Distensibility of Deformable Aortic Replicas Assessed by an Integrated In-Vitro and In-Silico Approach †
Abstract
:1. Introduction
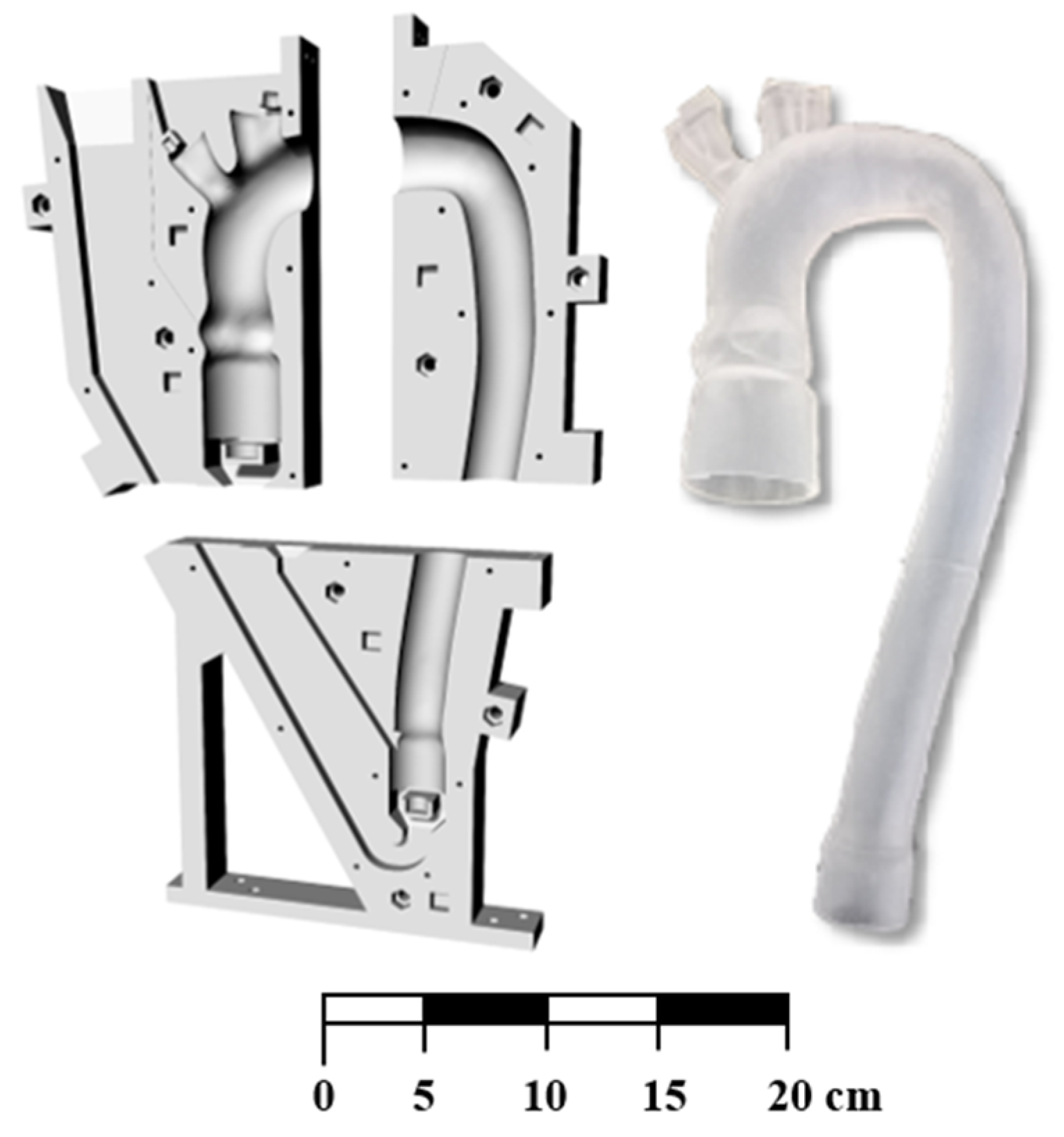
2. Materials and Methods
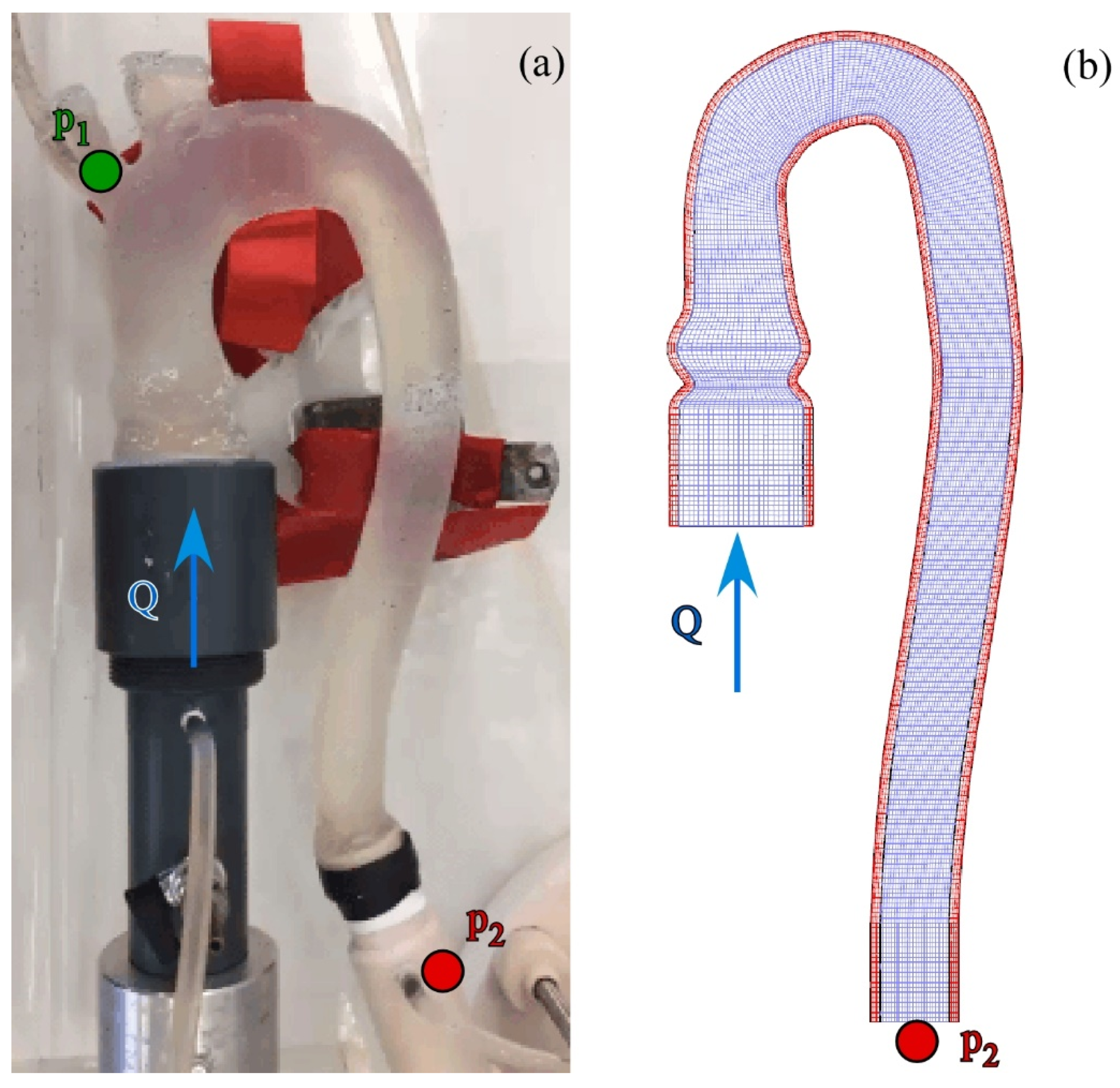
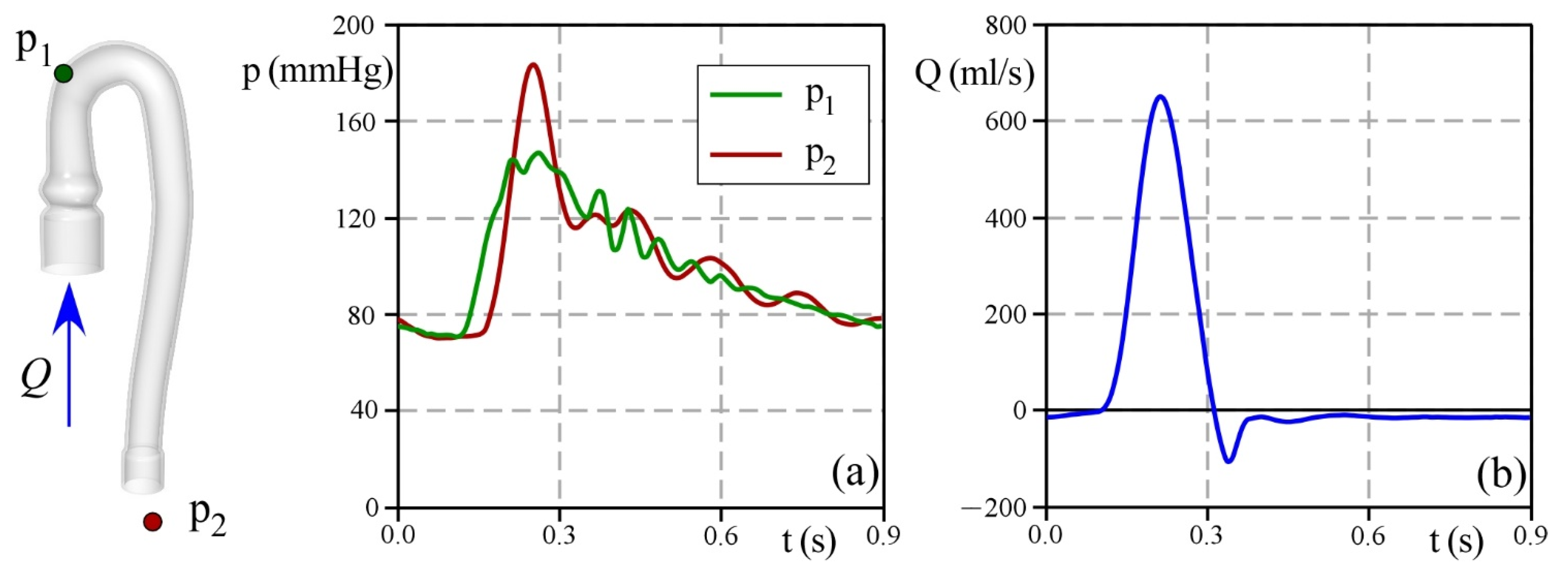
2.1. Experimental Set-Up
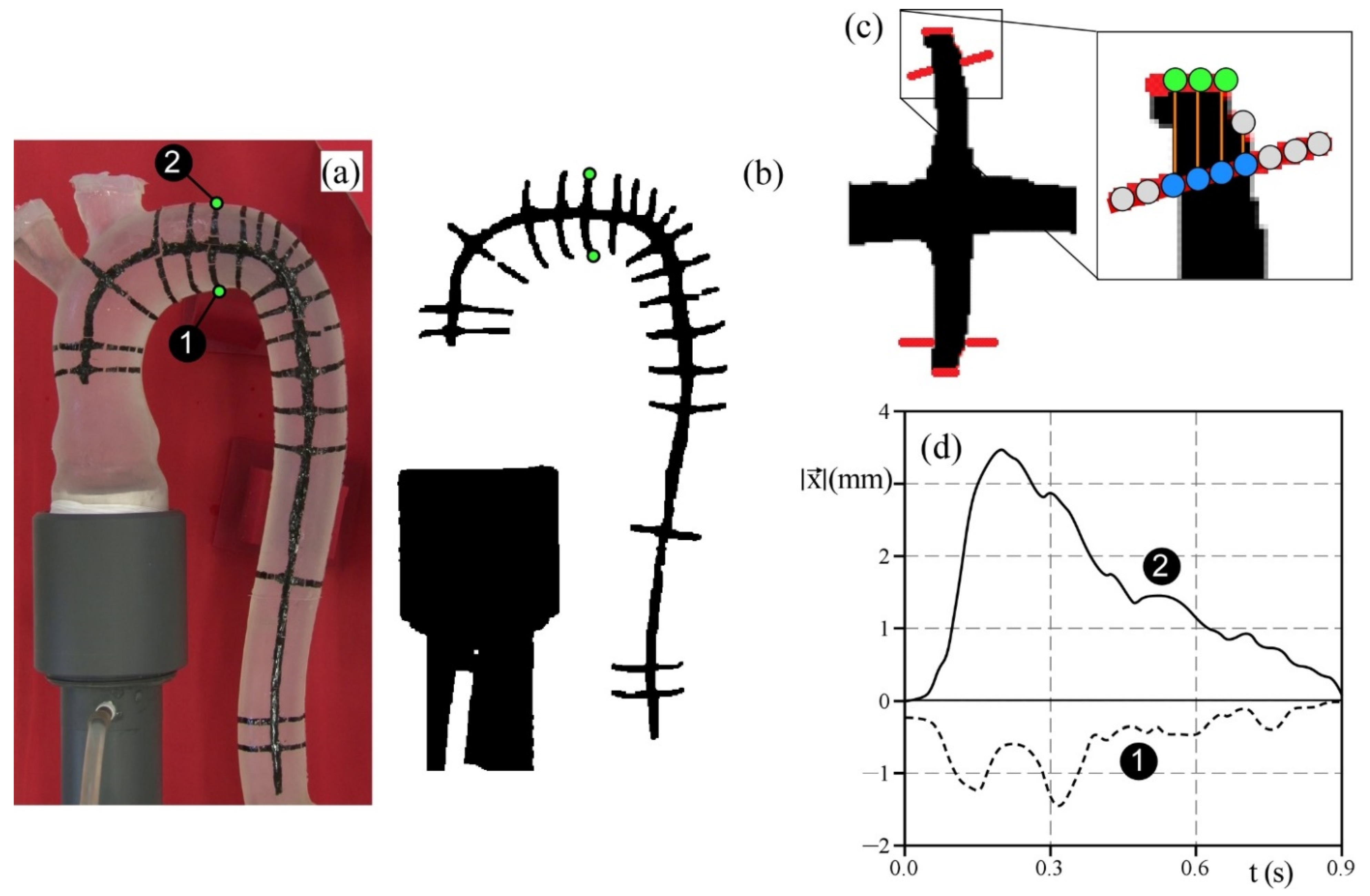
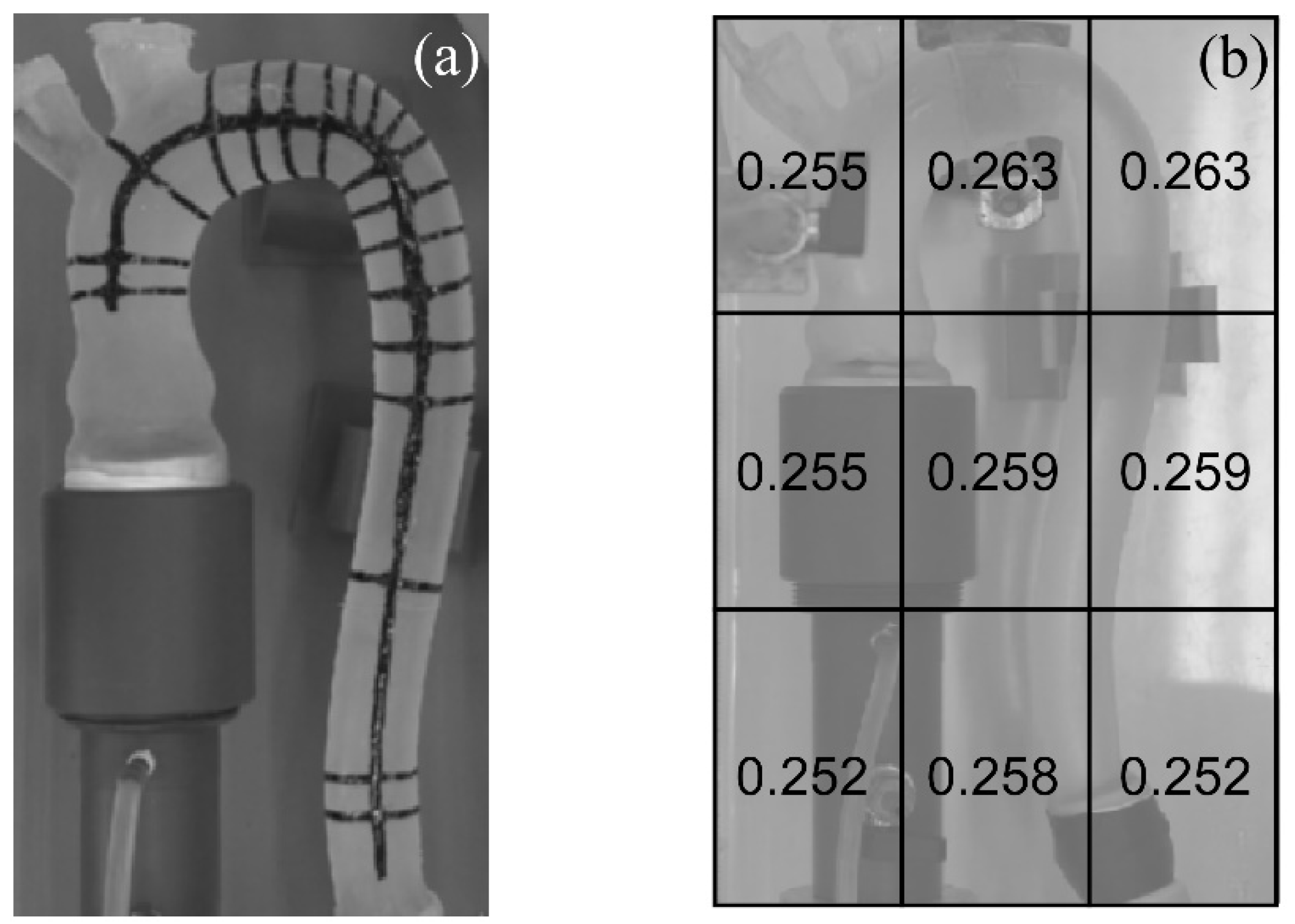
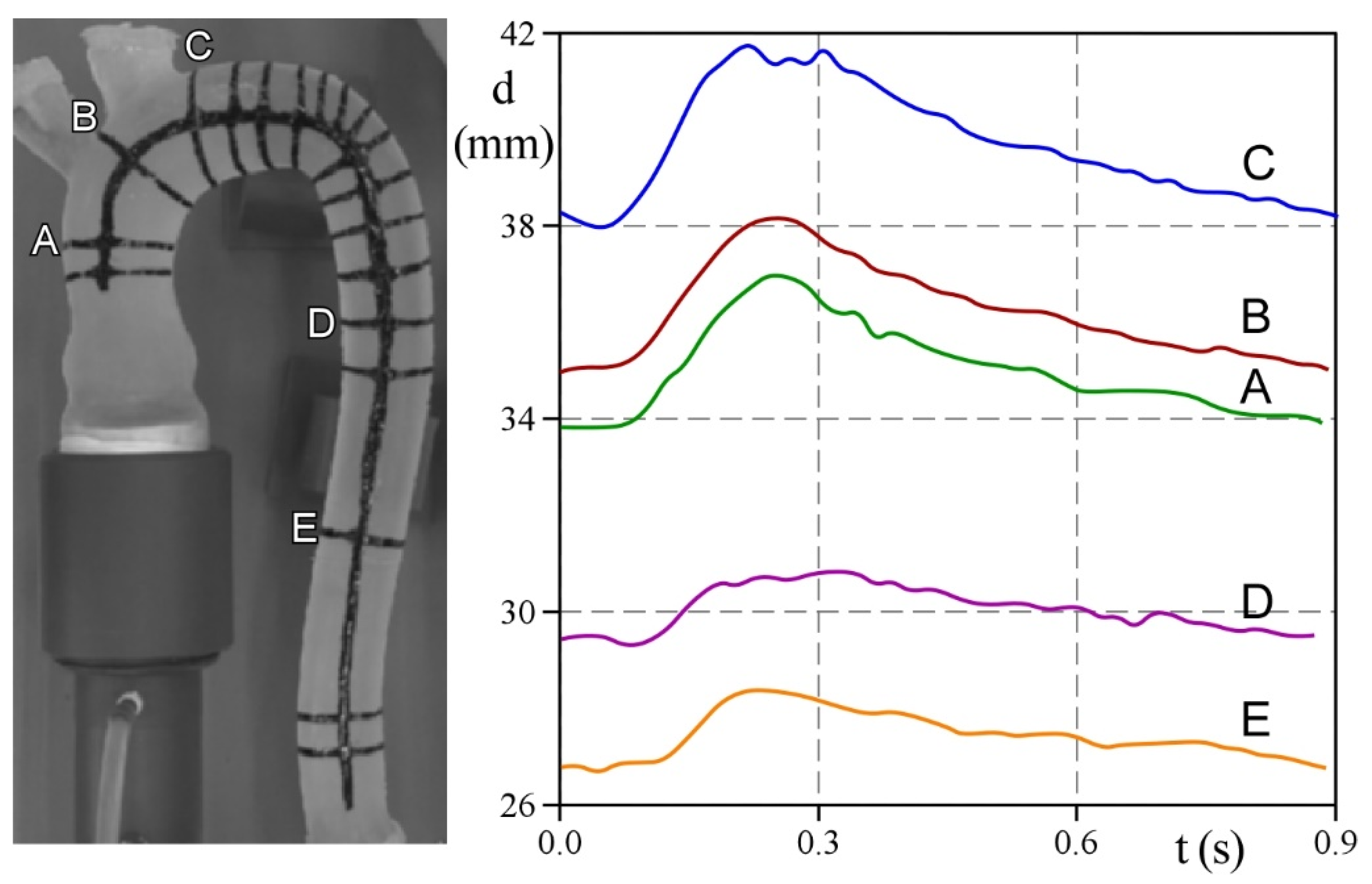
2.2. The Hydrodynamic Test and Deformation Measurements
2.3. The Numerical Analysis
3. Results and Discussion
3.1. In-Vitro Measurements
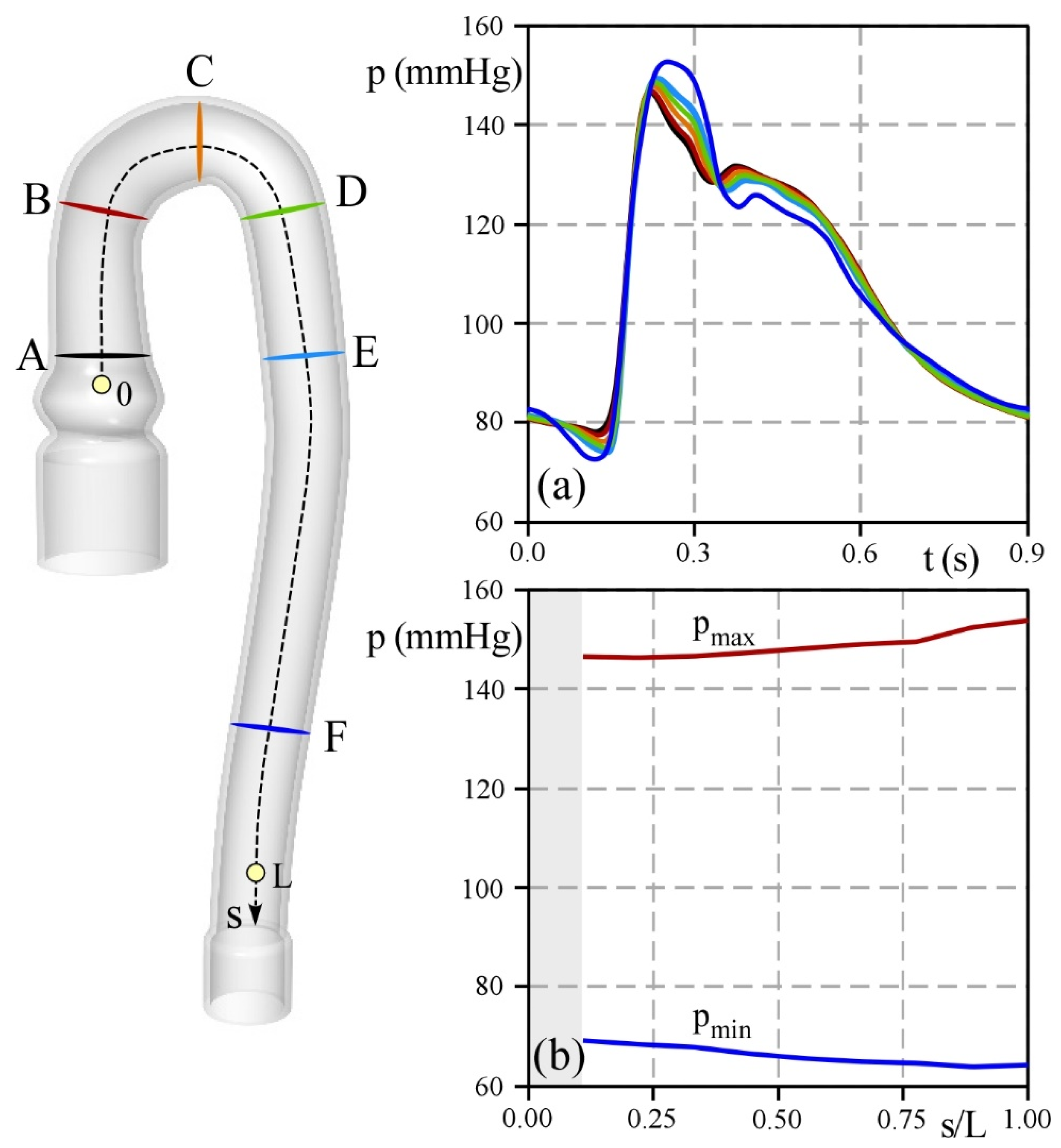
3.2. Numerical Outputs
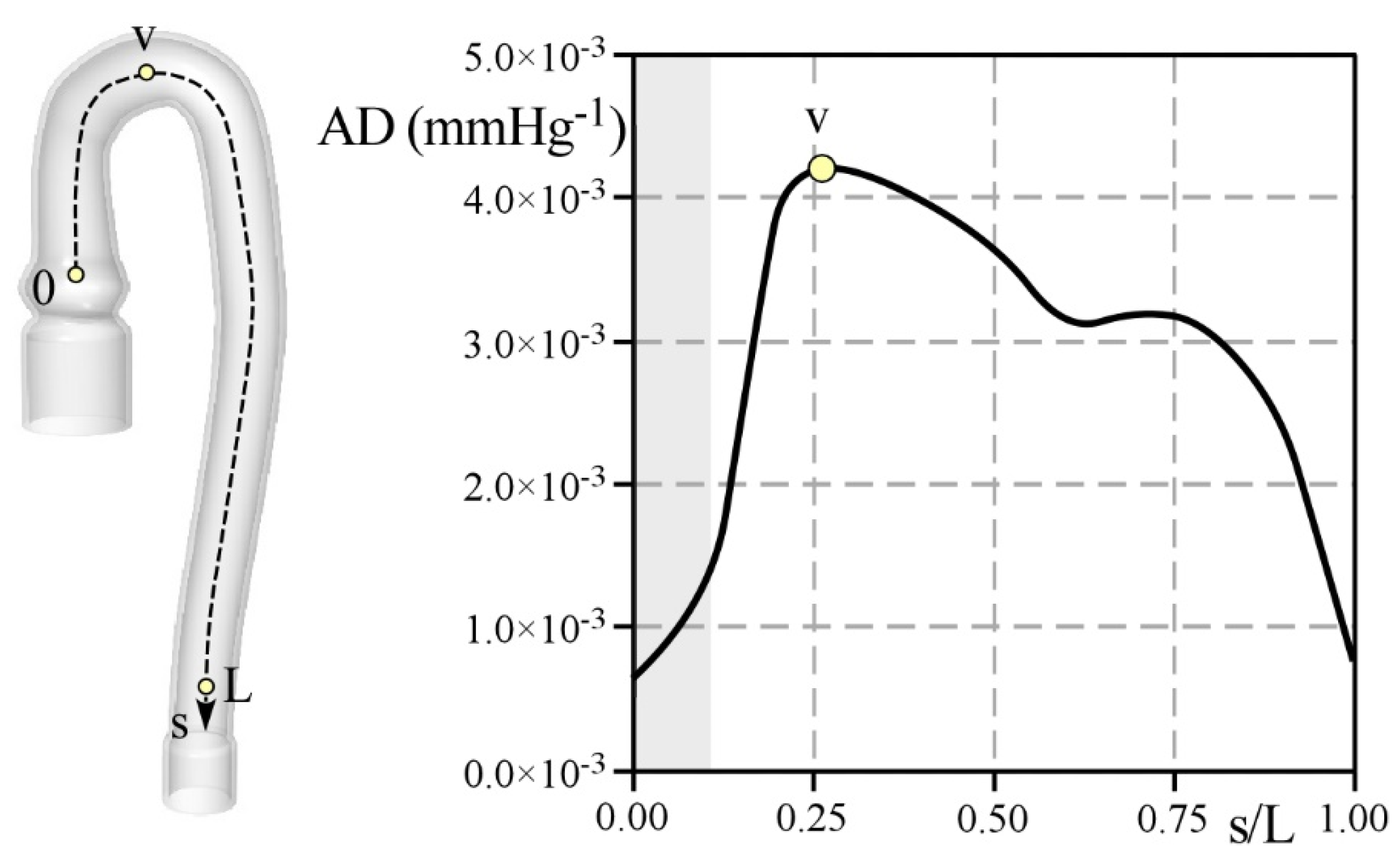
3.3. Estimation of the Phantom Distensibility
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A
References
- Peruzzo, P.; Burriesci, G.; Susin, F.M.; Colli, A. In Vitro and Ex Vivo Hemodynamic Testing of an Innovative Occluder for Paravalvular Leak After Transcather Aortic Valve Implantation. J. Cardiovasc. Transl. Res. 2019, 12, 551–559. [Google Scholar] [CrossRef]
- Colli, A.; Besola, L.; Bizzotto, E.; Peruzzo, P.; Pittarello, D.; Gerosa, G. Edge-to-edge mitral valve repair with transapical neochord implantation. J. Thorac. Cardiovasc. Surg. 2018, 156, 144–148. [Google Scholar] [CrossRef] [Green Version]
