The Impact of Drug Interactions in Patients with Community-Acquired Pneumonia on Hospital Length of Stay
Abstract
:1. Introduction
2. Materials and Methods
2.1. Design
2.2. Sample and Setting
2.3. Data Collection
2.4. Data Analysis
2.5. Ethical Considerations
3. Results
3.1. Impact of Drug Interaction on LOS for the Total Cohort
3.2. Impact of Drug Interaction on LOS for the Cohort of ≥80 Years old
4. Discussion
Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Chatterji, S.; Byles, J.; Cutler, D.; Seeman, T.; Verdes, E. Health, Functioning, and Disability in Older Adults—Present Status and Future Implications. Lancet Lond. Engl. 2015, 385, 563–575. [Google Scholar] [CrossRef] [Green Version]
- Krankenhäuser Müssen Sich Auf Mehr Alte Patienten Einstellen. Available online: https://www.aerzteblatt.de/nachrichten/105173/Krankenhaeuser-muessen-sich-auf-mehr-alte-Patienten-einstellen (accessed on 27 October 2021).
- Global Burden of Disease Study 2013 Collaborators. Global, Regional, and National Incidence, Prevalence, and Years Lived with Disability for 301 Acute and Chronic Diseases and Injuries in 188 Countries, 1990–2013: A Systematic Analysis for the Global Burden of Disease Study 2013. Lancet Lond. Engl. 2015, 386, 743–800. [Google Scholar] [CrossRef] [Green Version]
- Garin, N.; Koyanagi, A.; Chatterji, S.; Tyrovolas, S.; Olaya, B.; Leonardi, M.; Lara, E.; Koskinen, S.; Tobiasz-Adamczyk, B.; Ayuso-Mateos, J.L.; et al. Global Multimorbidity Patterns: A Cross-Sectional, Population-Based, Multi-Country Study. J. Gerontol. Ser. A Biol. Sci. Med. Sci. 2016, 71, 205–214. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Afshar, S.; Roderick, P.J.; Kowal, P.; Dimitrov, B.D.; Hill, A.G. Multimorbidity and the Inequalities of Global Ageing: A Cross-Sectional Study of 28 Countries Using the World Health Surveys. BMC Public Health 2015, 15, 776. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Internetredaktion, R.B.L. Wie Krank Sind wir Wirklich?-Erstmals Liegen Verlässliche Daten zu Mehrfacherkrankungen im Alter vor-DLR Gesundheitsforschung. Available online: https://www.gesundheitsforschung-bmbf.de/de/wie-krank-sind-wir-wirklich-erstmals-liegen-verlassliche-daten-zu-mehrfacherkrankungen-im-3113.php (accessed on 27 October 2021).
- Aiden, H. Understanding the Challenge. Available online: https://richmondgroupofcharities.org.uk/sites/default/files/multimorbidity_-_understanding_the_challenge.pdf (accessed on 27 October 2021).
- Moßhammer, D.; Haumann, H.; Mörike, K.; Joos, S. Polypharmacy-an Upward Trend with Unpredictable Effects. Dtsch. Arzteblatt Int. 2016, 113, 627–633. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Alsuwaidan, A.; Almedlej, N.; Alsabti, S.; Daftardar, O.; Al Deaji, F.; Al Amri, A.; Alsuwaidan, S. A Comprehensive Overview of Polypharmacy in Elderly Patients in Saudi Arabia. Geriatrics 2019, 4, 36. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Aggarwal, P.; Woolford, S.J.; Patel, H.P. Multi-Morbidity and Polypharmacy in Older People: Challenges and Opportunities for Clinical Practice. Geriatrics 2020, 5, 85. [Google Scholar] [CrossRef] [PubMed]
- Lau, M.H.M.; Tenney, J.W. Evaluation of Drug-Disease Interactions and Their Association with Unplanned Hospital Readmission Utilizing STOPP Version 2 Criteria. Geriatrics 2017, 2, 33. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Simonson, W.; Feinberg, J.L. Medication-Related Problems in the Elderly: Defining the Issues and Identifying Solutions. Drugs Aging 2005, 22, 559–569. [Google Scholar] [CrossRef] [PubMed]
- Tangiisuran, B.; Davies, J.G.; Wright, J.E.; Rajkumar, C. Adverse Drug Reactions in a Population of Hospitalized Very Elderly Patients. Drugs Aging 2012, 29, 669–679. [Google Scholar] [CrossRef] [PubMed]
- Gesundheitsausgaben im Jahr 2018 um 4% Gestiegen. Available online: https://www.destatis.de/DE/Presse/Pressemitteilungen/2020/05/PD20_164_23611.html (accessed on 27 October 2021).
