-
 Behavioural Change Interventions for Preventing Periodontal Disease in Older Adults: A Literature Review
Behavioural Change Interventions for Preventing Periodontal Disease in Older Adults: A Literature Review -
 The Communication Satisfaction of Geriatric Patients Treated by Dental Students and Dentists in a University Dental Clinic: A Cross-Sectional Study
The Communication Satisfaction of Geriatric Patients Treated by Dental Students and Dentists in a University Dental Clinic: A Cross-Sectional Study -
 Cardiorenal Syndrome in the Elderly: Challenges and Considerations
Cardiorenal Syndrome in the Elderly: Challenges and Considerations -
 Development of a Specialized Telemedicine Protocol for Cognitive Disorders: The TeleCogNition Project in Greece
Development of a Specialized Telemedicine Protocol for Cognitive Disorders: The TeleCogNition Project in Greece
Journal Description
Geriatrics
Geriatrics
is an international, peer-reviewed, scientific open access journal on geriatric medicine published bimonthly online by MDPI.
- Open Access— free for readers, with article processing charges (APC) paid by authors or their institutions.
- High Visibility: indexed within Scopus, ESCI (Web of Science), PubMed, PMC, and other databases.
- Journal Rank: CiteScore - Q2 (Health (Social Science))
- Rapid Publication: manuscripts are peer-reviewed and a first decision is provided to authors approximately 19.5 days after submission; acceptance to publication is undertaken in 3.6 days (median values for papers published in this journal in the first half of 2025).
- Recognition of Reviewers: reviewers who provide timely, thorough peer-review reports receive vouchers entitling them to a discount on the APC of their next publication in any MDPI journal, in appreciation of the work done.
- Testimonials: See what our editors and authors say about Geriatrics.
- Journal Cluster of Healthcare Sciences and Services: Geriatrics, Journal of Ageing and Longevity, Healthcare, Hospitals, Hygiene, International Journal of Environmental Research and Public Health and Nursing Reports.
Impact Factor:
2.1 (2024);
5-Year Impact Factor:
2.5 (2024)
Latest Articles
Associations Between Decision-Making Biases and Swallowing and Physical Functions in Community-Dwelling Older Adults: A Cross-Sectional Study
Geriatrics 2025, 10(6), 138; https://doi.org/10.3390/geriatrics10060138 (registering DOI) - 24 Oct 2025
Abstract
Background/Objective: In the context of global aging, maintaining daily habits such as adequate nutrition and regular exercise are essential to achieve healthy aging. Therefore, the preservation of swallowing and physical functions is fundamental. Jaw-opening force, an important swallowing function, is linked to physical
[...] Read more.
Background/Objective: In the context of global aging, maintaining daily habits such as adequate nutrition and regular exercise are essential to achieve healthy aging. Therefore, the preservation of swallowing and physical functions is fundamental. Jaw-opening force, an important swallowing function, is linked to physical function. Daily health behaviors are shaped by decision-making biases, which influence decision-making. Individuals with high procrastination tendencies may be less likely to engage in health-promoting behaviors, potentially leading to functional decline. While such tendencies are associated with general health behaviors, little is known about their associations with swallowing and physical functions among older adults. The objective of this study was to examine the associations between decision-making biases and swallowing and physical functions in community-dwelling older adults. Methods: A questionnaire survey was conducted to collect basic information and assess decision-making biases. The jaw-opening force (swallowing function) and grip strength (physical function) were measured. Associations of decision-making biases with jaw-opening force and grip strength were examined using multivariable linear regression analysis. We further conducted sex-stratified sensitivity analyses. Results: This cross-sectional study targeted 107 community-dwelling older adults. There was a significant negative association between procrastination tendency and jaw-opening force (B = −0.715, p = 0.005), and grip strength (B = −1.552, p = 0.003), indicating that individuals with a propensity for procrastination had lower jaw-opening force and grip strength. Conclusions: Procrastination tendency may be used as an indicator to detect swallowing and physical functions. Moreover, incorporating this modifiable factor to promote behavior change may prevent functional decline. The study results highlight the significance of considering individuals’ decision-making biases—particularly procrastination tendency—in clinical settings.
Full article
(This article belongs to the Section Dysphagia)
Open AccessArticle
Evaluating the Anticholinergic Burden in Older Patients: Comprehensive Insights from a Nationwide Survey Among Emergency Medicine Specialists in the UK
by
Piyawat Dilokthornsakul, Carrie Stewart, Phil Moss, Roy L. Soiza, Fraser Birse, Selvarani Subbarayan, Athagran Nakham, Nantawarn Kitikannakorn and Phyo K. Myint
Geriatrics 2025, 10(6), 137; https://doi.org/10.3390/geriatrics10060137 (registering DOI) - 24 Oct 2025
Abstract
►▼
Show Figures
Introduction: Older patients are often exposed to medications with anticholinergic activity. Anticholinergic burden (ACB) from medicines is linked to adverse health outcomes. However, healthcare professionals’ familiarity with ACB remains poor, and there is a lack of research on knowledge, attitudes, or practices
[...] Read more.
Introduction: Older patients are often exposed to medications with anticholinergic activity. Anticholinergic burden (ACB) from medicines is linked to adverse health outcomes. However, healthcare professionals’ familiarity with ACB remains poor, and there is a lack of research on knowledge, attitudes, or practices (KAPs) of ACB among Emergency department (ED) clinicians. Methods: A nationwide survey of ACB based on a pilot survey was developed using the KAP framework and assessed for face and content validity by ACB experts. It was distributed to ED physicians across the UK using REDCap through social media and professional networks. Results: Among the 108 ED physicians who responded, 54.6% (n = 59) were aware of the term ACB, but 54.2% (n = 32/59) of them were unable to describe it. Their mean scores for quantifying the ACB score and identifying side effects in older patients were 2.9 and 4.1 out of 10, respectively. 88.9% (n = 96) believed that ACB is an important consideration in older patients. 67.6% (n = 73) agreed that awareness of the consequences of prescribing anticholinergic medications to older patients is important. 50% (n = 54) emphasized the importance of being able to assess and quantify the ACB score. Of the 75 physicians who prescribed these medications, 40% (n = 30/75) were unaware of ACB. 38.7% (n = 29/75) rarely considered ACB, 30.7% (n = 23/75) never considered it, and only 1.3% (n = 1/75) always considered it. The majority of respondents (88.9%, n = 96) agreed that more education on ACB is needed in the ED. Conclusions: ED physicians in the UK have limited knowledge and awareness of ACB management and prescribing practices for older patients. However, they show positive attitudes towards their role in ACB management and a willingness to receive further education. The low response rate suggests that findings may reflect a motivated subset of clinicians. These results highlight the need for targeted education and further investigation into curricular coverage of prescribing safety and anticholinergic burden.
Full article
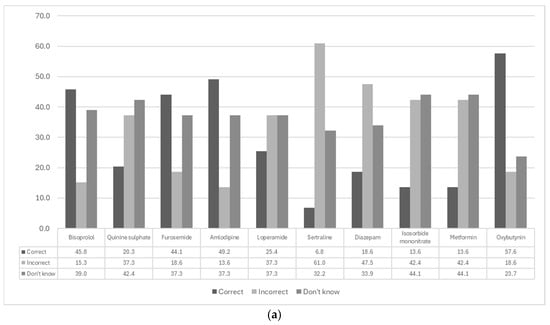
Figure 1
Open AccessArticle
Effect of Eight-Week Strength Training on Body Composition, Muscle Strength and Perceived Stress in Community-Dwelling Older Women
by
Laura Žlibinaitė, Laura Amšiejūtė, Daiva Baltaduonienė, Milda Gintilienė, Karolina Matukynienė and Ligita Mažeikė
Geriatrics 2025, 10(6), 136; https://doi.org/10.3390/geriatrics10060136 - 23 Oct 2025
Abstract
Background: Sarcopenia, characterized by loss of muscle mass, strength, and function, reduces independence and quality of life in older adults. Strength exercise (STR) mitigates these age-related declines, but evidence of short-term effectiveness remains limited. This study aimed to evaluate the effects of
[...] Read more.
Background: Sarcopenia, characterized by loss of muscle mass, strength, and function, reduces independence and quality of life in older adults. Strength exercise (STR) mitigates these age-related declines, but evidence of short-term effectiveness remains limited. This study aimed to evaluate the effects of eight weeks of STR on body composition, muscle strength, and psycho-emotional state in community-dwelling elderly women. Methods: A prospective, controlled, non-randomized study included 44 women assigned to an STR (n = 20) or control (CON, n = 22) group. The STR group performed supervised exercise twice weekly for eight weeks. The outcomes were body composition, handgrip strength (HGS), quadriceps (Q) and hamstrings (H) strength, and perceived stress (PSS-10), assessed at baseline and after intervention. Within-group changes were analyzed using paired t-tests, and between-group differences were evaluated using analysis of covariance (ANCOVA) adjusted for baseline values. Results: After baseline adjustment, body mass (p = 0.041, partial η2 = 0.103), BMI (body mass index, p = 0.030, partial η2 = 0.115), and body fat percentage (p = 0.047, partial η2 = 0.098) were significantly reduced in the STR group. Significant improvements were observed for H strength in both legs (p < 0.05, partial η2 = 0.128–0.131), right HGS (p = 0.025, partial η2 = 0.122), right HGS:BMI ratio (p = 0.013, partial η2 = 0.150), and H:Q ratios on both sides (p < 0.05, partial η2 = 0.109–0.118). No significant differences were observed for left-hand grip strength, knee extensor strength, or other body composition variables (p > 0.05). The perceived stress scores were significantly lower in the STR group post-intervention (p = 0.036, partial η2 = 0.108). Conclusions: An eight-week supervised strength exercise program was associated with favorable changes in muscle strength, body composition, and psycho-emotional state in elderly women.
Full article
(This article belongs to the Section Healthy Aging)
Open AccessArticle
Central Adiposity Assessed with Body Roundness Index and Mortality: The Seguimiento Universidad de Navarra Prospective Cohort
by
Ligia J. Dominguez, Carmen Sayon-Orea, Estefania Toledo, Maira Bes-Rastrollo, Carolina Donat-Vargas, Mario Barbagallo and Miguel A. Martínez-González
Geriatrics 2025, 10(6), 135; https://doi.org/10.3390/geriatrics10060135 - 23 Oct 2025
Abstract
►▼
Show Figures
Background/Objectives: Obesity is currently a global pandemic and a major risk factor for the development of chronic disease and increased mortality. Common methods used to define obesity, such as body mass index (BMI), do not accurately reflect body fat content or distribution. Methods:
[...] Read more.
Background/Objectives: Obesity is currently a global pandemic and a major risk factor for the development of chronic disease and increased mortality. Common methods used to define obesity, such as body mass index (BMI), do not accurately reflect body fat content or distribution. Methods: We investigated the prognostic significance of the body roundness index (BRI) on incident death in 12,642 participants (60.2% women, mean age: 39, standard deviation (SD): 12 years) from the “Seguimiento Universidad de Navarra” prospective cohort and compared it to waist-to-height ratio (WtHR) and waist circumference (WC). Participants were monitored through biennial questionnaires. The mean of the baseline BRI was 3.6 (SD: 1.4) units. Multivariable-adjusted Cox models were used to estimate hazard ratios (HR) and confidence intervals (CI) of death. Results: Over a median follow-up period of 11.5 years, 380 participants died (absolute mortality rate 1.74 × 10−3). In multivariable-adjusted models, higher quartiles of BRI were significantly associated with all-cause death, specifically in those ≥ 60 years (Quartile 4 vs. Quartile 1: HR 1.64; 95% CI: 1.00, 2.70). Considering the whole group (all ages), each 2-unit increase in BRI was linked to a 21% higher all-cause mortality risk in both men and women. This association was even stronger for participants aged over 60 years (multivariate adjusted HR for 2-unit BRI increase: 1.31; CI: 1.00, 1.72), while it was not significant when considering only those under 60 years. The associations of z-WtHR and z-WC with incident mortality for all participants were also significant in the fully adjusted model (HRs: 1.14; CI: 1.01, 1.27, and HRs: 1.16; CI: 1.04, 1.30, respectively). Mortality associations assessed using the BRI, WtHR, and WC were superior to associations based on the BMI. Conclusions: BRI shows a linear link with all-cause mortality in healthy adults ≥ 60, while WtHR and WC were also mortality predictors. Thus, lower central fat may help reduce early death risk.
Full article
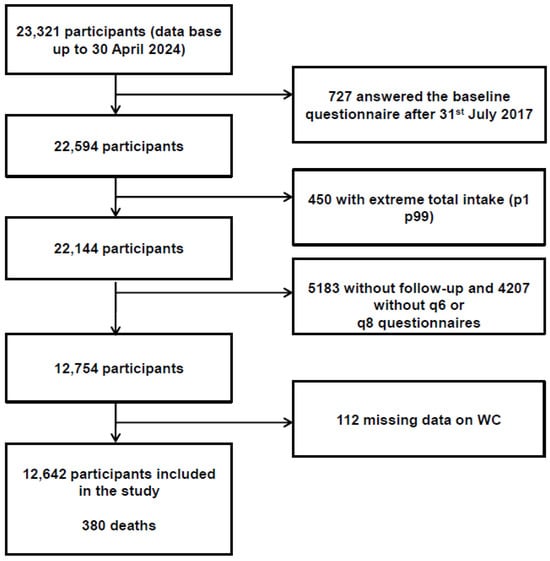
Figure 1
Open AccessArticle
Prevalence of Frailty and Associated Sociodemographic, Biomedical, and Biochemical Factors Amongst Participants Residing in Limpopo Province, South Africa
by
Reneilwe Given Mashaba, Kagiso P. Seakamela, Solomon S. R. Choma, Eric Maimela, Joseph Tlouyamma and Cairo Bruce Ntimana
Geriatrics 2025, 10(5), 134; https://doi.org/10.3390/geriatrics10050134 - 21 Oct 2025
Abstract
Background: Frailty is a common syndrome amongst older individuals characterized by a progressive long-term loss of physical and or cognitive resilience. Given the high prevalence and chronic conditions and the lack of literature on frailty among rural older individuals in South Africa, the
[...] Read more.
Background: Frailty is a common syndrome amongst older individuals characterized by a progressive long-term loss of physical and or cognitive resilience. Given the high prevalence and chronic conditions and the lack of literature on frailty among rural older individuals in South Africa, the present study aimed to investigate the prevalence of frailty and its associated factors in older individuals residing in Limpopo province. Methods: This was a cross-sectional study, comprising 546 participants (48.4% males and 51.6% females) using Africa Wits-INDEPTH Partnership for Genomic Research (AWI-Gen) phase 2 data. Convenient sampling was used to select the participants. Frailty was measured using the five criteria proposed by Fried. Data was analyzed using Statistical Package for the Social Sciences (SPSS) 27. Results: The mean age (SD) of the participants was 66.78 ± 5.72. The proportion of individuals living with frailty was 26.4%. Individuals living with frailty were significantly older than both pre-frail and non-frail individuals. Current smokers significantly had higher proportion of frailty compared to both pre-frail and non-frail. The proportion of frailty reduced as the level of education increased. The present study found no association between biological sex and frailty. The likelihood of having frailty increased with age. On the unadjusted model, there was a significant association between frailty and 66 and above age group (OR: 1.61; 95% CI: 1.00–2.60). On the fully adjusted model the same age group was 1.75 more likely to be frail with a p value of 0.001. The present study found no significant association between marital status, smoking, alcohol status, current smoker, hypertension, diabetes, and obesity with frailty. Centrally obese participants were 0.48 and 0.37 times less likely to have frailty on unadjusted and adjusted models, respectively. Participants with dyslipidemia indicated by high total cholesterol (TC) were 2.25 times more likely to be associated with frailty. Conclusions: The prevalence of frailty was 26.4% and it was associated with age, educational status and dyslipidemia. Based on the findings of the present study, the authors recommend implementation of screening programs, for frailty in healthcare settings, especially targeting older adults with comorbidities.
Full article
(This article belongs to the Collection Frailty in Older Adults)
►▼
Show Figures