- Peruzzo, P.; Susin, F.M.; Colli, A.; Burriesci, G. In vitro assessment of pacing as therapy for aortic regurgitation. Open Heart 2019, 6, e000976. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Burriesci, G.; Peruzzo, P.; Susin, F.M.; Tarantini, G.; Colli, A. In vitro hemodynamic testing of Amplatzer plugs for paravalvular leak occlusion after transcatheter aortic valve implantation. Int. J. Cardiol. 2016, 203, 1093–1099. [Google Scholar] [CrossRef] [PubMed]
- Rahmani, B.; Tzamtzis, S.; Ghanbari, H.; Burriesci, G.; Seifalian, A.M. Manufacturing and hydrodynamic assessment of a novel aortic valve made of a new nanocomposite polymer. J. Biomech. 2012, 45, 1205–1211. [Google Scholar] [CrossRef]
- Susin, F.M.; Espa, S.; Toninato, R.; Fortini, S.; Querzoli, G. Integrated strategy for in vitro characterization of a bileaflet mechanical aortic valve. BioMed. Eng. OnLine 2017, 16, 29. [Google Scholar] [CrossRef] [Green Version]
- Gawenda, M.; Knez, P.; Jaschke, G.; Wassmer, G.; Schmitz-Rixen, T.; Brunkwall, J. Endotension is influenced by wall compliance in a latex aneurysm model. Eur. J. Vasc. Endovasc. Surg. 2004, 27, 45–50. [Google Scholar] [CrossRef] [Green Version]
- Annio, G.; Franzetti, G.; Bonfanti, M.; Gallarello, A.; Palombi, A.; De Momi, E.; Homer-Vanniasinkam, S.; Wurdemann, H.A.; Tsang, V.; Diáz-Zuccarini, V.; et al. Low-cost fabrication of polyvinyl alcohol-based personalized vascular phantoms for in vitro hemodynamic studies: Three applications. J. Eng. Sci. Med. Diagn. Ther. 2020, 3, 034501. [Google Scholar] [CrossRef]
