Mesenchymal Stem Cells and MSCs-Derived Extracellular Vesicles in Infectious Diseases: From Basic Research to Clinical Practice
Abstract
1. Introduction
2. MSCs and MSC-Derived Extracellular Vesicles (MSC-EVs)
2.1. Extracellular Vesicles (EVs)
2.2. Application of Tissue Engineering Methods to Improve Therapeutic Effectiveness of MSCs and MSC-EVs
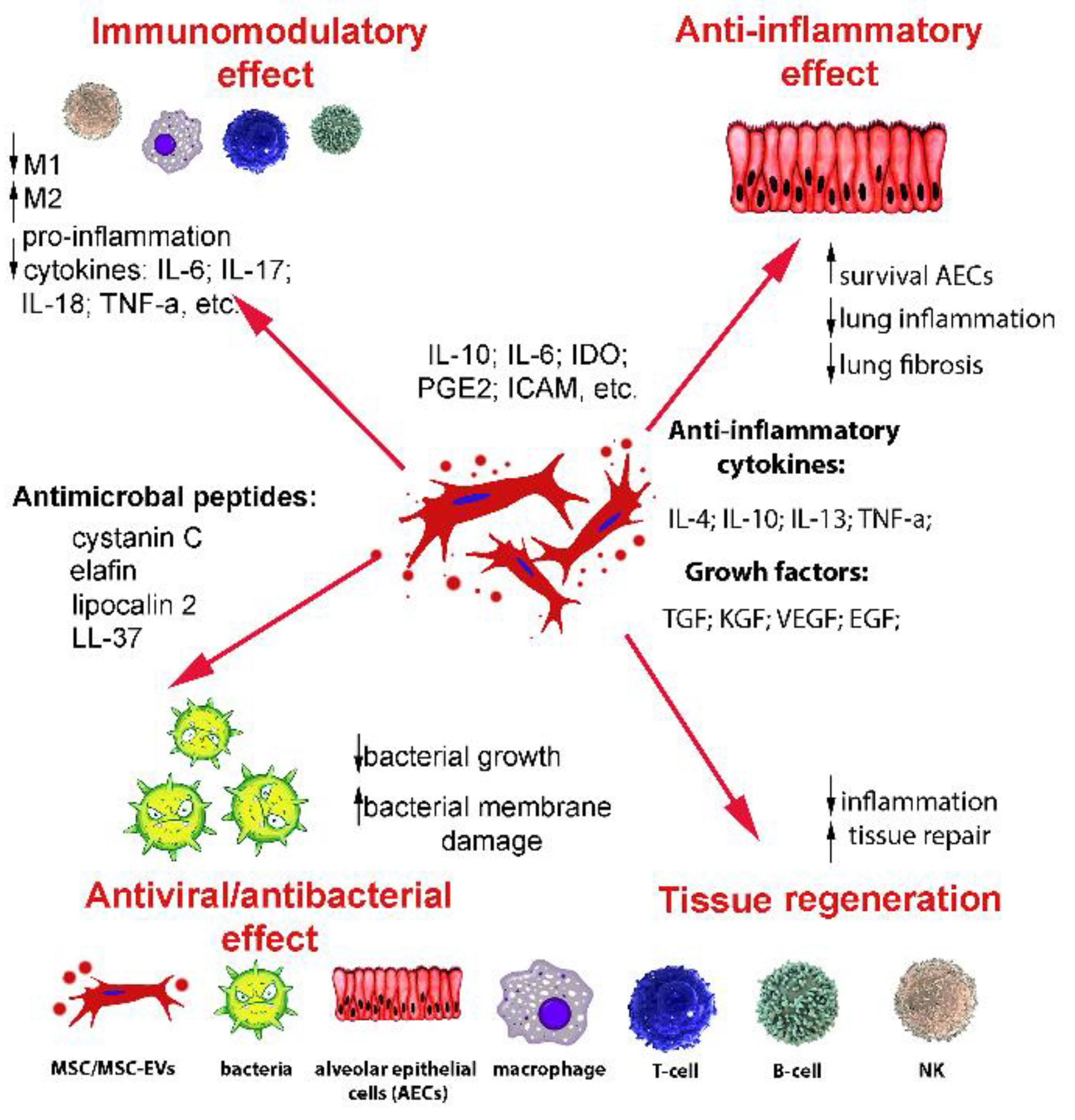
2.3. Mechanisms of Immunomodulatory Action of MSCs and MSC-EVs
3. Viral Infectious Diseases
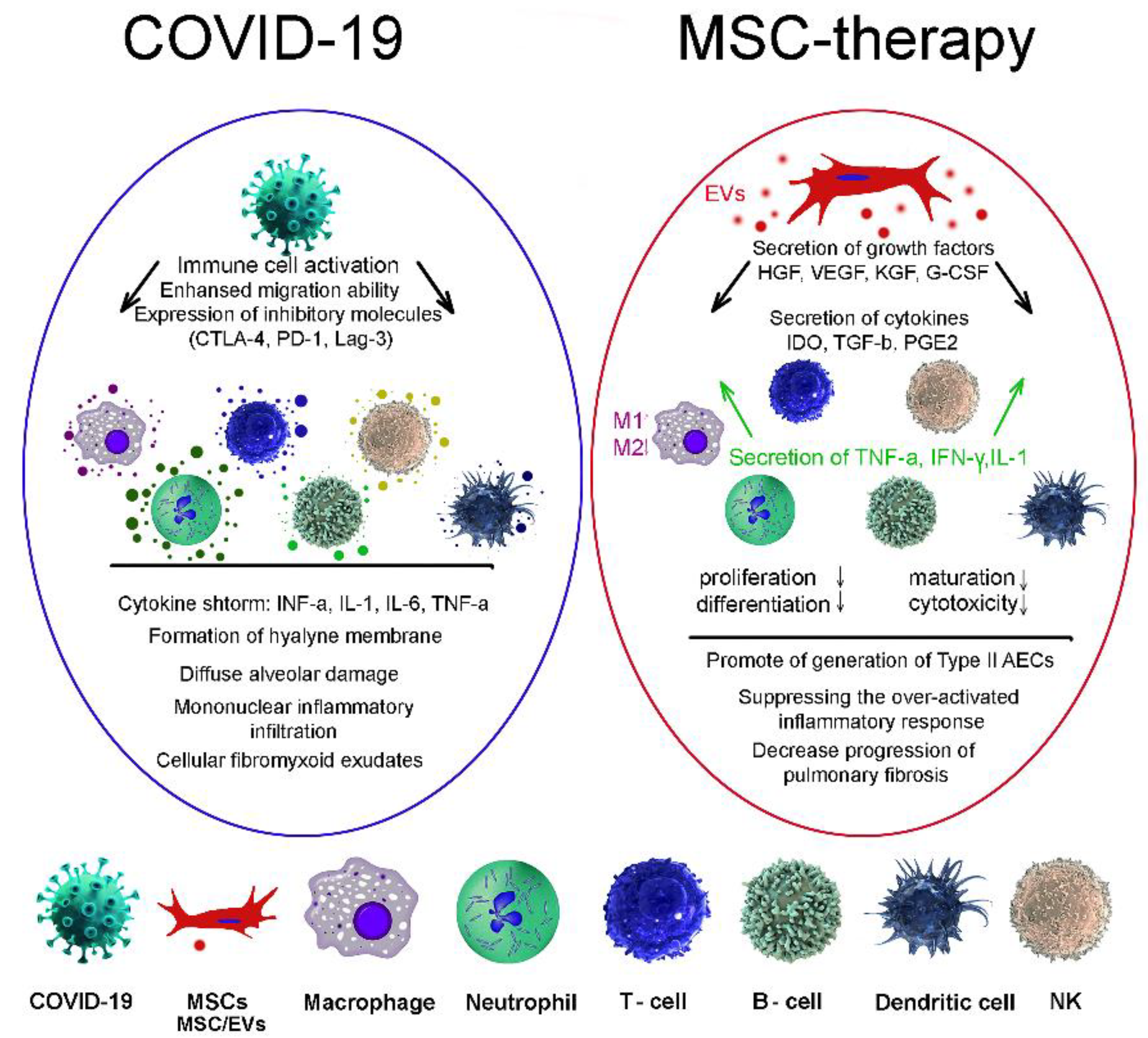
3.1. COVID-19
3.2. Flu
3.3. AIDS
4. Bacterial Infectious Diseases
4.1. Tuberculosis
4.2. Cholera
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Flaherty, G.T.; Hamer, D.H.; Chen, L.H. Travel in the Time of COVID: A Review of international travel health in a global pandemic. Curr. Infect. Dis. Rep. 2022, 24, 129–145. [Google Scholar] [CrossRef] [PubMed]
- Du, M.; Yuan, J.; Jing, W.; Liu, M.; Liu, J. The effect of international travel arrivals on the new HIV infections in 15-49 years aged group among 109 countries or territories from 2000 to 2018. Front. Public Health 2022, 10, 833551. [Google Scholar] [CrossRef] [PubMed]
- Bonato, F.; Ferreli, C.; Satta, R.; Rongioletti, F.; Atzori, L. Syphilis and the COVID-19 pandemic: Did the lockdown stop risky sexual behavior? Clin. Dermatol. 2021, 39, 710–713. [Google Scholar] [CrossRef] [PubMed]
- Abbas, M.; Aloudat, T.; Bartolomei, J.; Carballo, M.; Durieux-Paillard, S.; Gabus, L.; Jablonka, A.; Jackson, Y.; Kaojaroen, K.; Koch, D.; et al. Migrant and refugee populations: A public health and policy perspective on a continuing global crisis. Antimicrob. Resist. Infect. Control 2018, 7, 113. [Google Scholar] [CrossRef] [PubMed]
- Dunn, R.N.; Husien, M.B. Spinal tuberculosis: Review of current management. Bone Jt. J. 2018, 1, 425–431. [Google Scholar] [CrossRef]
- Greenaway, C.; Castelli, F. Infectious diseases at different stages of migration: An expert review. J. Travel. Med. 2019, 26, taz007. [Google Scholar] [CrossRef]
- Seedat, F.; Hargreaves, S.; Nellums, L.B.; Ouyang, J.; Brown, M.; Friedland, J.S. How effective are approaches to migrant screening for infectious diseases in Europe? A systematic review. Lancet Infect. Dis. 2018, 18, e259–e271. [Google Scholar] [CrossRef]
- Castelli, F.; Sulis, G. Migration and infectious diseases. Clin. Microbiol. Infect. 2017, 23, 283–289. [Google Scholar] [CrossRef]
- Lycett, S.J.; Duchatel, F.; Digard, P. A brief history of bird flu. Philos. Trans. R. Soc. Lond. B Biol. Sci. 2019, 74, 20180257. [Google Scholar] [CrossRef]
- Ashraf, N.; Kubat, R.C.; Poplin, V.; Adenis, A.A.; Denning, D.W.; Wright, L.; McCotter, O.; Schwartz, I.S.; Jackson, B.R.; Chiller, T.; et al. Redrawing the maps for endemic mycoses. Mycopathologia 2020, 185, 843–865. [Google Scholar] [CrossRef]
- Kotwal, A.; Yadav, A. Biothreat & One Health: Current scenario & way forward. Indian J. Med. Res. 2021, 153, 257–263. [Google Scholar] [CrossRef]
- Green, M.S.; LeDuc, J.; Cohen, D.; Franz, D.R. Confronting the threat of bioterrorism: Realities, challenges, and defensive strategies. Lancet Infect. Dis. 2019, 19, e2–e13. [Google Scholar] [CrossRef]
- Biselli, R.; Nisini, R.; Lista, F.; Autore, A.; Lastilla, M.; De Lorenzo, G.; Peragallo, M.S.; Stroffolini, T.; D’Amelio, R. A historical review of military medical strategies for fighting infectious diseases: From battlefields to global health. Biomedicines 2022, 10, 2050. [Google Scholar] [CrossRef]
- Cisse, G. Food-borne and water-borne diseases under climate change in low- and middle-income countries: Further efforts needed for reducing environmental health expo-sure risks. Acta Trop. 2019, 194, 181–188. [Google Scholar] [CrossRef]
- Kostyusheva, A.; Brezgin, S.; Babin, Y.; Vasilyeva, I.; Glebe, D.; Kostyushev, D.; Chulanov, V. CRISPR-Cas systems for diagnosing infectious diseases. Methods 2022, 203, 431–446. [Google Scholar] [CrossRef]
- Meiner, Z.; Marmor, A.; Jalagel, M.; Levine, H.; Shiri, S.; Schwartz, I. Risk factors for functional deterioration in a cohort with late effects of poliomyelitis: A ten-year follow-up study. NeuroRehabilitation 2021, 49, 491–499. [Google Scholar] [CrossRef]
- Pirrotta, P.; Tavares-Da-Silva, F.; Co, M.; Lecrenier, N.; Herve, C.; Stegmann, J.U. An analysis of spontaneously reported data of vesicular and bullous cutaneous eruptions occurring following vaccination with the adjuvanted recombinant zoster vaccine. Drug Saf. 2021, 44, 1341–1353. [Google Scholar] [CrossRef] [PubMed]
- Miceli, V.; Bulati, M.; Iannolo, G.; Zito, G.; Gallo, A.; Conaldi, G.P. Therapeutic properties of mesenchymal stromal/stem cells: The need of cell priming for cell-free therapies in regenerative medicine. Int. J. Mol. Sci. 2021, 22, 763. [Google Scholar] [CrossRef]
- Zakrzewski, W.; Dobrzyński, M.; Szymonowicz, M.; Rybak. Z. Stem cells: Past, present, and future. Stem Cell Res. Ther. 2019, 10, 68. [Google Scholar] [CrossRef]
- Galipeau, J.; Sensebe, L. Mesenchymal stromal cells: Clinical challenges and therapeutic opportunities. Cell Stem Cell 2018, 22, 824–833. [Google Scholar] [CrossRef]
- Squillaro, T.; Peluso, G.; Galderisi, U. Clinical trials with mesenchymal stem cells: An update. Cell Transplant. 2016, 25, 829–848. [Google Scholar] [CrossRef] [PubMed]
- Trounson, A.; McDonald, C. Stem cell therapies in clinical trials: Progress and challenges. Cell Stem Cell 2015, 17, 11–22. [Google Scholar] [CrossRef] [PubMed]
- Naji, A.; Rouas-Freiss, N.; Durrbach, A.; Carosella, E.D.; Sensébé, L.; Deschaseaux, F. Concise review: Combining human leukocyte antigen G and mesenchymal stem cells for immunosuppressant biotherapy. Stem Cells 2013, 31, 2296–2303. [Google Scholar] [CrossRef] [PubMed]
- Naji, A.; Suganuma, N.; Espagnolle, N.; Yagyu, K.; Baba, N.; Sensebe, L.; Deschaseaux, F. Rationale for determining the functional potency of mesenchymal stem cells in preventing regulated cell death for therapeutic use. Stem Cells Transl. Med. 2017, 6, 713–719. [Google Scholar] [CrossRef] [PubMed]
- Aleksandrushkina, N.A.; Danilova, N.V.; Grigorieva, O.A.; Mal’kov, P.G.; Popov, V.S.; Efimenko, A.Y.; Makarevich, P.I. Cell sheets of mesenchymal stromal cells effectively stimulate healing of deep soft tissue defects. Bull. Exp. Biol. Med. 2019, 167, 159–163. [Google Scholar] [CrossRef]
- Caplan, A.I. Mesenchymal stem cells. J. Orthop. Res. 1991, 9, 641–650. [Google Scholar] [CrossRef]
- Bianco, P. “Mesenchymal” stem cells. Annu. Rev. Cell Dev. Biol. 2014, 30, 677–704. [Google Scholar] [CrossRef]
- Caplan, A.I. Mesenchymal stem cells: Time to change the name! Stem Cells Transl. Med. 2017, 6, 1445–1451. [Google Scholar] [CrossRef]
- Bhartiya, D. The need to revisit the definition of mesenchymal and adult stem cells based on their functional attributes. Stem Cell Res. 2018, 9, 78. [Google Scholar] [CrossRef]
- Alvarez-Viejo, M.; Menendez-Menendez, Y.; Otero-Hernández, J. CD271 as a marker to identify mesenchymal stem cells from diverse sources be-fore culture. World J. Stem Cells 2015, 7, 470–476. [Google Scholar] [CrossRef]
- Lv, F.-J.; Tuan, R.S.; Cheung, K.M.C.; Leung, V.Y.L. Concise Review: The surface markers and identity of human mesenchymal stem cells. Stem Cells 2014, 32, 1408–1419. [Google Scholar] [CrossRef]
- Berebichez-Fridman, R.; Gomez-García, R.; Granados-Montiel, J.; Berebichez-Fastlicht, E.; Olivos-Meza, A.; Granados, J. The holy grail of orthopedic surgery: Mesenchymal stem cells—Their current uses and potential applications. Stem Cells Int. 2017, 2017, 2638305. [Google Scholar] [CrossRef]
- Hass, R.; Kasper, C.; Bohm, S.; Jacobs, R. Different populations and sources of human mesenchymal stem cells (MSC): A comparison of adult and neonatal tissue-derived MSC. Cell Commun. Signal. 2011, 9, 12. [Google Scholar] [CrossRef]
- Costela-Ruiz, V.J.; Melguizo-Rodriguez, L.; Bellotti, C.; Il-lescas-Montes, R.; Stanco, D.; Arciola, C.R.; Lucarelli, E. Different sources of mesenchymal stem cells for tissue regeneration: A guide to identifying the most favorable one in orthopedics and dentistry applications. Int. J. Mol. Sci. 2022, 23, 6356. [Google Scholar] [CrossRef]
- Mazini, L.; Rochette, L.; Amine, M.; Malka, G. Regenerative capacity of adipose-derived stem cells (ADSCs), Comparison with Mesenchymal Stem Cells (MSCs). Int. J. Mol. Sci. 2019, 20, 2523. [Google Scholar] [CrossRef]
- Jin, H.J.; Bae, Y.K.; Kim, M.; Kwon, S.J.; Jeon, H.B.; Choi, S.J.; Kim, S.W.; Yang, Y.S.; Oh, W.; Chang, J.W. Comparative analysis of human mesenchymal stem cells from bone marrow, adipose tissue, and umbilical cord blood as sources of cell therapy. Int. J. Mol. Sci. 2013, 14, 17986–18001. [Google Scholar] [CrossRef]
- Arutyunyan, I.; Elchaninov, A.; Makarov, A.; Fatkhudinov, T. Umbilical cord as prospective source for mesenchymal stem cell-based therapy. Stem Cells Int. 2016, 2016, 6901286. [Google Scholar] [CrossRef]
- Selich, A.; Zimmermann, K.; Tenspolde, M.; Dittrich-Breiholz, O.; von Kaisenberg, C.; Schambach, A.; Rothe, M. Umbilical cord as a long-term source of activatable mesenchymal stromal cells for immunomodulation. Stem Cell Res. Ther. 2019, 1, 285. [Google Scholar] [CrossRef]