Figure 1
Open AccessArticle
Exploring Frailty Status and Blood Biomarkers: A Multidimensional Approach to Alzheimer’s Diagnosis
by
Aurora Cermelli, Armando Crisafi, Alberto Mario Chiarandon, Giorgia Mirabelli, Chiara Lombardo, Virginia Batti, Silvia Boschi, Elisa Maria Piella, Fausto Roveta, Innocenzo Rainero and Elisa Rubino
Geriatrics 2025, 10(5), 133; https://doi.org/10.3390/geriatrics10050133 - 17 Oct 2025
Abstract
►▼
Show Figures
Background: Frailty is a multidimensional syndrome reflecting reduced physiological reserve, increasingly recognized as a relevant factor in the clinical assessment of older adults with cognitive disorders. Objective: To explore the association between frailty, as measured by the Multidimensional Prognostic Index (MPI), cognitive performance,
[...] Read more.
Background: Frailty is a multidimensional syndrome reflecting reduced physiological reserve, increasingly recognized as a relevant factor in the clinical assessment of older adults with cognitive disorders. Objective: To explore the association between frailty, as measured by the Multidimensional Prognostic Index (MPI), cognitive performance, and plasma biomarkers of Alzheimer’s disease (AD), and to examine the correlation between plasma and cerebrospinal fluid (CSF) biomarkers. Methods: This cross-sectional observational study included 40 patients (mean age 68.0 ± 9.0 years; 42.5% female) undergoing a diagnostic workup for cognitive decline. Patients were classified into AD (n = 20) and non-AD (n = 20) groups based on CSF AT[N] profiles. Frailty was assessed using the MPI. Linear and logistic regression models adjusted for age, sex, and education examined associations between MPI, cognitive scores, and plasma biomarkers (Aβ42, Aβ42/40, p-tau181, NfL). Correlations between plasma and CSF biomarkers and ROC analyses were also performed. Results: The AD group showed significantly higher plasma p-tau181 levels and MPI scores. MPI was positively associated with plasma p-tau181 levels (β = 4.26, p = 0.009). Plasma p-tau181 correlated strongly with CSF p-tau181 (R = 0.523, p < 0.001) and with CSF Aβ42/40 ratio (R = −0.541, p < 0.001) and showed high diagnostic accuracy (AUC = 0.910). Combining MPI with plasma biomarkers improved classification between AD and non-AD cases (AUC = 0.941). Conclusions: These findings support the value of incorporating frailty assessment in the diagnostic process of AD. The integration of geriatric tools and blood-based biomarkers may improve early detection and promote a more comprehensive approach in dementia evaluation.
Full article

