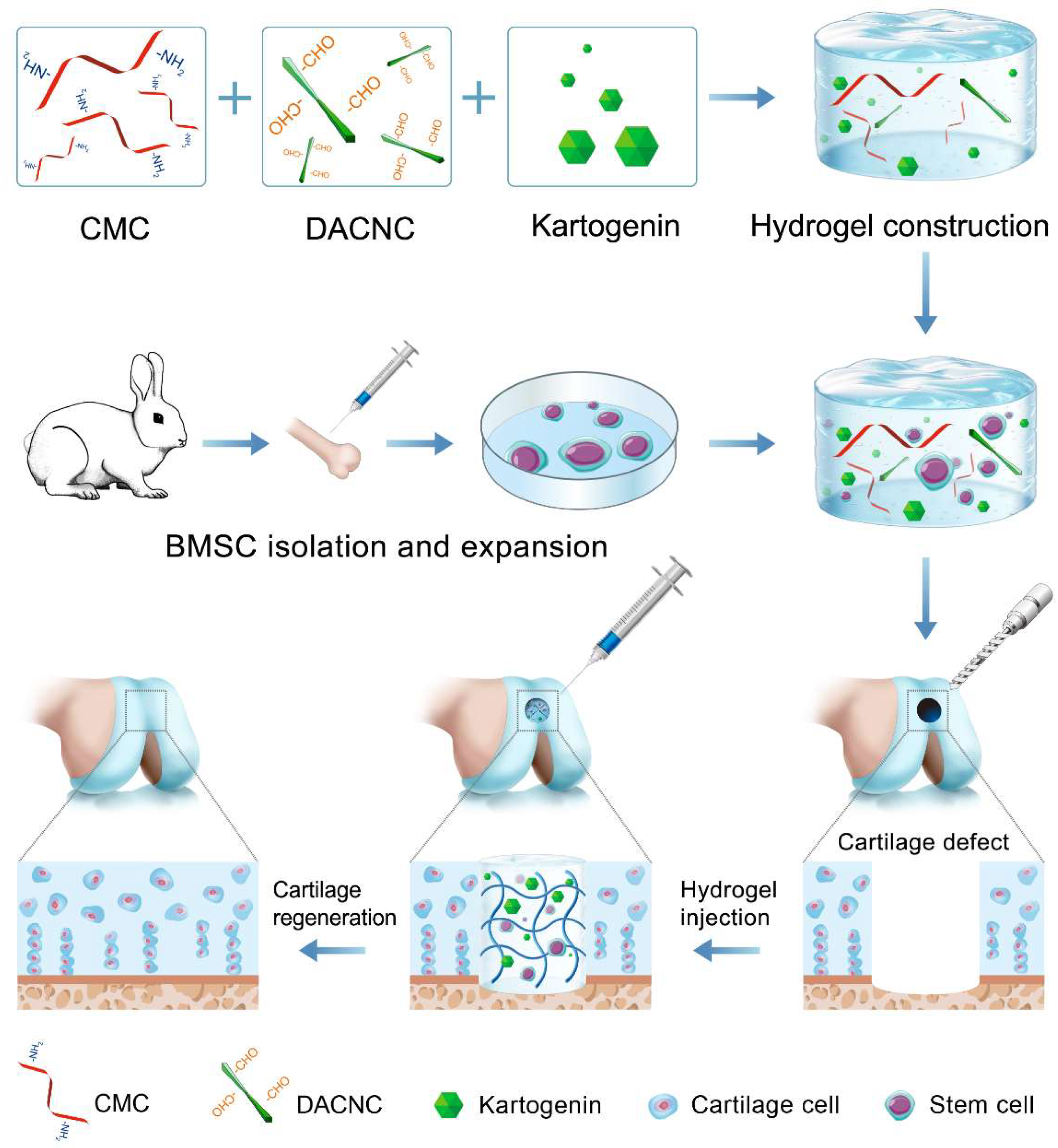
An Injectable Kartogenin-Incorporated Hydrogel Supports Mesenchymal Stem Cells for Cartilage Tissue Engineering
Abstract
:1. Introduction
2. Materials and Methods
2.1. Materials
2.2. Synthesis of CMC/DACNC Hydrogels
2.3. Material Characterization
2.3.1. Scanning Electron Microscope (SEM) Observation
2.3.2. Mechanical Properties Assay
2.3.3. Swelling Ratio and Injectable Analysis
2.4. Cell Culture
2.5. Cell Viability and Proliferation Analysis
2.6. In Vitro KGN-Induced Chondrogenic Differentiation
2.6.1. In Vitro Drug-Release Study
2.6.2. Histologic Section and Safranin-O Staining
2.6.3. Sulfated Glycosaminoglycan (sGAG) Content
2.7. In Vitro Differentiation of RBMSCs Encapsulated in the Hydrogels
2.7.1. Quantitative Real-Time Polymerase Chain Reaction (qRT-PCR) Assay
2.7.2. Enzyme-Linked Immunosorbent Assay (ELISA)
2.7.3. RNA Sequence Analysis of RBMSCs
2.8. In Vivo Test
2.8.1. In Vivo Degradation and Biocompatibility Test
2.8.2. The Animal Model for Cartilage Defects and Hydrogel Implantation
2.8.3. Histological Assessment
2.9. Statistical Analysis
3. Results
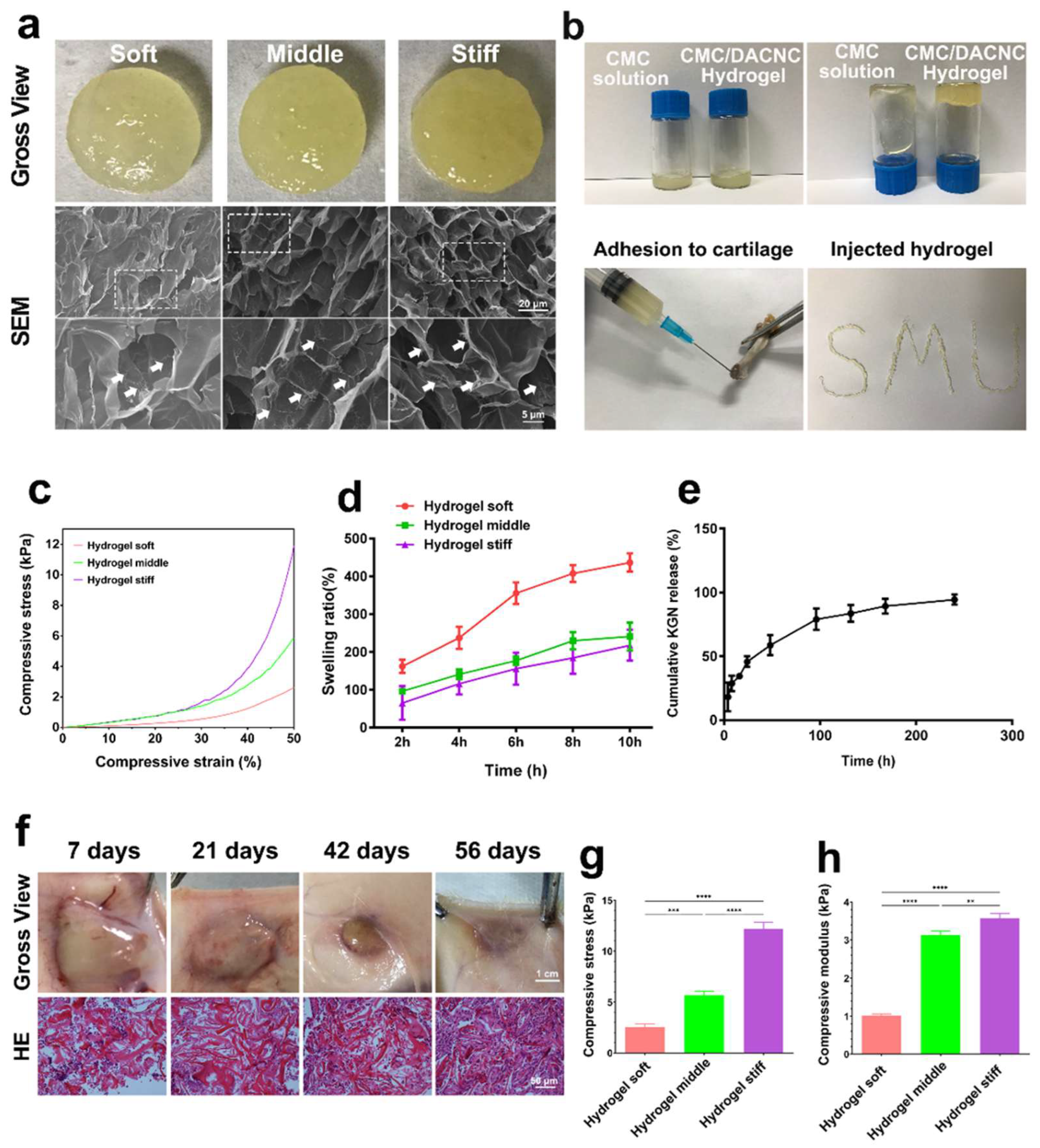
3.1. Synthesis and Characterization of Hydrogels
3.2. Sustained KGN-Release Behavior of Hydrogel In Vitro
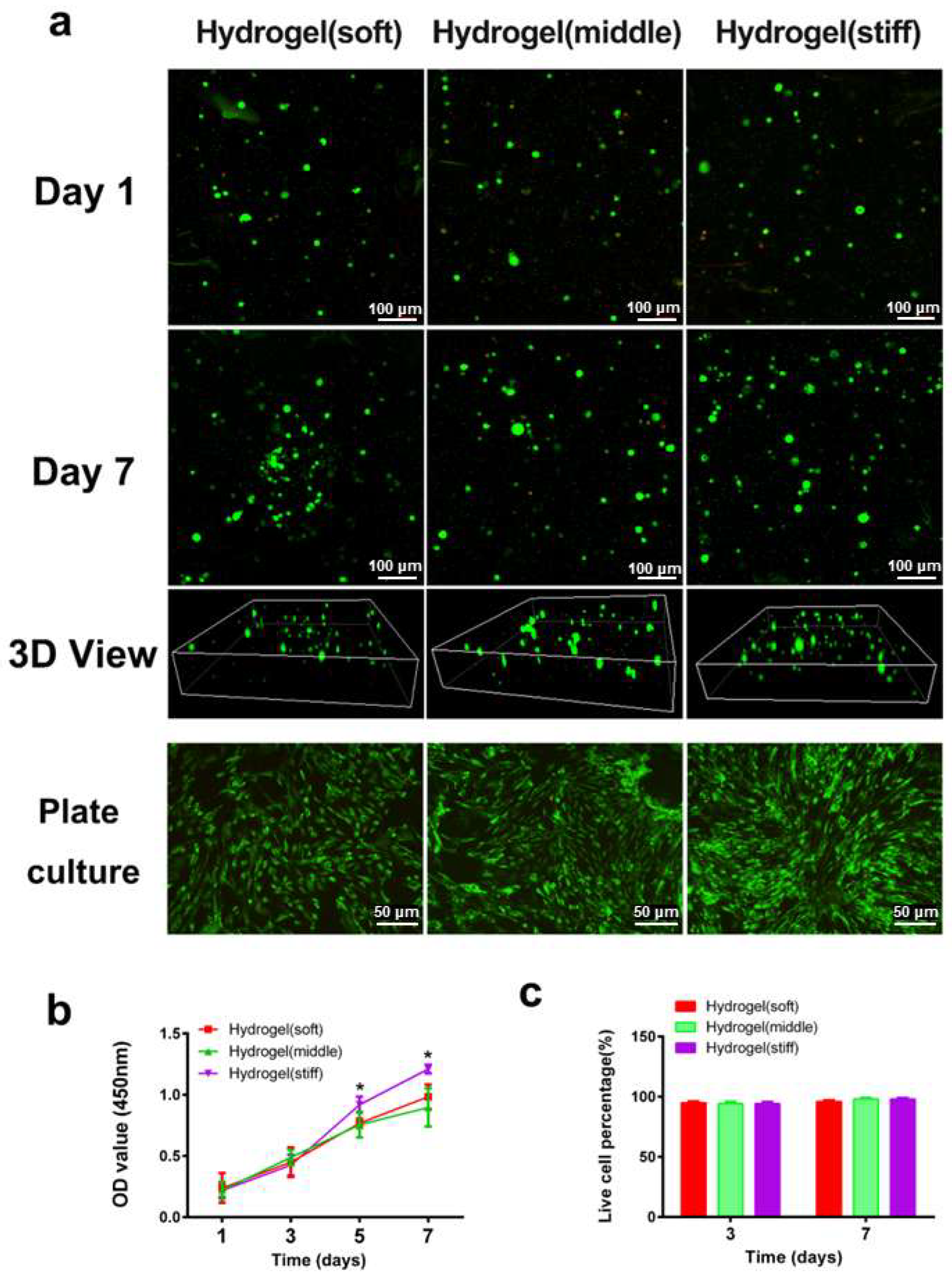
3.3. Cell Viability and Proliferation in Hydrogels
3.4. Cell Differentiation In Vitro
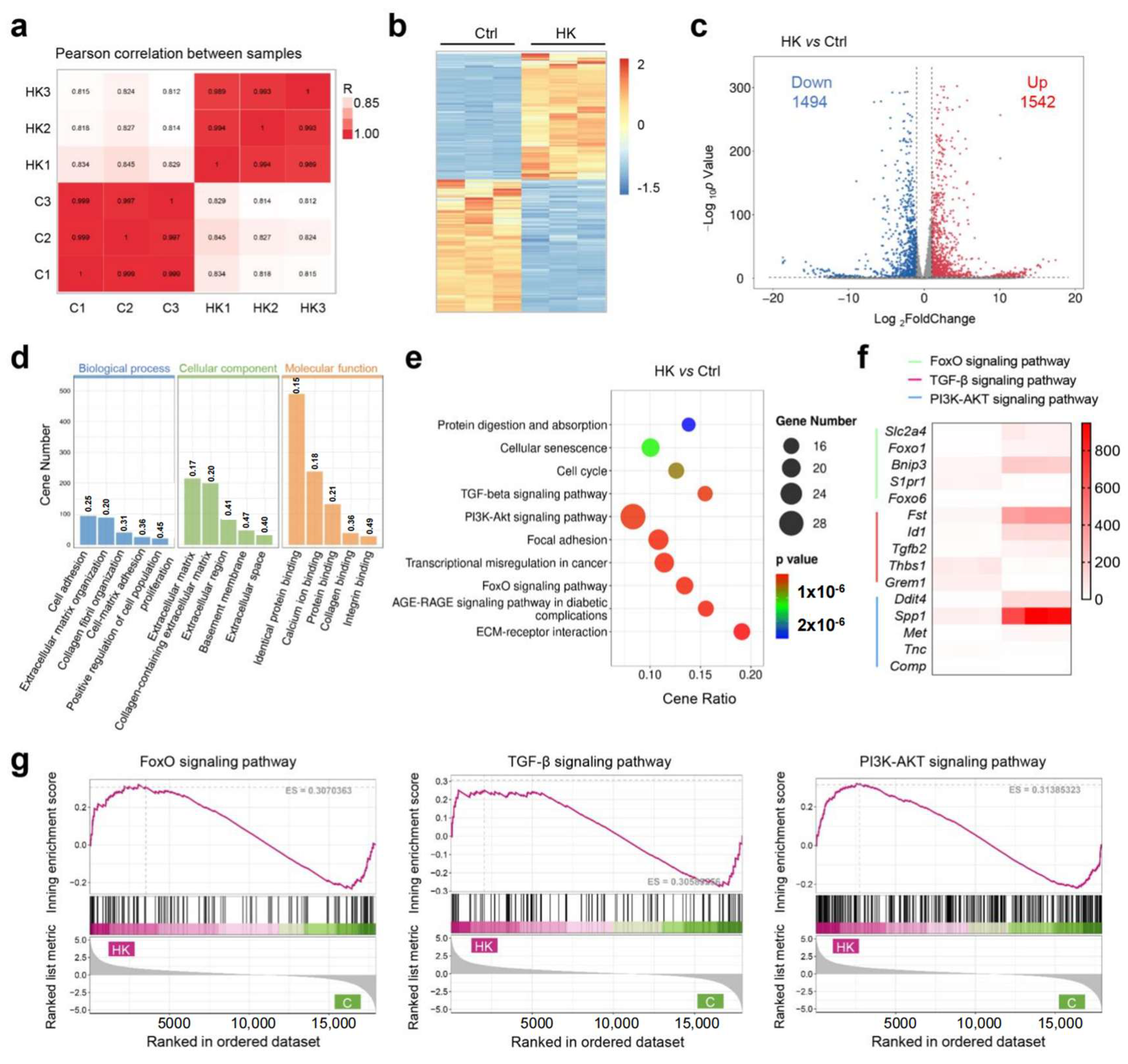
3.5. The Mechanism Study of Hydrogel to Enhance Cartilage Regeneration
3.6. In Vivo Evaluation of Full-Thickness Cartilage Defect Repair
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Hjelle, K.; Solheim, E.; Strand, T.; Muri, R.; Brittberg, M. Articular cartilage defects in 1000 knee arthroscopies. Arthrosc. J. Arthrosc. Relat. Surg. Off. Publ. Arthrosc. Assoc. N. Am. Int. Arthrosc. Assoc. 2002, 18, 730–734. [Google Scholar] [CrossRef]
- Lee, C.H.; Cook, J.L.; Mendelson, A.; Moioli, E.K.; Yao, H.; Mao, J.J. Regeneration of the articular surface of the rabbit synovial joint by cell homing: A proof of concept study. Lancet 2010, 376, 440–448. [Google Scholar] [CrossRef]