- Fukuchi, Y.; Nakajima, H.; Sugiyama, D.; Hirose, I.; Kitamura, T.; Tsuji, K. Human placenta-derived cells have mesenchymal stem/progenitor cell potential. Stem Cells 2004, 22, 649–658. [Google Scholar] [CrossRef]
- Thaweesapphithak, S.; Tantrawatpan, C.; Kheolamai, P.; Tantikanlayaporn, D.; Roytrakul, S.; Manochantr, S. Human serum enhances the proliferative capacity and immunomodulatory property of MSCs derived from human placenta and umbilical cord. Stem Cell Res. Ther. 2019, 10, 79. [Google Scholar] [CrossRef]
- Mastrolia, I.; Foppiani, E.M.; Murgia, A.; Candini, O.; Samarelli, A.V.; Grisendi, G.; Veronesi, E.; Horwitz, E.M.; Dominici, M. Challenges in clinical development of mesenchymal stromal/stem cells: Concise Review. Stem Cells Transl. Med. 2019, 8, 1135–1148. [Google Scholar] [CrossRef] [PubMed]
- Cheng, H.Y.; Ghetu, N.; Wallace, C.G.; Wei, F.C.; Liao, S.K. The impact of mesenchymal stem cell source on proliferation, differentiation, immunomodulation and therapeutic efficacy. J. Stem Cell Res. Ther. 2014, 4, 237. [Google Scholar] [CrossRef]
- Choudhery, M.S.; Badowski, M.; Muise, A.; Pierce, J.; Harris, D.T. Donor age negatively impacts adipose tissue-derived mesenchymal stem cell expansion and differentiation. J. Transl. Med. 2014, 12, 8. [Google Scholar] [CrossRef] [PubMed]
- Cagliani, J.; Grande, D.; Molmenti, E.P.; Miller, E.J.; Rilo, H.L.R. Immunomodulation by mesenchymal stromal cells and their clinical applications. J. Stem Cell Regen. Biol. 2017, 3, 1–26. [Google Scholar] [CrossRef]
- Kim, J.H.; Chris, H.J.; Kim, H.R.; Hwang, Y.I. Comparison of immunological characteristics of mesenchymal stem cells from the periodontal ligament, umbilical cord, and adipose tissue. Stem Cells Int. 2018, 2018, 8429042. [Google Scholar] [CrossRef]
- In’t Anker, P.S.; Scherjon, S.A.; Kleijburg-van der Keur, C.; de Groot-Swings, G.M.; Claas, F.H.; Fibbe, W.E. Isolation of mesenchymal stem cells of fetal or maternal origin from human placenta. Stem Cells 2004, 22, 1338–1345. [Google Scholar] [CrossRef]
- Pipino, C.; Shangaris, P.; Resca, E.; Zia, S.; Deprest, J.; Sebire, N.J.; David, A.L.; Guillot, P.V.; De Coppiet, P. Placenta as a reservoir of stem cells: An underutilized resource? Br. Med. Bull. 2013, 105, 43–68. [Google Scholar] [CrossRef]
- Dominici, M.; Le Blanc, K.; Mueller, I.; Slaper-Cortenbach, I.; Marini, F.; Krause, D.; Deans, R.; Keating, A.; Prockop, D.; Horwitz, E. Minimal criteria for defining multipotent mesenchymal stromal cells. The International Society for Cellular Therapy position statement. Cytotherapy 2006, 8, 315–317. [Google Scholar] [CrossRef] [PubMed]
- Mushahary, D.; Spittler, A.; Kasper, C.; Weber, V.; Charwat, V. Isolation, cultivation, and characterization of human mesenchymal stem cells. Cytometry A 2018, 1, 19–31. [Google Scholar] [CrossRef]
- Nagamura-Inoue, T.; He, H. Umbilical cord-derived mesenchymal stem cells: Their advantages and potential clinical utility. World J. Stem Cells 2014, 6, 195–202. [Google Scholar] [CrossRef]
- Chen, Y.; Shao, J.Z.; Xiang, L.X.; Dong, X.J.; Zhang, G.R. Mesenchymal stem cells: A promising candidate in regenerative medicine. Int. J. Biochem. Cell Biol. 2008, 40, 815–820. [Google Scholar] [CrossRef]
- Nimiritsky, P.P.; Eremichev, R.Y.; Alexandrushkina, N.A.; Efimenko, A.Y.; Tkachuk, V.A.; Makarevich, P.I. Unveiling mesenchymal stromal cells’ organizing function in regeneration. Int. J. Mol. Sci. 2019, 20, 823. [Google Scholar] [CrossRef]
- Dai, L.-J.; Moniri, M.R.; Zeng, Z.-R.; Zhou, J.X.; Rayat, J.; Warnock, G.L. Potential implications of mesenchymal stem cells in cancer therapy. Cancer Lett. 2011, 305, 8–20. [Google Scholar] [CrossRef]
- Shah, K. Mesenchymal stem cells engineered for cancer therapy. Adv. Drug Deliv. Rev. 2012, 64, 739–748. [Google Scholar] [CrossRef]
- Yudintceva, N.; Lomert, E.; Mikhailova, N.; Tolkunova, E.; Agadzhanian, N.; Samochernych, K.; Multhoff, G.; Timin, G.; Ryzhov, V.; Deriglazov, V.; et al. Targeting brain tumors with mesenchymal stem cells in the experimental model of the orthotopic glioblastoma in rats. Biomedicines 2021, 9, 1592. [Google Scholar] [CrossRef]
- Shi, Y.; Wang, Y.; Li, Q.; Liu, K.; Hou, J.; Shao, C.; Wang, Y. Immunoregulatory mechanisms of mesenchymal stem and stromal cells in inflammatory diseases. Nat. Rev. Nephrol. 2018, 14, 493–507. [Google Scholar] [CrossRef]
- Jin, S.S.; He, D.Q.; Luo, D.; Wang, Y.; Yu, M.; Guan, B.; Fu, Y.; Li, Z.X.; Zhang, T.; Zhou, Y.H.; et al. A Biomimetic hierarchical nanointerface orchestrates macrophage polarization and mesenchymal stem cell recruitment to promote endogenous bone regeneration. ACS Nano 2019, 13, 6581–6595. [Google Scholar] [CrossRef]
- Zhang, Y.; Xu, J.; Liu, S.; Lim, M.; Zhao, S.; Cui, K.; Zhang, K.; Wang, L.; Ji, Q.; Han, Z.; et al. Embryonic stem cell-derived extracellular vesicles enhance the therapeutic effect of mesenchymal stem cells. Theranostics 2019, 9, 6976–6990. [Google Scholar] [CrossRef]
- Cao, X.; Duan, L.; Hou, H.; Liu, Y.; Chen, S.; Zhang, S.; Liu, Y.; Wang, C.; Qi, X.; Liu, N.; et al. IGF-1C hydrogel improves the therapeutic effects of MSCs on colitis in mice through PGE2-mediated M2macrophage polarization. Theranostics 2020, 10, 7697–7709. [Google Scholar] [CrossRef]
- Ceccariglia, S.; Cargnoni, A.; Silini, A.R.; Parolini, O. Autophagy: A potential key contributor to the therapeutic action of mesenchymal stem cells. Autophagy 2020, 1, 28–37. [Google Scholar] [CrossRef]
- Liu, Y.; Cui, J.; Wang, H.; Hezam, K.; Zhao, X.; Huang, H.; Chen, S.; Han, Z.; Han, Z.C.; Guo, Z.; et al. Enhanced therapeutic effects of MSC-derived extracellular vesicles with an injectable collagen matrix for experimental acute kidney injury treatment. Stem Cell Res. Ther. 2020, 11, 161. [Google Scholar] [CrossRef] [PubMed]
- Tao, H.; Chen, X.; Cao, H.; Zheng, L.; Li, Q.; Zhang, K.; Han, Z.; Han, Z.C.; Guo, Z.; Li, Z.; et al. Mesenchymal stem cell-derived extracellular vesicles for corneal wound repair. Stem Cells Int. 2019, 2019, 5738510. [Google Scholar] [CrossRef] [PubMed]
- Crivelli, B.; Chlapanidas, T.; Perteghella, S.; Lucarelli, E.; Pascucci, L.; Brini, A.T.; Ferrero, I.; Marazzi, M.; Pessina, A.; Torre, M.L. Mesenchymal stem/stromal cell extracellular vesicles: From active principle to next generation drug delivery system. J. Control. Release 2017, 262, 104–117. [Google Scholar] [CrossRef] [PubMed]
- Taghavi-Frahabadi, M.; Mahmoudi, M.; Soudi, S.; Hashemi, S.M. Hypothesis for the management and treatment of the COVID-19-induced acute respiratory distress syndrome and lung injury using mesenchymal stem cell—Derived exosomes. Med. Hypotheses 2020, 144, 109865. [Google Scholar] [CrossRef] [PubMed]
- Rahmati, S.; Shojaei, F.; Shojaeian, A.; Rezakhani, L.; Dehkordi, M.B. An overview of current knowledge in biological functions and potential theragnostic applications of exosomes. Chem. Phys. Lipids 2020, 226, 104836. [Google Scholar] [CrossRef]
- Lener, T.; Gimona, M.; Aigner, L.; Borger, V.; Buzas, E.; Camussi, G.; Chaput, N.; Chatterjee, D.; Court, F.A.; Del Portillo, H.A.; et al. Applying extracellular vesicles based therapeutics in clinical trials—An ISEV position paper. J. Extracell. Vesicles 2015, 4, 30087. [Google Scholar] [CrossRef]
- Jia, X.H.; Lu, H.; Li, C.; Feng, G.W.; Yao, X.P.; Mao, L.N.; Ke, T.Y.; Che, Y.Z.; Xu, Y.; Li, Z.J.; et al. Human embryonic stem cells-derived endothelial cell therapy facilitates kidney regeneration by stimulating renal resident stem cell proliferation in acute kidney injury. Chin. Sci. Bull. 2013, 58, 2820–2827. [Google Scholar] [CrossRef][Green Version]
- Mardpour, S.; Hamidieh, A.A.; Taleahmad, S.; Sharifzad, F.; Taghikhani, A.; Baharvand, H. Interaction between mesenchymal stromal cell-derived extracellular vesicles and immune cells by distinct protein content. J. Cell Physiol. 2019, 234, 8249–8258. [Google Scholar] [CrossRef]
- Kim, H.; Lee, M.J.; Bae, E.H.; Ryu, J.S.; Kaur, G.; Kim, H.J.; Kim, J.Y.; Barreda, H.; Jung, S.Y.; Choi, J.M. Comprehensive Molecular Profiles of Functionally Effective MSC-Derived Extracellular Vesicles in Immunomodulation. Mol. Ther. 2020, 28, 1628–1644. [Google Scholar] [CrossRef]
- Franco da Cunha, F.; Andrade-Oliveira, V.; Candido de Almeida, D.; Borges da Silva, T.; Naffah de Souza Breda, C.; Costa Cruz, M. Extracellular vesicles isolated from mesenchymal stromal cells modulate CD4(+) T Lymphocytes toward a regulatory profile. Cells 2020, 9, 1059. [Google Scholar] [CrossRef]
- Shigemoto-Kuroda, T.; Oh, J.Y.; Kim, D.K.; Jeong, H.J.; Park, S.Y.; Lee, H.J.; Park, J.W.; Kim, T.W.; An, S.Y.; Prockop, D.J.; et al. MSC-derived extracellular vesicles attenuate immune responses in two autoimmune murine models: Type 1 diabetes and uveoretinitis. Stem Cell Rep. 2017, 8, 1214–1225. [Google Scholar] [CrossRef]