Figure 1
Open AccessReview
Alzheimer’s Disease in Illinois: Analyzing Disparities and Projected Trends
by
Temitope Adeleke, Aston Knelsen-Dobson, Sean McGinity, Kyle M. Fontaine, Benedict C. Albensi, Banibrata Roy and Aida Adlimoghaddam
Geriatrics 2025, 10(5), 132; https://doi.org/10.3390/geriatrics10050132 - 14 Oct 2025
Abstract
Alzheimer’s disease (AD) is a growing public health issue disproportionately affecting adults 65 years and older. This growing trend is accompanied by rising economic, social, emotional, and physical costs, both for patients and their caregivers. As the U.S. population ages, understanding disparities in
[...] Read more.
Alzheimer’s disease (AD) is a growing public health issue disproportionately affecting adults 65 years and older. This growing trend is accompanied by rising economic, social, emotional, and physical costs, both for patients and their caregivers. As the U.S. population ages, understanding disparities in AD prevalence particularly by gender and age has become increasingly important, particularly in high-burden states like Illinois. This review focuses on gender and age disparities in AD, with a specific emphasis on Illinois. This review integrates national and global trends with state-specific projections and explores modifiable and non-modifiable risk factors that may contribute to these disparities. We analyzed projections from the Illinois Department of Public Health and the Alzheimer’s Association to assess AD prevalence by gender and age across Illinois’ 102 counties from 2020 to 2030, disaggregated by gender and age. Rates were compared with U.S. and global trends. Risk factors such as diabetes, education, access to care, and socioeconomic status were reviewed in the context of these disparities. Women consistently show higher AD prevalence across age groups and regions, with the greatest increase in cases is projected among adults aged 75 to 84 years, particularly in regions with higher women populations and social vulnerability. If unaddressed, risk factors like lower education, rural residency, and limited healthcare access may worsen these disparities. Addressing them requires focused public health efforts that combine early screening, caregiver support, and regional resource allocation. Illinois serves as a case study for targeted interventions applicable to broader national strategies.
Full article
(This article belongs to the Section Basic Science)
►▼
Show Figures

