COVID-19 Infection among Older People Admitted to Hospital: A Cross-Sectional Analysis
Abstract
:1. Introduction
2. Materials and Methods
3. Results
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Wu, Z.; McGoogan, J.M. Characteristics of and Important Lessons from the Coronavirus Disease 2019 (COVID-19) Outbreak in China: Summary of a Report of 72,314 Cases From the Chinese Center for Disease Control and Prevention. JAMA 2020, 323, 1239–1242. [Google Scholar] [CrossRef]
- Onder, G.; Rezza, G.; Brusaferro, S. Case-Fatality Rate and Characteristics of Patients Dying in Relation to COVID-19 in Italy. JAMA 2020, 323, 1775–1776. [Google Scholar] [CrossRef]
- National Institutes of Health, Malaysia. Clinical Update in Covid-19. Available online: http://www.nih.gov.my/covid-19 (accessed on 14 January 2021).
- Ministry of Health. Covid-19 Malaysia. Available online: http://covid-19.moh.gov.my/terkini (accessed on 14 January 2021).
- Guan, W.J.; Liang, W.H.; Zhao, Y.; Liang, H.R.; Chen, Z.S.; Li, Y.M.; Liu, X.Q.; Chen, R.C.; Tang, C.L.; Wang, T.; et al. Comorbidity and its impact on 1590 patients with Covid-19 in China: A Nationwide Analysis. Eur. Respir. J. 2020, 55, 2000547. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rawle, M.J.; Bertfield, D.L.; Brill, S.E. Atypical presentations of COVID-19 in care home residents presenting to secondary care: A UK single centre study. Aging Med. (Milton) 2020, 3, 237–244. [Google Scholar] [CrossRef] [PubMed]
- Davis, P.; Gibson, R.; Wright, E.; Bryan, A.; Ingram, J.; Lee, R.P.; Godwin, J.; Evans, T.; Burleigh, E.; Wishart, S.; et al. Atypical presentations in the hospitalised older adult testing positive for SARS-CoV-2: A retrospective observational study in Glasgow, Scotland. Scott. Med. J. 2020. [Google Scholar] [CrossRef]
- Mustaffa, N.; Lee, S.Y.; Mohd Nawi, S.N.; Che Rahim, M.J.; Chee, Y.C.; Muhd Besari, A.; Lee, Y.Y. COVID-19 in the elderly: A Malaysian perspective. J. Glob. Health. 2020, 10, 020370. [Google Scholar] [CrossRef]
- Rockwood, K.; Theou, O. Using the Clinical Frailty Scale in Allocating Scarce Health Care Resources. Can. Geriatr. J. 2020, 23, 210–215. [Google Scholar] [CrossRef]
- Sim, B.L.H.; Chidambaram, S.K.; Wong, X.C.; Pathmanathan, M.D.; Peariasamy, K.M.; Hor, C.P.; Chua, H.J.; Goh, P.P. Clinical characteristics and risk factors for severe COVID-19 infections in Malaysia: A nationwide observational study. Lancet Reg. Health West. Pac. 2020, 4, 100055. [Google Scholar] [CrossRef] [PubMed]
- Mendes, A.; Serratrice, C.; Herrmann, F.R.; Genton, L.; Périvier, S.; Scheffler, M.; Fassier, T.; Huber, P.; Jacques, M.C.; Prendki, V.; et al. Predictors of In-Hospital Mortality in Older Patients With COVID-19: The COVIDAge Study. J. Am. Med. Dir. Assoc. 2020, 21, 1546–1554.e3. [Google Scholar] [CrossRef] [PubMed]
- Wei, C.; Liu, Y.; Liu, Y.; Zhang, K.; Su, D.; Zhong, M.; Meng, X. Clinical characteristics and manifestations in older patients with COVID-19. BMC Geriatr. 2020, 20, 395. [Google Scholar] [CrossRef]
- Sun, H.; Ning, R.; Tao, Y.; Yu, C.; Deng, X.; Zhao, C.; Meng, S.; Tang, F.; Xu, D. Risk factors for mortality in 244 older adults with COVID-19 in Wuhan, China: A retrospective study. J. Am. Geriatr. Soc. 2020, 68, E19–E23. [Google Scholar] [CrossRef]
- Zazzara, M.B.; Penfold, R.S.; Roberts, A.L.; Lee, K.A.; Dooley, J.; Sudre, C.H.; Welch, C.; Bowyer, R.C.E.; Visconti, A.; Mangino, M.; et al. Probable delirium is a presenting symptom of COVID-19 in frail, older adults: A cohort study of 322 hospitalised and 535 community-based older adults. Age Ageing 2021, 50, 40–48. [Google Scholar] [CrossRef]