- Zhang, Z.; Huang, S.; Wu, S.; Qi, J.; Li, W.; Liu, S. Clearance of apoptotic cells by mesenchymal stem cells contributes to immunosuppression via PGE2. EBioMedicine 2019, 45, 341–350. [Google Scholar] [CrossRef]
- Wang, K.; Shi, Y.J.; Song, Z.L.; Wu, B.; Zhou, C.L.; Liu, W.; Gao, W. Regulatory effect of rat bone marrow mesenchymal stem cells on Treg/Th17 immune balance in vitro. Mol. Med. Rep. 2020, 21, 2123–2130. [Google Scholar] [CrossRef]
- Luo, S.; Ding, S.; Liao, J.; Zhang, P.; Liu, Y.; Zhao, M.; Zhao, M.; Lu, Q. Excessive miR-152-3p Results in Increased BAFF Expression in SLE B-Cells by Inhibiting the KLF5 Expression. Front. Immunol. 2019, 10, 1127. [Google Scholar] [CrossRef]
- Adamo, A.; Brandi, J.; Caligola, S.; Delfino, P.; Bazzoni, R.; Carusone, R.; Cecconi, D.; Giugno, R.; Manfredi, M.; Robotti, E.; et al. Extracellular vesicles mediate mesenchymal stromal cell-dependent regulation of B cell PI3K-AKT signaling pathway and actin cytoskeleton. Front. Immunol. 2019, 10, 446. [Google Scholar] [CrossRef]
- Yang, L.; Li, N.; Yang, D.; Chen, A.; Tang, J.; Jing, Y.; Kang, D.; Jiang, P.; Dai, X.; Luo, L.; et al. CCL2 Regulation of MST1-mTOR-STAT1 Signaling Axis Controls BCR Signaling and B-Cell Differentiation. Cell Death Differ. 2021, 28, 2616–2633. [Google Scholar] [CrossRef]
- Reis, M.; Mavin, E.; Nicholson, L.; Green, K.; Dickinson, A.M.; Wang, X.N. Mesenchymal stromal cell-derived extracellular vesicles attenuate dendritic cell maturation and function. Front. Immunol. 2018, 9, 2538. [Google Scholar] [CrossRef]
- Hu, C.D.; Kosaka, Y.; Marcus, P.; Rashedi, I.; Keating, A. Differential immunomodulatory effects of human bone marrow-derived mesenchymal stromal cells on natural killer cells. Stem Cells Dev. 2019, 28, 933–943. [Google Scholar] [CrossRef]
- Najar, M.; Fayyad-Kazan, M.; Meuleman, N.; Bron, D.; Fayyad-Kazan, H.; Lagneaux, L. Mesenchymal stromal cells of the bone marrow and natural killer cells: Cell interactions and cross modulation. J. Cell Commun. Signal. 2018, 12, 673–688. [Google Scholar] [CrossRef]
- Selleri, S.; Bifsha, P.; Civini, S.; Pacelli, C.; Dieng, M.M.; Lemieux, W.; Jin, P.; Bazin, R.; Patey, N.; Marincolet, F.M.; et al. Human Mesenchymal Stromal Cell-Secreted Lactate Induces M2-Macrophage Differentiation by Metabolic Reprogramming. Oncotarget 2016, 7, 30193–30210. [Google Scholar] [CrossRef]
- Hyvarinen, K.; Holopainen, M.; Skirdenko, V.; Ruhanen, H.; Lehenkari, P.; Korhonen, M. Mesenchymal stromal cells and their extracellular vesicles enhance the anti-inflammatory phenotype of regulatory macrophages by downregulating the production of Interleukin (IL)-23 and IL-22. Front. Immunol. 2018, 9, 771. [Google Scholar] [CrossRef] [PubMed]
- Lo Sicco, C.; Reverberi, D.; Balbi, C.; Ulivi, V.; Principi, E.; Pascucci, L. Mesenchymal stem cell-derived extracellular vesicles as mediators of anti-inflammatory effects: Endorsement of macrophage polarization. Stem Cells Transl. Med. 2017, 6, 1018–1028. [Google Scholar] [CrossRef] [PubMed]
- He, X.; Dong, Z.; Cao, Y.; Wang, H.; Liu, S.; Liao, L.; Jin, Y.; Yuan, L.; Li, B. MSC-derived exosome promotes M2 polarization and enhances cutaneous wound healing. Stem Cells Int. 2019, 2019, 7132708. [Google Scholar] [CrossRef] [PubMed]
- Xin, D.; Li, T.; Chu, X.; Ke, H.; Yu, Z.; Cao, L.; Wang, Z. Mesenchymal stromal cell-derived extracellular vesicles modulate microglia/macrophage polarization and protect the brain against hypoxia-ischemic injury in neonatal mice by targeting delivery of miR-21a-5p. Acta Biomater. 2020, 113, 597–613. [Google Scholar] [CrossRef] [PubMed]
- Chen, X.; Wei, Q.; Sun, H.; Zhang, X.; Yang, C.; Tao, Y.; Nong, G. Exosomes derived from human umbilical cord mesenchymal stem cells regulate macrophage polarization to attenuate systemic lupus erythematosus-associated diffuse alveolar hemorrhage in mice. Int. J. Stem Cells 2021, 14, 331–340. [Google Scholar] [CrossRef]
- Costa, L.A.; Eiro, N.; Fraile, M.; Gonzalez, L.O.; Saa, J.; Garcia-Portabella, P.; Vega, B.; Schneider, J.; Vizoso, F.J. Functional heterogeneity of mesenchymal stem cells from natural niches to culture conditions: Implications for further clinical uses. Cell Mol. Life Sci. 2021, 78, 447–467. [Google Scholar] [CrossRef]
- Levy, O.; Kuai, R.; Siren, E.M.J.; Bhere, D.; Milton, Y.; Nissar, N.; De Biasio, M.; Heinelt, M.; Reeve, B.; Abdi, R.; et al. Shattering barriers toward clinically meaningful MSC therapies. Sci. Adv. 2020, 6, eaba6884. [Google Scholar] [CrossRef]
- Brown, C.; McKee, C.; Bakshi, S.; Walker, K.; Hakman, E.; Halassy, S.; Svinarich, D.; Dodds, R.; Govind, C.K.; Chaudhry, G.R. Mesenchymal stem cells: Cell therapy and regeneration potential. J. Tissue Eng. Regen. Med. 2019, 13, 1738–1755. [Google Scholar] [CrossRef]
- Tavakoli, S.; Ghaderi Jafarbeigloo, H.R.; Shariati, A.; Jahangiryan, A.; Jadidi, F.; Jadidi Kouhbanani, M.A.; Hassanzadeh, A.; Zamani, M.; Javidi, K.; Naimi, A. Mesenchymal stromal cells; a new horizon in regenerative medicine. J. Cell Physiol. 2020, 235, 9185–9210. [Google Scholar] [CrossRef]
- Tang, Y.; Zhou, Y.; Li, H.J. Advances in mesenchymal stem cell exosomes: A review. Stem Cell Res. Ther. 2021, 12, 71. [Google Scholar] [CrossRef]
- He, C.; Zheng, S.; Luo, Y.; Wang, B. Exosome Theranostics: Biology and Translational Medicine. Theranostics. 2018, 8, 237–255. [Google Scholar] [CrossRef]
- Wu, J.; Kuang, L.; Chen, C.; Yang, J.; Zeng, W.N.; Li, T.; Chen, H.; Huang, S.; Fu, Z.; Li, J.; et al. miR-100−5p-Abundant exosomes derived from infrapatellar fat pad MSCs protect articular cartilage and ameliorate gait abnormalities via inhibition of mTOR in osteoarthritis. Biomaterials 2019, 206, 87–100. [Google Scholar] [CrossRef]
- Zhang, S.; Teo, K.Y.W.; Chuah, S.J.; Lai, R.C.; Lim, S.; Toh, W.S. MSC exosomes alleviate temporomandibular joint osteoarthritis by attenuating inflammation and restoring matrix homeostasis. Biomaterials 2019, 200, 35–47. [Google Scholar] [CrossRef]
- Liao, Z.; Luo, R.; Li, G.; Song, Y.; Zhan, S.; Zhao, K.; Hua, W.; Zhang, Y.; Wu, X.; Yang, C. Exosomes from mesenchymal stem cells modulate endoplasmic reticulum stress to protect against nucleus pulposus cell death and ameliorate intervertebral disc degeneration in vivo. Theranostics 2019, 9, 4084–4100. [Google Scholar] [CrossRef]
- Mihajlovic, M.; Wever, K.E.; Van der Made, T.K.; de Vries, R.B.M.; Hilbrands, L.B.; Masereeuw, R. Are cell-based therapies for kidney disease safe? A systematic review of preclinical evidence. Pharmacol. Ther. 2019, 197, 191–211. [Google Scholar] [CrossRef]
- Lai, P.; Weng, J.; Guo, L.; Chen, X.; Du, X. Novel insights into MSC-EVs therapy for immune diseases. Biomark Res. 2019, 7, 6. [Google Scholar] [CrossRef]
- Gould, S.J.; Raposo, G. As we wait: Coping with an imperfect nomenclature for extracellular vesicles. J. Extracell. Vesicles 2013, 2, 2892. [Google Scholar] [CrossRef]
- Yuana, Y.; Sturk, A.; Nieuwland, R. Extracellular vesicles in physiological and pathological conditions. Blood Rev. 2013, 27, 31–39. [Google Scholar] [CrossRef]
- Ludwig, A.-K.; Giebel, B. Exosomes: Small vesicles participating in intercellular communication. Int. J. Biochem. Cell Boil. 2012, 44, 11–15. [Google Scholar] [CrossRef]
- Yanez-Mo, M.; Siljander, P.; Andreu, Z.; Zavec, A.B.; Borras, F.E.; Buzas, E.I.; Buzas, K.; Casal, E.; Cappello, F.; Carvalho, J.; et al. Biological properties of extracellular vesicles and their physiological functions. J. Extracell. Vesicles 2015, 4, 27066. [Google Scholar] [CrossRef]
- Yates, A.G.; Pink, R.C.; Erdbrügger, U.; Siljander, P.R.; Dellar, E.R.; Pantazi, P.; Akbar, N.; Cooke, W.R.; Vatish, M.; Dias-Neto, E.; et al. In sickness and in health: The functional role of extracellular vesicles in physiology and pathology in vivo: Part I: Health and Normal Physiology: Part I: Health and Normal Physiology. J. Extracell. Vesicles 2022, 11, e12151. [Google Scholar] [CrossRef] [PubMed]
- Thery, C.; Witwer, K.W.; Aikawa, E.; Alcaraz, M.J.; Anderson, J.D.; Andriantsitohaina, R.; Antoniou, A.; Arab, T.; Archer, F.; Atkin-Smith, G.K.; et al. Minimal information for studies of extracellular vesicles 2018 (MISEV2018): A position statement of the International Society for Extracellular Vesicles and update of the MISEV2014 guidelines. J. Extracell. Vesicles 2018, 7, 1535750. [Google Scholar] [CrossRef] [PubMed]
- Yates, A.G.; Pink, R.C.; Erdbrügger, U.; Siljander, P.R.; Dellar, E.R.; Pantazi, P.; Akbar, N.; Cooke, W.R.; Vatish, M.; Dias-Neto, E.; et al. In sickness and in health: The functional role of extracellular vesicles in physiology and pathology in vivo: Part II: Pathology: Part II: Pathology. J. Extracell. Vesicles 2022, 11, e12190. [Google Scholar] [CrossRef] [PubMed]
- Lobov, A.A.; Yudintceva, N.M.; Mittenberg, A.G.; Shabelnikov, S.V.; Mikhailova, N.A.; Malashicheva, A.B.; Khotin, M.G. Proteomic profiling of the human fetal multipotent mesenchymal stromal cells secretome. Molecules 2020, 25, 5283. [Google Scholar] [CrossRef] [PubMed]