- Chi, Q.-Z.; Mu, L.-Z.; He, Y.; Luan, Y.; Jing, Y.-C. A Brush–Spin–Coating Method for Fabricating In Vitro Patient-Specific Vascular Models by Coupling 3D-Printing. Cardiovasc. Eng. Technol. 2021, 12, 200–214. [Google Scholar] [CrossRef]
- Biglino, G.; Giardini, A.; Baker, C.; Figliola, R.S.; Hsia, T.Y.; Taylor, A.M.; Schievano, S. In Vitro Study of the Norwood Palliation. ASAIO J. 2012, 58, 25–31. [Google Scholar] [CrossRef] [PubMed]
- Yip, T.H.; Yu, S.C.M. Cyclic transition to turbulence in rigid abdominal aortic aneurysm models. Fluid Dyn. Res. 2001, 29, 81–113. [Google Scholar] [CrossRef]
- Chong, C.K.; Rowe, C.S.; Sivancsan, S.; Rattray, A.; Black, R.A.; Shortland, A.P.; How, T.V. Computer aided design and fabrication of models for in vitro studies of vascular fluid dynamics. Proc. Inst. Mech. Eng. Part H J. Eng. Med. 1999, 213, 1–4. [Google Scholar] [CrossRef]
- Asbury, C.L.; Ruberti, J.W.; Bluth, E.I.; Peattie, R.A. Experimental investigation of steady flow in rigid models of abdominal aortic aneurysms. Ann. Biomed. Eng. 1995, 23, 29–39. [Google Scholar] [CrossRef] [PubMed]
- Gardin, C.; Ferroni, L.; Latremouille, C.; Chachques, J.C.; Mitrečić, D.; Zavan, B. Recent Applications of Three Dimensional Printing in Cardiovascular Medicine. Cells 2020, 9, 742. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wang, H.; Song, H.; Yang, Y.; Cao, Q.; Hu, Y.; Chen, J.; Guo, J.; Wang, Y.; Jia, D.; Cao, S.; et al. Three-dimensional printing for cardiovascular diseases: From anatomical modeling to dynamic functionality. BioMed. Eng. OnLine 2020, 19, 76. [Google Scholar] [CrossRef] [PubMed]
- Huetter, L.; Geoghegan, P.H.; Docherty, P.D.; Lazarjan, M.S.; Clucas, D.; Jermy, M. Application of a meta-analysis of aortic geometry to the generation of a compliant phantom for use in particle image velocimetry experimentation. IFAC-Pap. 2015, 48, 407–412. [Google Scholar] [CrossRef]
- Sulaiman, A.; Boussel, L.; Taconnet, F.; Serfaty, J.M.; Alsaid, H.; Attia, C.; Huet, L.; Douek, P. In vitro non-rigid life-size model of aortic arch aneurysm for endovascular prosthesis assessment. Eur. J. Cardio-Thorac. Surg. 2008, 33, 53–57. [Google Scholar] [CrossRef]
- Gallarello, A.; Palombi, A.; Annio, G.; Homer-Vanniasinkam, S.; De Momi, E.; Maritati, G.; Torii, R.; Burriesci, G.; Wurdemann, H.A. Patient-Specific Aortic Phantom with Tunable Compliance. J. Eng. Sci. Med. Diagn. Ther. 2019, 2, 041005. [Google Scholar] [CrossRef]
- Sparks, A.J.; Smith, C.M.; Allman, A.B.; Senko, J.L.; Meess, K.M.; Ducharme, R.W.; Springer, M.E.; Waqas, M.; Siddiqui, A.H. Compliant vascular models 3D printed with the Stratasys J750: A direct characterization of model distensibility using intravascular ultrasound. 3D Print. Med. 2021, 7, 28. [Google Scholar] [CrossRef]
