Home Monitoring of Oxygen Saturation Using a Low-Cost Wearable Device with Haptic Feedback to Improve Sleep Quality in a Lung Cancer Patient: A Case Report
Abstract
:1. Introduction
2. Case Report and Methods
2.1. Case Description
2.2. Materials and Methods
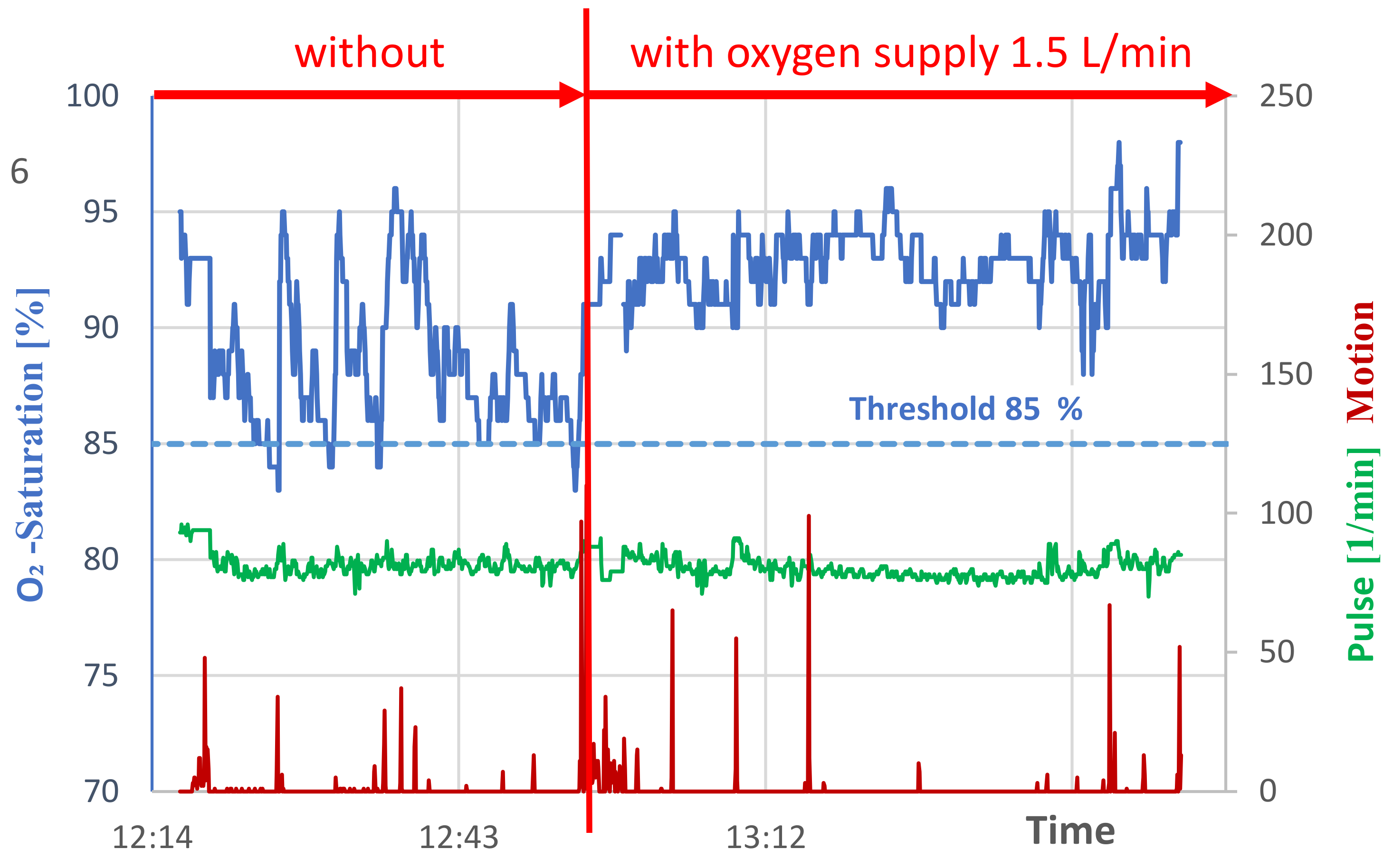
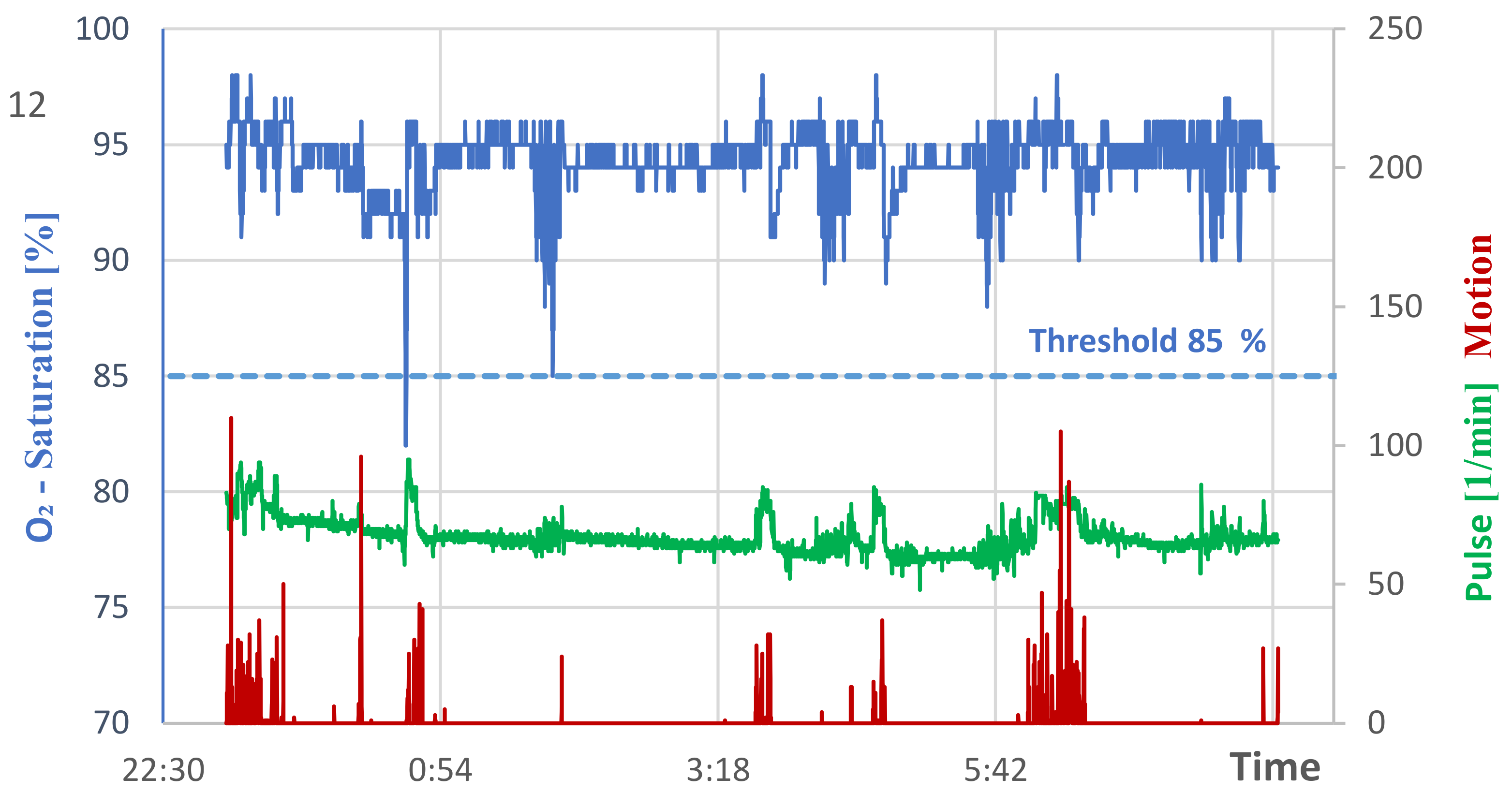
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Sokwoo, R.; Boo-Ho, Y.; Kuowei, C.; Asada, H.H. The ring sensor: A new ambulatory wearable sensor for twenty-four hour patient monitoring. In Proceedings of the 20th Annual International Conference of the IEEE Engineering in Medicine and Biology Society. Vol. 20 Biomedical Engineering Towards the Year 2000 and Beyond (Cat. No. 98CH36286), Hong Kong, China, 1 November 1998; IEEE: Manhattan, NY, USA, 1998; pp. 1906–1909. [Google Scholar] [CrossRef]
- Forra Wakidi, L.; Hari Wisana, I.D.; Miftahul Maghfiroh, A.; Sharma, V.K. Apnea monitor using pulse oxymetry with tactile stimulation to reduce respiration failure. J. Electron. Electromed. Eng. Med. Inform. 2021, 3, 79–84. [Google Scholar] [CrossRef]