- Rahbarghazi, R.; Jabbari, N.; Sani, N.A.; Asghari, R.; Salimi, L.; Kalashani, S.A. Tumor-derived extracellular vesicles: Reliable tools for Cancer diagnosis and clinical applications. Cell Commun. Signal. 2019, 17, 73. [Google Scholar] [CrossRef]
- Gonda, A.; Kabagwira, J.; Senthil, G.N.; Wall, N.R. Internalization of Exosomes through Receptor-Mediated Endocytosis. Mol. Cancer Res. 2019, 2, 337–347. [Google Scholar] [CrossRef]
- Cheng, H.; Chang, S.; Xu, R.; Chen, L.; Song, X.; Wu, J.; Qian, J.; Zou, Y.; Ma, J. Hypoxia-challenged MSC-derived exosomes deliver miR-210 to attenuate post-infarction cardiac apoptosis. Stem Cell Res. Ther. 2020, 11, 224. [Google Scholar] [CrossRef]
- Feng, J.; Wang, W. Hypoxia pretreatment and EPO-modification enhance the protective effects of MSC on neuron-like PC12 cells in a similar way. Biochem. Biophys. Res. Commun. 2017, 482, 232–238. [Google Scholar] [CrossRef]
- Carter, K.; Lee, H.J.; Na, K.S.; Fernandes-Cunha, G.M.; Blanco, I.J.; Djalilian, A.; Myung, D. Characterizing the impact of 2D and 3D culture conditions on the therapeutic effects of human mesenchymal stem cell secretome on corneal wound healing in vitro and ex vivo. Acta Biomater. 2019, 99, 247–257. [Google Scholar] [CrossRef]
- Fernandes-Cunha, G.M.; Na, K.S.; Putra, I.; Lee, H.; Hull, S.; Cheng, Y.C.; Blanco, I.J.; Eslani, M.; Djalilian, A.R.; Myung, D. Corneal wound healing effects of mesenchymal stem cell secretome delivered within a viscoelastic gel carrier. Stem Cells Transl. Med. 2019, 8, 478–489. [Google Scholar] [CrossRef]
- Kaminska, A.; Wedzinska, A.; Kot, M.; Sarnowska, A. Effect of long-term 3D spheroid culture on WJ-MSC. Cells 2021, 10, 719. [Google Scholar] [CrossRef]
- Kanada, M.; Ashammakhi, N. Discussion of the role of extracellular vesicles secreted from thermal stress-induced adipose-derived stem cells on bone regeneration. J. Craniofac. Surg. 2021, 32, 2251. [Google Scholar] [CrossRef]
- Jafari, D.; Shajari, S.; Jafari, R.; Mardi, N.; Gomari, H.; Ganji, F.; Moghadam, M.F.; Samadikuchaksaraei, A. Designer Exosomes: A new platform for biotechnology therapeutics. BioDrugs 2020, 34, 567–586. [Google Scholar] [CrossRef]
- Jiang, Y.; Zhang, P.; Zhang, X.; Lv, L.; Zhou, Y. Advances in mesenchymal stem cell transplantation for the treatment of osteoporosis. Cell Prolif. 2021, 54, e12956. [Google Scholar] [CrossRef]
- Xu, L.; Huang, S.; Hou, Y.; Liu, Y.; Ni, M.; Meng, F.; Wang, K.; Rui, Y.; Jiang, X.; Li, G. Sox11-modified mesenchymal stem cells (MSCs) accelerate bone fracture healing: Sox11 regulates differentiation and migration of MSCs. FASEB J. 2015, 29, 1143–1152. [Google Scholar] [CrossRef]
- Garcia-Sanchez, D.; Fernandez, D.; Rodríguez-Rey, J.C.; Perez-Campo, F.M. Enhancing survival, engraftment, and osteogenic potential of mesenchymal stem cells. World J. Stem Cells 2019, 11, 748–763. [Google Scholar] [CrossRef]
- Song, H.; Song, B.-W.; Cha, M.-J.; Choi, I.-G.; Hwang, K.-C. Modification of mesenchymal stem cells for cardiac regeneration. Expert Opin. Biol. Ther. 2010, 10, 309–319. [Google Scholar] [CrossRef]
- Ocansey, D.K.W.; Pei, B.; Yan, Y.; Qian, H.; Zhang, X.; Xu, W.; Mao, F. Improved therapeutics of modified mesenchymal stem cells: An update. J. Transl. Med. 2020, 18, 42. [Google Scholar] [CrossRef]
- Wang, H.; Wang, X.; Qu, J.; Yue, Q.; Hu, Y.; Zhang, H. VEGF enhances the migration of MSCs in neural differentiation by regulating focal adhesion turnover. J. Cell Physiol. 2015, 230, 2728–2742. [Google Scholar] [CrossRef]
- De Becker, A.; Van Riet, I. Homing and migration of mesenchymal stromal cells: How to improve the efficacy of cell therapy? World J. Stem Cells 2016, 8, 73–87. [Google Scholar] [CrossRef]
- Nolta, J.A.; Galipeau, J.; Phinney, D.G. Improving mesenchymal stem/stromal cell potency and survival: Proceedings from the International Society of Cell Therapy (ISCT) MSC preconference held in May 2018, Palais des Congrès de Montréal, Organized by the ISCT MSC Scientific Committee. Cytotherapy 2020, 22, 123–126. [Google Scholar] [CrossRef] [PubMed]
- Chen, L.; Xu, Y.; Zhao, J.; Zhang, Z.; Yang, R.; Xie, J.; Liu, X.; Qi, S. Conditioned medium from hypoxic bone marrow-derived mesenchymal stem cells enhances wound healing in mice. PLoS ONE 2014, 9, e96161. [Google Scholar] [CrossRef] [PubMed]
- Van der Pol, E.; Boing, A.N.; Harrison, P.; Sturk, A.; Nieuwland, R. Classification, functions, and clinical relevance of extracellular vesicles. Pharmacol. Rev. 2012, 64, 676–705. [Google Scholar] [CrossRef] [PubMed]
- Hu, L.; Wang, J.; Zhou, X.; Xiong, Z.; Zhao, J.; Yu, R.; Huang, F.; Zhang, H.; Chen, L. Exosomes derived from human adipose mensenchymal stem cells accelerates cutaneous wound healing via optimizing the characteristics of fibroblasts. Sci. Rep. 2016, 6, 32993. [Google Scholar] [CrossRef] [PubMed]
- Borges, F.T.; Reis, L.A.; Schor, N. Extracellular vesicles: Structure, function, and potential clinical uses in renal diseases. Braz. J. Med. Biol. Res. 2013, 46, 824–830. [Google Scholar] [CrossRef]
- Facklam, A.L.; Volpatti, L.R.; Anderson, D.G. Biomaterials for personalized cell therapy. Adv. Mater. 2020, 32, 1902005. [Google Scholar] [CrossRef]
- Qazi, T.H.; Mooney, D.J.; Duda, G.N.; Geissler, S. Biomaterials that promote cell–cell interactions enhance the paracrine function of MSCs. Biomaterials 2017, 140, 103–114. [Google Scholar] [CrossRef]
- Dergilev, K.V.; Makarevich, P.I.; Tsokolaeva, Z.I.; Bodyrva, M.A.; Beloglazova, I.B.; Zubkova, E.S.; Menshikov, M.Y.; Parfyonova, Y.V. Comparison of cardiac stem cell sheets detached by Versen solution and from termoresponsive dishes revealssimilar properties of constructs. Tissue Cell 2017, 49, 64–71. [Google Scholar] [CrossRef]
- Kim, K.; Bou-Ghannam, S.; Kameishi, S.; Oka, M.; Grainger, D.W.; Okano, T. Allogeneic mesenchymal stem cell sheet therapy: A new frontier in drug delivery systems. J. Control. Release 2021, 330, 696–704. [Google Scholar] [CrossRef]
- Chang, D.; Fan, T.; Gao, S.; Jin, Y.; Zhang, M.; Ono, M. Application of mesenchymal stem cell sheet to treatment of ischemic heart disease. Stem Cell Res. Ther. 2021, 12, 384. [Google Scholar] [CrossRef]
- Du, W.; Zhang, K.Y.; Zhang, S.Q.; Wang, R.; Nie, Y.; Tao, H.Y.; Han, Z.B.; Liang, L.; Wang, D.; Liu, J.F.; et al. Enhanced proangiogenic potential of mesenchymal stem cell-derived exosomes stimulated by a nitric oxide releasing polymer. Biomaterials 2017, 133, 70–81. [Google Scholar] [CrossRef]
- Zhu, L.; Kalimuthu, S.; Oh, J.M.; Gangadaran, P.; Baek, S.H.; Jeong, S.Y.; Lee, S.-W.; Lee, J.; Ahn, B.-C. Enhancement of Antitumor Potency of Extracellular Vesicles Derived from Natural Killer Cells by IL-15 Priming. Biomaterials 2019, 190, 38–50. [Google Scholar] [CrossRef]
- Hu, C.; Li, L. Preconditioning influences mesenchymal stem cell properties in vitro and in vivo. J. Cell Mol. Med. 2018, 3, 1428–1442. [Google Scholar] [CrossRef]
- Phillips, M.I.; Tang, Y.L. Genetic modification of stem cells for transplantation. Adv. Drug Deliv. Rev. 2008, 60, 160–172. [Google Scholar] [CrossRef]
- Olson, S.D.; Kambal, A.; Pollock, K.; Mitchell, G.M.; Stewart, H.; Kalomoiris, S.; Cary, W.; Nacey, C.; Pepper, K.; Nolta, J.A. Examination of mesenchymal stem cell-mediated RNAi transfer to Huntington’s disease affected neuronal cells for reduction of Huntingtin. Mol. Cell. Neurosci. 2012, 49, 271–281. [Google Scholar] [CrossRef]
- Armstrong, J.P.; Holme, M.N.; Stevens, M.M. Re-Engineering Extracellular Vesicles as Smart Nanoscale Therapeutics. ACS Nano 2017, 11, 69–83. [Google Scholar] [CrossRef]
- Gupta, D.; Zickler, A.M.; Andaloussi, S.E. Dosing extracellular vesicles. Adv. Drug Deliv. Rev. 2021, 178, 113961. [Google Scholar] [CrossRef]
- Villata, S.; Canta, M.; Cauda, V. EVs and Bioengineering: From cellular products to engineered nanomachines. Int. J. Mol. Sci. 2020, 21, 6048. [Google Scholar] [CrossRef]
- Mishra, A.; Singh, P.; Qayoom, I.; Prasad, A.; Kumar, A. Current strategies in tailoring methods for engineered exosomes and future avenues in biomedical applications. J. Mater. Chem. B 2021, 9, 6281–6309. [Google Scholar] [CrossRef]
- Wang, H.; Cui, J.; Zheng, Z.; Shi, Q.; Sun, T.; Liu, X.; Huang, Q.; Fukuda, T. Assembly of RGD-modified hydrogel micromodules into permeable three-dimensional hollow microtissues mimicking in vivo tissue structures. ACS Appl. Mater. Interfaces 2017, 9, 41669–41679. [Google Scholar] [CrossRef]
- Zheng, W.; Wang, Z.; Song, L.; Zhao, Q.; Zhang, J.; Li, D.; Wang, S.; Han, J.; Zheng, X.L.; Yang, Z.; et al. Endothelialization and patency of RGD-functionalized vascular grafts in a rabbit carotid artery model. Biomaterials 2012, 33, 2880–2891. [Google Scholar] [CrossRef] [PubMed]
- Wang, J.; Li, W.; Lu, Z.; Zhang, L.; Hu, Y.; Li, Q.; Du, W.; Feng, X.; Jia, H.; Liu, B.F. The use of RGD-engineered exosomes for enhanced targeting ability and synergistic therapy toward angiogenesis. Nanoscale 2017, 9, 15598–15605. [Google Scholar] [CrossRef] [PubMed]
- Han, C.; Zhou, J.; Liang, C.; Liu, B.; Pan, X.; Zhang, Y.; Wang, Y.; Yan, B.; Xie, W.; Liu, F.; et al. Human umbilical cord mesenchymal stem cell derived exosomes encapsulated in functional peptide hydrogels promote cardiac repair. Biomater. Sci. 2019, 7, 2920–2933. [Google Scholar] [CrossRef] [PubMed]
