.51 | 0.90 | (0.06, 0.99) | 0.300 | (0.27, 1.14) | 0.003 | (−0.47, 0.83) | 0.573 | |
| NTNH | Minimum | 0.11 | 0.01 | 0.12 | 0.01 | 0.13 | 0.01 | (−0.01, −0.01) | <0.001 | (−0.02, −0.02) | <0.001 | (−0.01, −0.01) | <0.001 |
| ROM | 0.07 | 0.002 | 0.06 | 0.01 | 0.05 | 0.01 | (0.01, 0.02) | <0.001 | (0.02, 0.03) | <0.001 | (0.01, 0.02) | 0.005 | |
| vGRF (N/kg) | First peak | 1.17 | 0.03 | 1.19 | 0.06 | 1.27 | 0.06 | (−0.05, −0.01) | 0.031 | (−0.15, −0.05) | <0.001 | (−0.12, −0.02) | 0.008 |
| Second peak | 1.20 | 0.03 | 1.15 | 0.03 | 1.21 | 0.09 | (0.01, 0.08) | 0.009 | (−0.07, 0.05) | 0.608 | (−0.12, −0.1) | 0.045 | |
| MTPJ | Maximum angle (°) | 29.92 | 7.34 | 26.47 | 5.29 | 23.88 | 4.25 | (0.94, 5.95) | 0.08 | (3.41, 8.66) | <0.001 | (1.55, 3.67) | <0.001 |
| ROM (°) | 22.27 | 5.75 | 19.77 | 4.05 | 17.83 | 3.19 | (0.54, 4.44) | 0.013 | (1.01, 6.45) | <0.001 | (1.14, 2.75) | <0.001 | |
| Peak moment (Nm/kg) | 0.26 | 0.06 | 0.29 | 0.06 | 0.31 | 0.06 | (−0.06, −0.01) | 0.002 | (−0.07, −0.03) | <0.001 | (−0.05, −0.04) | 0.004 | |
| Subtalar | Maximum angle (°) | 10.43 | 1.40 | 14.46 | 1.37 | 14.69 | 2.27 | (−5.17, −2.89) | <0.001 | (−6.49, −2.02) | 0.002 | (−2.04, 1.58) | 0.784 |
| ROM (°) | 21.08 | 1.83 | 16.29 | 1.92 | 16.91 | 1.71 | (3.17, 6.41) | <0.001 | (2.53, 5.79) | <0.001 | (−2.63, 1.38) | 0.501 | |
| Peak moment (Nm/kg) | 0.61 | 0.02 | 0.45 | 0.04 | 0.431 | 0.04 | (0.13, 0.20) | <0.001 | (0.153, 0.213) | <0.001 | (−0.02, 0.06) | 0.300 | |
| Ankle | Maximum angle (°) | 12.83 | 1.79 | 9.25 | 2.71 | 8.86 | 1.67 | (1.66, 5.51) | 0.002 | (2.73, 5.22) | <0.001 | (−0.95,1.73) | 0.551 |
| ROM (°) | 24.55 | 2.75 | 21.26 | 3.68 | 20.70 | 2.13 | (−0.17, 6.75) | 0.061 | (2.20, 5.50) | <0.001 | (−2.6, 3.76) | 0.710 | |
| Peak moment (Nm/kg) | 2.10 | 0.15 | 1.83 | 0.14 | 1.88 | 0.09 | (0.14, 0.41) | <0.001 | (0.13, 0.30) | <0.001 | (−0.166, 0.05) | 0.276 | |
| Knee | Maximum angle (°) | 47.44 | 6.24 | 47.17 | 6.24 | 45.37 | 5.51 | (−4.33, 4.86) | 0.90 | (−2.20, 6.35) | 0.320 | (−1.24, 4.85) | 0.228 |
| ROM (°) | 39.45 | 6.71 | 39.80 | 6.81 | 36.46 | 5.55 | (−5.44, 4.76) | 0.90 | (−1.60, 7.32) | 0.194 | (−0.41, 6.81) | 0.079 | |
| Peak moment (Nm/kg) | 0.75 | 0.04 | 0.76 | 0.08 | 0.76 | 0.06 | (−0.07, 0.50) | 0.73 | (−0.05, 0.02) | 0.288 | (−0.07, 0.06) | 0.848 | |
| Hip | Maximum angle (°) | 29.02 | 1.44 | 40.42 | 2.66 | 30.22 | 3.22 | (−2.81, −0.22) | 0.057 | (−0.59, 0.16) | 0.080 | (−0.94, 1.35) | 0.717 |
| ROM (°) | 46.12 | 3.09 | 43.91 | 5.28 | 45.27 | 4.92 | (−0.36, 4.77) | 0.09 | (−1.74, 3.43) | 0.503 | (−3.36, 0.64) | 0.171 | |
| Peak moment (Nm/kg) | 0.84 | 0.15 | 0.88 | 0.16 | 0.86 | 0.10 | (−0.20, 0.11) | 0.56 | (−0.14, 0.11) | 0.804 | (−0.07, 0.15) | 0.488 | |
| Variables | Results | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Mean ± SD | CG vs. SFO | CG vs. DFO | SFO vs. DFO | ||||||||||
| CG | SFO | DFO | 95% Confidence Interval | p | 95% Confidence Interval | p | 95% Confidence Interval | p | |||||
| vGRF (N/kg) | Maximum | 2.28 | 0.13 | 2.34 | 0.19 | 2.45 | 0.27 | (−0.15, −0.01) | 0.030 | (−0.26, −0.10) | <0.001 | (−0.15, −0.46) | 0.010 |