- Chen, Q.; Tang, L. A wearable blood oxygen saturation monitoring system based on bluetooth low energy technology. Comput. Commun. 2020, 160, 101–110. [Google Scholar] [CrossRef]
- Fu, Y.; Liu, J. System design for wearable blood oxygen saturation and pulse measurement device. Procedia Manuf. 2015, 3, 1187–1194. [Google Scholar] [CrossRef] [Green Version]
- Hang, L.W.; Wang, H.L.; Chen, J.H.; Hsu, J.C.; Lin, H.H.; Chung, W.S.; Chen, Y.F. Validation of overnight oximetry to diagnose patients with moderate to severe obstructive sleep apnea. BMC Pulm. Med. 2015, 15, 24. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sanfilippo, F.; Pettersen, K.Y. A sensor fusion wearable health-monitoring system with haptic feedback. In Proceedings of the 11th International Conference on Innovations in Information Technology (IIT), Dubai, United Arab Emirates, 1–3 November 2015; IEEE: Manhattan, NY, USA, 2015; pp. 262–266. [Google Scholar] [CrossRef]
- Brugarolas, R.; Valero-Sarmiento, J.M.; Brna, A. Wearable SpO2 and sleep posture monitoring system for obstructive sleep apnea patients. In Proceedings of the IEEE Virtual Conference on Applications of Commercial Sensors (VCACS), Raleigh, NC, USA, 15 March–15 October 2015; IEEE: Manhattan, NY, USA, 2015; pp. 1–6. [Google Scholar] [CrossRef]
- Adiputra, R.R.; Hadiyoso, S.; Hariyani, Y.S. Internet of things: Low cost and wearable SpO2 device for health monitoring. Int. J. Electr. Comput. Eng. 2018, 8, 939. [Google Scholar] [CrossRef]
- Nitzan, M.; Nitzan, I.; Arieli, Y. The various oximetric techniques used for the evaluation of blood oxygenation. Sensors 2020, 20, 4844. [Google Scholar] [CrossRef] [PubMed]
- Muratyan, A.; Cheung, W.; Dibbo, S.V.; Vhaduri, S. Opportunistic multi-modal user authentication for health-tracking IoT wearables. arXiv 2021, arXiv:2109.13705. [Google Scholar] [CrossRef]
- Martins, S.J.; Ho, N.; Cavamura, S.O.; Harada, C.M.; Yamamoto, C.A.; Takagaki, T.Y. Lung cancer symptoms and pulse oximetry in the prognostic assessment of patients with lung cancer. BMC Cancer 2005, 5, 72. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zander, R. Pathophysiologie des Arteriellen O2-Status. Available online: https://www.physioklin.de/physiooxy/pathophysiologie-des-arteriellen-o2-status.html (accessed on 12 October 2021).