- Wang, C.; Wang, M.; Xu, T.; Zhang, X.; Lin, C.; Gao, W.; Xu, H.; Lei, B.; Mao, C. Engineering bioactive self-healing antibacterial exosomes hydrogel for promoting chronic diabetic wound healing and complete skin regeneration. Theranostics 2019, 9, 65–76. [Google Scholar] [CrossRef] [PubMed]
- Zhang, C.; Shang, Y.; Chen, X.; Midgley, A.C.; Wang, Z.; Zhu, D.; Wu, J.; Chen, P.; Wu, L.; Wang, X.; et al. Supramolecular nanofibers containing Arginine-Glycine-Aspartate (RGD) peptides boost therapeutic efficacy of extracellular vesicles in kidney repair. ACS Nano 2020, 14, 12133–12147. [Google Scholar] [CrossRef]
- Mardpour, S.; Ghanian, M.H.; Sadeghi-Abandansari, H.; Mardpour, S.; Nazari, A.; Shekari, F.; Baharvand, H. Hydrogel-mediated sustained systemic delivery of mesenchymal stem cell-derived extracellular vesicles improves hepatic regeneration in chronic liver failure. ACS Appl. Mater. Interfaces 2019, 11, 37421–37433. [Google Scholar] [CrossRef]
- Liu, X.; Yang, Y.; Li, Y.; Niu, X.; Zhao, B.; Wang, Y.; Bao, C.; Xie, Z.; Lin, Q.; Zhu, L. Integration of stem cell-derived exosomes with in situ hydrogel glue as a promising tissue patch for articular cartilage regeneration. Nanoscale 2017, 9, 4430–4438. [Google Scholar] [CrossRef]
- Aryani, A.; Denecke, B. Exosomes as a nanodelivery system: A key to the future of neuromedicine? Mol. Neurobiol. 2016, 53, 818–834. [Google Scholar] [CrossRef]
- Malekian, F.; Shamsian, A.; Kodam, S.P.; Ullah, M. Exosome engineering for efficient and targeted drug delivery: Current status and future perspective. J. Physiol. 2022, 16, 1–20. [Google Scholar] [CrossRef]
- Luan, X.; Sansanaphongpricha, K.; Myers, I.; Chen, H.; Yuan, H. Engineering exosomes as refined biological nanoplatforms for drug delivery Acta Pharmacol. Sin. 2017, 38, 754–763. [Google Scholar] [CrossRef]
- Zhou, Y.; Yamamoto, Y.; Xiao, Z.; Ochiya, T. The immunomodulatory functions of mesenchymal stromal/stem cells mediated via paracrine activity. J. Clin. Med. 2019, 8, 1025. [Google Scholar] [CrossRef]
- Ghannam, S.; Pene, J.; Moquet-Torcy, G.; Jorgensen, C.; Yssel, H. Mesenchymal stem cells inhibit human Th17 cell differentiation and function and induce a T regulatory cell phenotype. J. Immunol. 2010, 185, 302–312. [Google Scholar] [CrossRef]
- Spaggiari, G.M.; Capobianco, A.; Abdelrazik, H.; Becchetti, F.; Mingari, M.C.; Moretta, L. Mesenchymal stem cells inhibit natural killer–cell proliferation, cytotoxicity, and cytokine production: Role of indoleamine 2,3-dioxygenase and prostaglandin E2. Blood 2008, 111, 1327–1333. [Google Scholar] [CrossRef]
- Liras, A. Future research and therapeutic applications of human stem cells: General, regulatory, and bioethical aspects. J. Transl. Med. 2010, 8, 131. [Google Scholar] [CrossRef]
- Melief, S.M.; Geutskens, S.B.; Fibbe, W.E.; Roelofs, H. Multipotent stromal cells skew monocytes towards an anti-inflammatory interleukin-10-producing phenotype by production of interleukin-6. Haematologica 2013, 98, 888–895. [Google Scholar] [CrossRef]
- Franquesa, M.; Mensah, F.K.; Huizinga, R.; Strini, T.; Boon, L.; Lombardo, E.; DelaRosa, O.; Laman, J.D.; Grinyó, J.M.; Weimar, W.; et al. Human adipose tissue-derived mesenchymal stem cells abrogate plasmablast formation and induce regulatory B cells independently of T helper cells. Stem Cells 2015, 33, 880–891. [Google Scholar] [CrossRef]
- Tabera, S.; Perez-Simón, J.A.; Diez-Campelo, M.; Sanchez-Abarca, L.I.; Blanco, B.; Lopez, A.; Benito, A.; Ocio, E.; Sanchez-Guijo, F.M.; Canizo, C.; et al. The effect of mesenchymal stem cells on the viability, proliferation and differentiation of B-lymphocytes. Haematologica 2008, 93, 1301–1309. [Google Scholar] [CrossRef]
- Jiang, D.; Muschhammer, J.; Qi, Y.; Kügler, A.; de Vries, J.C.; Saffarzadeh, M.; Sindrilaru, A.; Beken, S.V.; Wlaschek, M.; Kluth, M.A.; et al. Suppression of neutrophil-mediated tissue damage—A novel skill of mesenchymal stem cells. Stem Cells 2016, 3, 2393–2406. [Google Scholar] [CrossRef]
- Aly, R.M. Current state of stem cell-based therapies: An overview. Stem Cell Investig. 2020, 7, 8. [Google Scholar] [CrossRef]
- Chari, S.; Nguyen, A.; Saxe, J. Stem cells in the clinic. Cell Stem Cell 2018, 22, 781–782. [Google Scholar] [CrossRef]
- Volarevic, V.; Markovic, B.S.; Gazdic, M.; Volarevic, A.; Jovicic, N.; Arsenijevic, N.; Armstrong, L.; Djonov, V.; Lako, M.; Stojkovic, M. Ethical and safety issues of stem cell-based therapy. Int. J. Med. Sci. 2018, 15, 36–45. [Google Scholar] [CrossRef] [PubMed]
- Wang, L.T.; Liu, K.J.; Sytwu, H.K.; Yen, M.L.; Yen, B.L. Advances in mesenchymal stem cell therapy for immune and inflammatory diseases: Use of cell-free products and human pluripotent stem cell-derived mesenchymal stem cells. Stem Cells Transl. Med. 2021, 10, 1288–1303. [Google Scholar] [CrossRef] [PubMed]
- Metcalfe, S.M. Mesenchymal stem cells and management of COVID-19 pneumonia. Med. Drug Discov. 2020, 5, 100019. [Google Scholar] [CrossRef] [PubMed]
- Gentile, P.; Sterodimas, A. Adipose-derived stromal stem cells (ASCs) as a new regenerative immediate therapy combating coronavirus (COVID-19)-induced pneumonia. Expert Opin. Biol. Ther. 2020, 20, 711–716. [Google Scholar] [CrossRef] [PubMed]
- Leng, Z.; Zhu, R.; Hou, W.; Feng, Y.; Yang, Y.; Han, Q.; Zhao, R.C. Transplantation of ACE2-mesenchymal stem cells improves the outcome of patients with COVID-19 pneumonia. Aging Dis. 2020, 11, 216. [Google Scholar] [CrossRef]
- Golchin, A.; Seyedjafari, E.; Ardeshirylajimi, A. Mesenchymal stem cell therapy for COVID-19: Present or future. Stem Cell Rev. Rep. 2020, 16, 427–433. [Google Scholar] [CrossRef]
- Ji, F.; Li, L.; Li, Z.; Jin, Y.; Liu, W. Mesenchymal stem cells as a potential treatment for critically ill patients with coronavirus disease Stem Cells Transl. Med. 2020, 9, 813–814. [Google Scholar] [CrossRef]
- Zhao, L.; Hu, C.; Zhang, P.; Jiang, H.; Chen, J. Preconditioning strategies for improving the survival rate and paracrine ability of mesenchymal stem cells in acute kidney injury. J. Cell Mol. Med. 2019, 23, 720–730. [Google Scholar] [CrossRef]
- Shu, L.; Niu, C.; Li, R.; Huang, T.; Wang, Y.; Huang, M.; Ji, N.; Zheng, Y.; Chen, X.; Shi, L.; et al. Treatment of severe COVID-19 with human umbilical cord mesenchymal stem cells. Stem Cell Res. Ther. 2020, 11, 361. [Google Scholar] [CrossRef]
- Zhang, K.; Chen, S.; Sun, H.; Wang, L.; Li, H.; Zhao, J.; Zhang, C.; Li, N.; Guo, Z.; Han, Z.; et al. In vivo two-photon microscopy reveals the contribution of Sox9+ cell to kidney regeneration in a mouse model with extracellular vesicle treatment. J. Biol. Chem. 2020, 295, 12203–12213. [Google Scholar] [CrossRef]
- Eirin, A.; Zhu, X.Y.; Puranik, A.S.; Tang, H.; McGurren, K.A.; van Wijnen, A.J.; Lerman, A.; Lerman, L.O. Mesenchymal stem cell-derived extracellular vesicles attenuate kidney inflammation. Kidney Int. 2017, 92, 114–124. [Google Scholar] [CrossRef]
- Vader, P.; Mol, E.A.; Pasterkamp, G.; Schiffelers, R.M. Extracellular vesicles for drug delivery. Adv. Drug Deliv. Rev. 2016, 106, 148–156. [Google Scholar] [CrossRef]
- Gupta, P.S.; Krishnakumar, V.; Sharma, Y.; Dinda, A.K.; Mohanty, S. Mesenchymal stem cell derived exosomes: A nano platform for therapeutics and drug delivery in combating COVID-19. Stem Cell Rev. Rep. 2020, 1, 33–43. [Google Scholar] [CrossRef]
- Baker, S.C. Coronaviruses: From common colds to severe acute respiratory syndrome. Pediatr. Infect. Dis. J. 2004, 23, 1049–1050. [Google Scholar] [CrossRef]
- Sloots, T.P.; Whiley, D.M.; Lambert, S.B.; Nissena, M.D. Emerging respiratory agents: New viruses for old diseases? J. Clin. Virol. 2008, 42, 233–243. [Google Scholar] [CrossRef]
- Khatri, M.; Richardson, L.A.; Meulia, T. Mesenchymal stem cell-derived extracellular vesicles attenuate influenza virus-induced acute lung injury in a pig model. Stem Cell Res. Ther. 2018, 9, 17. [Google Scholar] [CrossRef]
- Du, J.; Li, H.; Lian, J.; Zhu, X.; Qiao, L.; Lin, J. Stem cell therapy: A potential approach for treatment of influenza virus and coronavirus-induced acute lung injury. Stem Cell Res. Ther. 2020, 11, 192. [Google Scholar] [CrossRef]
- Chan, M.C.; Kuok, D.I.; Leung, C.Y.; Hui, K.P.; Valkenburg, S.A.; Lau, E.H.; Peiris, J.M. Human mesenchymal stromal cells reduce influenza A H5N1-associated acute lung injury in vitro and in vivo. Proc. Natl. Acad. Sci. USA 2016, 113, 3621–3626. [Google Scholar] [CrossRef]
- Li, Y.; Xu, J.; Shi, W.; Chen, C.; Shao, Y.; Zhu, L.; Lu, W.; Hanet, X. Mesenchymal stromal cell treatment prevents H9N2 avian influenza virus-induced acute lung injury in mice. Stem Cell Res. Ther. 2016, 7, 159. [Google Scholar] [CrossRef]
- Loy, H.; Kuok, D.I.T.; Hui, K.P.Y.; Choi, M.H.L.; Yuen, W.; Nicholls, J.M.; Peiris, J.S.M.; Chan, M.C.W. Therapeutic implications of human umbilical cord mesenchymal stromal cells in attenuating influenza A (H5N1) virusassociated acute lung injury. J. Infect. Dis. 2019, 219, 186–196. [Google Scholar] [CrossRef]