Figure 1
Open AccessArticle
Exploring the Effect of Social Media and Group Chat Use on Social Isolation Among the Older Adults: A Study in Urban Japan
by
Yohei Sekikawa, Masafumi Kunishige, Taichi Hitomi and Kazumi Kikuchi
Geriatrics 2025, 10(5), 131; https://doi.org/10.3390/geriatrics10050131 - 13 Oct 2025
Abstract
Background: Although research has been conducted on older adults and social media, the relationship between social media use and social isolation remains unclear. This study aimed to explore the relationship between social isolation and the frequency of use of social media and group
[...] Read more.
Background: Although research has been conducted on older adults and social media, the relationship between social media use and social isolation remains unclear. This study aimed to explore the relationship between social isolation and the frequency of use of social media and group chats. Methods: We measured social isolation using the Japanese version of the Lubben Social Network Scale (LSNS-6) in 411 older adults people living in urban areas. We used a questionnaire to survey their use of social networking services (SNS) such as LINE, Facebook, X (formerly Twitter), and Instagram, and their use of group chats. A separate questionnaire surveyed frequency of and participation in group chats. We analyzed associations between variables with logistic regression and a chi-squared test. Results: The most used service was LINE, with 51.3% of users participating in group chat. The analysis did not show an association between frequency of social media use and social isolation. However, group chat use, especially in groups of friends and acquaintances, was significantly negatively associated with social isolation (OR = 0.30, p < 0.001). Conclusions: This study revealed that LINE group chats may ameliorate social isolation among older adults. It also suggests that research focusing on its content and usage is needed.
Full article
(This article belongs to the Special Issue Healthy Ageing and Lifestyle Medicine: Current Knowledge and Future Direction (2nd Edition))
Open AccessSystematic Review
Fall-Related Adverse Events of Anti-Epileptic Drugs Used for Neuropathic Pain in Older Adults: A Systematic Review and Meta-Analysis
by
Arun Vamadevan, Vijesh Vijayan, Fellisha Marwein and Nishad Yoosuf
Geriatrics 2025, 10(5), 130; https://doi.org/10.3390/geriatrics10050130 - 11 Oct 2025
Abstract
►▼
Show Figures
Background: Older adults are at elevated risk of falls, especially when prescribed AEDs (AEDs) for neuropathic pain. The sedative and neuropsychiatric effects of these agents contribute significantly to fall-related morbidity. However, existing studies often lack stratification by age and dose. Objective: To systematically
[...] Read more.
Background: Older adults are at elevated risk of falls, especially when prescribed AEDs (AEDs) for neuropathic pain. The sedative and neuropsychiatric effects of these agents contribute significantly to fall-related morbidity. However, existing studies often lack stratification by age and dose. Objective: To systematically evaluate the incidence and drug-specific risk of falls and fall-related adverse events (AEs) in older adults prescribed AEDs for neuropathic pain. Methods: A systematic search was performed across PubMed, Scopus, CINAHL, ScienceDirect, and Cochrane Library databases up to May 2025. Studies were selected using PICOS criteria and included RCTs and controlled cohort studies reporting on AED-related AEs among participants aged ≥60 years. The methodological quality was assessed using RoB 2, ROBINS-I, and GRADE frameworks. Meta-analyses were performed using logit event rates and fixed-effects modeling via Comprehensive Meta-Analysis v3.7. Publication bias was evaluated using Begg’s and Egger’s tests. Results: Twenty-three studies met the inclusion criteria. The pooled logit event rate for falls was −1.693 (95% CI: −1.993 to −1.393), corresponding to a 15.5% incidence. Gabapentin showed the lowest fall risk (~10%), while pregabalin and carbamazepine were associated with higher rates of dizziness (up to 21.6%), sedation (~15.5%), and ataxia (~17.8%). Heterogeneity was low (I2 = 0–22.3%) across outcomes. Conclusions: AEDs carry a clinically significant fall risk in older adults, with dose-dependent patterns. Gabapentin may present a safer profile, while pregabalin and carbamazepine warrant cautious use and monitoring. These findings inform individualized prescribing and fall prevention strategies in geriatric neuropathic pain management.
Full article