- Siemieniuk, R.A.C.; Chu, D.K.; Kim, L.H.-Y.; Güell-Rous, M.R.; Alhazzani, W.; Soccal, P.M.; Karanicolas, P.J.; Farhoumand, P.D.; Siemieniuk, J.L.K.; Satia, I.; et al. Oxygen therapy for acutely ill medical patients: A clinical practice guideline. BMJ 2018, 363, k4169. [Google Scholar] [CrossRef] [PubMed]
- Grensemann, J.; Wachs, C.; Kluge, S. Sauerstofftherapie in der Notfall- und Intensivmedizin. Dtsch. Med. Wochenschr. 2021, 146, 108–120. [Google Scholar] [CrossRef] [PubMed]

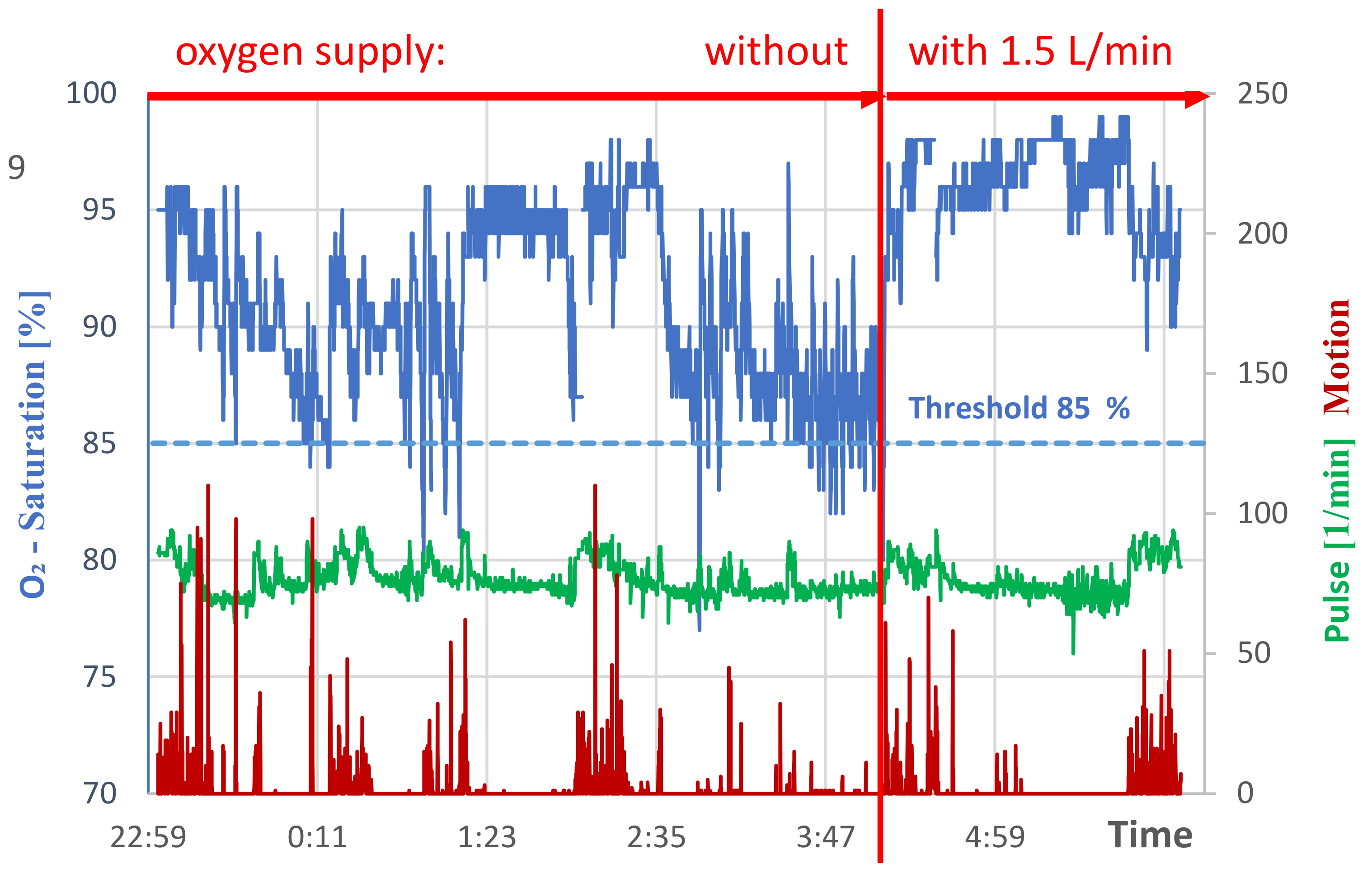
| Duration Sec. | Time from | to | Duration Sec. | Time from | to |
|---|---|---|---|---|---|
| 4 | 0:08:31 | 0:08:35 | 12 | 3:44:31 | 3:44:43 |
| 48 | 0:15:55 | 0:16:43 | 20 | 3:46:27 | 3:46:47 |
| 8 | 0:50:47 | 0:50:55 | 32 | 3:49:27 | 3:49:59 |
| 48 | 0:55:55 | 0:56:43 | 32 | 3:51:31 | 3:52:03 |
| 12 | 0:59:43 | 0:59:55 | 32 | 3:54:27 | 3:54:59 |
| 44 | 1:05:27 | 1:06:11 | 4 | 3:55:03 | 3:55:07 |
| 32 | 1:11:31 | 1:12:03 | 4 | 3:58:07 | 3:58:11 |
| 24 | 2:53:43 | 2:54:07 | 32 | 3:58:15 | 3:58:47 |
| 12 | 2:57:31 | 2:57:43 | 8 | 4:01:55 | 4:02:03 |
| 16 | 3:01:59 | 3:02:15 | 20 | 4:03:59 | 4:04:19 |
| 8 | 3:02:39 | 3:02:47 | 16 | 4:07:55 | 4:08:11 |
| 20 | 3:40:47 | 3:41:07 | 36 | 4:11:31 | 4:12:07 |
| 4 | 3:41:35 | 3:41:39 | 12 | 4:12:15 | 4:12:27 |
| Duration Sec. | Time from | to |
|---|---|---|