- Ärzteblatt, D.Ä.G. Redaktion Deutsches Pflegemangel im Krankenhaus: Die Situation Wird Immer Dramatischer. Available online: https://www.aerzteblatt.de/archiv/198658/Pflegemangel-im-Krankenhaus-Die-Situation-wird-immer-dramatischer (accessed on 27 October 2021).
- Wohlgemuth, A.; Michalowsky, B.; Wucherer, D.; Eichler, T.; Thyrian, J.R.; Zwingmann, I.; Rädke, A.; Hoffmann, W. Drug-Related Problems Increase Healthcare Costs for People Living with Dementia. J. Alzheimers Dis. JAD 2020, 73, 791–799. [Google Scholar] [CrossRef] [PubMed]
- Davies, E.C.; Green, C.F.; Taylor, S.; Williamson, P.R.; Mottram, D.R.; Pirmohamed, M. Adverse Drug Reactions in Hospital In-Patients: A Prospective Analysis of 3695 Patient-Episodes. PLoS ONE 2009, 4, e4439. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kolditz, M.; Tesch, F.; Mocke, L.; Höffken, G.; Ewig, S.; Schmitt, J. Burden and Risk Factors of Ambulatory or Hospitalized CAP: A Population Based Cohort Study. Respir. Med. 2016, 121, 32–38. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Breitling, L.P.; Saum, K.-U.; Schöttker, B.; Holleczek, B.; Herth, F.J.; Brenner, H. Pneumonia in the Noninstitutionalized Older Population. Dtsch. Arzteblatt Int. 2016, 113, 607–614. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Institut für Qualitätssicherung und Transparenz im Gesundheitswesen Beschreibung der Qualitätsindikatoren und Kennzahlen Nach QSKH-RL Ambulant Erworbene Pneumonie. 2019. Available online: https://iqtig.org/downloads/auswertung/2019/pneu/QSKH_PNEU_2019_BUAW_V02_2020-07-14.pdf (accessed on 29 November 2021).
- Official Webside of the “Institut für das Entgeltsystem im Krankenhaus” (InEK). Available online: https://www.g-drg.de/aG-DRG-System_2020/Definitionshandbuch/Definitionshandbuch_2020InEKGmbH (accessed on 4 December 2021).
- AiDKlinik®—Dosing GmbH Heidelberg. Available online: https://www.dosing-gmbh.de/produktloesungen/aidklinik-2/ (accessed on 4 December 2021).
- Wagner, R. Welche Auswirkungen hat ein elektronisches Arzneimittel-Informations- und CDS-System auf den Medikationsprozess? Untersuchung in Apotheke und stationärem Bereich eines Klinikums der Maximalversorgung. Available online: https://archiv.ub.uni-heidelberg.de/volltextserver/27902/ (accessed on 4 December 2021).
- R: The R Project for Statistical Computing. Available online: https://www.r-project.org/ (accessed on 4 December 2021).