- Kennedy, M.; Helfand, B.; Gou, R.Y.; Gartaganis, S.L.; Webb, M.; Moccia, J.M.; Bruursema, S.N.; Dokic, B.; McCulloch, B.; Ring, H.; et al. Delirium in Older Patients With COVID-19 Presenting to the Emergency Department. JAMA Netw. Open 2020, 3, e2029540. [Google Scholar] [CrossRef]
- Poloni, T.E.; Carlos, A.F.; Cairati, M.; Cutaia, C.; Medici, V.; Marelli, E.; Ferrari, D.; Galli, A.; Bognetti, P.; Davin, A.; et al. Prevalence and prognostic value of Delirium as the initial presentation of COVID-19 in the elderly with dementia: An Italian retrospective study. EClinicalMedicine 2020, 26, 100490. [Google Scholar] [CrossRef] [PubMed]
- Achar, A.; Ghosh, C. COVID-19-Associated Neurological Disorders: The Potential Route of CNS Invasion and Blood-Brain Relevance. Cells 2020, 9, 2360. [Google Scholar] [CrossRef] [PubMed]
- Inouye, S.K.; Charpentier, P.A. Precipitating factors for delirium in hospitalized elderly persons. Predictive model and interrelationship with baseline vulnerability. JAMA 1996, 275, 852–857. [Google Scholar] [CrossRef] [PubMed]
- Huang, J.T.; Ran, R.X.; Lv, Z.H.; Feng, L.N.; Ran, C.Y.; Tong, Y.Q.; Li, D.; Su, H.W.; Zhu, C.L.; Qiu, S.L.; et al. Chronological Changes of Viral Shedding in Adult Inpatients With COVID-19 in Wuhan, China. Clin. Infect Dis. 2020, 71, 2158–2166. [Google Scholar] [CrossRef] [PubMed]
- Faíco-Filho, K.S.; Passarelli, V.C.; Bellei, N. Is Higher Viral Load in SARS-CoV-2 Associated with Death? Am. J. Trop. Med. Hyg. 2020, 103, 2019–2021. [Google Scholar] [CrossRef]
- He, X.; Lau, E.H.Y.; Wu, P.; Deng, X.; Wang, J.; Hao, X.; Lau, Y.C.; Wong, J.Y.; Guan, Y.; Tan, X.; et al. Temporal dynamics in viral shedding and transmissibility of COVID-19. Nat. Med. 2020, 26, 672–675. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Liu, Y.L.; Liao, W.; Wan, L.; Xiang, T.; Zhang, W. Correlation between relative nasopharyngeal virus RNA load and lymphocyte count disease severity in patients with COVID-19. Viral Immunol. 2020. [Google Scholar] [CrossRef] [Green Version]
- Shah, S.; Singhal, T.; Davar, N.; Thakkar, P. No correlation between Ct values and severity of disease or mortality in patients with COVID 19 disease. Indian J. Med. Microbiol. 2020. [Google Scholar] [CrossRef]
- Wölfel, R.; Corman, V.M.; Guggemos, W. Virological assessment of hospitalized patients with COVID-2019. Nature 2020, 581, 465–469. [Google Scholar] [CrossRef] [Green Version]
- Popkin, M.B.; Du, S.; Green, W.D.; Beck, M.A.; Algaith, T.; Herbst, C.H.; Alsukait, R.F.; Alluhidan, M.; Alazemi, N.; Shekar, M. Individuals with obesity and COVID-19: A global perspective on the epidemiology and biological relationships. Obes. Rev. 2020, 21, e13128. [Google Scholar] [CrossRef]
- Leung, C. Risk factors for predicting mortality in elderly patients with COVID-19: A review of clinical data in China. Mech. Ageing Dev. 2020, 188, 111255. [Google Scholar] [CrossRef]
- Chinnadurai, R.; Ogedengbe, O.; Agarwal, P.; Money-Coomes, S.; Abdurrahman, A.Z.; Mohammed, S.; Kalra, P.A.; Rothwell, N.; Pradhan, S. Older age and frailty are the chief predictors of mortality in COVID-19 patients admitted to an acute medical unit in a secondary care setting- a cohort study. BMC Geriatr. 2020, 20, 409. [Google Scholar] [CrossRef] [PubMed]
- Zuin, M.; Guasti, P.; Roncon, L.; Cervellati, C.; Zuliani, G. Dementia and the risk of death in elderly patients with COVID-19 infection: Systematic review and meta-analysis. Int. J. Geriatr. Psychiatry 2021. [Google Scholar] [CrossRef]
- Hasmuk, K.; Sallehuddin, H.; Tan, M.P.; Cheah, W.K.; Ibrahim, R.; Chai, S.T. The Long Term Care COVID-19 Situation in Malaysia. Available online: https://ltccovid.org/wp-content/uploads/2020/05/Malaysia-LTC-COVID-situation-report-30-May.pdf (accessed on 11 January 2021).