- Yoon, K.H.; Park, J.Y.; Lee, J.Y.; Lee, E.; Lee, J.; Kim, S.G. Costal chondrocyte-derived pellet-type autologous chondrocyte implantation for treatment of articular cartilage defect. Am. J. Sports Med. 2020, 48, 1236–1245. [Google Scholar] [CrossRef] [PubMed]
- Everhart, J.S.; Campbell, A.B.; Abouljoud, M.M.; Kirven, J.C.; Flanigan, D.C. Cost-efficacy of knee cartilage defect treatments in the United States. Am. J. Sports Med. 2020, 48, 242–251. [Google Scholar] [CrossRef] [PubMed]
- Kwon, H.; Brown, W.E.; Lee, C.A.; Wang, D.; Paschos, N.; Hu, J.C.; Athanasiou, K.A. Surgical and tissue engineering strategies for articular cartilage and meniscus repair. Nature Reviews. Rheumatology 2019, 15, 550–570. [Google Scholar] [PubMed]
- Li, L.; Li, J.; Guo, J.; Zhang, H.; Zhang, X.; Yin, C.; Wang, L.; Zhu, Y.; Yao, Q. 3D molecularly functionalized cell-free biomimetic scaffolds for osteochondral regeneration. Adv. Funct. Mater. 2019, 29, 1807356. [Google Scholar] [CrossRef]
- Zheng, Z.; Sun, J.; Wang, J.; He, S.; Huang, Y.; Yang, X.; Zhao, Y.; Yu, C.-Y.; Wei, H. A negative feedback bionic hydrogel reverses damaged cartilage microenvironment and induces targeted BMSCs differentiation for cartilage regeneration. Chem. Eng. J. 2023, 473, 145228. [Google Scholar] [CrossRef]
- Zhang, W.; Xue, W.; Jia, Z.; Yang, R.; Wang, P.; Hu, Y.; Tan, X.; Chen, Q.; Chi, B. Photo-driven dynamic hydrogel modulates bone marrow mesenchymal stem cells behavior for enhanced cartilage regeneration. Chem. Eng. J. 2024, 484, 149689. [Google Scholar] [CrossRef]
- Toh, W.S.; Lee, E.H.; Guo, X.M.; Chan, J.K.Y.; Yeow, C.H.; Choo, A.B.; Cao, T. Cartilage repair using hyaluronan hydrogel-encapsulated human embryonic stem cell-derived chondrogenic cells. Biomaterials 2010, 31, 6968–6980. [Google Scholar] [CrossRef]
- Shi, D.; Xu, X.; Ye, Y.; Song, K.; Cheng, Y.; Di, J.; Hu, Q.; Li, J.; Ju, H.; Jiang, Q.; et al. Photo-cross-linked scaffold with kartogenin-encapsulated nanoparticles for cartilage regeneration. ACS Nano 2016, 10, 1292–1299. [Google Scholar] [CrossRef]