- Hilbe, J.M. Modeling Count Data. In International Encyclopedia of Statistical Science; Lovric, M., Ed.; Springer: Berlin/Heidelberg, Germany, 2011; pp. 836–839. ISBN 978-3-642-04898-2. [Google Scholar]
- Becker, M.L.; Visser, L.E.; van Gelder, T.; Hofman, A.; Stricker, B.H.C. Increasing Exposure to Drug-Drug Interactions between 1992 and 2005 in People Aged > or = 55 Years. Drugs Aging 2008, 25, 145–152. [Google Scholar] [CrossRef] [PubMed]
- Geer, M.I.; Koul, P.A.; Tanki, S.A.; Shah, M.Y. Frequency, Types, Severity, Preventability and Costs of Adverse Drug Reactions at a Tertiary Care Hospital. J. Pharmacol. Toxicol. Methods 2016, 81, 323–334. [Google Scholar] [CrossRef] [PubMed]
- Brahma, D.; Wahlang, J.; Marak, M.; Sangma, M.C. Adverse Drug Reactions in the Elderly. J. Pharmacol. Pharmacother. 2013, 4, 91. [Google Scholar] [CrossRef] [PubMed]
- Moura, C.S.; Acurcio, F.A.; Belo, N.O. Drug-Drug Interactions Associated with Length of Stay and Cost of Hospitalization. J. Pharm. Pharm. Sci. 2009, 12, 266. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Holt, S.; Schmiedl, S.; Thürmann, P.A. Potentially Inappropriate Medications in the Elderly: The PRISCUS List. Dtsch. Arzteblatt Int. 2010, 107, 543–551. [Google Scholar] [CrossRef]
| Variable | Total | Age < 65 Years | Age 65–79 Years | Age ≥ 80 Years |
|---|---|---|---|---|
| N (%) | 547 (100) | 94 (21) | 164 (36) | 199 (44) |
| Age, mean (±SD) | 74.0 (±15.3) | 49.5 (±11.7) | 73.1 (±4.1) | 86.4 (±4.7) |
| Gender | ||||
| Male | 224 (49) | 36 (38) | 97 (59) | 91 (46) |
| Female | 233 (51) | 58 (62) | 67 (41) | 108 (54) |
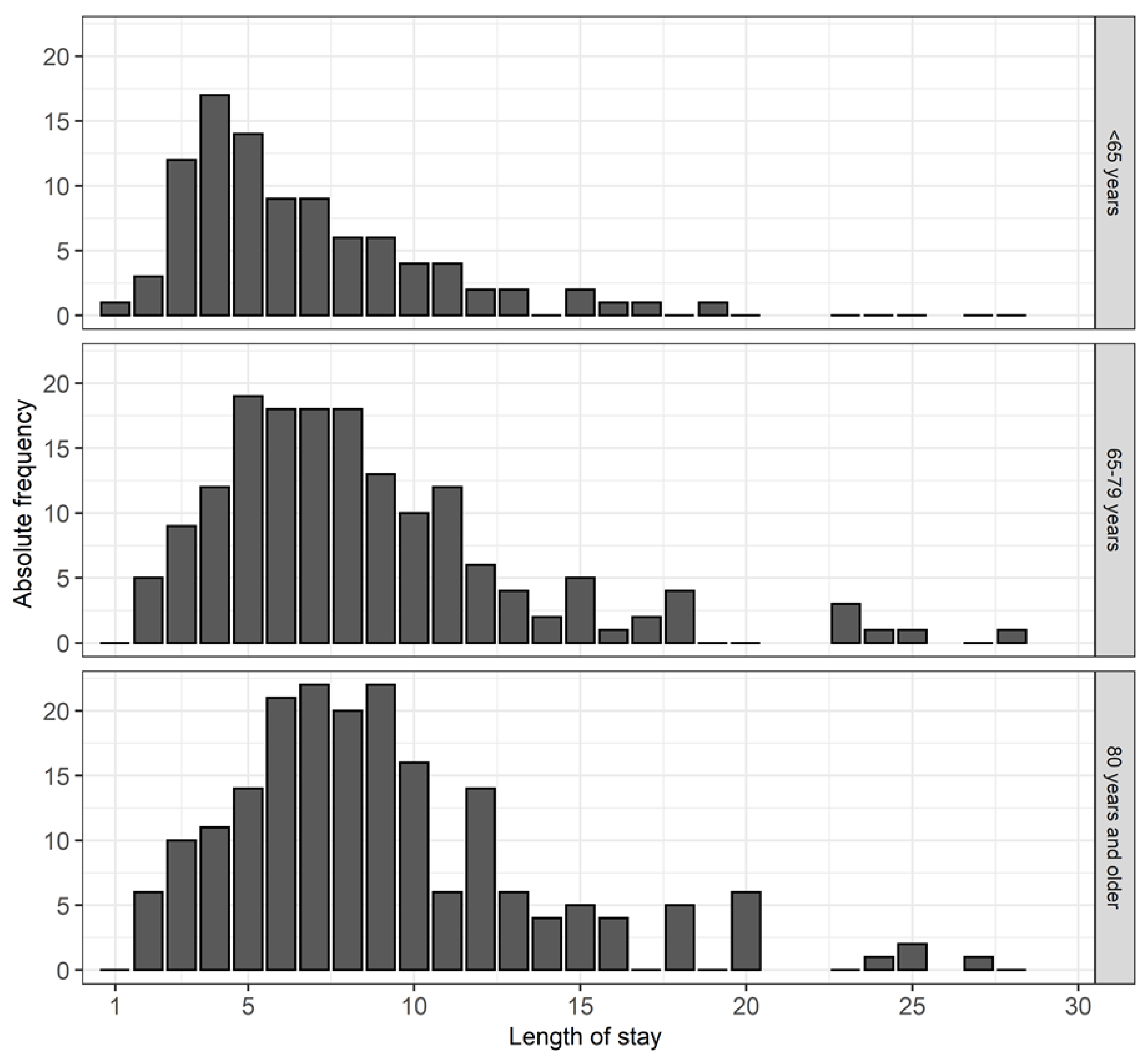
| Length of stay, mean (±SD) | 8.5 (±5.0) | 6.6 (±3.6) | 8.6 (±4.8) | 9.4 (±5.6) |
| PCCL | ||||
| 0 | 134 (29) | 45 (48) | 44 (27) | 45 (23) |
| 1 | 56 (12) | 9 (10) | 18 (11) | 29 (15) |
| 2 | 65 (14) | 11 (12) | 28 (17) | 26 (13) |
| 3 | 136 (30) | 23 (25) | 49 (30) | 64 (32) |
| 4 | 66 (14) | 6 (6) | 25 (15) | 35 (18) |
| No. of drug interaction | ||||
| none | 207 (35) | 62 (66) | 73 (45) | 72 (36) |