- Biglino, G.; Verschueren, P.; Zegels, R.; Taylor, A.M.; Schievano, S. Rapid prototyping compliant arterial phantoms for in-vitro studies and device testing. J. Cardiovasc. Magn. Reson. Off. J. Soc. Cardiovasc. Magn. Reson. 2013, 15, 2. [Google Scholar] [CrossRef] [Green Version]
- Comunale, G.; di Micco, L.; Boso, D.P.; Susin, F.M.; Peruzzo, P. Numerical models can assist choice of an aortic phantom for in vitro testing. Bioengineering 2021, 8, 101. [Google Scholar] [CrossRef] [PubMed]
- Vukicevic, M.; Mosadegh, B.; Min, J.K.; Little, S.H. Cardiac 3D Printing and its Future Directions. JACC Cardiovasc. Imaging 2017, 10, 171–184. [Google Scholar] [CrossRef]
- Dong, E.; Zhao, Z.; Wang, M.; Xie, Y.; Li, S.; Shao, P.; Cheng, L.; Xu, R.X. Three-dimensional fuse deposition modeling of tissue-simulating phantom for biomedical optical imaging. J. Biomed. Opt. 2015, 20, 121311. [Google Scholar] [CrossRef] [PubMed]
- Jalali, A.; Jones, G.F.; Licht, D.J.; Nataraj, C. Application of mathematical modeling for simulation and analysis of hypoplastic left heart syndrome (HLHS) in pre-and postsurgery conditions. BioMed Res. Int. 2015, 2015, 987293. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Comunale, G.; Peruzzo, P.; Castaldi, B.; Razzolini, R.; Di Salvo, G.; Padalino, M.A.; Susin, F.M. Understanding and recognition of the right ventricular function and dysfunction via a numerical study. Sci. Rep. 2021, 11, 3709. [Google Scholar] [CrossRef] [PubMed]