- Balakrishnan, B.; Banerjee, R. Biopolymer-based hydrogels for cartilage tissue engineering. Chem. Rev. 2011, 111, 4453–4474. [Google Scholar] [CrossRef] [PubMed]
- Han, Y.; Yang, J.; Zhao, W.; Wang, H.; Sun, Y.; Chen, Y.; Luo, J.; Deng, L.; Xu, X.; Cui, W.; et al. Biomimetic Injectable Hydrogel Microspheres with Enhanced Lubrication and Controllable Drug Release for the Treatment of Osteoarthritis. Bioact. Mater. 2021, 6, 3596–3607. [Google Scholar] [CrossRef]
- Si, X.; Zhang, Q.; Ning, B.; Qiang, L.; Li, Q.; Liu, Y.; Fan, M.; Shan, J.; Shen, G.; Lin, Z.; et al. Injectable photocrosslinkable acellular cartilage matrix hydrogel loaded with exosomes for promoting growth plate injury repair. Chem. Eng. J. 2024, 493, 152463. [Google Scholar] [CrossRef]
- Chuah, Y.J.; Peck, Y.; Lau, J.E.; Hee, H.T.; Wang, D.A. Hydrogel based cartilaginous tissue regeneration: Recent insights and technologies. Biomater. Sci. 2017, 5, 613–631. [Google Scholar] [CrossRef]
- Geng, Y.; Xue, H.; Zhang, Z.; Panayi, A.C.; Knoedler, S.; Zhou, W.; Mi, B.; Liu, G. Recent advances in carboxymethyl chitosan-based materials for biomedical applications. Carbohydr. Polym. 2023, 305, 120555. [Google Scholar] [CrossRef] [PubMed]
- Huang, W.; Wang, Y.; Huang, Z.; Wang, X.; Chen, L.; Zhang, Y.; Zhang, L. On-demand dissolvable self-healing hydrogel based on carboxymethyl chitosan and cellulose nanocrystal for deep partial thickness burn wound healing. ACS Appl. Mater. Interfaces 2018, 10, 41076–41088. [Google Scholar] [CrossRef]
- Wang, L.S.; Du, C.; Toh, W.S.; Wan, A.C.; Gao, S.J.; Kurisawa, M. Modulation of chondrocyte functions and stiffness-dependent cartilage repair using an injectable enzymatically crosslinked hydrogel with tunable mechanical properties. Biomaterials 2014, 35, 2207–2217. [Google Scholar] [CrossRef]
- Zuscik, M.J.; Hilton, M.J.; Zhang, X.; Chen, D.; O’keefe, R.J. Regulation of chondrogenesis and chondrocyte differentiation by stress. J. Clin. Investig. 2008, 118, 429–438. [Google Scholar] [CrossRef]
