Long-Term Care Resident Awareness and Interest in Spasticity Treatments
Abstract
:1. Introduction
2. Materials and Methods
2.1. Setting
2.2. Treatment Awareness and Interest Interview
2.3. Analysis
3. Results
3.1. Study Participants
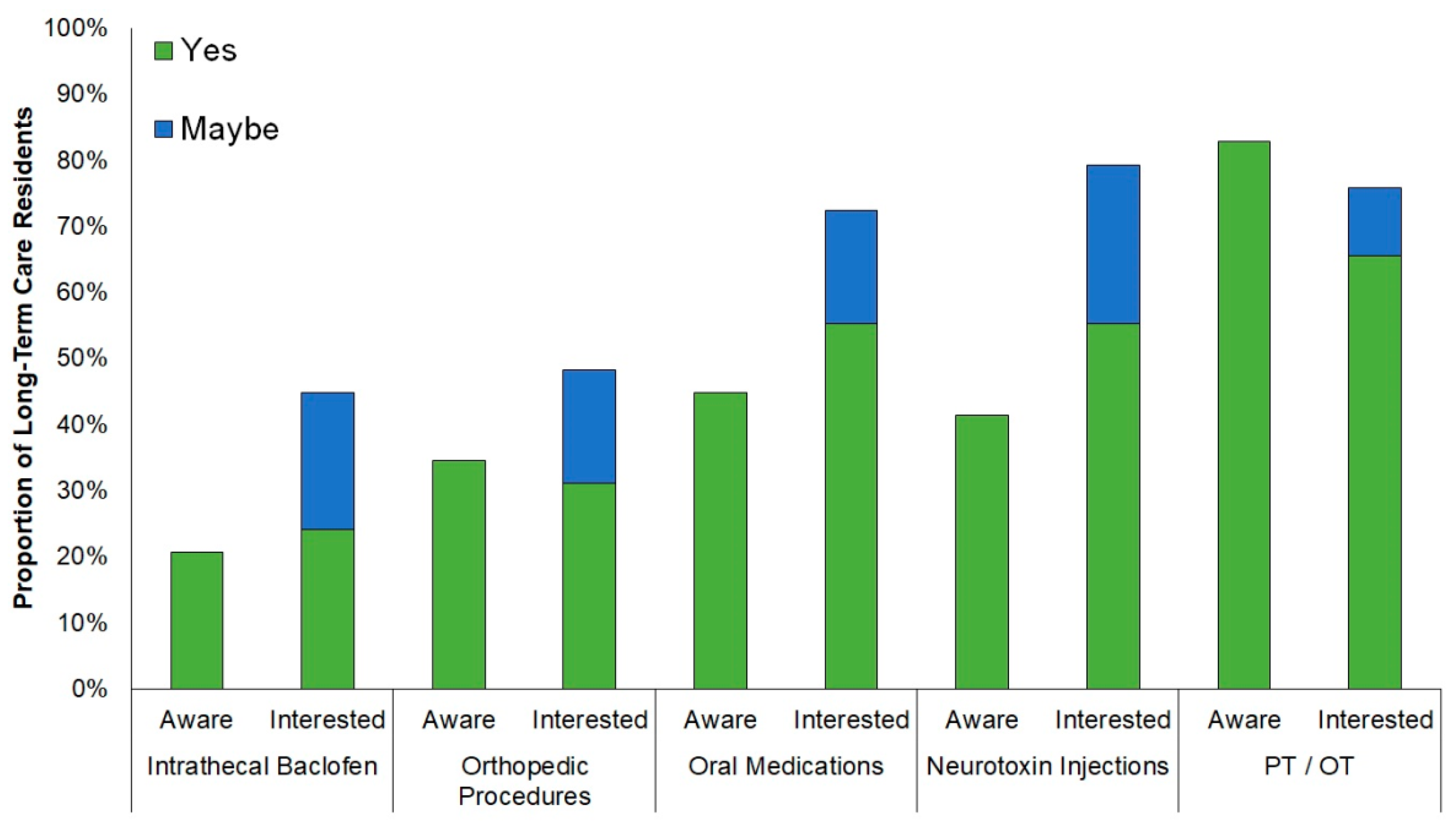
3.2. Treatment Awareness and Interest Interview
3.3. Barriers to Treatment
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Pfister, A.A.; Roberts, A.G.; Taylor, H.M.; Noel-Spaudling, S.; Damian, M.M.; Charles, P.D. Spasticity in Adults Living in a Developmental Center. Arch. Phys. Med. Rehabil. 2003, 84, 1808. [Google Scholar] [CrossRef]
- Turchan, M.; Hudson, T.S.; Gill, C.E.; Currie, A.; Molinari, A.L.; Hacker, M.L.; Phibbs, F.T.; Tolleson, C.; Millan, S.H.; Heusinkveld, L.E.; et al. The Prevalence of Spasticity in Veterans Living in a Long-Term Care Facility. Int. J. Neurol. Neurother. 2017, 3, 2–5. [Google Scholar] [CrossRef]
- Gill, C.E.; Hacker, M.L.; Meystedt, J.; Turchan, M.; Schnelle, J.F.; Simmons, S.F.; Habermann, R.; Phibbs, F.T.; Charles, D. Prevalence of Spasticity in Nursing Home Residents. J. Am. Med. Dir. Assoc. 2020, 8, 1157–1160. [Google Scholar] [CrossRef] [PubMed]
- Hacker, M.L.; Ploucher, S.; Naik, A.G.; Turchan, M.; Meystedt, J.C.; Harper, K.; Hedera, P.; Pirtle, C.J.; Stubblefield, K.; Charles, D. A simple bedside screening tool for spasticity referral. Clin. Interv. Aging 2020, 15, 655–662. [Google Scholar] [CrossRef] [PubMed]
- Pattuwage, L.; Olver, J.; Martin, C.; Lai, F.; Piccenna, L.; Gruen, R.; Bragge, P. Management of Spasticity in Moderate and Severe Traumatic Brain Injury. J. Head Trauma Rehabil. 2017, 32, E1–E12. [Google Scholar] [CrossRef] [PubMed]
- Sommerfeld, D.K.; Eek, E.U.-B.; Svensson, A.-K.; Holmqvist, L.W.; von Arbin, M.H. Spasticity After Stroke. Stroke 2004, 35, 134–140. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ganapathy, V.; Graham, G.D.; Dibonaventura, M.D.; Gillard, P.J.; Goren, A.; Zorowitz, R.D. Caregiver burden, productivity loss, and indirect costs associated with caring for patients with poststroke spasticity. Clin. Interv. Aging 2015. [Google Scholar] [CrossRef] [Green Version]
- Satkunam, L.E. Rehabilitation medicine: 3. Management of adult spasticity. CMAJ 2003, 169, 1173–1179. [Google Scholar]
- Haisma, J.A.; van der Woude, L.H.; Stam, H.J.; Bergen, M.P.; Sluis, T.A.; Post, M.W.; Bussmann, J.B. Complications following spinal cord injury: Occurrence and risk factors in a longitudinal study during and after inpatient rehabilitation. J. Rehabil. Med. 2007, 39, 393–398. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rekand, T. Clinical assessment and management of spasticity: A review. Acta Neurol. Scand. 2010, 122, 62–66. [Google Scholar] [CrossRef] [PubMed]