Figure 1
Open AccessArticle
Prevalence and Associated Factors of Depression Among Elderly Hypertensive Patients in Vietnam
by
Tuan Van Nguyen, Tung Son Vu, Thang Thien Tran, Thong Thai Nguyen, Hoang Minh Le, Thang Nguyen, Kha Ai To Tran, Chau Minh Tran and Thong Van Nguyen
Geriatrics 2025, 10(5), 129; https://doi.org/10.3390/geriatrics10050129 - 1 Oct 2025
Abstract
Background/Objectives: Depression accompanying hypertension increases the burden of illness and negatively affects patients’ lives. However, depression among elderly with cardiovascular diseases in general and hypertension in specific has not been paid proper attention, especially in the context of Vietnam. Therefore, we expected to
[...] Read more.
Background/Objectives: Depression accompanying hypertension increases the burden of illness and negatively affects patients’ lives. However, depression among elderly with cardiovascular diseases in general and hypertension in specific has not been paid proper attention, especially in the context of Vietnam. Therefore, we expected to examine the prevalence, characteristics, and related factors of depression on elderly patients with hypertension. Methods: A cross-sectional study at the Department of Geriatrics, Can Tho Central General Hospital (from April 2020 to February 2022), involving 414 patients aged ≥60 years with hypertension. Depression was assessed using ICD-10 diagnostic criteria; related factors were evaluated using the Pittsburgh Sleep Quality Index (PSQI), KATZ12 index, and UCLA-LS3-J11 scale. Results: 31.4% of participants were found to have depression (mild 17.7%, moderate 9.7%, severe 4.0%). Common characteristics of depression included sleep disturbances, decreased energy, and low mood. Poor sleep quality, being female, lower socioeconomic status, higher hypertension grade, and increased loneliness were found to be significantly associated with depression. Conclusions: The high prevalence of depression among elderly hypertensive patients highlights the need for effective screening and intervention strategies. Addressing factors such as sleep quality, gender, socioeconomic challenges, and social isolation may help mitigate the burden of depression in this vulnerable population. This research should be expanded to elderly patients with hypertension in society, outpatients, and individuals with other chronic diseases. Developing a predictive model for depression in elderly patients, particularly those with chronic diseases, can improve early detection, treatment effectiveness, and overall care quality.
Full article
(This article belongs to the Section Geriatric Psychiatry and Psychology)
►▼
Show Figures

Figure 1
Open AccessArticle
Coping Together: A Qualitative Study Exploring the Work of Home Health Care Assistants in Ireland
by
Suzanne Cullen-Smith, Aoibheann McKeown, Kevin McKenna and Oonagh M. Giggins
Geriatrics 2025, 10(5), 128; https://doi.org/10.3390/geriatrics10050128 - 30 Sep 2025
Abstract
►▼
Show Figures
Background/Objectives: Home healthcare assistants (HHCAs) play a vital role in supporting older adults to remain in their homes. Yet, this work is often performed under conditions of emotional strain, limited resources, and systemic undervaluation. This study answers the question, how do HHCAs
[...] Read more.
Background/Objectives: Home healthcare assistants (HHCAs) play a vital role in supporting older adults to remain in their homes. Yet, this work is often performed under conditions of emotional strain, limited resources, and systemic undervaluation. This study answers the question, how do HHCAs cope with work-related stress? Methods: Undertaken during the COVID-19 pandemic, a period of heightened stress and mandated social distancing, online interviews were conducted with HHCAs (n = 10). Data were inductively analyzed and themes were identified. Results: It was found that amid experiences of fear, caregiver stress, grief, and exhaustion, HHCAs coped with resource, communication, and care challenges by relying on informal peer-managed communication systems with colleagues. Leveraging existing peer-support coping strategies, HHCAs negotiated caring for others while taking care of themselves alongside a care ecosystem under unprecedented strain. Conclusions: HHCAs are increasingly vital to front-line home health care amid global aging and a shift toward community-based services. Urgent organizational reform is needed to support their well-being, prevent stress, and avoid burnout. Research-informed sector-wide planning must ensure adequate resources to maintain high-quality home care in the face of rising demand and anticipated future health crises.
Full article

Graphical abstract
Open AccessArticle
The Association of Periodontal Status, Salivary Flow Rate, Salivary Cortisol Levels, and Cytokine Levels with Cognitive Status in Elderly Subjects
by
Mirsarinda Anandia Leander, Zalfa Karimah, Sandra Olivia Kuswandani, Robert Lessang, Sri Lelyati C. Masulili, Benso Sulijaya, Dimas Ilham Hutomo, Herlis Rahdewati, Koichi Tabeta and Fatimah Maria Tadjoedin
Geriatrics 2025, 10(5), 127; https://doi.org/10.3390/geriatrics10050127 - 23 Sep 2025
Abstract
►▼
Show Figures
Background/objectives: Aging is associated with a decline in physiological and cognitive functions. Periodontitis, a disease affecting the periodontal tissues, increases in prevalence with age. Bacteria and inflammatory mediators resulting from periodontitis can trigger neuroinflammation and potentially accelerate the progression of neurodegenerative diseases. This
[...] Read more.
Background/objectives: Aging is associated with a decline in physiological and cognitive functions. Periodontitis, a disease affecting the periodontal tissues, increases in prevalence with age. Bacteria and inflammatory mediators resulting from periodontitis can trigger neuroinflammation and potentially accelerate the progression of neurodegenerative diseases. This study aimed to evaluate the association between periodontal status, salivary flow rate, salivary cortisol levels, and cytokine levels with cognitive status in elderly Indonesian subjects. Methods: This cross-sectional study involved 70 participants aged ≥ 60 years from several social institutions in Jakarta and the Dental Hospital, Faculty of Dentistry, Universitas Indonesia. All participants provided written informed consent before the examination. Periodontal parameters, including plaque score, calculus index, bleeding on probing, number of remaining teeth, and functional tooth units, were assessed. Unstimulated salivary flow was collected over five minutes, and salivary cortisol levels were measured. Gingival crevicular fluid samples from the deepest periodontal pockets were collected to measure cytokine levels (TNF-α and IL-1β). Both cortisol and cytokine levels were analyzed using ELISA. Cognitive function was evaluated using the Hopkins Verbal Learning Test. Results: Plaque score, calculus index, and bleeding on probing were moderately associated with cognitive scores (p < 0.05). In contrast, the number of remaining teeth, functional tooth units, periodontitis severity, salivary flow rate, salivary cortisol, and cytokine levels were not significantly associated with cognitive scores (p > 0.05). Conclusions: These findings suggest that elderly individuals with cognitive impairment tend to have poorer periodontal health than those with normal cognitive function.
Full article