- Varela-Eirin, M.; Loureiro, J.; Fonseca, E.; Corrochano, S.; Caeiro, J.R.; Collado, M.; Mayan, M.D. Cartilage regeneration and ageing: Targeting cellular plasticity in osteoarthritis. Ageing Res. Rev. 2018, 42, 56–71. [Google Scholar] [CrossRef]
- Chen, Z.; Zhou, T.; Luo, H.; Wang, Z.; Wang, Q.; Shi, R.; Li, Z.; Pang, R.; Tan, H. HWJMSC-EVs promote cartilage regeneration and repair via the ITGB1/TGF-β/Smad2/3 axis mediated by microfractures. J. Nanobiotechnol. 2024, 22, 177. [Google Scholar] [CrossRef]
- Johnson, K.; Zhu, S.; Tremblay, M.S.; Payette, J.N.; Wang, J.; Bouchez, L.C.; Meeusen, S.; Althage, A.; Cho, C.Y.; Wu, X.; et al. A stem cell-based approach to cartilage repair. Science 2012, 336, 717–721. [Google Scholar] [CrossRef]
- Chen, P.; Liao, X. Kartogenin delivery systems for biomedical therapeutics and regenerative medicine. Drug Deliv. 2023, 30, 2254519. [Google Scholar] [CrossRef] [PubMed]
- Zhou, Y.; Xie, S.; Tang, Y.; Li, X.; Cao, Y.; Hu, J.; Lu, H. Effect of book-shaped acellular tendon scaffold with bone marrow mesenchymal stem cells sheets on bone-tendon interface healing. J. Orthop. Transl. 2021, 26, 162–170. [Google Scholar] [CrossRef] [PubMed]
- Lim, J.K.; Hui, J.; Li, L.; Thambyah, A.; Goh, J.; Lee, E.H. Enhancement of tendon graft osteointegration using mesenchymal stem cells in a rabbit model of anterior cruciate ligament reconstruction. Arthroscopy 2004, 20, 899–910. [Google Scholar] [CrossRef] [PubMed]
- Zhou, M.; Smith, A.M.; Das, A.K.; Hodson, N.W.; Collins, R.F.; Ulijn, R.V.; Gough, J.E. Self-assembled peptide-based hydrogels as scaffolds for anchorage-dependent cells. Biomaterials 2009, 30, 2523–2530. [Google Scholar] [CrossRef]
- Liu, X.; Chen, Y.; Mao, A.S.; Xuan, C.; Wang, Z.; Gao, H.; An, G.; Zhu, Y.; Shi, X.; Mao, C. Molecular recognition-directed site-specific release of stem cell differentiation inducers for enhanced joint repair. Biomaterials 2020, 232, 119644. [Google Scholar] [CrossRef]