- Song, N.; Scholtemeijer, M.; Shah, K. Mesenchymal stem cell immunomodulation: Mechanisms and therapeutic potential. Trends Pharmacol. Sci. 2020, 41, 653–664. [Google Scholar] [CrossRef] [PubMed]
- Suzdaltseva, Y.; Goryunov, K.; Silina, E.; Manturova, N.; Stupin, V.; Kiselev, S.L. Equilibrium among inflammatory factors determines human MSC-mediated immunosuppressive effect. Cells 2022, 11, 1210. [Google Scholar] [CrossRef] [PubMed]
- Chen, J.; Hu, C.; Chen, L.; Tang, L.; Zhu, Y.; Xu, X.; Chen, L.; Gao, H.; Lu, X.; Yu, L.; et al. Clinical study of mesenchymal stem cell treatment for acute respiratory distress syndrome induced by epidemic influenza A (H7N9) infection: A hint for COVID-19 treatment. Engineering 2020, 6, 1153–1161. [Google Scholar] [CrossRef] [PubMed]
- Gotts, J.E.; Abbott, J.; Matthay, M.A. Influenza causes prolonged disruption of the alveolar-capillary barrier in mice unresponsive to mesenchymal stem cell therapy. Am. J. Physiol. Lung Cell Mol. Physiol. 2014, 307, L395–L406. [Google Scholar] [CrossRef] [PubMed]
- Darwish, I.; Banner, D.; Mubareka, S.; Kim, H.; Besla, R.; Kelvin, D.J.; Kain, K.C.; Liles, W.C. Mesenchymal stromal (stem) cell therapy fails to improve outcomes in experimental severe influenza. PLoS ONE 2013, 8, e71761. [Google Scholar] [CrossRef]
- Taylor, B.S.; Sobieszczyk, M.E.; McCutchan, F.E.; Hammer, S.M. The challenge of HIV-1 subtype diversity. N. Engl. J. Med. 2008, 358, 1590–1602. [Google Scholar] [CrossRef]
- Cohen, J. Has a second person with HIV been cured? Sci. Mag. 2019, 363, 1021. [Google Scholar] [CrossRef]
- Cohen, J. An intriguing—But far from proven—HIV cure in the ‘São Paulo Patient’. Sci. Mag. 2020. [Google Scholar] [CrossRef]
- Kitchen, S.G.; Zack, J.A. Stem cell-based approaches to treating HIV infection. Curr. Opin. HIV AIDS 2011, 6, 68–73. [Google Scholar] [CrossRef]
- Kandula, U.R.; Wake, A. Promising stem cell therapy in the management of HIV and AIDS: A narrative review. Biol. Targets Ther. 2022, 16, 89–105. [Google Scholar] [CrossRef]
- Khalid, K.; Padda, J.; Fernando, R.W.; Mehta, K.A.; Almanie, A.H.; Hennawi, H.A.; Padda, S.; Cooper, A.C.; Jean-Charles, G. Stem cell therapy and its significance in HIV infection. Cureus 2021, 13, e17507. [Google Scholar] [CrossRef]
- Allers, K.; Hutter, G.; Hofmann, J.; Loddenkemper, C.; Rieger, K.; Thiel, E.; Schneider, T. Evidence for the cure of HIV infection by CCR5Δ32/Δ32 stem cell transplantation. Blood 2011, 117, 2791–2799. [Google Scholar] [CrossRef]
- Fackler, O.T.; Murooka, T.T.; Imle, A.; Mempel, T.R. Adding new dimensions: Towards an integrative understanding of HIV-1 spread. Nat. Rev. Microbiol. 2014, 12, 563–574. [Google Scholar] [CrossRef]
- Weber, M.G.; Walters-Laird, C.J.; Kol, A.; Rocha, C.S.; Hirao, L.A.; Mende, A.; Balan, B.; Arredondo, J.; Elizaldi, S.R.; Iyer, S.S.; et al. Gut germinal center regeneration and enhanced antiviral immunity by mesenchymal stem/stromal cells in SIV infection. JCI Insight 2021, 6, e149033. [Google Scholar] [CrossRef]
- Clinicaltrials.gov. Bone Marrow-Derived Mesenchymal Stem Cell Treatment for Severe Patients with Coronavirus Disease 2019 (COVID-19) ClinicalTrials.gov Identifier: NCT04346368. Available online: https://clinicaltrials.gov/ct2/show/NCT04346368 (accessed on 15 April 2020).
- Clinicaltrials.gov. Treatment of Severe COVID-19 Pneumonia with Allogeneic Mesenchymal Stromal Cells (COVID_MSV) Clinical Trials.gov Identifier: NCT04361942. Available online: https://clinicaltrials.gov/ct2/show/NCT04361942 (accessed on 28 October 2021).
- Clinicaltrials.gov. Mesenchymal Stem Cell Therapy for SARS-CoV-2-Related Acute Respiratory Distress Syndrome. ClinicalTrials.gov Identifier: NCT04366063. Available online: https://clinicaltrials.gov/ct2/show/NCT04366063 (accessed on 28 April 2021).
- Clinicaltrials.gov. Cellular Immuno-Therapy for COVID-19 Acute Respiratory Distress Syndrome—Vanguard (CIRCA-19). ClinicalTrials.gov Identifier: NCT04400032. Available online: https://clinicaltrials.gov/ct2/show/NCT04400032 (accessed on 26 April 2021).
- Clinicaltrials.gov. Mesenchymal Stromal Cells for the Treatment of SARS-CoV-2 Induced Acute Respiratory Failure (COVID-19 Disease). ClinicalTrials.gov Identifier: NCT04345601. Available online: https://clinicaltrials.gov/ct2/show/NCT04345601 (accessed on 26 September 2022).
- Clinicaltrials.gov. A Pilot Clinical Study on Inhalation of Mesenchymal Stem Cells Exosomes Treating Severe Novel Coronavirus Pneumonia. ClinicalTrials.gov Identifier: NCT 04276987. Available online: https://clinicaltrials.gov/ct2/show/NCT04276987 (accessed on 7 September 2020).
- Clinicaltrials.gov. Evaluation of Safety and Efficiency of Method of Exosome Inhalation in SARS-CoV-2 Associated Pneumonia. (COVID-19EXO). ClinicalTrials.gov Identifier: NCT04491240. Available online: https://clinicaltrials.gov/ct2/show/NCT04491240 (accessed on 4 November 2020).
- Clinicaltrials.gov. Mesenchymal Stem Cells (MSCs) in Inflammation-Resolution Programs of Coronavirus Disease 2019 (COVID-19) Induced Acute Respiratory Distress Syndrome (ARDS). ClinicalTrials.gov Identifier: NCT04377334. Available online: https://clinicaltrials.gov/ct2/show/NCT04377334 (accessed on 27 January 2020).
- Clinicaltrials.gov. Safety and Efficacy of Mesenchymal Stem Cells in the Management of Severe COVID-19 Pneumonia (CELMA). ClinicalTrials.gov Identifier: NCT 04429763. Available online: https://clinicaltrials.gov/ct2/show/NCT04429763 (accessed on 12 June 2020).
- Clinicaltrials.gov. Therapy for Pneumonia Patients Infected by 2019 Novel Coronavirus ClinicalTrials.gov Identifier: NCT04293692. Available online: https://clinicaltrials.gov/ct2/show/NCT04293692 (accessed on 18 March 2020).
- Clinicaltrials.gov. Use of UC-MSCs for COVID-19 Patients. ClinicalTrials.gov Identifier: NCT04355728. Available online: https://clinicaltrials.gov/ct2/show/NCT04355728 (accessed on 6 December 2021).
- Clinicaltrials.gov. Study of Human Umbilical Cord Mesenchymal Stem Cells in the Treatment of Severe COVID-19. ClinicalTrials.gov Identifier: NCT04273646. Available online: https://clinicaltrials.gov/ct2/show/NCT04273646 (accessed on 14 April 2020).
- Clinicaltrials.gov. Clinical Research of Human Mesenchymal Stem Cells in the Treatment of COVID-19 Pneumonia. ClinicalTrials.gov Identifier: NCT04339660. Available online: https://clinicaltrials.gov/ct2/show/NCT04339660 (accessed on 9 April 2020).
- Clinicaltrials.gov. Autologous Adipose-Derived Stem Cells (AdMSCs) for COVID-19. ClinicalTrials.gov Identifier: NCT04428801. Available online: https://clinicaltrials.gov/ct2/show/NCT04428801 (accessed on 5 May 2022).
- Clinicaltrials.gov. Battle against COVID-19 Using Mesenchymal Stromal Cells. ClinicalTrials.gov Identifier: NCT 04348461. Available online: https://clinicaltrials.gov/ct2/show/NCT04348461 (accessed on 17 March 2021).
- Clinicaltrials.gov. Clinical Trial to Assess the Safety and Efficacy of Intravenous Administration of Allogeneic Adult Mesenchymal Stem Cells of Expanded Adipose Tissue in Patients with Severe Pneumonia Due to COVID-19. ClinicalTrials. gov Identifier: NCT04366323. Available online: https://clinicaltrials.gov/ct2/show/NCT04366323 (accessed on 6 April 2022).
- Clinicaltrials.gov. ASC Therapy for Patients with Severe Respiratory COVID-19. ClinicalTrials.gov Identifier: NCT 04341610. Available online: https://clinicaltrials.gov/ct2/show/NCT04341610 (accessed on 27 May 2020).
- Clinicaltrials.gov. Zofin (Organicell Flow) for Patients with COVID-19. ClinicalTrials.gov Identifier: NCT04384445. Available online: https://clinicaltrials.gov/ct2/show/NCT04384445 (accessed on 21 September 2022).
- Clinicaltrials.gov. Umbilical Cord Mesenchymal Stem Cells for Immune Reconstitution in HIV-Infected Patients. ClinicalTrials.gov Identifier: NCT01213186. Available online: https://clinicaltrials.gov/ct2/show/NCT01213186 (accessed on 29 May 2013).
- Clinicaltrials.gov. Treatment with MSC in HIV-Infected Patients with Controlled Viremia and Immunological Discordant Response. ClinicalTrials.gov Identifier: NCT02290041. Available online: https://clinicaltrials.gov/ct2/show/NCT02290041 (accessed on 4 May 2020).
- Clinicaltrials.gov. A Tolerance Clinical Study on Aerosol Inhalation of Mesenchymal Stem Cells Exosomes in Healthy Volunteers. ClinicalTrials.gov Identifier: NCT04313647. Available online: https://clinicaltrials.gov/ct2/show/NCT04313647 (accessed on 4 August 2021).
- Clinicaltrials.gov. Using Human Menstrual Blood Cells to Treat Acute Lung Injury Caused by H7N9 Bird Flu Virus Infection. ClinicalTrials.gov Identifier: NCT02095444. Available online: https://clinicaltrials.gov/ct2/show/NCT02095444 (accessed on 24 March 2014).
- Clinicaltrials.gov. Regenerative Medicine for COVID-19 and Flu-Elicited ARDS Using Lomecel-B (RECOVER). ClinicalTrials.gov Identifier: NCT04629105. Available online: https://clinicaltrials.gov/ct2/show/NCT04629105 (accessed on 26 September 2022).