Figure 1
Open AccessArticle
Relationship Between Incidence of Knee Pain and Ground Reaction Force During Stepping Motion in Older Adults
by
Yusuke Oyama, Koki Ishikawa, Toshio Murayama and Tamaki Ohta
Geriatrics 2025, 10(5), 126; https://doi.org/10.3390/geriatrics10050126 - 23 Sep 2025
Abstract
Background: This 2-year longitudinal study was undertaken to investigate the relationship between incidence of knee pain and ground reaction force (GRF) in stepping motion in older adults. Methods: In all, 29 older participants, aged 50 and over (11 males and 18 females; 63.0
[...] Read more.
Background: This 2-year longitudinal study was undertaken to investigate the relationship between incidence of knee pain and ground reaction force (GRF) in stepping motion in older adults. Methods: In all, 29 older participants, aged 50 and over (11 males and 18 females; 63.0 ± 6.2 years), presented without knee pain at baseline. The participants performed a 10 s stepping motion at optimal speed on a force plate, and 14 mechanical and temporal parameters of vertical GRF were obtained. Knee pain was evaluated based on subjective complaint during daily activities. The participants were classified into a no pain (NP) group or a knee pain (KP) group. Results: Of the 29 participants (11 males, 18 females), 9 (all female) developed knee pain, representing 31.0% of the total participants and comprising the KP group at the follow-up. We compared the amount of change in the evaluated parameters between the two groups and found moderate effect sizes for the mechanical parameters, ΔMshaped (p = 0.07, d = 0.77) and ΔF2 (p = 0.08, d = 0.72), as well as a flatter change in the bimodal waveform of the GRF in the KP group. Conclusions: It was thus suggested that a flattening of the vertical GRF waveform during stepping motion may indicate early biomechanical changes associated with incident knee pain and that waveform changes in GRF may be useful for early detection of functional decline.
Full article
(This article belongs to the Special Issue Pain in Aging and Impaired Cognition, Especially Dementia: Clinical and Experimental Studies)
►▼
Show Figures

Figure 1
Open AccessFeature PaperArticle
Associations Between Physical Activity Frequency, Handgrip Strength, and Limitations in Activities of Daily Living in Middle-Aged and Older Adults with Widespread Pain: A Cross-Sectional Study Using Data from the SHARE Project
by
Ángel Denche-Zamorano, José Carmelo Adsuar, Sabina Barrios-Fernandez and Diana Salas-Gómez
Geriatrics 2025, 10(5), 125; https://doi.org/10.3390/geriatrics10050125 - 14 Sep 2025
Abstract
Background: The increase in life expectancy has led to a higher prevalence of chronic conditions, including widespread pain (WP), which often compromises functional independence and quality of life in older adults. WP is strongly associated with limitations in Basic and Instrumental Activities of
[...] Read more.
Background: The increase in life expectancy has led to a higher prevalence of chronic conditions, including widespread pain (WP), which often compromises functional independence and quality of life in older adults. WP is strongly associated with limitations in Basic and Instrumental Activities of Daily Living (BADLs and IADLs). While physical activity (PA) and muscle strength (handgrip) are known to enhance general health, their specific role in preserving functional capacity in individuals with WP remains underexplored. Methods: This cross-sectional study analyzed data from 1154 adults aged 50–80 reporting WP, drawn from the Ninth Wave of The Survey of Health, Ageing and Retirement in Europe (SHARE). Associations between moderate and vigorous PA (MPA and VPA), handgrip strength (HGS), and limitations in BADLs and IADLs were examined using multivariate logistic regression, adjusting for demographic and health-related variables. Results: Lower MPA was significantly associated with greater odds of all BADL and most IADL limitations, while VPA had no significant associations. Higher relative HGS was significantly associated with lower odds of limitations in BADLs and IADLs. Conclusions: Among older adults with WP, MPA and muscular strength appear to reduce the risk of functional limitations. These findings highlight the relevance of promoting sustainable strategies to support independence in aging populations.
Full article
(This article belongs to the Section Healthy Aging)
►▼
Show Figures

Figure 1
Open AccessArticle
Examination of Social Participation in Older Adults Undergoing Frailty Health Checkups Using Deep Learning Models
by
Yoshiharu Yokokawa, Keisuke Nakamura, Tomohiro Sasaki, Shinobu Yokouchi and Fumikazu Kimura
Geriatrics 2025, 10(5), 124; https://doi.org/10.3390/geriatrics10050124 - 12 Sep 2025
Abstract
Background/Objectives: Frailty in older adults limits social participation. We aimed to predict social participation in older individuals undergoing frailty health checkups using three machine learning (ML) models and identify key predictive factors through deep neural network (DNN) analysis. Methods: Overall, 301
[...] Read more.
Background/Objectives: Frailty in older adults limits social participation. We aimed to predict social participation in older individuals undergoing frailty health checkups using three machine learning (ML) models and identify key predictive factors through deep neural network (DNN) analysis. Methods: Overall, 301 older individuals were enrolled; 295 were included in the final analysis. The survey measured 18 attributes, including demographic, physical, cognitive, and social factors. Logistic regression (LR), nonlinear support vector machine (NLSVM), and DNN were used for prediction, with precision, accuracy, sensitivity, specificity, F1 score, and area under the curve (AUC) calculated as evaluation metrics. Results: Among 295 participants, 236 (80%) engaged in social activities, whereas 59 (20%) did not. The three models demonstrated complementary strengths: DNN provided the most balanced performance with superior sensitivity for detecting social participants; NLSVM showed the best overall discriminative ability but with higher false positive rates; and LR achieved the highest precision for correctly identifying participants but missed detecting social participants. AUC values ranged from 0.776 to 0.795 across models, indicating moderate discriminative performance. Contribution analysis revealed information-collection ability as the strongest predictor of social participation, followed by walking speed and number of cohabitants. Conclusions: ML models achieved moderate discriminative performance for predicting social participation among frailty-screened older adults. The DNN provided the most balanced performance. Each model exhibited distinct characteristics suitable for different screening purposes, with information-collection ability emerging as a key factor. The findings suggest that models must be carefully selected based on specific community health screening objectives.
Full article
(This article belongs to the Collection Frailty in Older Adults)
►▼
Show Figures