- Shan, B.H.; Wu, F.G. Hydrogel-based growth factor delivery platforms: Strategies and recent advances. Adv. Mater. 2024, 36, e2210707. [Google Scholar] [CrossRef]
- Li, X.; Xu, M.; Geng, Z.; Liu, Y. Functional hydrogels for the repair and regeneration of tissue defects. Front. Bioeng. Biotechnol. 2023, 11, 1190171. [Google Scholar] [CrossRef]
- Liu, H.; Cheng, Y.; Chen, J.; Chang, F.; Wang, J.; Ding, J.; Chen, X. Component effect of stem cell-loaded thermosensitive polypeptide hydrogels on cartilage repair. Acta Biomater. 2018, 73, 103–111. [Google Scholar] [CrossRef]
- Zhang, H.; Wu, S.; Chen, W.; Hu, Y.; Geng, Z.; Su, J. Bone/cartilage targeted hydrogel: Strategies and applications. Bioact. Mater. 2023, 23, 156–169. [Google Scholar] [CrossRef]
- Jelodari, S.; Sadrabadi, A.E.; Zarei, F.; Jahangir, S.; Azami, M.; Sheykhhasan, M.; Hosseini, S. New insights into cartilage tissue engineering: Improvement of tissue-scaffold integration to enhance cartilage regeneration. Biomed Res. Int. 2022, 2022, 7638245. [Google Scholar] [CrossRef] [PubMed]
- Li, Z.; Yang, B.; Yang, Z.; Xie, X.; Guo, Z.; Zhao, J.; Wang, R.; Fu, H.; Zhao, P.; Zhao, X.; et al. Supramolecular hydrogel with ultra-rapid cell-mediated network adaptation for enhancing cellular metabolic energetics and tissue regeneration. Adv. Mater. 2024, 36, e2307176. [Google Scholar] [CrossRef]
- Shang, F.; Yu, Y.; Liu, S.; Ming, L.; Zhang, Y.; Zhou, Z.; Zhao, J.; Jin, Y. Advancing application of mesenchymal stem cell-based bone tissue regeneration. Bioact. Mater. 2021, 6, 666–683. [Google Scholar] [CrossRef]
- Lin, H.; Sohn, J.; Shen, H.; Langhans, M.T.; Tuan, R.S. Bone marrow mesenchymal stem cells: Aging and tissue engineering applications to enhance bone healing. Biomaterials 2019, 203, 96–110. [Google Scholar] [CrossRef]
- Zhou, C.; Wang, C.; Xu, K.; Niu, Z.; Zou, S.; Zhang, D.; Qian, Z.; Liao, J.; Xie, J. Hydrogel platform with tunable stiffness based on magnetic nanoparticles cross-linked GelMA for cartilage regeneration and its intrinsic biomechanism. Bioact. Mater. 2023, 25, 615–628. [Google Scholar] [CrossRef] [PubMed]