- Eveni, J.; Filipo, K.; Garfin, A.M.C.; Geocaniga-Gaviola, D.M.; Huot, C.; Iavro, E.; Ismail, K.; Itogo, N.; Kako, H.; Kal, M.; et al. Global Tuberculosis Report 2021; World Health Organization: Geneva, Switzerland, 2021; pp. 1–57. [Google Scholar]
- Can Sarinoglu, R.; Sili, U.; Eryuksel, E.; Olgun Yildizeli, S.; Cimsit, C.; Karahasan Yagci, A. Tuberculosis and COVID-19: An overlapping situation during pandemic. J. Infect. Dev. Ctries 2020, 14, 721–725. [Google Scholar] [CrossRef]
- Lange, C.; Dheda, K.; Chesov, D.; Mandalakas, A.M.; Udwadia, Z.; Horsburgh, C.R.J. Management of drug-resistant tuberculosis. Lancet 2019, 394, 953–966. [Google Scholar] [CrossRef]
- Cohen, S.B.; Gern, B.H.; Delahaye, J.L.; Adams, K.N.; Plumlee, C.R.; Winkler, J.K.; Sherman, D.R.; Gerner, M.Y.; Urdahl, K.B. Alveolar macrophages provide an early mycobacterium tuberculosis niche and initiate dissemination. Cell Host Microbe 2018, 24, 439–446.e4. [Google Scholar] [CrossRef]
- Orme, I.M.; Basaraba, R.J. The Formation of the granuloma in tuberculosis infection. Semin. Immunol. 2014, 26, 601–609. [Google Scholar] [CrossRef]
- Sandor, M.; Weinstock, J.V.; Wynn, T.A. Granulomas in Schistosome and Mycobacterial Infections: A Model of Local Immune Responses. Trends Immunol. 2003, 24, 44–52. [Google Scholar] [CrossRef]
- Raghuvanshi, S.; Sharma, P.; Singh, S.; Van Kaer, L.; Das, G. Mycobacterium tuberculosis evades host immunity by recruiting mesenchymal stem cells. Proc. Natl. Acad. Sci. USA 2010, 107, 21653–21658. [Google Scholar] [CrossRef]
- Schwartz, Y.S.; Belogorodtsev, S.N.; Filimonov, P.N.; Cherednichenko, A.G.; Pustylnikov, S.V.; Krasnov, V.A. BCG infection in mice is promoted by naive mesenchymal stromal cells (MSC) and suppressed by Poly(A:U)-conditioned MSC. Tuberculosis 2016, 101, 130–136. [Google Scholar] [CrossRef] [PubMed]
- Khan, A.; Mann, L.; Papanna, R.; Lyu, M.A.; Singh, C.R.; Olson, S. Mesenchymal stem cells internalize mycobacterium tuberculosis through scavenger receptors and restrict bacterial growth through autophagy. Sci. Rep. 2017, 7, 15010. [Google Scholar] [CrossRef] [PubMed]
- Alquraini, A.; Khoury, J.E. Scavenger receptors. Curr. Biol. 2020, 30, R790–R795. [Google Scholar] [CrossRef] [PubMed]
- Jain, N.; Kalam, H.; Singh, L.; Sharma, V.; Kedia, S.; Das, P.; Ahuja, V.; Kumar, D. Mesenchymal stem cells offer a drug-tolerant and immune-privileged niche to mycobacterium tuberculosis. Nat. Commun. 2020, 11, 3062. [Google Scholar] [CrossRef] [PubMed]
- Singh, V.K.; Mishra, A.; Bark, S.; Mani, A.; Subbian, S.; Hunter, R.L.; Jagannath, C.; Khan, A. Human mesenchymal stem cell based intracellular dormancy model of mycobacterium tuberculosis. Microbes Infect. 2020, 22, 423–431. [Google Scholar] [CrossRef]
- Shamputa, I.C.; Van Deun, A.; Salim, M.A.; Hossain, M.A.; Fissette, K.; de Rijk, P.; Rigouts, L.; Portaels, F. Endogenous reactivation and true treatment failure as causes of recurrent tuberculosis in a high incidence setting with a low HIV infection. Trop. Med. Int. Health 2007, 12, 700–708. [Google Scholar] [CrossRef]
- Tsenova, L.; Singhal, A. Effects of host-directed therapies on the pathology of tuberculosis. J. Pathol. 2020, 250, 636–646. [Google Scholar] [CrossRef]
- Yudintceva, N.M.; Bogolyubova, I.O.; Muraviov, A.N.; Sheykhov, M.G.; Vinogradova, T.I.; Sokolovich, E.G.; Samusenko, I.A.; Shevtsov, M.A. Application of the allogenic mesenchymal stem cells in the therapy of the bladder tuberculosis. J. Tissue Eng. Regen. Med. 2018, 12, e1580–e1593. [Google Scholar] [CrossRef]
- Harman, R.M.; Yang, S.; He, M.K.; Van de Walle, G.R. Antimicrobial peptides secreted by equine mesenchymal stromal cells inhibit the growth of bacteria commonly found in skin wounds. Stem Cell Res. Ther. 2017, 8, 157. [Google Scholar] [CrossRef]
- Chow, L.; Johnson, V.; Impastato, R.; Coy, J.; Strumpf, A.; Dow, S. Antibacterial activity of human mesenchymal stem cells mediated directly by constitutively secreted factors and indirectly by activation of innate immune effector cells. Stem Cells Transl. Med. 2020, 9, 235–249. [Google Scholar] [CrossRef]
- Sutton, M.T.; Fletcher, D.; Ghosh, S.K.; Weinberg, A.; van Heeckeren, R.; Kaur, S.; Sadeghi, Z.; Hijaz, A.; Reese, J.; Lazarus, H.M.; et al. Antimicrobial properties of mesenchymal stem cells: Therapeutic potential for cystic fibrosis infection, and treatment. Stem Cells Int. 2016, 2016, 5303048. [Google Scholar] [CrossRef]
- Colombo, M.; Raposo, G.; Thery, C. Biogenesis, secretion, and intercellular interactions of exosomes and other extracellular vesicles. Ann. Rev. Cell Dev. Biol. 2014, 30, 255–289. [Google Scholar] [CrossRef]
- Favaro, E.; Carpanetto, A.; Lamorte, S.; Fusco, A.; Caorsi, C.; Deregibus, M.C.; Bruno, S.; Amoroso, A.; Giovarelli, M.; Port, M.; et al. Human Mesenchymal Stem Cell-Derived Microvesicles Modulate T Cell Response to Islet Antigen Glutamic Acid Decarboxylase in Patients With Type 1 Diabetes. Diabetologia 2014, 57, 1664–1673. [Google Scholar] [CrossRef]
- Li, P.; Zhao, Y.; Ge, L. Therapeutic Effects of Human Gingiva-Derived Mesenchymal Stromal Cells on Murine Contact Hypersensitivity via Prostaglandin E2-EP3 Signaling. Stem Cell Res. Ther. 2016, 7, 103. [Google Scholar] [CrossRef]
- Huang, F.; Chen, M.; Chen, W.; Gu, J.; Yuan, J.; Xue, Y.; Dang, J.; Su, W.; Wang, J.; Zadeh, H.H.; et al. Human Gingiva-Derived Mesenchymal Stem Cells Inhibit Xeno-Graft-Versus-Host Disease via CD39-CD73-Adenosine and IDO Signals. Front. Immunol. 2017, 8, 68. [Google Scholar] [CrossRef]
- Zhang, X.; Huang, F.; Li, W.; Dang, J.L.; Yuan, J.; Wang, J.; Zeng, D.-L.; Sun, C.-X.; Liu, Y.-Y.; Ao, Q.; et al. Human Gingiva-Derived Mesenchymal Stem Cells Modulate Monocytes/Macrophages and Alleviate Atherosclerosis. Front. Immunol. 2018, 9, 878. [Google Scholar] [CrossRef]
- Ren, W.; Hou, J.; Yang, C.; Wang, H.; Wu, S.; Wu, Y.; Zhao, X.; Lu, C. Extracellular Vesicles Secreted by Hypoxia Pre-Challenged Mesenchymal Stem Cells Promote non-Small Cell Lung Cancer Cell Growth and Mobility as Well as Macrophage M2 Polarization via miR-21-5p Delivery. J. Exp. Clin. Cancer Res. 2019, 38, 62. [Google Scholar] [CrossRef]
- Peng, Y.; Chen, X.; Liu, Q.; Zhang, X.; Huang, K.; Liu, L.; Li, H.; Zhou, M.; Huang, F.; Fan, Z.; et al. Mesenchymal Stromal Cells Infusions Improve Refractory Chronic Graft Versus Host Disease Through an Increase of CD5+ Regulatory B Cells Producing Interleukin 10. Leukemia 2015, 29, 636–646. [Google Scholar] [CrossRef]
- Budoni, M.; Fierabracci, A.; Luciano, R.; Petrini, S.; Di Ciommo, V.; Muraca, M. The Immunosuppressive Effect of Mesenchymal Stromal Cells on B Lymphocytes is Mediated by Membrane Vesicles. Cell Transplant. 2013, 22, 369–379. [Google Scholar] [CrossRef]
- Bernard, O.; Jeny, F.; Uzunhan, Y.; Dondi, E.; Terfous, R.; Label, R.; Sutton, A.; Larghero, J.; Vanneaux, V.; Nunes, H.; et al. Mesenchymal Stem Cells Reduce Hypoxia-Induced Apoptosis in Alveolar Epithelial Cells by Modulating HIF and ROS Hypoxic Signaling. Am. J. Physiol. Lung Cell Mol. Physiol. 2018, 314, L360–L371. [Google Scholar] [CrossRef]
- Yudintceva, N.; Mikhailova, N.; Bobkov, D.; Yakovleva, L.; Nikolaev, B.; Krasavina, D.; Muraviov, A.; Vinogradova, T.; Yablonskiy, P.; Samusenko, I.; et al. Evaluation of the biodistribution of mesenchymal stem cells in a pre-clinical renal tuberculosis model by non-linear magnetic response measurements. Front. Phys. 2021, 9, 198. [Google Scholar] [CrossRef]
- Chen, S.; Cui, G.; Peng, C.; Lavin, M.F.; Sun, X.; Zhang, E. Transplantation of Adipose-Derived Mesenchymal Stem Cells Attenuates Pulmonary Fibrosis of Silicosis via Anti-Inflammatory and Anti-Apoptosis Effects in Rats. Stem Cell Res. Ther. 2018, 9, 110. [Google Scholar] [CrossRef] [PubMed]
- Zhu, Y.G.; Feng, X.M.; Abbott, J.; Fang, X.H.; Hao, Q.; Monsel, A.; Qu, J.; Matthay, M.A.; Lee, J.W. Human Mesenchymal Stem Cell Microvesicles for Treatment of Escherichia Coli Endotoxin-Induced Acute Lung Injury in Mice. Stem Cells 2014, 3, 116–125. [Google Scholar] [CrossRef] [PubMed]
- Li, X.; Wang, Y.; An, G.; Liang, D.; Zhu, Z.; Lian, X.; Niu, P.; Guo, C.; Tian, L. Bone Marrow Mesenchymal Stem Cells Attenuate Silica-Induced Pulmonary Fibrosis via Paracrine Mechanisms. Toxicol. Lett. 2017, 270, 96–107. [Google Scholar] [CrossRef] [PubMed]
- Poggi, A.; Zocchi, M.R. Immunomodulatory properties of mesenchymal stromal cells: Still unresolved “Yin and Yang”. Curr. Stem Cell Res. Ther. 2019, 14, 344–350. [Google Scholar] [CrossRef]
- Sack, D.A.; Sack, R.B.; Chaignat, C.L. Getting serious about cholera. N. Engl. J. Med. 2006, 355, 649–651. [Google Scholar] [CrossRef]
- Bishop, A.L.; Camilli, A. Vibrio cholerae: Lessons for mucosal vaccine design. Expert Rev. Vaccines 2011, 10, 79–94. [Google Scholar] [CrossRef]
- Bhattacharya, D.; Dey, S.; Roy, S.; Parande, M.V.; Telsang, M.; Seema, M.H.; Parande, A.V.; Mantur, B.G. Multidrug-resistant Vibrio cholerae O1 was responsible for a cholera outbreak in 2013 in Bagalkot, North Karnataka. Jpn. J. Infect. Dis. 2015, 68, 347–350. [Google Scholar] [CrossRef]
- Bhattacharya, D.; Sayi, D.S.; Thamizhmani, R.; Bhattacharjee, H.; Bharadwaj, A.P.; Roy, A.; Sugunan, A.P. Emergence of multidrug-resistant Vibrio cholerae O1 biotype El Tor in Port Blair, India. Am. J. Trop. Med. Hyg. 2012, 86, 1015–1017. [Google Scholar] [CrossRef]
- Chatterjee, S.N.; Chaudhuri, K. Lipopolysaccharides of Vibrio cholerae: III. Biological functions. Biochim. Biophys. Acta 2006, 1762, 1–16. [Google Scholar] [CrossRef]
- Saeedi, P.; Halabian, R.; Fooladi, A.I. Antimicrobial effects of mesenchymal stem cells primed by modified LPS on bacterial clearance in sepsis. J. Cell Physiol. 2019, 234, 4970–4986. [Google Scholar] [CrossRef]
- Moulazadeh, A.; Soudi, S.; Bakhshi, B. Immunomodulatory effects of adipose-derived mesenchymal stem cells on epithelial cells function in response to Vibrio cholera in a co-culture model. Iran. J. Allergy Asthma Immunol. 2021, 20, 550–562. [Google Scholar] [CrossRef]
- Clinicaltrials.gov. Effectivity of Local Implantation of the Mesenchymal Stem Cell on Vertebral Bone Defect Due to Mycobaterium Tuberculosis Infection (Clinical Trial) Clinicaltrials.gov, Identifier: NCT04493918. Available online: https://clinicaltrials.gov/ct2/show/NCT04493918 (accessed on 3 August 2020).