Figure 1
Open AccessArticle
Association Between Ultra-Processed Food Consumption Frequency and Frailty: Findings from the InCHIANTI Study of Aging
by
Xin Li, Yichen Jin, Stefania Bandinelli, Luigi Ferrucci, Toshiko Tanaka and Sameera A. Talegawkar
Geriatrics 2025, 10(5), 123; https://doi.org/10.3390/geriatrics10050123 - 11 Sep 2025
Abstract
Background/Objectives: As individuals age, they experience declines in multiple physiological domains, which increases their vulnerability to health challenges and frailty. While adherence to healthy dietary patterns has been shown to protect against frailty, consuming ultra-processed foods (UPFs)—which are high in added sugars and
[...] Read more.
Background/Objectives: As individuals age, they experience declines in multiple physiological domains, which increases their vulnerability to health challenges and frailty. While adherence to healthy dietary patterns has been shown to protect against frailty, consuming ultra-processed foods (UPFs)—which are high in added sugars and saturated fat—may contribute to frailty risk. This study investigates the association between UPF consumption and frailty progression among 938 participants aged 65 years and older who were in the InCHIANTI study, Italy. Methods: The patients’ dietary intakes over the past year were assessed using a validated food frequency questionnaire, with items categorized into food groups based on the Nova classification. Frailty was operationalized using a 42-item frailty index (FI). Multivariable linear regression was used to examine the association between the baseline UPF consumption frequency and baseline frailty status, while linear mixed-effects models were used to examine the frailty progression over time. Results: Overall, the participants with the lowest UPF consumption frequency were younger, had more years of education, and had a lower baseline FI. Higher UPF consumption was significantly associated with a greater baseline FI after adjustments for the sociodemographic and health characteristics (β = 0.026, 95% CI = 0.010–0.041, p = 0.001), and this difference persisted over a 16.1-year follow-up period (β = 0.022, 95% CI = 0.006–0.037, p = 0.006). Conclusions: These findings underscore the potential negative health impacts of UPF on frailty prevalence and progression in older adults.
Full article
Open AccessSystematic Review
Effects of the Prescription of Physical Exercises Mediated by Mobile Applications on the Health of Older Adults: A Systematic Review
by
Débora Vanessa Santos Dias Costa, Evellin Pereira Dourado, Mayara Bocchi Fernandes, Eduardo Vignoto Fernandes and David Michel de Oliveira
Geriatrics 2025, 10(5), 122; https://doi.org/10.3390/geriatrics10050122 - 10 Sep 2025
Abstract
Background/Objectives: Aging and a sedentary lifestyle aggravate hypokinetic diseases, compromising the functional capacity of older adults. Thus, the prescription of physical exercise (PE) through mobile applications (MA) has emerged as a remote and personalized alternative. However, there are still gaps in the effectiveness
[...] Read more.
Background/Objectives: Aging and a sedentary lifestyle aggravate hypokinetic diseases, compromising the functional capacity of older adults. Thus, the prescription of physical exercise (PE) through mobile applications (MA) has emerged as a remote and personalized alternative. However, there are still gaps in the effectiveness of prescribing physical exercise via mobile apps for older people. This study aimed to analyze the effects of prescribing PE through MAs on the health of older adults. Materials and Methods: This systematic review included studies with older people (≥60 years) that used MAs to prescribe PE, published between 2014 and 2024, in Portuguese or English. The search strategy used the descriptors “older adults,” “physical exercise,” “mobile applications,” and “health,” combined with Boolean operators. The screening followed previously defined eligibility criteria regarding population, intervention, outcomes, and study design. Two independent reviewers extracted data, mediated by a third party in case of disagreement; they screened and extracted data from the PubMed and VHL/Medline databases from 2004 to 2024. Risk of bias was assessed according to levels of evidence, and the results were categorized. Results: Of the 2298 publications initially identified, 7 studies were eligible for this review, totaling 748 participants, predominantly female. The studies included prospective and observational clinical trials with older people suffering from Parkinson’s disease, cardiovascular disease, sarcopenia, and breast cancer. The findings showed favorable effects on adherence to the program (6 studies; n = 654), an increase in PE (5 studies; n = 502), and improvements in functional capacity (4 studies; n = 389), perceived quality of life (5 studies; n = 481), and muscle strength (3 studies; n = 298). Conclusions: The prescription of MA-mediated PE showed positive effects on the health of older people, indicating its viability as a complementary strategy in clinical practice or public health.
Full article
(This article belongs to the Topic Exercise and Human Aging: Physiological and Psychological Functions)
►▼
Show Figures

Figure 1
Open AccessArticle
Sleep Disturbances and Dementia in the UK South Asian Community: A Qualitative Study to Inform Future Adaptation of the DREAMS-START Intervention
by
Penny Rapaport, Malvika Muralidhar, Sarah Amador, Naaheed Mukadam, Ankita Bhojwani, Charles Beeson and Gill Livingston
Geriatrics 2025, 10(5), 121; https://doi.org/10.3390/geriatrics10050121 - 8 Sep 2025
Abstract
Background/Objectives: Little is known about experiences of sleep disturbance in dementia amongst South Asian families, the UK’s biggest minority ethnic group. We aimed to explore their experiences of these alongside translation and preliminary cultural adaptation of an existing effective multicomponent intervention, DREAMS-START.
[...] Read more.
Background/Objectives: Little is known about experiences of sleep disturbance in dementia amongst South Asian families, the UK’s biggest minority ethnic group. We aimed to explore their experiences of these alongside translation and preliminary cultural adaptation of an existing effective multicomponent intervention, DREAMS-START. Methods: We interviewed family carers of people living with dementia who had participated in the DREAMS-START (n = 7) trial or other dementia studies (n = 4), conducting reflective thematic analysis. We translated DREAMS-START into Hindi and consulted with Hindi speakers with experience in dementia care, revising iteratively. Results: We identified two overarching themes: (i) the experience of dementia-related sleep disturbance in South Asian families, including the impact of multigenerational living, cultural expectations and practices, and existing relationships; and (ii) considerations for culturally adapting DREAMS-START, including language barriers, linguistic and other changes to peripheral elements to increase engagement and relevance, and culturally competent facilitation of the intervention. Conclusions: Consideration of multigenerational family structures, within-member dynamics, culturally appropriate activities and lack of access to support are important during consultation and intervention. It was thought that cultural adaptation of the intervention in language and facilitator cultural competence, including consideration of the schedule of prayer, would increase relevance and thus community access. We will use this preliminary work to inform future cultural adaptation and testing of the intervention with the intention to widen access for UK-based South Asian families.
Full article
(This article belongs to the Section Geriatric Psychiatry and Psychology)
►▼
Show Figures