- Zhang, A.; Sun, L.; Chen, K.; Liu, C.; Yuan, Y. 3D printing viscoelastic hydrogel-based scaffolds with a swelling-dependent gate for cartilage injury regeneration. Chem. Eng. J. 2024, 480, 147260. [Google Scholar] [CrossRef]
- Baei, P.; Daemi, H.; Mostafaei, F.; Sayahpour, F.A.; Baharvand, H.; Eslaminejad, M.B. A tough polysaccharide-based cell-laden double-network hydrogel promotes articular cartilage tissue regeneration in rabbits. Chem. Eng. J. 2021, 418, 129277. [Google Scholar] [CrossRef]
- Fu, L.; Li, L.; Bian, Q.; Xue, B.; Jin, J.; Li, J.; Cao, Y.; Jiang, Q.; Li, H. Cartilage-like protein hydrogels engineered via entanglement. Nature 2023, 618, 740–747. [Google Scholar] [CrossRef] [PubMed]
- Engler, A.J.; Sen, S.; Sweeney, H.L.; Discher, D.E. Matrix elasticity directs stem cell lineage specification. Cell 2006, 126, 677–689. [Google Scholar] [CrossRef]
- Mitra, S.K.; Hanson, D.A.; Schlaepfer, D.D. Focal adhesion kinase: In command and control of cell motility. Nat. Rev. Mol. Cell Biol. 2005, 6, 56–68. [Google Scholar] [CrossRef]
- Elosegui-Artola, A.; Andreu, I.; Beedle, A.E.M.; Lezamiz, A.; Uroz, M.; Kosmalska, A.J.; Oria, R.; Kechagia, J.Z.; Rico-Lastres, P.; Le Roux, A.-L.; et al. Force triggers YAP nuclear entry by regulating transport across nuclear pores. Cell 2017, 171, 1397–1410.e14. [Google Scholar] [CrossRef] [PubMed]
- Trappmann, B.; Baker, B.M.; Polacheck, W.J.; Choi, C.K.; Burdick, J.A.; Chen, C.S. Matrix degradability controls multicellularity of 3D cell migration. Nat. Commun. 2017, 8, 371. [Google Scholar] [CrossRef] [PubMed]
- Li, Q.; Xu, S.; Feng, Q.; Dai, Q.; Yao, L.; Zhang, Y.; Gao, H.; Dong, H.; Chen, D.; Cao, X. 3D printed silk-gelatin hydrogel scaffold with different porous structure and cell seeding strategy for cartilage regeneration. Bioact. Mater. 2021, 6, 3396–3410. [Google Scholar] [CrossRef]
- Chaudhuri, O.; Gu, L.; Klumpers, D.; Darnell, M.; Bencherif, S.A.; Weaver, J.C.; Huebsch, N.; Lee, H.P.; Lippens, E.; Duda, G.N.; et al. Hydrogels with tunable stress relaxation regulate stem cell fate and activity. Nat. Mater. 2016, 15, 326–334. [Google Scholar] [CrossRef] [PubMed]