| MTPJ | Maximum angle (°) | 17.90 | 4.10 | 14.97 | 3.16 | 13.50 | 2.58 | (1.55, 4.38) | <0.001 | (2.97, 5.89) | <0.001 | (0.89, 2.04) | <0.001 |
| ROM (°) | 10.14 | 2.28 | 8.28 | 1.77 | 7.46 | 1.42 | (1.08, 2.66) | <0.001 | (1.88, 3.48) | <0.001 | (0.49, 1.15) | <0.001 | |
| Peak moment (Nm/kg) | 0.40 | 0.09 | 0.45 | 0.10 | 0.48 | 0.09 | (−0.08, −0.02) | 0.004 | (−0.11, −0.05) | <0.001 | (−0.05, −0.01) | <0.001 | |
| Subtalar | Maximum angle (°) | 11.46 | 1.35 | 13.19 | 1.38 | 13.98 | 1.44 | (−2.76, −0.71) | 0.040 | (−3.92, −1.12) | 0.020 | (−1.86, 0.28) | 0.131 |
| ROM (°) | 12.59 | 1.93 | 10.78 | 1.68 | 11.31 | 2.05 | (−0.13, 3.74) | 0.064 | (−0.44, 2.94) | 0.131 | (−2.34, 1.23) | 0.503 | |
| Peak moment (Nm/kg) | 1.28 | 0.21 | 1.18 | 0.08 | 1.24 | 0.07 | (−0.05, 0.25) | 0.173 | (−0.11, 0.20) | 0.546 | (−0.13, 0.01) | 0.107 | |
| Ankle | Maximum angle (°) | 22.93 | 2.09 | 20.21 | 3.38 | 21.03 | 4.23 | (1.04, 4.39) | 0.004 | (0.15, 3.65) | 0.036 | (−2.59, 0.95) | 0.336 |
| ROM (°) | 40.02 | 6.32 | 34.76 | 7.11 | 38.07 | 5.67 | (0.92, 9.59) | 0.021 | (−0.54, 4.44) | 0.114 | (−6.86, 0.24) | 0.065 | |
| Peak moment (Nm/kg) | 3.14 | 0.15 | 3.09 | 0.12 | 3.07 | 0.155 | (−0.03, 0.11) | 0.237 | (−0.17, 0.142) | 0.119 | (−0.05, 0.10) | 0.560 | |
| Knee | Maximum angle (°) | 49.86 | 3.73 | 49.40 | 1.92 | 49.32 | 1.44 | (−0.72, 1.65) | 0.427 | (−0.76, 1.84) | 0.402 | (−0.57, 0.72) | 0.818 |
| ROM (°) | 29.81 | 4.63 | 30.80 | 3.02 | 31.34 | 2.39 | (−2.38, 0.39) | 0.154 | (−3.21, 0.15) | 0.072 | (−1.79, 0.72) | 0.388 | |
| Peak moment (Nm/kg) | 1.62 | 0.20 | 1.66 | 0.14 | 1.67 | 0.15 | (−0.13, 0.05) | 0.358 | (−0.11, 0.04) | 0.31 | (0.04, 0.07) | 0.789 | |
| Hip | Maximum angle (°) | 29.98 | 5.14 | 30.77 | 3.96 | 30.86 | 3.68 | (−2.97, 1.38) | 0.461 | (−2.82, 1.07) | 0.366 | (−0.11, 0.92) | 0.868 |
| ROM (°) | 39.03 | 5.62 | 39.08 | 5.34 | 39.87 | 4.63 | (−2.61, 2.59) | 0.996 | (−3.31, 1.73) | 0.525 | (−2.01, 0.44) | 0.201 | |
| Peak moment (Nm/kg) | 1.99 | 0.26 | 1.99 | 0.42 | 2.05 | 0.35 | (−0.39, 0.41) | 0.959 | (−0.40, 0.28) | 0.715 | (-0.32, 0.18) | 0.567 | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zhang, L.; Zhang, Q.; Liu, Q.; Jiang, X.; Simon, J.; Hortobágyi, T.; Gu, Y. Dual Transverse Arch Foot Orthosis Improves Gait Biomechanics in Females with Flexible Flatfoot. Bioengineering 2025, 12, 418. https://doi.org/10.3390/bioengineering12040418
Zhang L, Zhang Q, Liu Q, Jiang X, Simon J, Hortobágyi T, Gu Y. Dual Transverse Arch Foot Orthosis Improves Gait Biomechanics in Females with Flexible Flatfoot. Bioengineering. 2025; 12(4):418. https://doi.org/10.3390/bioengineering12040418
Chicago/Turabian StyleZhang, Linjie, Qiaolin Zhang, Qian Liu, Xinyan Jiang, János Simon, Tibor Hortobágyi, and Yaodong Gu. 2025. "Dual Transverse Arch Foot Orthosis Improves Gait Biomechanics in Females with Flexible Flatfoot" Bioengineering 12, no. 4: 418. https://doi.org/10.3390/bioengineering12040418
APA StyleZhang, L., Zhang, Q., Liu, Q., Jiang, X., Simon, J., Hortobágyi, T., & Gu, Y. (2025). Dual Transverse Arch Foot Orthosis Improves Gait Biomechanics in Females with Flexible Flatfoot. Bioengineering, 12(4), 418. https://doi.org/10.3390/bioengineering12040418