Figure 1
Open AccessArticle
Cognitive Function and Subjective Well-Being in Japanese Community-Dwelling Older Adults: A Cross-Sectional Study
by
Baoxing Li, Tianshu Chu, Ziming Gong, Le Tian and Hiro Kishimoto
Geriatrics 2025, 10(5), 120; https://doi.org/10.3390/geriatrics10050120 - 6 Sep 2025
Abstract
►▼
Show Figures
Background: The relationship between mild cognitive impairment (MCI) and subjective well-being remains poorly understood. We examined associations between cognitive function and well-being domains in community-dwelling older Japanese adults with and without MCI. Subjects and Methods: A cross-sectional analysis of 710 community-dwelling
[...] Read more.
Background: The relationship between mild cognitive impairment (MCI) and subjective well-being remains poorly understood. We examined associations between cognitive function and well-being domains in community-dwelling older Japanese adults with and without MCI. Subjects and Methods: A cross-sectional analysis of 710 community-dwelling Japanese adults aged 65–75 years was carried out. Well-being was measured using the Philadelphia Geriatric Center Morale Scale (PGCMS score ≥ 13 indicates high well-being), comprising agitation, attitude toward aging, and lonely dissatisfaction subscales. MCI was defined as a Montreal Cognitive Assessment (MoCA) score of 18–25. Multivariable logistic regression examined potential associations between socio-demographic and health factors. Results: Among the participants (mean age 70.0 ± 2.5 years, 49% women), 423 (59.6%) had MCI. The MCI status was not associated with overall well-being (OR 1.06, 95% CI: 0.72–1.57, p = 0.77). However, within the MCI group, each 1-point increase in the MoCA score was associated with lower agitation (OR 1.21, 95% CI: 1.04–1.41) but higher lonely dissatisfaction (OR 0.83, 95% CI: 0.70–0.98, p = 0.02). No associations were observed in the non-MCI group. Conclusions: Cognitive function shows domain-specific rather than global associations with well-being in individuals with MCI.
Full article

Figure 1
Open AccessArticle
Floor-to-Stand Transfers in Older Adults: Insights into Strategies and Lower Extremity Demands
by
Lyndsay Stutzenberger and Tyler Whited
Geriatrics 2025, 10(5), 119; https://doi.org/10.3390/geriatrics10050119 - 6 Sep 2025
Abstract
Background/Objectives: Getting up from the floor is an important functional skill for independence in older adults but is not often assessed clinically. The purpose of this study was to investigate how floor-to-stand transfer (FTS) ability is related to self-report measures and five-time sit-to-stand
[...] Read more.
Background/Objectives: Getting up from the floor is an important functional skill for independence in older adults but is not often assessed clinically. The purpose of this study was to investigate how floor-to-stand transfer (FTS) ability is related to self-report measures and five-time sit-to-stand (5XSTS) performance, as well as compare peak joint angles during common FTS strategies and lower extremity demands between the 5XSTS and a commonly instructed FTS strategy. Methods: Thirty-four community-dwelling older adults completed self-report measures and performed the 5XSTS, a FTS in a self-selected manner, and an instructed FTS strategy. Biomechanical analysis of the lower extremities was used to determine peak joint angles, moments, and powers during study tasks. Correlation analyses were used to determine associations between FTS time and self-report scores, 5XSTS time, and lower extremity demands during the 5XSTS. One-way analysis of variance (ANOVA) and Kruskal–Wallis tests were used to determine the differences in self-report measures, 5XSTS performance, and FTS time between self-selected FTS strategies. Lower extremity demands between the 5XSTS and the instructed FTS strategy were compared with Wilcoxon Signed-Rank tests. Results: Self-report measures were not associated with FTS time or different between FTS strategies. Knee flexion was greater in the roll-over compared to the quadruped strategy (p < 0.001). Ankle and hip demands were greater during the instructed FTS, and knee demands were greater during the 5XSTS (p < 0.001) when comparing the tasks. Conclusions: The study findings may improve clinical decision-making related to FTS assessment and interventions in older adults. Prescribing exercises with greater hip and ankle demand than the 5XSTS may help maximize FTS ability.
Full article
(This article belongs to the Topic Exercise and Human Aging: Physiological and Psychological Functions)
►▼
Show Figures

Graphical abstract
Highly Accessed Articles
Latest Books
E-Mail Alert
News
Topics
Topic in
Behavioral Sciences, Brain Sciences, Geriatrics
Psychopathology and Developmental Trajectories
Topic Editors: Donatella Rita Petretto, Carmelo Masala, Stefan BogaertsDeadline: 31 December 2025
Topic in
Diagnostics, Geriatrics, JCDD, Medicina, JPM, Medicines
New Research on Atrial Fibrillation
Topic Editors: Michele Magnocavallo, Domenico G. Della Rocca, Stefano Bianchi, Pietro Rossi, Antonio BisignaniDeadline: 31 March 2026
Topic in
Geriatrics, IJMS, Life, Sports, Neurology International, Obesities
Exercise and Human Aging: Physiological and Psychological Functions
Topic Editors: Samuel Da Silva Aguiar, Ismael Perez-SuarezDeadline: 20 September 2026
Topic in
AI, Geriatrics, JAL, Healthcare
AI-Driven Smart Elderly Care: Innovations and Solutions
Topic Editors: Mahmoud Elkhodr, Ergun GideDeadline: 30 June 2027

Special Issues
Special Issue in
Geriatrics
Chronic Kidney Disease and Pharmacoepidemiology in Older Individuals: Challenges, Insights, and Therapeutic Advances
Guest Editor: Luca SoraciDeadline: 15 December 2025
Special Issue in
Geriatrics
Current Issues in Cognitive Testing of Older Adults
Guest Editors: Ruth Marchand Tappen, Mónica RosselliDeadline: 31 January 2026
Special Issue in
Geriatrics
Comprehensive Geriatric Assessment of Older Surgical Patients
Guest Editors: David Shipway, Frances RickardDeadline: 20 March 2026
Special Issue in
Geriatrics
Neurodegenerative Diseases, Physical Fitness, and Exercise Interventions in Aging
Guest Editors: José Daniel Jiménez García, Antonio Martinez-AmatDeadline: 30 April 2026
Topical Collections
Topical Collection in
Geriatrics
Joint Arthroplasty in the Oldest People
Collection Editors: Juan F. Blanco, Carmen da Casa
Topical Collection in
Geriatrics
Ageism, the Black Sheep of the Decade of Healthy Ageing
Collection Editor: Lydia Gimenez Llort
Topical Collection in
Geriatrics
Responding to the Pandemic: Geriatric Care Models
Collection Editor: James Powers
Topical Collection in
Geriatrics
Molecular Mechanisms of Obesity, Diabetes, Inflammation and Aging
Collection Editors: Yuxiang Sun, Susanne Talcott