- Comunale, G.; Padalino, M.; Maiorana, C.; di Salvo, G.; Susin, F.M. Ventricular outflow tract obstruction: An in-silico model to relate the obstruction to hemodynamic quantities in cardiac paediatric patients. PLoS ONE 2021, 16, e0258225. [Google Scholar] [CrossRef]
- Reymond, P.; Merenda, F.; Perren, F.; Rüfenacht, D.; Stergiopulos, N. Validation of a one-dimensional model of the systemic arterial tree. Am. J. Physiol.-Heart Circ. Physiol. 2009, 297, H208–H222. [Google Scholar] [CrossRef] [Green Version]
- Rampazzo, M.; Manzoni, E.; Lionello, M.; di Micco, L.; Susin, F.M. Automation of the peripheral resistance valve in a hydro-mechanical cardiovascular pulse duplicator system. Control Eng. Pract. 2021, 116, 104929. [Google Scholar] [CrossRef]
- Lanir, Y.; Fung, Y.C. Two-dimensional mechanical properties of rabbit skin—II. Experimental results. J. Biomech. 1974, 7, 171–182. [Google Scholar] [CrossRef]
- Ogden, R.W.; Saccomandi, G.; Sgura, I. Fitting hyperelastic models to experimental data. Comput. Mech. 2004, 34, 484–502. [Google Scholar] [CrossRef] [Green Version]
- Stefanadis, C.; Stratos, C.; Boudoulas, H.; Kourouklis, C.; Toutouzas, P. Distensibility of the ascending aorta: Comparison of invasive and non-invasive techniques in healthy men and in men with coronary artery disease. Eur. Heart J. 1990, 11, 990–996. [Google Scholar] [CrossRef] [PubMed]