- Xu, J.; Feng, Q.; Lin, S.; Yuan, W.; Li, R.; Li, J.; Wei, K.; Chen, X.; Zhang, K.; Yang, Y.; et al. Injectable Stem Cell-Laden Supramolecular Hydrogels Enhance In Situ Osteochondral Regeneration via the Sustained Co-Delivery of Hydrophilic and Hydrophobic Chondrogenic Molecules. Biomaterials 2019, 210, 51–61. [Google Scholar] [CrossRef]
- Li, X.; Ding, J.; Zhang, Z.; Yang, M.; Yu, J.; Wang, J.; Chang, F.; Chen, X. Kartogenin-Incorporated Thermogel Supports Stem Cells for Significant Cartilage Regeneration. ACS Appl. Mater. Interfaces 2016, 8, 5148–5159. [Google Scholar] [CrossRef]
- Fan, W.; Yuan, L.; Li, J.; Wang, Z.; Chen, J.; Guo, C.; Mo, X.; Yan, Z. Injectable double-crosslinked hydrogels with kartogenin-conjugated polyurethane nano-particles and transforming growth factor β3 for in-situ cartilage regeneration. Mater. Sci. Eng. C Mater. Biol. Appl. 2020, 110, 110705. [Google Scholar] [CrossRef]
- Lee, S.S.; Choi, G.E.; Lee, H.J.; Kim, Y.; Choy, J.H.; Jeong, B. Layered double hydroxide and polypeptide thermogel nanocomposite system for chondrogenic differentiation of stem cells. ACS Appl. Mater. Interfaces 2017, 9, 42668–42675. [Google Scholar] [CrossRef]
- Maličev, E.; Jazbec, K. An overview of mesenchymal stem cell heterogeneity and concentration. Pharmaceuticals 2024, 17, 350. [Google Scholar] [CrossRef]
- Bernardo, M.E.; Emons, J.A.M.; Karperien, M.; Nauta, A.J.; Willemze, R.; Roelofs, H.; Romeo, S.; Marchini, A.; Rappold, G.A.; Vukicevic, S.; et al. Human mesenchymal stem cells derived from bone marrow display a better chondrogenic differentiation compared with other sources. Connect. Tissue Res. 2007, 48, 132–140. [Google Scholar] [CrossRef]
- Klabukov, I.; Atiakshin, D.; Kogan, E.; Ignatyuk, M.; Krasheninnikov, M.; Zharkov, N.; Yakimova, A.; Grinevich, V.; Pryanikov, P.; Parshin, V.; et al. Post-implantation inflammatory responses to xenogeneic tissue-engineered cartilage implanted in rabbit trachea: The role of cultured chondrocytes in the modification of inflammation. Int. J. Mol. Sci. 2023, 24, 16783. [Google Scholar] [CrossRef] [PubMed]