| 1–2 interactions | 115 (25) | 22 (23) | 32 (20) | 61 (31) |
| >2 interaction | 135 (30) | 10 (11) | 59 (36) | 66 (33) |
| Intensity of drug interaction | ||||
| none/mild | 227 (50) | 64 (70) | 82 (50) | 79 (40) |
| moderate, severe and/or contraindicated | 230 (50) | 28 (30) | 82 (50) | 120 (60) |
| Variable | RR | 95% CI of RR | p Value |
|---|---|---|---|
| Intercept | 4.88 | ||
| PCCL (ref: 0) | <0.001 | ||
| 1 | 1.10 | 0.94–1.28 | |
| 2 | 1.47 | 1.28–1–69 | |
| 3 | 1.36 | 1.20–1.53 | |
| 4 | 1.86 | 1.61–2.14 | |
| Age (ref: <65 years) | 0.017 | ||
| 65–79 | 1.09 | 0.97–1.24 | |
| ≥80 | 1.18 | 1.05–1.34 | |
| No. of drug interactions | 1.02 | 1.01–1.04 | 0.005 |
| Intensity of drug interactions (ref: none/mild) | <0.001 | ||
| moderate, severe, and/or contraindicated | 1.22 | 1.09–1.37 |
| Variable | RR | 95% CI of RR | p Value |
|---|---|---|---|
| Intercept | 5.63 | ||
| PCCL (ref: 0) | <0.001 | ||
| 1 | 1.17 | 0.92–1.49 | |
| 2 | 1.59 | 1.26–2.02 | |
| 3 | 1.46 | 1.20–1.78 | |
| 4 | 1.73 | 1.39–2.16 | |
| No. of drug interaction | 1.03 | 1.00–1.06 | 0.025 |
| Intensity of drug interactions (ref: none/mild) | 0.071 | ||
| moderate, severe, and/or contraindicated | 1.18 | 0.99–1.40 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Schmitt, J.P.; Kirfel, A.; Schmitz, M.-T.; Kohlhof, H.; Weisbarth, T.; Wittmann, M. The Impact of Drug Interactions in Patients with Community-Acquired Pneumonia on Hospital Length of Stay. Geriatrics 2022, 7, 11. https://doi.org/10.3390/geriatrics7010011
Schmitt JP, Kirfel A, Schmitz M-T, Kohlhof H, Weisbarth T, Wittmann M. The Impact of Drug Interactions in Patients with Community-Acquired Pneumonia on Hospital Length of Stay. Geriatrics. 2022; 7(1):11. https://doi.org/10.3390/geriatrics7010011
Chicago/Turabian StyleSchmitt, Johannes Peter, Andrea Kirfel, Marie-Therese Schmitz, Hendrik Kohlhof, Tobias Weisbarth, and Maria Wittmann. 2022. "The Impact of Drug Interactions in Patients with Community-Acquired Pneumonia on Hospital Length of Stay" Geriatrics 7, no. 1: 11. https://doi.org/10.3390/geriatrics7010011