- Stefanadis, C.; Wooley, C.F.; Bush, C.A.; Kolibash, A.J.; Boudoulas, H. Aortic distensibility abnormalities in coronary artery disease. Am. J. Cardiol. 1987, 59, 1300–1304. [Google Scholar] [CrossRef]
- Fung, G.S.K.; Lam, S.K.; Cheng, S.W.K.; Chow, K.W. On stent-graft models in thoracic aortic endovascular repair: A computational investigation of the hemodynamic factors. Comput. Biol. Med. 2008, 38, 484–489. [Google Scholar] [CrossRef]
- Li, Z.; Kleinstreuer, C. Blood flow and structure interactions in a stented abdominal aortic aneurysm model. Med. Eng. Phys. 2005, 27, 369–382. [Google Scholar] [CrossRef] [PubMed]
- Rinaudo, A.; Pasta, S. Regional variation of wall shear stress in ascending thoracic aortic aneurysms. Proc. Inst. Mech. Eng. Part H J. Eng. Med. 2014, 228, 627–638. [Google Scholar] [CrossRef] [PubMed]
- Tan, F.P.P.; Borghi, A.; Mohiaddin, R.H.; Wood, N.B.; Thom, S.; Xu, X.Y. Analysis of flow patterns in a patient-specific thoracic aortic aneurysm model. Comput. Struct. 2009, 87, 680–690. [Google Scholar] [CrossRef]
- Herment, A.; Lefort, M.; Kachenoura, N.; De Cesare, A.; Taviani, V.; Graves, M.J.; Pellot-Barakat, C.; Frouin, F.; Mousseaux, E. Automated estimation of aortic strain from steady-state free-precession and phase contrast MR images. Magn. Reson. Med. 2011, 65, 986–993. [Google Scholar] [CrossRef]