- Erokhin, V.V.; Vasil’eva, I.A.; Konopliannikov, A.G.; Chukanov, V.I.; Tsyb, A.F.; Bagdasarian, T.R.; Danilenko, A.A.; Lepekhina, L.A.; Kal’sina, S.S.; Semenkova, I.V.; et al. Systemic transplantation of autologous mesenchymal stem cells of the bone marrow in the treatment of patients with multidrug-resistant pulmonary tuberculosis. Probl. Tuberk. Bolezn. Legk. 2008, 10, 3–6. [Google Scholar]
- Skrahin, A.; Ahmed, R.K.; Ferrara, G.; Rane, L.; Poiret, T.; Isaikina, Y.; Skrahina, A.; Zumla, A.; Maeurer, M.J. Autologous mesenchymal stromal cell infusion as adjunct treatment in patients with multidrug and extensively drug-resistant tuberculosis: An open-label Phase 1 Safety Trial. Lancet Respir. Med. 2014, 2, 108–122. [Google Scholar] [CrossRef]
- Skrahin, A.; Jenkins, H.E.; Hurevich, H.; Solodovnikova, V.; Isaikina, Y.; Klimuk, D.; Rohava, Z.; Skrahina, A. Effectiveness of a Novel Cellular Therapy to Treat Multidrug-Resistant Tuberculosis. Int. J. Mycobacteriol. 2016, 5, 23. [Google Scholar] [CrossRef]
| Source | Abbreviation | Proliferation Rate | Doubling Time | Immunogenicity | MSCs Phenotype | References | |
|---|---|---|---|---|---|---|---|
| 1 | Bone Marrow | BM-MSCs | Lowest | 40 h | Medium | Stro-1, CD271, SSEA-4, CD146 | [30,31,32,33,34,35,36] |
| 2 | Adipose Tissue | A-MSCs | Higher | 5 days | High | CD271, CD146 | [33,34,35,36] |
| 3 | Umbilical Cord | UC-MSCs | Medium | 30 h | High | CD146 | [35,36,37,38] |
| 4 | Placenta | P-MSCs | High | 36 h | High | c-Kit, Oct-4, SSEA-4, Y-box 2 | [39,40] |
| Abbreviation | Immune Cell | Mechanism | Effect | Reference | |
|---|---|---|---|---|---|
| 1 | BM-MSC-EVs | CD4 + T cell | EVs-encapsulating miR-23a-3p and post-transcriptionally regulated TGF-beta receptor 2 in T cells | suppressive Th1 differentiation | [70] |
| 2 | BM-MSC-EVs | T cell | increasing IL-10 and TGF-beta | promote T cells apoptosis and inhibit proliferation | [71] |
| 3 | UC-MSCs | T cell | through the COX2/PGE2/NF-kB signaling pathway | inhibiting T cell proliferation and DC differentiation | [72] |
| 4 | AD-MSC | T cell | through regulating TGF-beta and PGE2 | regulate the Th17/Treg balance | [73] |
| 5 | BM-MSC | B cell | inhibition of BAFF production | suppress the excessive activation of B-cells | [74] |
| 6 | BM-MSC-EVs | B cell | targeting PI3K/AKT signaling pathway | inhibit activation of B cell | [75] |
| 7 | BM-MSC | B cell | increased expression of CCL2 by CCL2-MST1-mTOR-STAT1 mediated metabolic signaling pathway | prevent inhibition differentiation, proliferation, and antibody secretion of B-cell | [76] |
| 8 | BM-MSC-EVs | DCs | expression of anti-inflammatory factors (TGF-beta 1 and IL-10) and reduce the generation of proinflammatory cytokines (L-6 and IL-12p70) | attenuate DCs maturation and function | [77] |
| 9 | G-MSC | NK cell | regulating IDO and PGE2 | inhibit the activity of NK cells | [78] |
| 10 | BM-MSCs | NK cell | inhibit IL-12 and IL-21 | suppression NK cell proliferation but increase IFN-gamma and IFN-alpha production | [79] |
| 11 | UC-MSC | macrophage | regulating macrophage metabolic pathways | affect M1/M2 balance | [80] |
| 12 | BM-MSC-EVs | macrophage | down-regulating IL-23 and IL-22 | enhances the anti-inflammatory phenotype of macrophages, promoting inflammation remission | [81] |
| 13 | AD-MSCs | macrophage | down-regulating IL-23 and IL-22 | toward M2 phenotype polarization | [82] |
| 14 | BM-MSC-EVs | macrophage | through miR-223/pKNOX1 pathway | promoting macrophages differentiation toward M2 | [83] |
| 15 | BM-MSC-EVs | macrophage | through TLR4/NF-kB/PI3K/Akt signaling cascade | toward M2 phenotype polarization | [84] |
| 16 | UC-MSC-EVs | macrophage | increased the proportion of M2 macrophage polarization | attenuate DAH induced inflammatory responses and alveolar hemorrhage | [85] |
| Study Title | Abbreviation | Viral Infectious Diseases | Status | Country | Description | Reference | |
|---|---|---|---|---|---|---|---|
| 1 | Bone Marrow-Derived Mesenchymal Stem Cell Treatment for Severe Patients With Coronavirus Disease 2019 (COVID-19) | BM-MSCs | COVID-19 | Phase 2 | China | Conventional treatment plus BM-MSCs (1 × 106 cells/kg body weight intravenously | [195] |
| 2 | Treatment of Severe COVID-19 Pneumonia with Allogeneic Mesenchymal Stromal Cells (COVID_MSV) | BM-MSCs | COVID-19 | Phase 2 | Spain | IV injection of 1 × 106 cells/kg diluted in 100 mL saline | [196] |
| 3 | Mesenchymal Stem Cell Therapy for SARS-CoV-2-related Acute Respiratory Distress Syndrome | BM-MSCs/ BM-MSC-EVs | COVID-19 | Phase 3 | Iran | Two doses of MSCs 1 × 108 at Day 0 and Day 2 plus conventional treatment | [197] |
| 4 | Cellular Immuno-Therapy for COVID-19 Acute Respiratory Distress Syndrome—Vanguard (CIRCA-19) | BM-MSCs | COVID-19 | Phase 1 | Canada | IV administration | [198] |
| 5 | Mesenchymal Stromal Cells for the Treatment of SARS-CoV-2 Induced Acute Respiratory Failure (COVID-19 Disease) | BM-MSCs | COVID-19 | Early Phase 1 | USA | 1 × 108 cells/kg body weight intravenously | [199] |
| 6 | A Pilot Clinical Study on Inhalation of Mesenchymal Stem Cells Exosomes Treating Severe Novel Coronavirus Pneumonia | BM-MSC-EVs | COVID-19 | Phase 1 | China | 5 times aerosol inhalation of MSC-EVs (2 × 108/3 mL at Day 1, Day 2, Day 3, Day 4, Day 5) | [200] |
| 7 | Evaluation of Safety and Efficiency of Method of Exosome Inhalation in SARS-CoV-2 Associated Pneumonia. (COVID-19EXO) | BM-MSC-EVs | COVID-19 | Phase 1 Phase 2 | Russia | Twice a day during 10 days inhalation of 3 mL special solution contained 0.5–2 × 1010 of EVs. | [201] |
| 8 | Mesenchymal Stem Cells (MSCs) in Inflammation-Resolution Programs of Coronavirus Disease 2019 (COVID-19) Induced Acute Respiratory Distress Syndrome (ARDS) | BM-MSCs | COVID-19 | Phase 2 | Germany | Infusion of allogeneic bone marrow-derived human mesenchymal stem (stromal) cells | [202] |
| 9 | Safety and Efficacy of Mesenchymal Stem Cells in the Management of Severe COVID-19 Pneumonia (CELMA) | UC-MSCs | COVID-19 | Phase 2 | USA | 1 × 106 cells/kg body weight intravenously | [203] |
| 10 | Therapy for Pneumonia Patients Infected by 2019 Novel Coronavirus | UC-MSCs | COVID-19 | With- drawn | China | 0.5 × 106/kg body weight suspended in 100 mL saline intravenously at Day 1, Day 3, Day 5, Day 7 | [204] |
| 11 | Use of UC-MSCs for COVID-19 Patients | UC-MSCs | COVID-19 | Phase 2 | USA | Conventional treatment plus UC-MSCs (1 × 108/kg body weight intravenously | [205] |
| 12 | Study of Human Umbilical Cord Mesenchymal Stem Cells in the Treatment of Severe COVID-19 | UC-MSCs | COVID-19 | Not yet recruiting | China | 4 times of UC-MSCs (0.5 × 106 UC-MSCs cell/kg body weight intravenously at Day 1, Day 3, Day 5, Day 7) | [206] |
| 13 | Clinical Research of Human Mesenchymal Stem Cells in the Treatment of COVID-19 Pneumonia | UC-MSCs | COVID-19 | Phase 2 | China | 1 × 106 UC-MSCs/kg suspended in 100 mL saline | [207] |
| 14 | Autologous Adipose-derived Stem Cells (AdMSCs) for COVID-19 | A-MSCs | COVID-19 | Phase 2 | USA | 3 doses of 2 × 106 cells through IV every 3 days | [208] |
| 15 | Battle Against COVID-19 Using Mesenchymal Stromal Cells | A-MSCs | COVID-19 | Phase 2 | Spain | Two serial doses of 1.5 × 106 cells/kg | [209] |
| 16 | Clinical Trial to Assess the Safety and Efficacy of Intravenous Administration of Allogeneic Adult Mesenchymal Stem Cells of Expanded Adipose Tissue in Patients With Severe Pneumonia Due to COVID-19 | A-MSCs | COVID-19 | Phase 2 | Spain | Two doses of 8 × 106 A-MSCs | [210] |
| 17 | ASC Therapy for Patients with Severe Respiratory COVID-19 | A-MSCs | COVID-19 | Phase 2 | Denmark | 1 × 108 cells/kg diluted in 100 mL saline | [211] |
| 18 | Zofin (Organicell Flow) for Patients With COVID-19 | MSC-EVs | COVID-19 | Phase 1 | USA | Zofin with 1ml, containing 2–5 × 1011 EVs/mL in addition to the Standard care. | [212] |
| 19 | Umbilical Cord Mesenchymal Stem Cells for Immune Reconstitution in HIV-infected Patients | UC-MSCs | HIV/AIDS | Phase 2 | China | High and low doses of MSCs (at 0, 4, 12, 24, 36 and 48 week since the onset of treatment) | [213] |
| 20 | Treatment with MSC in HIV-infected Patients with Controlled Viremia and Immunological Discordant Response | A-MSCs | HIV/AIDS | Phase 1 Phase 2 | Spain | Intravenous infusion of 4 doses of A-MSCs (1 × 106 cells/kg, weeks 0-4-8-20). | [214] |
| 21 | A Tolerance Clinical Study on Aerosol Inhalation of Mesenchymal Stem Cells Exosomes In Healthy Volunteers | MSC-EVs | Healthy Volunteers | Phase 1 | China | Aerosol inhalation of MSC-EVs | [215] |
| 22 | Using Human Menstrual Blood Cells to Treat Acute Lung Injury Caused by H7N9 Bird Flu Virus Infection | MSCs | H7N9 Bird Flu Virus Infection | Phase 1 Phase 2 | China | 1~10 × 107 cells/kg infusion frequency: 2 times a week, 2 weeks for infusion | [216] |
| 23 | Regenerative Medicine for COVID-19 and Flu-Elicited ARDS Using Lomecel-B (RECOVER) | MSCs | ARDS COVID-19 | Phase 1 | USA | 1 × 108 cells/kg on Day 0 | [217] |
| Study Title | Abbreviation | Bacterial Diseases | Status | Country | Description | Reference | |
|---|---|---|---|---|---|---|---|
| 1 | Effectivity of Local Implantation of the Mesenchymal Stem Cell on Vertebral Bone Defect Due to Mycobaterium Tuberculosis Infection (Clinical Trial) | MSCs | Extrapulmonary tuberculosis | Phase 2 | Indonesia | 3 × 107 cells/kg diluted in 2 mL 0.9% NaCl intravenously | [257] |
| 2 | Systemic Transplantation of Autologous Mesenchymal Stem Cells of the Bone Marrow in the Treatment of Patients With Multidrug-Resistant Pulmonary Tuberculosis | MSCs | Tuberculosis; multidrug resistant, extensive drug resistant | Completed | Russia | Not stated | [258] |
| 3 | Autologous Mesenchymal Stromal Cell Infusion as Adjunct Treatment in Patients With Multidrug and Extensively Drug-Resistant Tuberculosis: An Open-Label Phase 1 Safety Trial. | BM-MSCs | Tuberculosis; multidrug resistant, extensive drug resistant | Phase 1 | Belarus | 1 × 107 cells/kg diluted in saline | [259] |
| 4 | Effectiveness of a Novel Cellular Therapy to Treat Multidrug-Resistant Tuberculosis. | BM-MSCs | Tuberculosis; multidrug resistant, extensive drug resistant | Phase 1 | Belarus | 1 × 107 cells/kg diluted in saline | [260] |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yudintceva, N.; Mikhailova, N.; Fedorov, V.; Samochernych, K.; Vinogradova, T.; Muraviov, A.; Shevtsov, M. Mesenchymal Stem Cells and MSCs-Derived Extracellular Vesicles in Infectious Diseases: From Basic Research to Clinical Practice. Bioengineering 2022, 9, 662. https://doi.org/10.3390/bioengineering9110662
Yudintceva N, Mikhailova N, Fedorov V, Samochernych K, Vinogradova T, Muraviov A, Shevtsov M. Mesenchymal Stem Cells and MSCs-Derived Extracellular Vesicles in Infectious Diseases: From Basic Research to Clinical Practice. Bioengineering. 2022; 9(11):662. https://doi.org/10.3390/bioengineering9110662
Chicago/Turabian StyleYudintceva, Natalia, Natalia Mikhailova, Viacheslav Fedorov, Konstantin Samochernych, Tatiana Vinogradova, Alexandr Muraviov, and Maxim Shevtsov. 2022. "Mesenchymal Stem Cells and MSCs-Derived Extracellular Vesicles in Infectious Diseases: From Basic Research to Clinical Practice" Bioengineering 9, no. 11: 662. https://doi.org/10.3390/bioengineering9110662
APA StyleYudintceva, N., Mikhailova, N., Fedorov, V., Samochernych, K., Vinogradova, T., Muraviov, A., & Shevtsov, M. (2022). Mesenchymal Stem Cells and MSCs-Derived Extracellular Vesicles in Infectious Diseases: From Basic Research to Clinical Practice. Bioengineering, 9(11), 662. https://doi.org/10.3390/bioengineering9110662