- Emanuel, E.J.; Persad, G.; Upshur, R.; Thome, B.; Parker, M.; Glickman, A.; Zhang, C.; Boyle, C.; Smith, M.; Phillips, J.P. Fair Allocation of Scarce Medical Resources in the Time of Covid-19. N. Engl. J. Med. 2020, 382, 2049–2055. [Google Scholar] [CrossRef]
- O’Mara, L.; Streiter, S.; Orkaby, A.R.; Ouchi, K.; Bernacki, R. A Framework to Triage Older Adults with Covid-19 to Provide Patient-Centered Care. NEJM Catal. Innov. Care Deliv. 2020. [Google Scholar] [CrossRef]
- Ritchey, K.C.; Foy, A.; McArdel, E.; Gruenewald, D.A. Reinventing Palliative Care Delivery in the Era of COVID-19: How Telemedicine Can Support End of Life Care. Am. J. Hosp. Palliat Care 2020, 37, 992–997. [Google Scholar] [CrossRef] [PubMed]
- Rivi, V.; Melegari, G.; Blom, J.M. How to humanise the COVID-19 intensive care units. BMJ Evid. Based Med. 2021. [Google Scholar] [CrossRef] [PubMed]

| All, N = 26 | Alive, N = 20 | Death, N = 6 | ||
|---|---|---|---|---|
| n (%) | n (%) | n (%) | p | |
| Age, mean (SD) years | 76.2(8.2) | 74.5(7.6) | 81.8(8.0) | 0.053 |
| Female | 15(57.7%) | 12(60.0%) | 3(50.0%) | >0.999 |
| Nursing home resident | 8(30.8%) | 5(25.0%) | 3(50.0%) | 0.330 |
| BADL a independent | 15(57.7%) | 13(65.0%) | 2(33.3%) | 0.348 |
| Ambulation with aids/wheelchair | 12(46.2%) | 8(40.0%) | 4(66.7%) | 0.365 |
| Clinical Frailty Scale ≥ 4 | 13(50.0%) | 8(40.0%) | 5(83.3%) | 0.160 |
| Hospital-acquired COVID-19 | 9(34.6%) | 5(25.0%) | 4(66.7%) | 0.138 |
| Comorbidities | ||||
| Diabetes Mellitus | 16(61.5%) | 14(70.0%) | 2(33.3%) | 0.163 |
| Hypertension | 22(84.6%) | 19(95.0%) | 3(50.0%) | 0.028 |
| IHD/CCF b | 5(19.2%) | 5(25.0%) | 0 | 0.298 |