- Wang, Y.; Joannic, D.; Delassus, P.; Lalande, A.; Juillion, P.; Fontaine, J.-F. Comparison of the strain field of abdominal aortic aneurysm measured by magnetic resonance imaging and stereovision: A feasibility study for prediction of the risk of rupture of aortic abdominal aneurysm. J. Biomech. 2015, 48, 1158–1164. [Google Scholar] [CrossRef]



Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Di Micco, L.; Comunale, G.; Bonvini, S.; Peruzzo, P.; Susin, F.M. Distensibility of Deformable Aortic Replicas Assessed by an Integrated In-Vitro and In-Silico Approach. Bioengineering 2022, 9, 94. https://doi.org/10.3390/bioengineering9030094
Di Micco L, Comunale G, Bonvini S, Peruzzo P, Susin FM. Distensibility of Deformable Aortic Replicas Assessed by an Integrated In-Vitro and In-Silico Approach. Bioengineering. 2022; 9(3):94. https://doi.org/10.3390/bioengineering9030094
Chicago/Turabian StyleDi Micco, Luigi, Giulia Comunale, Stefano Bonvini, Paolo Peruzzo, and Francesca Maria Susin. 2022. "Distensibility of Deformable Aortic Replicas Assessed by an Integrated In-Vitro and In-Silico Approach" Bioengineering 9, no. 3: 94. https://doi.org/10.3390/bioengineering9030094
APA StyleDi Micco, L., Comunale, G., Bonvini, S., Peruzzo, P., & Susin, F. M. (2022). Distensibility of Deformable Aortic Replicas Assessed by an Integrated In-Vitro and In-Silico Approach. Bioengineering, 9(3), 94. https://doi.org/10.3390/bioengineering9030094