- Li, C.S.; Xu, Y.; Li, J.; Qin, S.H.; Huang, S.W.; Chen, X.M.; Luo, Y.; Gao, C.T.; Xiao, J.H. Ultramodern natural and synthetic polymer hydrogel scaffolds for articular cartilage repair and regeneration. Biomed. Eng. Online 2025, 24, 13. [Google Scholar] [CrossRef] [PubMed]




| Gene | Forward Primer Sequence (5′-3′) | Reverse Primer Sequence (3′-5′) |
|---|---|---|
| ACAN | CTCAGACCTCGACAACGCAT | TAGTTGGGCAGCGAGACCTT |
| Collagen-II | TGCAGGAGGGGAAGAGGTAT | TCCTTTCTGCCCCTTTGGTC |
| Sox-9 | GGCTCCGACACCGAGAATA | GTCTCCAGAGCTTCCCGAGG |
| Collagen-X | GGCATAAAAGGCCCACAACC | TTGGTCCTCTCTCCCCTTGT |
| GAPDH | AGAGCACCAGAGGAGGACG | TGGGATGGAAACTGTGAAGAG |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Huang, C.; Zhong, G.; Xiao, J.; Wang, X.; Huang, W.; Chen, L.; Zhang, Y.; Cheng, S. An Injectable Kartogenin-Incorporated Hydrogel Supports Mesenchymal Stem Cells for Cartilage Tissue Engineering. Bioengineering 2025, 12, 434. https://doi.org/10.3390/bioengineering12050434
Huang C, Zhong G, Xiao J, Wang X, Huang W, Chen L, Zhang Y, Cheng S. An Injectable Kartogenin-Incorporated Hydrogel Supports Mesenchymal Stem Cells for Cartilage Tissue Engineering. Bioengineering. 2025; 12(5):434. https://doi.org/10.3390/bioengineering12050434
Chicago/Turabian StyleHuang, Chongquan, Guoqing Zhong, Jin Xiao, Xiaolan Wang, Weijuan Huang, Lingyun Chen, Yu Zhang, and Shi Cheng. 2025. "An Injectable Kartogenin-Incorporated Hydrogel Supports Mesenchymal Stem Cells for Cartilage Tissue Engineering" Bioengineering 12, no. 5: 434. https://doi.org/10.3390/bioengineering12050434
APA StyleHuang, C., Zhong, G., Xiao, J., Wang, X., Huang, W., Chen, L., Zhang, Y., & Cheng, S. (2025). An Injectable Kartogenin-Incorporated Hydrogel Supports Mesenchymal Stem Cells for Cartilage Tissue Engineering. Bioengineering, 12(5), 434. https://doi.org/10.3390/bioengineering12050434