| Chronic kidney disease | 5(19.2%) | 3(15.0%) | 2(33.3%) | 0.558 |
| Dementia | 8(30.8%) | 4(20.0%) | 4(66.7%) | 0.051 |
| Stroke | 8(30.8%) | 5(25.0%) | 3(50.0%) | 0.330 |
| Charlson Comorbidity Index, median (IQR) | 6.0(3.5–7.0) | 6.0(3.0–7.0) | 5.5(4.0–7.3) | 0.458 |
| Use of ARB/ACE-I c- before admission | 12(46.2%) | 11(55.0%) | 1(16.7%) | 0.170 |
| Presenting symptoms | ||||
| Symptomatic on admission | 23(88.5%) | 17(85.0%) | 6(100.0%) | >0.999 |
| Fever | 11(42.3%) | 8(40.0%) | 3(50.0%) | >0.999 |
| Respiratory symptoms d | 14(53.8%) | 12(60.0%) | 2(33.3%) | 0.365 |
| Gastrointestinal symptoms e | 9(34.6%) | 9(45.0%) | 0 | 0.063 |
| Loss of appetite | 10(38.5%) | 9(45.0%) | 1(16.7%) | 0.352 |
| Lethargy | 10(38.5%) | 6(30.0%) | 4(66.7%) | 0.163 |
| Delirium on presentation | 7(26.9%) | 3(15.0%) | 4(66.7%) | 0.028 |
| Laboratory parameters | ||||
| Haemoglobin, g/dL, mean (SD) | 12.15(2.48) | 12.09(1.91) | 12.38(4.27) | 0.889 |
| White cell count ×109 L, median (Q1–Q3) | 6.90(5.90–9.90) | 6.60(5.30–7.88) | 8.10(6.16–13.10) | 0.628 |
| Absolute lymphocyte count ×109 L, median (Q1–Q3) | 1.28(1.03–2.11) | 1.41(1.11–2.29) | 1.00(0.91–1.41) | 0.061 |
| Absolute neutrophil count ×109 L, median (Q1–Q3) | 4.02(3.11–6.60) | 3.93(2.68–5.21) | 6.60(4.62–10.58) | 0.031 |
| Urea, mmol/L, median (Q1–Q3) | 6.8(5.3–12.4) | 6.9(4.4–15.3) | 8.0(6.3–13.0) | 0.724 |
| Creatinine, mmol/L median (IQR) | 78.0(68.0–103.0) | 89.0(52.5–114.5) | 78.0(73.5–149.5) | 0.667 |
| Albumin, g/L, mean (SD) | 29.0(7.6) | 29.6(5.9) | 26.8(12.0) | 0.079 |
| Ferritin, ng/mL, median (Q1–Q3) | 561(360–1174) | 556(360–784) | 1176(574–2224) | 0.090 |