| 56 | 12:25:23 | 12:26:19 |
| 20 | 12:30:59 | 12:31:19 |
| 20 | 12:35:31 | 12:35:51 |
| 24 | 12:53:55 | 12:54:19 |
| Duration Sec. | Time from | to |
|---|---|---|
| 28 | 0:36:33 | 0:37:01 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lachenmeier, W.; Lachenmeier, D.W. Home Monitoring of Oxygen Saturation Using a Low-Cost Wearable Device with Haptic Feedback to Improve Sleep Quality in a Lung Cancer Patient: A Case Report. Geriatrics 2022, 7, 43. https://doi.org/10.3390/geriatrics7020043
Lachenmeier W, Lachenmeier DW. Home Monitoring of Oxygen Saturation Using a Low-Cost Wearable Device with Haptic Feedback to Improve Sleep Quality in a Lung Cancer Patient: A Case Report. Geriatrics. 2022; 7(2):43. https://doi.org/10.3390/geriatrics7020043
Chicago/Turabian StyleLachenmeier, Walter, and Dirk W. Lachenmeier. 2022. "Home Monitoring of Oxygen Saturation Using a Low-Cost Wearable Device with Haptic Feedback to Improve Sleep Quality in a Lung Cancer Patient: A Case Report" Geriatrics 7, no. 2: 43. https://doi.org/10.3390/geriatrics7020043
APA StyleLachenmeier, W., & Lachenmeier, D. W. (2022). Home Monitoring of Oxygen Saturation Using a Low-Cost Wearable Device with Haptic Feedback to Improve Sleep Quality in a Lung Cancer Patient: A Case Report. Geriatrics, 7(2), 43. https://doi.org/10.3390/geriatrics7020043