- Nair, K.P.S.; Marsden, J. The management of spasticity in adults. BMJ 2014, 349, 1–10. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Shiner, C.T.; Vratsistas-Curto, A.; Bramah, V.; Faux, S.G.; Watanabe, Y. Prevalence of upper-limb spasticity and its impact on care among nursing home residents with prior stroke. Disabil. Rehabil. 2019, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Tong, B.C.; Wallace, S.; Hartwig, M.G.; D’Amico, T.A.; Huber, J.C. Patient Preferences in Treatment Choices for Early-Stage Lung Cancer. Ann. Thorac. Surg. 2016, 102, 1837–1844. [Google Scholar] [CrossRef] [Green Version]
- Shpiner, D.S.; Di Luca, D.G.; Cajigas, I.; Diaz, J.S.; Margolesky, J.; Moore, H.; Levin, B.E.; Singer, C.; Jagid, J.; Luca, C.C. Gender Disparities in Deep Brain Stimulation for Parkinson’s Disease. Neuromodulation 2019, 22, 484–488. [Google Scholar] [CrossRef] [PubMed]
- Magaziner, J.; German, P.; Zimmerman, S.I.; Hebel, J.R.; Burton, L.; Gruber-Baldini, A.L.; May, C.; Kittner, S. The prevalence of dementia in a statewide sample of new nursing home admissions aged 65 and older: Diagnosis by expert panel. Gerontologist 2000, 40, 663–672. [Google Scholar] [CrossRef] [PubMed]

| Nursing Home | Veterans’ Home | |
|---|---|---|
| Participants, n | 18 | 11 |
| Age in Years Mean ± SD (Age Range) | 79.5 ± 14.1 (51.4 to 100.3) | 77.5 ± 8.2 (66.5 to 91.1) |
| Sex, n (%) | ||
| Male | 7/18 (39%) | 11/11 (100%) |
| Female | 11/18 (61%) | 0/11 (0%) |
| Spasticity Being Treated, n (%) | 2/18 (11%) | 0/11 (0%) |
| Question, % (n) | Easy | Sometimes Difficult | Difficult | Unsure |
| How easy is it for you to get a doctor’s appointment when you want one? | 55% (6) | 9% (1) | 18% (2) | 18% (2) |
| How easy is it for you to get from where you live to doctor’s office? | 45% (5) | 18% (2) | 9% (1) | 27% (3) |
| Question, % (n) | Yes | No | Unsure | |
| Do you have the option to see a special doctor, like a heart doctor or brain doctor, if you want? | 82% (9) | 18% (2) | 0% (0) | |
| Do you think getting treated for spasticity would make your quality of life better? | 64% (7) | 36% (4) | 0% (0) | |
| Do you know if your insurance covers any of the treatments? | 27% (3) | 9% (1) | 64% (7) | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hacker, M.L.; Putman, M.S.; Gill, C.E.; Turchan, M.; Hudson, T.S.; Currie, A.D.; Phibbs, F.T.; Charles, D. Long-Term Care Resident Awareness and Interest in Spasticity Treatments. Geriatrics 2021, 6, 21. https://doi.org/10.3390/geriatrics6010021
Hacker ML, Putman MS, Gill CE, Turchan M, Hudson TS, Currie AD, Phibbs FT, Charles D. Long-Term Care Resident Awareness and Interest in Spasticity Treatments. Geriatrics. 2021; 6(1):21. https://doi.org/10.3390/geriatrics6010021
Chicago/Turabian StyleHacker, Mallory L., Michael S. Putman, Chandler E. Gill, Maxim Turchan, Taylor S. Hudson, Amanda D. Currie, Fenna T. Phibbs, and David Charles. 2021. "Long-Term Care Resident Awareness and Interest in Spasticity Treatments" Geriatrics 6, no. 1: 21. https://doi.org/10.3390/geriatrics6010021
APA StyleHacker, M. L., Putman, M. S., Gill, C. E., Turchan, M., Hudson, T. S., Currie, A. D., Phibbs, F. T., & Charles, D. (2021). Long-Term Care Resident Awareness and Interest in Spasticity Treatments. Geriatrics, 6(1), 21. https://doi.org/10.3390/geriatrics6010021