| C-Reactive Protein, mg/L, median (Q1–Q3) | 21.3(11.4–127.4) | 19.9(11.4–39.2) | 168.0(39.1–211.7) | 0.073 |
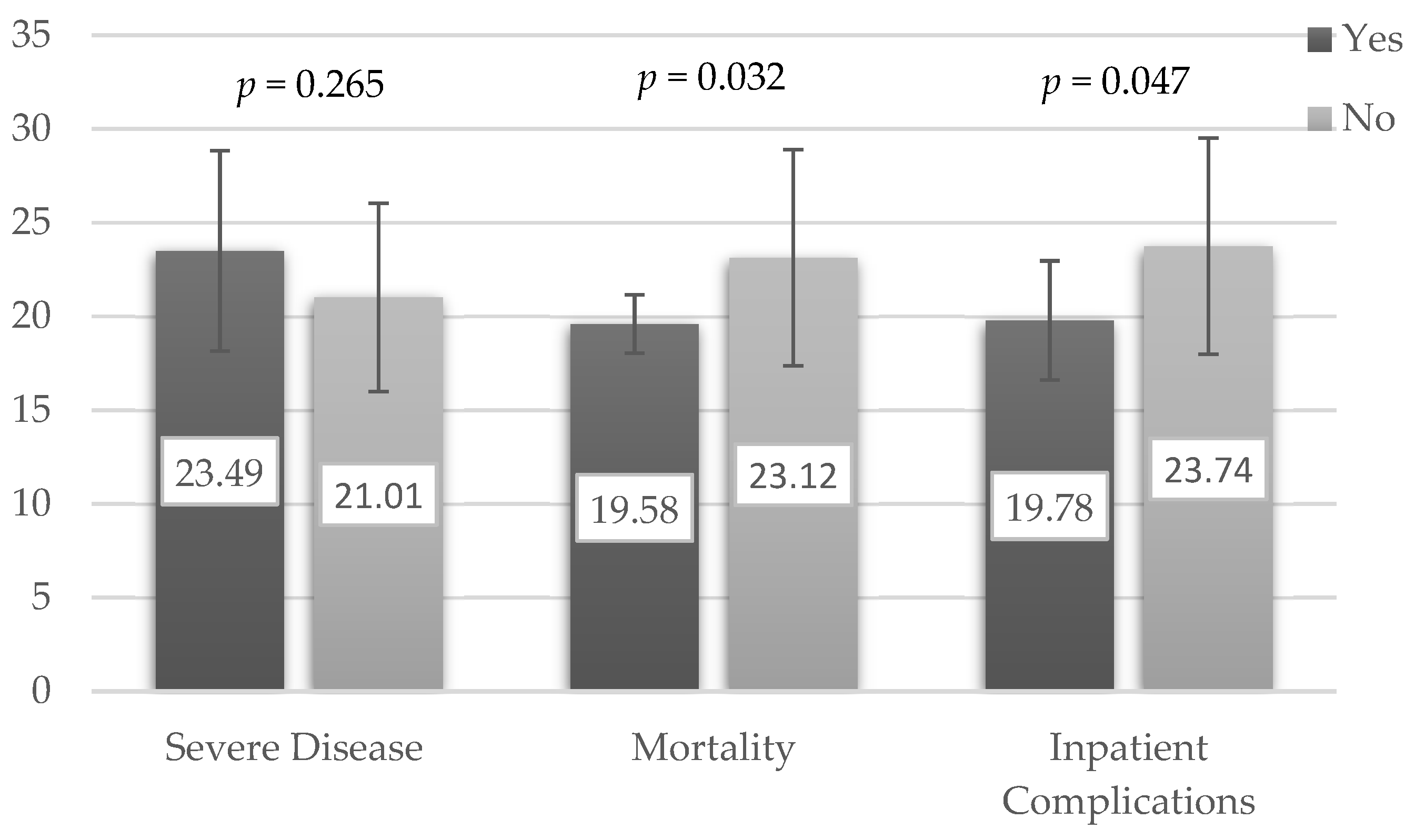
| Lowest Ct-value f, mean(SD) | 22.35(5.29) | 23.11(5.77) | 19.58(1.56) | 0.032 |
| Treatment | ||||
| Concomitant antibiotic use | 18(69.2%) | 13(65.0%) | 5(83.3%) | 0.628 |
| COVID-19 targeted therapy | 12(46.2%) | 11(55.0%) | 1(16.7%) | 0.170 |
| VTE g prophylaxis | 9(34.6%) | 8(40.0%) | 1(16.7%) | 0.380 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Thiam, C.N.; Hasmukharay, K.; Lim, W.C.; Ng, C.C.; Pang, G.H.M.; Abdullah, A.; Saedon, N.I.; Khor, H.M.; Ong, T. COVID-19 Infection among Older People Admitted to Hospital: A Cross-Sectional Analysis. Geriatrics 2021, 6, 25. https://doi.org/10.3390/geriatrics6010025
Thiam CN, Hasmukharay K, Lim WC, Ng CC, Pang GHM, Abdullah A, Saedon NI, Khor HM, Ong T. COVID-19 Infection among Older People Admitted to Hospital: A Cross-Sectional Analysis. Geriatrics. 2021; 6(1):25. https://doi.org/10.3390/geriatrics6010025
Chicago/Turabian StyleThiam, Chiann Ni, Kejal Hasmukharay, Wan Chieh Lim, Chai Chen Ng, Gordon Hwa Mang Pang, Aimy Abdullah, Nor Izzati Saedon, Hui Min Khor, and Terence Ong. 2021. "COVID-19 Infection among Older People Admitted to Hospital: A Cross-Sectional Analysis" Geriatrics 6, no. 1: 25. https://doi.org/10.3390/geriatrics6010025
APA StyleThiam, C. N., Hasmukharay, K., Lim, W. C., Ng, C. C., Pang, G. H. M., Abdullah, A., Saedon, N. I., Khor, H. M., & Ong, T. (2021). COVID-19 Infection among Older People Admitted to Hospital: A Cross-Sectional Analysis. Geriatrics, 6(1), 25. https://doi.org/10.3390/geriatrics6010025






